Abstract
Background
Kidney transplant recipients are recognized as a vulnerable population that is at increased risk of adverse health outcomes. However, there have been few studies that have compared hospital-related morbidity of these patients to the general population, and how this differs with respect to time since transplantation. Such analyses are useful in estimating the health burden in this patient population.
Methods
We assembled a population-based Canadian cohort (excluding Quebec) of 6,116 kidney transplant recipients who underwent transplantation between 1 April 2001 and 31 December 2008. Record linkage was used to identify hospital discharge records of these patients from 1 April 2001 through 31 March 2009. Hospital discharges were tabulated across the main disease chapters of the ICD10, and person-years of follow-up were calculated across age and sex strata. Comparisons of hospital-related morbidity to the general population were made by using a standardized hospitalization ratio (SHR). For those who underwent transplantation in 2004, stratified analyses were performed to explore differences in hospital discharge rates both before and after transplantation.
Results
After excluding hospitalizations due to complications from transplantation, when compared to the general population, transplant recipients were approximately 6.4 (95% CI: 6.3, 6.5) times more likely to be hospitalized during follow-up. The SHRs were highest during the time periods proximate to transplantation, and then decreased to approximately a five-fold increase from 3 years post transplantation onwards. The largest disease-specific excesses were observed with infectious diseases and diseases of the endocrine system. Among those who underwent transplantation in 2004, the SHR decreased from 11.2 to 5.0 in the periods before and after surgery, respectively.
Conclusions
Our results indicate that, even more than 5-years post transplantation, there remains a more than six-fold difference in hospitalization rates relative to the general population. Additional work is needed to confirm these findings, and to develop strategies to reduce long-term morbidity in this patient population.
Similar content being viewed by others
Background
In Canada, the prevalence of end-stage renal disease has increased steadily over the past 20 years [1–3]. Kidney transplantation is the preferred treatment among individuals with end-stage renal disease, and improvements in treatment have produced a 1-year survival probability following transplantation that now exceeds 90% [4]. Improved survival implies a substantially increased opportunity to experience adverse health events post transplantation. Kidney transplant recipients have higher incidence rates of cancer, particularly non-Hodgkin’s lymphoma and skin cancer when compared to the general population [5, 6]. These recipients are also more likely to be at an increased risk of developing cardiovascular disease [7, 8], diabetes mellitus [9, 10], fractures [11–13], and infection [14] post transplantation. In addition, some have recently suggested that transplant patients are more likely than the general population to have higher rates of depression or other psychiatric illnesses [15, 16].
To date, there have been relatively few studies that have evaluated the long-term hospitalization patterns among kidney transplant patients. Those that have were typically single-center studies that have been focused on specific diseases and were based on relatively small numbers of transplant patients [9, 13, 15]. Hospitalization admissions patterns have previously been evaluated using data from the Dialysis Outcomes and Practice Patterns Study (DOPPS) that examined hospital admissions among dialysis patients. Unfortunately these analyses excluded transplant patients [17]. Another study [18] based on US transplant patients was more focused on statistical methods and did not provide comparisons to the general population. In our view, there is insufficient information to adequately characterize the long-term hospitalization burden in the post-transplant renal recipient.
This study aims to address two important research questions that remain unanswered. First, to what extent does transplantation reduce hospital-related morbidity among kidney transplant recipients post transplantation; and second, does the increased need for hospitalization among transplant recipients change with increasing time since transplantation? We used two population-based administrative datasets to create a longitudinal dataset that allows these research questions to be addressed.
Methods
Study population
Our study cohort was created by abstracting data from a national information system for renal and extra-renal organ failure and transplantation in Canada, the Canadian Organ Replacement Registry (CORR), which is maintained by the Canadian Institute for Health Information (CIHI). Data are provided to the CORR from all 27 kidney transplant programs across Canada. It has been estimated that the CORR covers approximate 99% of all transplant patients in Canada [19]. Patients included in this analysis consisted of those in the CORR database who underwent renal transplantation between 1 April 2001 and 31 December 2008. We restricted analyses to records that represented an individual’s first transplantation. Patients who underwent more than one kidney transplantation were excluded from analysis. Individual-level variables extracted from the CORR included date of birth, gender, province of residence, and vital status.
Ascertainment of hospital admissions
The hospitalization experience of the cohort members was determined by linking the personal identifiable data from the CORR to information from the Canadian Discharge Abstract Database (DAD) [20]. The DAD is a population-based database that contains information on all separations from acute care institutions, including discharges, deaths, sign-outs, and transfers (excluding Quebec). It has been estimated that the DAD captures >95% of all hospitalization in Canada (excluding Quebec).
The DAD and CORR record linkage process generated an analysis dataset for the time period between 1 April 2001 and 31 March 2009 identifying hospital discharges among the renal transplant patients. The Most Responsible Diagnosis was used at the time of hospital discharge to classify morbidity among the study population. Hospital admissions were classified based on International Classification of Diseases-10 version (ICD10) chapter definitions [21]. Since DAD does not capture information in Quebec, all records from Quebec in CORR were also excluded for the linkage and analysis.
Since hospitalization during the first couple of months after renal transplant likely reflects morbidity related to the transplant procedure itself, the follow-up interval within the first 60 days after the procedure was examined separately. Initially, a total of 6,116 renal transplant recipients who underwent transplantation between 1 April 2001 and 31 December 2008 were identified. Patients who ended the follow-up within the first 60 days after transplant (n=37) were analyzed only for the short-term follow-up in the study. In summary, our risk estimates for medium- and long-term hospital utilization were based on 6,079 renal transplant patients. All transplant patients were followed up until either death (between 1 April 2001 and 31 March 2009) or the end of the study (31 March 2009).
Statistical analysis
Person-years of follow-up and the number of hospitalizations were tabulated across strata defined by: 5-year age-group, sex (male, female), length of follow-up (<60 days, 60 days to <3 years, 3 years to <5 years, and 5 years and over), and calendar year (2001 to 2008). The DATAB module in the Epicure software program was used to tabulate these person-years [22]. Hospital discharge rates for the Canadian general population exclude Quebec were also obtained from the DAD, and were computed across the same age-group and sex strata.
Hospital discharge rates for the kidney transplant cohort were compared to those of the general population using the Standardized Hospitalization Ratio (SHR). The SHR represents the ratio of observed-to-expected numbers of hospital admissions, with the ‘expected’ reflecting the number of hospitalizations that would be expected in the transplant cohort if it had the same age-sex specific hospital discharge rates as the general population. The 95% confidence intervals (CIs) for the SHRs were constructed using the normal approximation [23].
Disease categories for complications of procedures/ transplanted organs rejection, follow-up examination and adjustment, and other supplementary classifications related to transplant procedure (ICD-10 codes: S01-T99, V01-Y98, and Z00-Z99) were investigated separately and not included in the SHRs comparison. Statistical significance was determined based on a two-tailed alpha of 5%. To adjust for differences in the sex and length of follow-up distribution, the stratified SHRs were also calculated. Analyses were repeated for each of the following main disease categories comprising the ICD-10. The proportions of hospital admission on major disease category were calculated by length of follow-up and compared to those in the general population.
To evaluate whether transplantation reduced morbidity, we conducted a period-rates comparison among individuals having sufficient follow-up time both before and after surgery. Specifically, among kidney transplant recipients who underwent transplantation between 1 April 2004 and 31 March 2005 we compared the SHRs in the pre-transplant (1 April 2001 to 31 March 2003) and post-transplant periods (1 April 2006 to 31 March 2008).
Results and discussion
Results
Descriptive statistics
The basic statistics for the study cohort are provided in Table 1. The cohort consisted of 6,116 renal failure patients who underwent transplantation between 1 April 2001 and 31 December 2008. The mean age of the recipients was 47.2 years, and the 25th and 75th age percentiles were 37.2 and 58.8, respectively. Approximately 62% of the cohort was male. In total, 22,619.3 person-years were accrued between the date of transplantation and the end of follow-up. Approximately 8% of the cohort (n=482) was deceased at the end of the follow-up interval, of which 37 patients died between within the first 60 days post transplant. In the study, 6,079 patients were followed-up for post-transplant hospital admissions commencing 60 days after the transplant.
Hospital admission rates
A total of 17,431 hospitalizations were observed among the kidney transplant recipients over the follow-up interval. After excluding patients with <60 days of follow-up and hospitalization for transplant procedure related causes, the total number of hospital admissions in this cohort was 14,147. The SHR was 6.4 relative to the Canadian general population, with similar ratios for men and women (male: SHR=6.2; female: SHR=6.5). Among disease categories, SHRs were most elevated for infectious diseases, endocrine disorders, and congenital anomalies. Complications of pregnancy in women was the only condition for which the hospitalization rates were lower among the kidney transplant patients relative to the general population (SHR=0.2) (Table 2).
During the first 60 days after the transplant procedure, 60% of hospital admissions were attributable to the procedure itself or to related causes which included complications of procedure, transplanted organs rejection, and follow-up examination and other factors influencing health status (Table 3). This decreased to 30% thereafter. After excluding procedure-related causes, during the first 60 days post transplant, the patient cohort experienced higher standardized hospitalization ratios due to infectious disease, endocrine and genitourinary disease, and lower SHRs for neoplasms and circulatory disease. In the long-term follow-up analysis the proportions of hospital admission of major causes of disease, such as circulatory disease and respiratory disease, tended to return closely to those in the general population (data not shown). There were significant differences on hospital admission rates by province during the follow-up periods. Between 2006 and 2008, the SHR in Ontario was 380/100,000 person-years which was significantly lower than British Columbia (508/100,000 person-years) and that of the Atlantic region (NB 583/100,000 person-years, NS 633/100,000 person-years, and NL 795/100,000 person-years).
In Table 3 SHRs of hospital admissions decreased by time since transplantation. In general, the highest SHR was observed in the period immediately after transplant procedure (<60 days); then it decreased and stabilized after 3 years post transplant. Excluding hospitalization <60 days after transplantation disease-specific SHRs were the highest for infectious diseases (SHR=38.9; 95% CI=36.0-42.0) and endocrine disorders (SHR=25.3, 95% CI=23.5-27.1). It is worth noting that the SHRs of infectious diseases and genitourinary diseases were extremely high, but decreased rapidly, while the SHRs for neoplasms and circulatory diseases were relatively stable throughout the follow-up intervals (3.0 and 4.5, respectively), excluding the fellow-up period of <60 days.
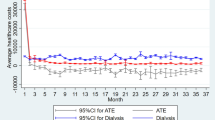
Figure 1 displays trends in the hospitalization rates by follow-up period. The highest hospitalization rates were in the first year of follow-up post transplant. After the first year, SHRs decreased considerably for the next 2 to 3 years of follow-up. After 3 to 4 years post transplant, hospitalization rates appeared to level off, and remained stable for the rest of the follow-up period. Figure 2 reveals that such trends were very similar when analyzed separately by age group.
Morbidity impact on transplant procedure
Table 4 provided hospital admission rates and SHRs of both pre- (1 April 2001 to 31 March 2003) and post- (1 April 2006 to 31 March 2008) transplant periods among patients who underwent transplantation in 2004. The overall pre-transplant hospital admission rate was 11 times higher than that of the general population while the post-transplant hospital admission rate was 5 times higher. The disease specific statistics shown the SHRs had reduced from 61 to 3 for blood disorders, 57 to 17 for endocrine disorders, 14 to 4 for circulatory diseases, and 43 to 13 for genitourinary diseases. In general, the post-transplant admission rate was about 40% of the pre-transplant hospital rate. With the exceptions of admissions for infection, neoplasms, and respiratory diseases, transplant patients had much lower hospital admission rates post transplantation compared to pre transplantation, especially for blood disorders, endocrine disorders, and circulatory and genitourinary diseases.
Discussion
This study found that kidney transplant recipients had higher hospital admission rates both overall and for many different disease groupings when compared to the general population. These results are consistent across the entire cohort and all the subgroup analyses. A similar observation of higher rates of hospitalization among kidney transplant recipients has been noted by Boubaker et al. who also reported that the most common causes of hospitalization in their study were infections and renal dysfunction [24]. Abbott el al. noted that renal transplant recipients were at high risk for hospitalizations for cytomegalovirus disease and fractures [25, 26].
In this patient cohort, the two most common causes of hospitalization were infectious diseases and endocrine disorders. This finding is consistent with other studies [14, 24, 27, 28]. However, over the follow-up period of the study, the hospitalizations for these diseases have decreased greatly. For example, the incidence of infection has dropped from approximately 70% to between 15% and 44% [14]. In our study, except for the first 60 days after a transplant procedure, close to 6% of total hospitalization was associated with infection through the study period. These reductions might be due to recent improvements in surgical techniques, immunosuppressive drugs, methods of diagnosis, and therapy. Urinary tract infection is the most common form of infection, and occurs in approximately 30% of patients within the first 3 months following transplantation [29]. Cytomegalovirus (CMV) is also a common infection among renal transplant patients [26]. The sole exception of an increased SHR was hospitalization due to complications of pregnancy which was likely due a much lower predisposition of transplant patients to become pregnant as these patients are likely older and may already have children or not want to become pregnant. Hospitalizations due to endocrine disorders are likely due to diabetes, a known complication of treatment with steroids. However the data are not granular enough to permit this to be ascertained.
The finding of the highest risk of hospital admission among those follow-up <60 days is not unexpected. This is likely related to the transplant procedure itself in addition to increased intensity of immune suppression during this period. Thereafter, SHR decreased over time, with a stable five-fold increased risk relative to the general population achieved at 3 years post transplant. The differences in hospitalization rates by province in particular between Ontario and BC or Atlantic region may be related to their follow-up care provision after transplant. In BC and Atlantic Canada patients are discharged to the community, and in the rest of the country (including Ontario) most care continues to be provided by the transplant centers.
Given the high quality and completeness in both CORR and DAD, it is reasonable to assume that losses to follow-up and primary diagnostic misclassification were low. As mentioned it has been estimated that <5% of hospital admissions would be missed across Canada (except Quebec), and therefore, the overall bias on the analysis should not be common. It is possible patients would be lost to follow-up if they moved outside the country after transplant procedure. However, given the medical needs of the kidney transplantation patients and the healthcare services provided within Canada, this number would be minimal.
Patients who underwent transplantation in 2004 could provide 2 years of hospital admission data for both pre transplant (2001 to 2003) and post transplant (2006 to 2008), allowing for a comparison of hospital admission between pre and post transplant except transplant procedure. The SHR decreased considerably pre to post transplant, from nearly 11 to approximately 5 suggesting that their overall health status improved significantly.
Caution should be exercised in interpreting the SHRs in this study. First, the DAD is an administrative database which only captures hospitalizations where patients were formally admitted to hospital and only those conditions severe enough to require hospitalization. It is unable to capture the morbidity among kidney transplant patients associated with increased visits to emergency departments where they are treated on an outpatient basis, or increased physician or prescription drug utilization. Second, biases may have been introduced from the patient selection process for transplantation. The selection criterion would differ by individual, and may reflect either a patient with optimum access to or with the most need for a transplant, or in sufficiently good health to be able to undergo transplantation. Since there is no patient level information on the criteria used to identify who underwent transplantation, the magnitude and the direction of the bias are unknown.
Conclusions
In summary, the present study confirmed and quantified kidney transplant patients’ much higher rates of hospitalization in reference to the general population. The highest cause specific excesses were from infectious diseases and endocrine disorders. Hospital admissions among the patient cohort decreased by time after transplant and reached equilibrium at 3 years. Subsequently, the post-transplant patients had a relative risk for hospitalization approximately 5 times than of the general population. These results may help guide the formulation and implementation of preventive programs after the transplant procedure.
Abbreviations
- CI:
-
Confidence interval
- CIHI:
-
Canadian Institute for Health Information
- CORR:
-
Canadian Organ Replacement Registry
- DAD:
-
Discharge abstract database
- ICD:
-
International Classification of Diseases
- SHR:
-
Standardized hospitalization ratio.
References
Schaubel DE, Morrison HI, Desmeules M, Parsons DA, Fenton SS: End-stage renal disease in Canada: prevalence projections to 2005. CMAJ. 1999, 160: 1557-1563.
Chauhan T: End-stage renal disease patients up nearly 19%. CMAJ. 2004, 170: 1087-
Canadian Institute for Health Information: 2012 CORR Report-Treatment of End-Stage Organ Failure in Canada. 2001, https://secure.cihi.ca/estore/productSeries.htm?pc=PCC24 , to 2010,
Pascual M, Theruvath T, Kawai T, Tolkoff-Rubin N, Cosimi AB: Strategies to improve long-term outcomes after renal transplantation. N Engl J Med. 2002, 346: 580-590. 10.1056/NEJMra011295.
Adami J, Gabel H, Lindelof B, Ekstrom K, Rydh B, Glimelius B, Ekbom A, Adami HO, Granath F: Cancer risk following organ transplantation: a nationwide cohort study in Sweden. Br J Cancer. 2003, 89: 1221-1227. 10.1038/sj.bjc.6601219.
Villeneuve PJ, Schaubel DE, Fenton SS, Shepherd FA, Jiang Y, Mao Y: Cancer incidence among Canadian kidney transplant recipients. Am J Transplant. 2007, 7: 941-948. 10.1111/j.1600-6143.2007.01736.x.
Kiberd BA: Cardiovascular disease in kidney transplant recipients. Johns Hopkins Adv Stud Med. 2007, 7: 169-178.
Kasiske BL, Guijarro C, Massy ZA, Wiederkehr MR, Ma JZ: Cardiovascular disease after renal transplantation. J Am Soc Nephrol. 1996, 7: 158-165.
Cosio FG, Pesavento TE, Osei K, Henry ML, Ferguson RM: Post-transplant diabetes mellitus: increasing incidence in renal allograft recipients transplanted in recent years. Kidney Int. 2001, 59: 732-737. 10.1046/j.1523-1755.2001.059002732.x.
Kasiske BL, Snyder JJ, Gilbertson D, Matas AJ: Diabetes mellitus after kidney transplantation in the United States. Am J Transplant. 2003, 3: 178-185. 10.1034/j.1600-6143.2003.00010.x.
Nisbeth U, Lindh E, Ljunghall S, Backman U, Fellstrom B: Increased fracture rate in diabetes mellitus and females after renal transplantation. Transplantation. 1999, 67: 1218-1222. 10.1097/00007890-199905150-00004.
Rodino MA, Shane E: Osteoporosis after organ transplantation. Am J Med. 1998, 104: 459-469. 10.1016/S0002-9343(98)00081-3.
Vautour LM, Melton LJ, Clarke BL, Achenbach SJ, Oberg AL, McCarthy JT: Long-term fracture risk following renal transplantation: a population-based study. Osteoporos Int. 2004, 15: 160-167. 10.1007/s00198-003-1532-y.
Silkensen JR: Long-term complications in renal transplantation. J Am Soc Nephrol. 2000, 11: 582-588.
Kalman TP, Wilson PG, Kalman CM: Psychiatric morbidity in long-term renal transplant recipients and patients undergoing hemodialysis. A comparative study. JAMA. 1983, 250: 55-58. 10.1001/jama.1983.03340010037025.
Tsunoda T, Yamashita R, Kojima Y, Takahara S: Risk factors for depression after kidney transplantation. Transplant Proc. 2010, 42: 1679-1681. 10.1016/j.transproceed.2009.12.073.
Rayner HC, Pisoni RL, Bommer J, Canaud B, Hecking E, Locatelli F, Piera L, Bragg-Gresham JL, Feldman HI, Goodkin DA, Gillespie B, Wolfe RA, Held PJ, Port FK: Mortality and hospitalization in haemodialysis patients in five European countries: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol Dial Transplant. 2004, 19: 108-120. 10.1093/ndt/gfg483.
Schaubel DE, Cai J: Analysis of clustered recurrent event data with application to hospitalization rates among renal failure patients. Biostatistics. 2005, 6: 404-419. 10.1093/biostatistics/kxi018.
Data Quality Study on the Canadian Organ Replacement Register: Canadian Institute for Health information. 2009, http://www.cihi.ca/CIHI-ext-portal/pdf/internet/CORR_DATA_QUALITY_STUDY_EN ,
Data Quality Documentation for External Users: Discharge Abstract Database, 2010--2011. Canadian Institute for Health information. 2011, http://www.cihi.ca/CIHI-ext-portal/pdf/internet/DAD_EXECUTIVE_SUM_10_11_EN ,
International Classification of Disease (ICD): 10 version. 2012, Geneva: World Health Organization, http://apps.who.int/classifications/icd/en/index.html ,
Preston DL, Lubin JH, Pierce DA, McConney M: EPICURE: Risk Regression and Data Analysis Software. 1996, Seattle, WA: Hirosoft International Corporation
Breslow NE, Day NE: Statistical Methods in Cancer Research. Volume II. The design and analysis of cohort study. 1987, International Agency for Research on Cancer: Lyon
Boubaker K, Harzallah A, Ounissi M, Becha M, Guergueh T, Hedri H, Kaaroud H, Abderrahim E, Ben Abdellah T, Kheder A: Rehospitalization after kidney transplantation during the first year: length, causes and relationship with long-term patient and graft survival. Transplant Proc. 2011, 43: 1742-1746. 10.1016/j.transproceed.2011.01.178.
Abbott KC, Oglesby RJ, Hypolite IO, Kirk AD, Ko CW, Welch PG, Agodoa LY, Duncan WE: Hospitalizations for fractures after renal transplantation in the United States. Ann Epidemiol. 2001, 11: 450-457. 10.1016/S1047-2797(01)00226-5.
Abbott KC, Hypolite IO, Viola R, Poropatich RK, Hshieh P, Cruess D, Hawkes CA, Agodoa LY: Hospitalizations for cytomegalovirus disease after renal transplantation in the United States. Ann Epidemiol. 2002, 12: 402-409. 10.1016/S1047-2797(01)00283-6.
Sagedal S, Hartmann A, Nordal KP, Osnes K, Leivestad T, Foss A, Degre M, Fauchald P, Rollag H: Impact of early cytomegalovirus infection and disease on long-term recipient and kidney graft survival. Kidney Int. 2004, 66: 329-337. 10.1111/j.1523-1755.2004.00735.x.
Dharnidharka VR, Agodoa LY, Abbott KC: Risk factors for hospitalization for bacterial or viral infection in renal transplant recipients—an analysis of USRDS data. Am J Transplant. 2007, 7: 653-661. 10.1111/j.1600-6143.2006.01674.x.
Tolkoff-Rubin NE, Rubin RH: Urinary tract infection in the immunocompromised host. Lessons from kidney transplantation and the AIDS epidemic. Infect Dis Clin North Am. 1997, 11: 707-717. 10.1016/S0891-5520(05)70381-0.
Acknowledgments
We thank Dr Graham Marko for his dedicated support on literature review and methodology preparation. We also thank the CIHI CORR/DAD data management team for all their assistance, especially data linkage.
This study was operationally supported by the Public Health Agency of Canada and the Canadian Institute for Health Information.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
YJ: linked datasets, analyzed data, drafted the manuscript. PV: participated in the data analysis and results interpretation. DS: critically revised the manuscript and helped to finalize the manuscript. YM: designed research and made substantial contributions to interpretation of data. PR: critically revised the manuscript and helped to finalize the manuscript. HM: critically revised the manuscript and gave final approval of the version to be published. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Jiang, Y., Villeneuve, P.J., Schaubel, D. et al. Long-term follow-up of kidney transplant recipients: comparison of hospitalization rates to the general population. Transplant Res 2, 15 (2013). https://doi.org/10.1186/2047-1440-2-15
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/2047-1440-2-15