Abstract
Objective
To compare the suitability of CO2 laser with steel instruments for margin excision in transoral laser microsurgery.
Methods
Prospective randomized blinded study. Patients with glottic cancer undergoing laser resection were randomized to margin excision by either steel instruments or CO2 laser. Margins were analyzed for size, interpretability and degree of artifact by a pathologist who was blinded to technique.
Results
45 patients were enrolled in the study with 226 total margins taken. 39 margins taken by laser had marked artifact and 0 were uninterpretable. 20 margins taken by steel instruments had marked artifact, and 2 were uninterpretable. Controlling for margin size, the laser technique was associated with increasing degrees of margin artifact (p = 0.210), but there was no difference in crude rates of uninterpretability (p = 0.24).
Conclusion
Laser margin excision is associated with a greater degree of artifact than steel instrument excision, but was not associated with higher rate of uninterpretability.
Similar content being viewed by others
Introduction
In 1972, Strong and Jako were the first to report the use of transoral laser microsurgery (TLM) in the treatment of glottic cancer [1]. Since the early 1990s, the indications for TLM have expanded to include all tumor categories of the upper aero-digestive tract [2–5]. Alongside with radiation therapy, TLM has become one of the primary modalities in the treatment of early glottic cancer [6–10]. In TLM, as with the rest of head and neck cancer surgery, local control is maximized by complete excision with adequate margins. Positive margin status in glottic cancer has been associated with increased risk of local recurrence and poorer prognosis [11–14].
Despite the importance of achieving clear margins in head and neck cancer surgery, there is no consensus on how wide a surgical margin is needed to be defined as “clear” [15–17]. In glottic cancer over excision of normal tissue can unnecessarily impair post-treatment vocal function. Several authors have suggested that in glottic cancer a margin can be considered free if the distance to the disease is at least 1 mm [15, 16, 18, 19].
The degree of artifact in margin specimens is another important factor that can affect the interpretation of a margin. An artifact on histological examination refers to an alteration of tissue or cellular structures that resulted from an external factor [20]. These artifacts can be attributed to either trauma from surgical instruments, or the various stages of histopathology slide preparation (fixation, processing, embedding, sectioning, or staining of tissues sections) [20, 21]. Artifacts from surgical excision technique can take many forms including crush injury, haemorrhage, splitting or fragmentation [20, 22–26]. In addition to these artifacts, the use of electrocautery and laser can cause tissue fulguration from the thermal damage [27]. As artifact increases, the interpretability of margins decreases. Uninterpretability or misinterpretation of a margin due to artifact can have significant effects on both downstream treatment pathways and prognosis for a patient.
Several modifications to the application of carbon dioxide (CO2) in TLM have been made to minimize the thermal damage. Many of these modifications have been studied in procedures involving benign lesions of the vocal cords. Several studies have showed that the use pulsed CO2 laser is superior and has better wound healing when compared to continuous wave CO2 laser as it allows tissue cutting and hemostasis while limiting thermal damage to surrounding tissues [28–31]. The two most common pulsed modes in TLM using CO2 laser are ultrapulse and superpulse (pulse duration < 1 millisecond), both perform a precise cut while producing less damage to the surrounding tissue [31]. Cutaneous and mucosal incisions made by CO2 laser in the continuous wave mode were compared to cold steel resulting in significant thermal damage to surrounding tissue and delayed wound healing [32–36]. However, when used in the pulsed mode for either benign vocal cord lesions or cutaneous incisions both vocal outcomes and wound healing were found to be comparable [34, 37, 38].
Removal of adequate glottic resection margins after TLM can be technically challenging, and margins must be taken precisely to balance the need for sufficient tissue to analyze while maximizing the preservation of normal tissue. Steel instruments have traditionally been used to take margins due to concerns regarding interpretation of margins with laser artifact. Unfortunately, margin resection with steel instruments does not have the hemostatic benefits of CO2 or the stabilized cutting of the micromanipulator. As the pulsed setting of the laser significantly reduces the amount of thermal damage and artifact, margins at our center have routinely been taken by ultrapulsed laser to achieve these benefits.
The main objective of this study is to compare the degree of artifact and the rate of uninterpretability for glottic cancer margin specimens when excised using either CO2 laser on ultrapulse mode or steel phonomicrosurgical instruments. Our hypothesis is that margin excision using CO2 laser on ultrapulse mode can be as interpretable as using steel instruments.
Methods
This is a blinded randomized trial approved by the Capital Health research ethics board. Patients were enrolled from multidisciplinary head and neck oncology clinic. All participants provided informed consent prior to inclusion in the study.
Subjects
All patients ≥ 18 years old undergoing TLM as primary modality for T1 or T2 glottic cancer from January 2010 to Dec 2011 were eligible for enrolment in the study. Patients with locally advanced glottic cancer (T3 & T4), undergoing TLM for recurrence, or salvage post-radiation therapy were excluded. Patients were randomized to margin excision with either CO2 laser or steel instruments using a computer generated random list. The patient and the pathologist were both blinded as to what technique was used for margin acquisition. Specimens were all submitted to the pathologist with a laryngeal template (Figure 1) indicating the site of excision without the mention of technique used. Only one pathologist (MB) and one surgeon (SMT) was involved in the study.
Surgical procedure
Patients were placed under general anaesthesia and intubated using laser resistant endotracheal tube. Laser safety measures were implemented to minimize the risk of complications from the laser surgery. Patients were placed in suspension laryngoscopy and an operative microscope with CO2 laser micromanipulator was used for glottic cancer excision. Carbon dioxide laser settings were 2-4 watts in ultrapulse mode. Depending on size, the tumours were removed either en bloc or via a tumour splitting technique. After primary tumor excision, margins were taken from the surgical site using either steel phonomicrosurgical instruments or CO2 laser at 2 watts based on our randomization list. The same phonomicrosurgical instruments were used to retract specimens for both cutting techniques. The locations of margins were diagrammed on the laryngeal template to assist the pathologist in their orientation.
Histopathology examination
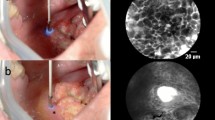
All margin specimens were sent to the same pathologist who was blinded to margin excision technique. Prior to the study, a trial of margin excision using both techniques was performed and reviewed with the pathologist to assess for obvious signs of thermal artifact. On histological analysis there weren’t any obvious difference between the two techniques, which allowed for blinding of the pathologist to technique. Histopathology slides were prepared as per standard protocol. The specimens were fixed in 10% formalin immediately following excision, paraffin-embedded and then 5-micron sections were stained with hematoxylin and eosin. For each margin, the pathologist was provided with three levels through the tissue at approximately 40-micron intervals. All margin specimens were examined for their size (following formalin fixation but prior to embedding in paraffin), malignancy/dysplasia status, and degree of artifact. For the study artifact was defined as an alteration of tissue or cellular structures that resulted from an external factor. The degree of artifact was divided into: none, minor, marked, and uninterpretable as defined in Table 1 and shown in Figure 2.
Examples of histological grading system for artifact. A) None: Well preserved surface epithelium, seromucinous glands and stroma. B) Minor: Well preserved surface epithelium. Seromucinous glands show some indistinct hyperchromatic areas (arrow). C) Marked: Surface epithelium is partially denuded with remainder showing severe artifact (arrow). Lamina propria is relatively preserved and can be assessed for invasive carcinoma (asterisk). D) Uninterpretable: Fragmented margin tissue with detached surface epithelium (arrow) and indistinct fragments of lamina propria.
Data collection & statistical analysis
Data collected included demographic information, procedural details (margin excision technique, number of margin specimens, and location of each margin), and pathological description (degree of differentiation, size of margin specimens, margin status for dysplasia and invasive carcinoma, degree of dysplasia, grade of carcinoma, and degree of artifact).
Statistical analysis was performed using Stata v11.2 (StataCorp, Texas). The sample size was calculated to have 0.8 power to detect a difference in proportions of 0.1 in the crude rates of uninterpretability between techniques with a two-tailed α of 0.05. A pre-planned analysis was used to determine the relationship between margin interpretability and harvest technique. The study included two primary endpoints. These were set as the relationship between harvest technique and uninterpretable margins, and the relationship between harvest technique and marked artifact or uninterpretable margins. Two-tailed Fisher exact tests were used for this analysis. For all tests, significance was set at an α < 0.05 level. A descriptive analysis was performed for demographic variables. Analyses of variables between assigned groups were performed using Fisher exact tests for categoric variables, and T-test for continuous variables.
The secondary endpoints were to the relationship between harvest technique and margin size and the relationship between harvest techniques and marked artifact/uninterpretable margins independent of margin size. This was performed to assess the potential role of vaporization and destruction of tissue caused by laser excision in the interpretability of margins. A t-test was used to determine the relationship between harvest technique and margin size. A logistic regression model, controlling for margin size, was used to analyse the relationship between harvest technique and presence of either marked artifact or uninterpretable margins.
Results
The study cohort was composed of 45 patients with 23 randomized to have margins taken by CO2 laser and 22 randomized to have margins taken with steel phonomicrosurgical instruments. See Table 2 for patient demographics. Overall, there were 226 margins taken, 115 margins taken with CO2 laser and 111 taken with steel phonomicrosurgical instruments (Table 3).
Primary analysis
There were no margins taken by laser (n=115) that were uninterpretable (0%), and 2 margins taken by steel instruments (n=111) that were uninterpretable (1.8%). The difference between these was not significant (p = 0.24). There were 39 (33.9%) margins taken by laser that had marked artifact, and 22 (19.8%) margins taken by steel instruments that had either marked artifact [20] or were uninterpretable [2]. The difference between these was statistically significant (p = 0.024) with margins taken by laser having a relative risk of 1.7 (95% CI 1.0-2.7) for having either marked artifact being uninterpretable.
Secondary analysis
The mean size of margins harvested by CO2 laser was 2.45 mm (95% CI 2.17-2.73 mm) and the mean size of margins harvested with steel instruments was 2.64 mm (95% CI 2.34-2.94 mm). This difference was not statistically significant (p = 0.37). The potential for laser to cause artifact by superficial vaporization of surface epithelium was also assessed (Table 4). After excluding deep margins, there were 89 margins taken by steel instruments and 94 margins taken by laser that were harvested from epithelial surfaces. Of these specimens, 36% and 38% of the margins harvested by steel and laser respectively had complete loss or destruction of the epithelium. Using Fisher’s exact test, the difference between these groups was not significant (p = 0.76). It is important to note that since the oncologic resection was performed by laser, at least one side of these already small margins would contain pre-existing thermal damage prior to margin harvest.
The planned logistic regression model for the relationship between technique and uninterpretable margins controlling for margin size could not be performed as all cases of uninterpretable margins occurred with steel instrument technique. Controlling for margin size, the laser technique for obtaining margins was associated with an odds ratio of 2.05 (95% CI 1.12-3.77) for obtaining either marked artifact or uninterpretable margins when compared to steel instrument technique. This relationship was statistically significant (p = 0.020) (Table 5). Independent of technique, an increase in margin size by 1 mm was associated with a non-significant (p = 0.31) decreased odds ratio of 0.9 for obtaining margins that were uninterpretable or had marked artifact.
Discussion
Positive margin status in glottic cancer is associated with increased risk of local recurrence and decreased disease specific survival [11–14]. Given these associations, surgical re-excision is warranted whenever possible. Rates of local recurrence are also significantly higher for glottic cancers resected with margins containing severe dysplasia or carcinoma in situ. It is generally recommended that these cases be considered for further surgical management in order to appropriately clear the margin [39–41].
We have introduced a classification system for artifact assessment in laser surgery for upper aero-digestive tract tumors. In this study, degree of artifact was classified into four categories: none, minor, marked, and uninterpretable. The classification schema is based on the presence of artifact and, when artifact is present, takes into account the impact on patient management of the resulting ability, or lack thereof, to interpret presence of dysplasia and invasive disease.
All surgical instruments can cause histological artifacts on microscopic examination [27, 42]. By causing tissue destruction or simulating pathological findings, the degree of artifact can affect the interpretability of surgical specimens. [43, 44] In cases with artifact affecting the surface epithelium, the changes can either prevent the diagnosis of dysplasia or can simulate dysplasia in non-dysplastic tissue. [44] Therefore, the pathologist has to disregard the areas with artifact and assess only those areas without artifact if they exist. Additionally, the laser may cause higher incidence of complete or partial denudation of the surface epithelium, leaving only the lamina propria. The latter can be assessed for the presence or absence of invasion, but not dysplasia.
There have been no previous studies comparing the effect of the use of CO2 laser to steel instruments on the interpretation of glottic cancer margin specimens. Our results demonstrated that the use of CO2 laser for margin harvest is associated with significantly higher odds of obtaining either a marked artifact or uninterpretable margins (p = 0.024).
A surprising finding in our study was the higher proportion of uninterpretable margins, but lower proportion of margins with marked artifact in the steel instrument group. It was expected that the degree of artifact would be distributed along a continuum, and that a higher proportion of uninterpretable margins would accompany a higher proportion of margins with marked artifact. The isolated finding of higher rates of uninterpretability in the steel instrument group was not statistically significant (p = 0.24) and the disparity between groups may represent an inadequate sample size. Alternatively, it could be due to differing mechanisms of artifact generation given the potential for the laser to denude the surface epithelium of these small specimens. This makes assessment of dysplasia impossible, while preserving the ability to interpret invasive malignancy. Steel instruments may preserve the epithelium more frequently, but may be more prone causing crush injury to an entire specimen making it completely uninterpretable. These potential differences in the mechanisms of artifact generation and rates of surface epithelium preservation between techniques are not supported by our current data.
Conclusion
Accurate assessment of surgical margins is a key factor in proper management and the predictive risk of local recurrence. The present study demonstrates that both steel instruments and CO2 laser cause a significant degree of artifact that can interfere with accurate margin assessment in TLM for early glottic cancer. The use of laser to harvest margins in our study was not associated with increased crude rates of uninterpretability for malignancy but was associated with increasing artifact affecting the ability of the pathologist to assess for dysplasia.
References
Strong MS, Jako GJ: Laser surgery in the larynx. Early clinical experience with continuous CO2 laser. Ann Otol Rhinol Laryngol. 1972, 81: 791-798.
Steiner W, Ambrosch P, Hess CF, Kron M: Organ preservation by transoral laser microsurgery in piriform sinus carcinoma. Otolaryngol Head Neck Surg. 2001, 124: 58-67. 10.1067/mhn.2001.111597.
Steiner W: Results of curative laser microsurgery of laryngeal carcinomas. Am J Otolaryngol. 1993, 14: 116-121. 10.1016/0196-0709(93)90050-H.
Steiner W: Experience in endoscopic laser surgery of malignant tumours of the upper aero-digestive tract. Adv Otorhinolaryngol. 1988, 39: 135-144.
Canis M, Ihler F, Wolff HA, Christiansen H, Matthias C, Steiner W: Oncologic and functional results after transoral laser microsurgery of tongue base carcinoma. Eur Arch Otorhinolaryngol. 2013, 270: 1075-1083. 10.1007/s00405-012-2097-1.
Ambrosch P: The role of laser microsurgery in the treatment of laryngeal cancer. Curr Opin Otolaryngol Head Neck Surg. 2007, 15: 82-88. 10.1097/MOO.0b013e3280147336.
Brondbo K, Benninger MS: Laser resection of T1a glottic carcinomas: results and postoperative voice quality. Acta Otolaryngol. 2004, 124: 976-979. 10.1080/00016480410017413.
Moreau PR: Treatment of laryngeal carcinomas by laser endoscopic microsurgery. Laryngoscope. 2000, 110: 1000-1006. 10.1097/00005537-200006000-00022.
Gallo A, de Vincentiis M, Manciocco V, Simonelli M, Fiorella ML, Shah JP: CO2 laser cordectomy for early-stage glottic carcinoma: a long-term follow-up of 156 cases. Laryngoscope. 2002, 112: 370-374. 10.1097/00005537-200202000-00030.
Ledda GP, Puxeddu R: Carbon dioxide laser microsurgery for early glottic carcinoma. Otolaryngol Head Neck Surg. 2006, 134: 911-915. 10.1016/j.otohns.2005.10.049.
Peretti G, Piazza C, Cocco D, De Benedetto L, Del Bon F, Redaelli De Zinis LO, Nicolai P: Transoral CO(2) laser treatment for T(is)-T(3) glottic cancer: the University of Brescia experience on 595 patients. Head Neck. 2010, 32: 977-983.
Crespo AN, Chone CT, Gripp FM, Spina AL, Altemani A: Role of margin status in recurrence after CO2 laser endoscopic resection of early glottic cancer. Acta Otolaryngol. 2006, 126: 306-310. 10.1080/00016480500316985.
Blanch JL, Vilaseca I, Caballero M, Moragas M, Berenguer J, Bernal-Sprekelsen M: Outcome of transoral laser microsurgery for T2–T3 tumors growing in the laryngeal anterior commissure. Head Neck. 2011, 33: 1252-1259. 10.1002/hed.21605.
Spector JG, Sessions DG, Lenox J, Simpson J: Management of T3N1 glottic carcinoma: therapeutic outcomes. Laryngoscope. 2006, 116: 106-110. 10.1097/01.mlg.0000184767.62682.3d.
Hinni ML, Ferlito A, Brandwein-Gensler MS, Takes RP, Silver CE, Westra WH, Seethala RR, Rodrigo JP, Corry J, Bradford CR, Hunt JL, Strojan P, Devaney KO, Gnepp DR, Hartl DM, Kowalski LP, Rinaldo A, Barnes L: Surgical margins in head and neck cancer: A contemporary review. Head Neck. 2012, doi:10.1002/hed.23110
Ansarin M, Santoro L, Cattaneo A, Massaro MA, Calabrese L, Giugliano G, Maffini F, Ostuni A, Chiesa F: Laser surgery for early glottic cancer: impact of margin status on local control and organ preservation. Arch Otolaryngol Head Neck Surg. 2009, 135: 385-390. 10.1001/archoto.2009.10.
Makki FM, Williams B, Rajaraman M, Hart RD, Trites J, Brown T, Taylor SM: Current practice patterns in the management of glottic cancer in Canada: results of a national survey. J Otolaryngol Head Neck Surg. 2011, 40: 205-210.
Nakayama M, Holsinger C, Okamoto M, Seino Y, Miyamoto S, Takeda M, Yokobori S, Masaki T, Hayashi S: Clinicopathological analyses of fifty supracricoid laryngectomized specimens: evidence base supporting minimal margins. ORL J Otorhinolaryngol Relat Spec. 2009, 71: 305-311. 10.1159/000261836.
Ossoff RH, Sisson GA, Shapshay SM: Endoscopic management of selected early vocal cord carcinoma. Ann Otol Rhinol Laryngol. 1985, 94: 560-564.
Meghana SM, Ahmedmujib BR: Surgical artefacts in oral biopsy specimens: Punch biopsy compared to conventional scalpel biopsy. J Oral Maxillofac Pathol. 2007, 11: 11-14. 10.4103/0973-029X.33957.
Yellowitz J, Horowitz AM, Goodman HS, Canto MT, Farooq NS: Knowledge, opinions and practices of general dentists regarding oral cancer: a pilot survey. J Am Dent Assoc. 1998, 129: 579-583. 10.14219/jada.archive.1998.0275.
Zegarelli DJ: Commn problems in biopsy procedure. J Oral Surg. 1978, 36: 644-647.
Lynch DP, Morris LF: The oral mucosal punch biopsy: Indications and technique. J Am Dent Assoc. 1990, 121: 145-149.
Seoane J, Varela-Centelles P, Ramirez JR, Romero MA, De La Cruz A: Artefacts produced by suture traction during incisional biopsy of oral lesions. Clin Otolaryngol Allied Sci. 2002, 27: 549-553. 10.1046/j.1365-2273.2002.00619.x.
Saunders WH, Wakely P: Atlas of head and neck pathology. 1998, Philadelphia US: Ohio State University, 271-295.
Seoane J, Varela-Centelles PI, Ramírez JR, Cameselle-Teijeiro J, Romero MA: Artefacts in oral incisional biopsies in general dental practice: a pathology audit. Oral Dis. 2004, 10: 113-117. 10.1111/j.1354-523X.2003.00983.x.
Kumar K, Shetty DC, Dua M: Biopsy and tissue processing artifacts in oral mucosal tissues. Int J Head Neck Surg. 2012, 3: 92-98.
Walsh JT, Flotte TJ, Anderson RR, Deutsch TF: Pulsed CO2 laser tissue ablation: effect of tissue type and pulse duration on thermal damage. Lasers Surg Med. 1988, 8: 108-118. 10.1002/lsm.1900080204.
Fortune DS, Huang S, Soto J, Pennington B, Ossoff RH, Reinisch L: Effect of pulse duration on wound healing using a C02 laser. Laryngoscope. 1998, 108: 843-848. 10.1097/00005537-199806000-00012.
Ossoff J, Coleman JR, Deriso W, Smith S, Ossoff RH, Reinisch L: Wound healing in canine oral mucosa with pulsed and continuous wave carbon dioxide laser incisions. Lasers Surg Med. 1997, 20: 23.
Rubinstein M, Armstrong WB: Transoral laser microsurgery for laryngeal cancer: a primer and review of laser dosimetry. Lasers Med Sci. 2011, 26: 113-124. 10.1007/s10103-010-0834-5.
Ryu SW, Lee SH, Yoon HJ: A comparative histological and immunohistochemical study of wound healing following incision with a scalpel, CO2 laser or Er, Cr:YSGG laser in the Guinea pig oral mucosa. Acta Odontol Scand. 2012, 70: 448-454. 10.3109/00016357.2011.635598.
Liboon J, Funkhouser W, Terris DJ: A comparison of mucosal incisions made by scalpel, CO2 laser, electrocautery, and constant-voltage electrocautery. Otolaryngol Head Neck Surg. 1997, 116: 379-385. 10.1016/S0194-5998(97)70277-8.
Sanders DL, Reinisch L: Wound healing and collagen thermal damage in 7.5-microsec pulsed CO(2) laser skin incisions. Lasers Surg Med. 2000, 26: 22-32. 10.1002/(SICI)1096-9101(2000)26:1<22::AID-LSM5>3.0.CO;2-R.
Howard J, Arango P, Ossoff J, Ossoff RH, Reinisch L: Healing of laser incisions in rat dermis: comparisons of the carbon dioxide laser under manual and computer control and the scalpel. Lasers Surg Med. 1997, 20: 90-96. 10.1002/(SICI)1096-9101(1997)20:1<90::AID-LSM14>3.0.CO;2-D.
Bryant GL, Davidson JM, Ossoff RH, Garrett CG, Reinisch L: Histologic study of oral mucosa wound healing: a comparison of a 6.0- to 6.8-mm pulsed laser and a carbon dioxide laser. Laryngoscope. 1998, 108: 13-17. 10.1097/00005537-199801000-00003.
Garrett CG, Reinisch L: New-generation pulsed carbon dioxide laser: comparative effects on vocal fold wound healing. Ann Otol Rhinol Laryngol. 2002, 111: 471-476.
Rogerson AR, Clark KF, Bandi SR, Bane B: Voice and healing after vocal fold epithelium removal by CO2 laser vs. microlaryngeal stripping. Otolaryngol Head Neck Surg. 1996, 115: 352-359. 10.1016/S0194-5998(96)70050-5.
Rohde M, Grøntved ÅM, Krogdahl A, Godballe C: Aggressive elimination of precancerous lesions of the vocal cords to avoid risk of cancer. Dan Med J. 2012, 59: A4399.
Gallo A, de Vincentiis M, Della Rocca C, Moi R, Simonelli M, Minni A, Shaha AR: Evolution of precancerous laryngeal lesions: a clinicopathologic study with long-term follow-up on 259 patients. Head Neck. 2001, 23: 42-47. 10.1002/1097-0347(200101)23:1<42::AID-HED7>3.0.CO;2-1.
Spielmann PM, Palmer T, McClymont L: 15-Year review of laryngeal and oral dysplasias and progression to invasive carcinoma. Eur Arch Otorhinolaryngol. 2010, 267: 423-427. 10.1007/s00405-009-1013-9.
Camacho Alonso F, López Jornet P, Jiménez Torres MJ, Orduña Domingo A: Analysis of the histopathological artefacts in punch biopsies of the normal oral mucosa. Med Oral Patol Oral Cir Bucal. 2008, 13: 636-639.
Lee HW, Ahn SJ, Lee MW, Choi JH, Moon KC, Koh JK: Pseudomelanoma following laser therapy. J Eur Acad Dermatol Venereol. 2006, 20: 342-344. 10.1111/j.1468-3083.2006.01391.x.
Seoane J, Caballero TG, Urizar JM, Almagro M, Mosquera AG, Varela-Centelles P: Pseudodysplastic epithelial artefacts associated with oral mucosa CO2 laser excision: an assessment of margin status. Int J Oral Maxillofac Surg. 2010, 39: 783-787. 10.1016/j.ijom.2010.04.046.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
FM: Ethics approval, patient enrollment, & manuscript. MR: Statistics and Data analysis. RH, SMT & JT: head & neck surgeons involved in patient selection and enrollment. TB: laryngologist involved in patient selection and enrollment. MB: pathologist. MH: involved in manuscript review and data analysis. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Makki, F.M., Rigby, M.H., Bullock, M. et al. CO2 laser versus cold steel margin analysis following endoscopic excision of glottic cancer. J of Otolaryngol - Head & Neck Surg 43, 6 (2014). https://doi.org/10.1186/1916-0216-43-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1916-0216-43-6