Abstract
Among Swedish families with an inherited predisposition for breast cancer, less than one third segregate mutations in genes known to be associated with an increased risk of breast cancer in combination with other types of tumours. In a search for new putative familial breast cancer syndromes we studied Swedish families undergoing genetic counselling during 1992-2000.
Four thousand families from counselling clinics in Sweden were eligible for study. Families with breast cancer only were excluded, as were families with mutations in genes already known to be associated with malignant diseases. We identified 803 families with two or more cases of breast cancer and at least one other type of cancer. The observed proportion of different types of non-breast cancer was compared with the percentage distribution of non-breast cancer tumours in Sweden in 1958 and 1999.
We found tumours in the colon, ovary, endometrium, pancreas and liver, as well as leukaemia in a significantly larger proportion of the study population than in the general population in both years. These tumours were also seen among families where several members had one additional tumour, suggesting that malignancies at these sites, in combination with breast tumours, could constitute genetic syndromes. Endometrial carcinoma has not previously been described in the context of breast cancer syndromes and the excess of malignancies at this site could not be explained by secondary tumours. Thus, we suggest that endometrial carcinoma and breast cancer constitute a new breast cancer syndrome. Further investigation is warranted to categorize phenotypes of both breast and endometrial tumours in this subgroup.
Similar content being viewed by others
Introduction
Breast cancer is by far the most frequently diagnosed malignant tumour in females: one Swedish woman in ten will be affected during her lifetime [1]. Most cases occur late in life and are sporadic. A Scandinavian twin study has revealed that hereditary factors are important in 27% of all breast cancers [2], and 5-10% of the cases appear to be the result of autosomal dominant genes [3]. Familial aggregations of breast cancer have been observed all over the world; in general, early onset and bilateral disease are two important features in these families [4].
Studies have revealed that autosomal dominant inherited mutations in certain genes are associated with an increased risk of breast cancer. Breast cancer in association with other tumours constitutes different syndromes in these families. A substantial risk of breast cancer as well as ovarian cancer is seen in women harbouring a mutation in BRCA1 or BRCA2 [5].
Although rare, other inherited syndromes associated with an increased risk of breast cancer and other tumours are known. An example is Li-Fraumeni syndrome, characterised by breast cancer occurring at an exceptionally young age in combination with brain tumour, adrenocortical carcinoma and soft-tissue sarcoma [6]. This syndrome has also been associated with an overrepresentation of tumours in the stomach, colon, rectum, pancreas and ovary, as well as malignant lymphoma, all at an extremely young age and along with the typical tumours constituting classical Li-Fraumeni syndrome [7]. However, mutations in the causative gene p53 are rarely seen in families where breast cancer cases predominate [8]. Some families with the Li-Fraumeni phenotype also bear mutations in the CHEK2 gene [9]. Studies of families with multiple cases of breast cancer have indicated that a certain mutation in the CHEK2 gene, 1100delC, is associated with an increased risk of both sporadic and familial breast cancer [10]. In Cowden's syndrome, females are afflicted with malignant tumours of the breast and the thyroid gland caused by germ line mutations in the PTEN gene [11]. PTEN mutations in familial breast cancer outside this syndrome are rare [12]. Germ line mutations in the tumour suppressor gene E-cadherin are associated with an increased risk of diffuse gastric cancer and to some extent also of lobular breast carcinoma but are not seen in familial breast cancer without diffuse gastric cancer [13, 14]. An increased familial risk of breast cancer and pancreatic cancer has been described in Swedish families segregating the CDKN2A/p16-mutation and that show multiple cases of malignant melanoma [15]. The role of ataxia-telangiectasia (AT) heterozygosity in breast cancer has been controversial. Heterozygotes have been found to be at increased risk, in particular at older age [16]. Occasional germ line mutations have also been reported in familial breast cancer [17]. Some recent studies have suggested an association with breast cancer to be restricted to certain variants of the ATM gene [18, 19], while in others no such risk could be demonstrated [20, 21].
In the counselling situation in Sweden mutation analysis of the BRCA1 and BRCA2 genes is usually offered to families fulfilling any of the following criteria: 1) at least three cases of breast cancer in first degree relatives, one of whom was under the age of 50 at the time of diagnosis, 2) two first degree relatives with breast cancer, one before the age of 40 years, or 3) one case of breast cancer before 35. Additional criteria are: 4) any combination of breast cancer and ovarian cancer in a family regardless of age, 5) one case of ovarian cancer before age 45. Screening methods use an exon-by-exon based strategy of both genes. Among Swedish families with a pedigree fulfilling these criteria less than one third segregate mutations in any of the two genes [22–24]. Families with a distribution of tumours typical for Li-Fraumeni syndrome are offered mutation analyses of p53 but only a handful of germ line p53 mutations have been found. Thus, there is reason to believe that other syndromes with an increased risk of breast cancer exist among the other two thirds of the breast cancer families. The aim of the present hypothesis-generating study was to search for putative breast cancer associated syndromes in families with two or more cases of breast malignancies.
Materials and methods
Four thousand Swedish families who underwent genetic counselling during the period January 1992 to January 2000 were eligible for recruitment. This group comprises all families in Sweden that had ever been subject to oncogenetic counselling in an oncogenetic clinic up to January 2000. The families were either self-referred or referred by their doctors to one of eight oncogenetic clinics in Sweden. Families known to be positive for mutations in any of the genes associated with breast or colon cancer were excluded, as were families with any of these two malignancies as the only observed malignancy in the family. In some families that fulfilled the criteria, mutation screening was not practicable, since there was no affected woman alive to give a blood sample.
We examined all pedigrees from the 4000 families and identified 803 families with two or more cases of breast cancer and at least one other type of cancer and with no exclusion criteria. These families were defined as "study families" (Fig. 1). Diagnoses from both maternal and paternal branches were included and every case of cancer in first- and second-degree relatives and in first cousins was recorded. Kinships were always related to the proband. Malignant tumours in relatives more distant than first cousins were included only if the diagnosis could be verified as below. More than one study family could originate from one pedigree, depending on which pedigree branch was chosen (Fig. 2A, B). In this way, one case of cancer could be included in two or, sometimes, in three study families but no case of malignancy was ever counted more than once as an observed case of that particular type of tumour.
Altogether, 803 study families originated out of 750 pedigrees. The vast majority of the diagnoses were histologically verified as shown by medical records or the Swedish cancer registry. A few of the cases originated from the beginning of the 20th century, before the cancer registry was established. These cases were mostly verified by checking the Swedish cause of death registry, to which doctors have been required to report all deaths since 1911.
In addition to serving as a means of verifying diagnoses, the Swedish cancer registry was used as a reference population in this study. The population-based registry, to which reporting is required by law, was established in 1958. All new cases of malignant primary tumours must be reported by both physician and pathologist. In 1958, Sweden had 7.5 million inhabitants of whom 19 324 were reported to the cancer registry. In 1999 the corresponding figures were 8.8 million and 45 180. In order to compare our data with official statistics of cancer incidence in Sweden, all different subtypes of leukaemia, all soft tissue and all central nervous system tumours were pooled in data from 1958 as well as from 1999. In official data from 1958 tumours of lip, mouth and tongue were presented together as were all lymphomas and myelomas.
The proportion of different cancers other than breast cancer in the study families was computed and 95% confidence intervals (CI) were calculated. When the observed numbers were less than 10, StatXact-4 (Cytel Inc., Cambridge, MA, USA) was used to calculate the exact confidence interval. If the 95% CI did not cover the proportion from 1958 (or 1999) a significant difference from that year could be demonstrated. The population data were obtained from official Swedish statistics from two separate years and comparisons were made using statistics from the first and last years for which Swedish cancer statistics were available. Only malignancies with a significant difference in proportions in comparison with the general population in both 1958 and 1999 were considered over-represented.
To make it possible to compare the frequency of non-breast cancers in our study families with data from Statistics Sweden, we corrected for the fact that 87% of the cancers reported in 1958 and 86% in 1999 were non-breast cancers:
The 95% CI for the proportion among study families does not cover the proportion of pancreatic cancer among non-breast cancers in Sweden in 1958; consequently the difference is considered significant for that year.
Date of diagnosis, sex and age at diagnosis were not recorded. As the excess of ovarian cancer in the study families could be due to "confounding by indication", corresponding proportions of all non-breast/ovarian tumours with 95% CI were also calculated. We explored the occurrence of families with one or several types of additional malignancies including multiple cases of each type and together with two or more breast cancer cases. These families are defined as "multiple-case families".
Results
In the 803 study families we found 2203 breast cancers, equivalent to 2.7 cases per family. Thirty-five different non-breast cancer diagnoses were observed, totalling 1 706 cases, corresponding to 2.12 cases per family.
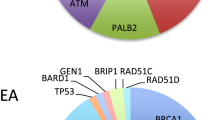
In the study families tumours in the colon, ovary, endometrium, pancreas and liver, as well as leukaemia, were statistically over-represented compared to the calculated proportion from the official statistics of the years 1958 and 1999 (Table 1). The data and method used for comparison are described under the methods section. Proportions of all non-breast/ovarian tumours were also calculated using the same method with the same five malignancies (ovarian tumours not included), as well as malignant connective tissue tumours and larynx, also having an observed proportion that was significantly higher than that in the general population in 1958 and 1999. All of the over-represented types of cancer, except for tumours in the larynx, were also present among the multiple case families (Fig. 3). All cancers of the urinary tract, except for tumours of the kidney, and all malignancies of the lymphoproliferative system, such as lymphomas and myelomas together, were present in a smaller proportion of the study families than in the reference population of the Swedish cancer registry in 1958 and 1999.
Discussion
Tumours in the ovary, endometrium, colon, pancreas and liver as well as leukaemia were all found in a larger proportion of the study population than in the reference population in 1958 and 1999 and were also seen among the multiple-case families. This suggests that malignancies at these sites, in combination with breast tumours, could constitute breast cancer syndromes.
However, there are several issues that need to be discussed. When recording the cancer history of the study families, we found that the vast majority of the diagnoses recorded by the counsellor could be verified through medical records. In our analysis we accepted both verified diagnoses (the vast majority) and unverified diagnoses, since in the counselling situation attempts were made to verify diagnoses crucial for delineating the hereditary pattern. Thus, for some malignancies, like lung cancer and head and neck tumours, diagnoses were not always verified. In contrast, counsellors generally made great efforts to verify gynaecological cancers in families with a putative breast/ovarian syndrome, where genetic testing is possible. By allowing also unverified diagnoses we obtained a more complete picture of the distribution of non-breast cancers in the families.
As many of the recorded diagnoses are dated several years back, and the incidence of some malignant disorders has changed over the past decades, it might be misleading to compare the distribution of non-breast cancers in the study families with the distribution of cancer in general in Sweden in the late 1990s. To overcome this problem we used official statistics from two separate years for comparison. The first and the last years for which official Swedish cancer statistics are available - 1958 and 1999 - were chosen to capture as many as possible of the changes in cancer incidence over the years. The official statistics used for comparison in our study did not take gender or age at diagnosis into account; nor do our data.
The use of expanded pedigrees of individuals from all branches can be questioned. It can result in an overestimation of the cancer incidence when more than one study family is registered from one pedigree. To overcome this problem, all counted families were studied but individual tumours were only included once as an observed case of that particular type of tumour. Thus, even though this might exaggerate the total number of non-breast cancer cases in the study families, it should not influence the distribution of the different kinds of tumours.
Since the statistics from 1958 report tumours of the lip, mouth and tongue all together, and the same for lymphomas and myelomas, the distribution of these disorders could not be compared individually with figures describing their distribution in the study families.
A substantial number of probands at the oncogenetic clinics in Sweden ask for genetic counselling because of several cases of colon cancer in close relatives. As breast cancer is a fairly common malignant disease, two or more cases could occur simply by chance in these families. This might explain a minor fraction of the observed excess of colon malignancies in the study families. The observed excess of ovarian cancer cases could be explained by undetected BRCA1 and BRCA2 mutations. However, the screening techniques in use today detect small single base-pair alterations, insertions and deletions as well as large rearrangements, making it unlikely that many of our breast-ovarian cancer families segregate undetected BRCA1/2 mutations. Even if the sensitivity of the molecular techniques is not 100 percent it cannot be excluded that a still unknown gene, associated with breast/ovarian cancer syndrome, could account for some of the observed cases. The excess of endometrial carcinoma could correspond to the previously described combination of papillary serous adenocarcinoma of endometrium and breast cancer [25] but probably only accounts for a minor part of the observed cases. In hereditary non-polyposis colorectal cancer (HNPCC), tumours in the colon are frequently seen in combination with other malignancies, e.g. endometrial cancer. However, among cases of endometrial cancer in our study families, only four out of 124 cases occurred in combination with colon cancer, thus suggesting that the observed excess of endometrial malignancy would not be a result of HNPCC in our families. Further investigation is warranted to categorize phenotypes of both breast and endometrial tumours in this subgroup. The excess of pancreatic tumours could in part be due to CDKN2A/p16-mutation-positive Swedish families. As discussed above, some of the diagnoses were never verified but simply recorded as the type of malignancy known to the proband. Secondary tumours or metastases from different cancer sites are commonly seen in lung, liver and bone and could probably explain some of the tumours observed at these sites. Nevertheless, only malignancy in the liver was seen more often in the study families than in the reference population, indicating that diagnoses at these three sites are probably not exaggerated. Leukaemia is seen in Li-Fraumeni syndrome and study families with mutations in TP53, CHEK2 or other genes in the same pathway could explain the excess of this type of malignancy.
The findings of the present study are in congruence with the findings of Bermejo and Hemminki [26] showing an association between breast cancer and ovarian, colon, endometrial and pancreatic cancer in study populations from Sweden.
We suggest that breast cancer in combination with tumours in the colon, ovary, endometrium or pancreas, or leukaemia, could constitute genetic breast cancer syndromes. Earlier described syndromes could, at least in part, explain the higher frequency of tumours in ovary and pancreas and leukaemia in study families. The excess of cancer in ovary and colon could partly be a result of confounding by indication. Neither can we rule out the possibility that the excess of malignancies in the liver is a result of secondary tumours in the study families. However, endometrial carcinoma has not been described previously in that context, suggesting that endometrial carcinoma and breast cancer could constitute a new breast cancer syndrome. The result can be used to define subgroups of families suitable for studies aiming to identify additional genes predisposing to breast and endometrial cancer.
References
Cancer incidence in Sweden 1999: Swedish National Board of Health and Welfare.
Lichtenstein P, Holm NV, Verkasalo PK, Iliadou A, Koskenvuo M, Pukkala E, Skytthe A, Hemminki K: Environmental and heritable factors in the causation of cancer - analyses of cohorts of twins from Sweden, Denmark, and Finland. N Engl J Med 2000, 343: 78–85. 10.1056/NEJM200007133430201
Claus EB, Risch N, Thompson WD: Genetic analysis of breast cancer in the cancer and steroid hormone study. Am J Hum Genet 1991, 48: 232–242.
Claus EB, Risch NJ, Thompson WD: Age at onset as an indicator of familialrisk of breast cancer. Am J Epidemiol 1990, 131: 961–972.
King MC, Go RC, Lynch HT Elston RC, Terasaki PI, Petrakis NL, Rodgers GC, Lattanzio D, Bailey-Wilson J: Genetic epidemiology of breast cancer and associated cancers in high-risk families. II. Linkage analysis. J Natl Cancer Inst 1983, 71: 463–467.
Li FP, Fraumeni JF Jr: Soft-tissue sarcomas, breast cancer, and other neoplasms. A familial syndrome? Ann Intern Med 1969, 71: 747–752.
Nichols KE, Malkin D, Garber JE, Fraumeni JF Jr, Li FP: Germ-line p53 mutations predispose to a wide spectrum of early-onset cancers. Cancer Epidemiol Biomarker Prev 2001, 10: 83–87.
Zelada-Hedman M, Borresen-Dale AL, Claro A, Chen J, Skoog L, Lindblom A: Screening for TP53 mutations in patients and tumours from 109 Swedish breast cancer families. Br J Cancer 1997, 75: 1201–1204.
Bell DW, Varley JM, Szydlo TE, Kang DH, Wahrer DC, Shannon KE, Lubratovich M, Verselis SJ, Isselbacher KJ, Fraumeni JF, Birch JM, Li FP, Garber JE, Haber DA: Heterozygous germ line hCHK2 mutations in Li-Fraumeni syndrome. Science 1999, 286: 2528–2531. 10.1126/science.286.5449.2528
CHEK2 Breast Cancer Case-Control Consortium: CHEK2*1100delC and susceptibility to breast cancer: a collaborative analysis involving 10,860 breast cancer cases and 9,065 controls from 10 studies. Am J Hum Genet 2004, 74: 1175–1182. 10.1086/421251
Liaw D, Marsh DJ, Li J, Dahia PL, Wang SI, Zheng Z, Bose S, Call KM, Tsou HC, Peacocke M, Eng C, Parsons R: Germline mutations of the PTEN gene in Cowden disease, an inherited breast and thyroid cancer syndrome. Nat Genet 1997, 16: 64–67. 10.1038/ng0597-64
Chen J, Lindblom P, Lindblom A: A study of the PTEN/MMAC1 gene in 136 breast cancer families. Hum Genet 1998, 102: 124–125.
Keller G, Vogelsang H, Becker I, Hutter J, Ott K, Candidus S, Grundei T, Becker KF, Mueller J, Siewert JR, Hofler H: Diffuse type gastric and lobular breast carcinoma in a familial gastric cancer patient with an E-cadherin germline mutation. Am J Pathol 1999, 155: 337–342.
Salahshor S, Haixin L, Huo H, Kristensen VN, Loman N, Sjoberg-Margolin S, Borg A, Borresen-Dale AL, Vorechovsky I, Lindblom A: Low frequency of E-cadherin alterations in familial breast cancer. Breast Cancer Res 2001, 3: 199–207. 10.1186/bcr295
Borg A, Sandberg T, Nilsson K, Johannsson O, Klinker M, Masback A, Westerdahl J, Olsson H, Ingvar C: High frequency of multiple melanomas and breast and pancreas carcinomas in CDKN2A mutation-positive melanoma families. J Natl Cancer Inst 2000, 92: 1260–1266. 10.1093/jnci/92.15.1260
Athma P, Rappaport R, Swift M: Molecular genotyping shows that ataxia-telangiectasia heterozygotes are predisposed to breast cancer. Cancer Genet Cytogenet 1996, 92: 130–134. 10.1016/S0165-4608(96)00328-7
Chen J, Birkholtz GG, Lindblom P, Rubio C, Lindblom A: The role of ataxia-telangiectasia heterozygotes in familial breast cancer. Cancer Res 1998, 58: 1376–1379.
Chenevix-Trench G, Spurdle AB, Gatei M, Kelly H, Marsh A, Chen X, Donn K, Cummings M, Nyholt D, Jenkins MA, Scott C, Pupo GM, Dork T, Bendix R, Kirk J, Tucker K, McCredie MR, Hopper JL, Sambrook J, Mann GJ, Khanna KK: Dominant negative ATM mutations in breast cancer families. J Natl Cancer Inst 2002, 94: 205–215.
Buchholz TA, Weil MM, Ashorn CL, Strom EA, Sigurdson A, Bondy M, Chakraborty R, Cox JD, McNeese MD, Story MD: A Ser49Cys variant in the ataxia telangiectasia, mutated, gene that is more common in patients with breast carcinoma compared with population controls. Cancer 2004, 100: 1345–1351. 10.1002/cncr.20133
Szabo CI, Schutte M, Broeks A, Houwing-Duistermaat JJ, Thorstenson YR, Durocher F, Oldenburg RA, Wasielewski M, Odefrey F, Thompson D, Floore AN, Kraan J, Klijn JG, Ouweland AM, Wagner TM, Devilee P, Simard J, van't Veer LJ, Goldgar DE, Meijers-Heijboer H: Are ATM mutations 7271T->G and IVS10–6T->G really high-risk breast cancer-susceptibility alleles. Cancer Res 2004, 64: 840–843. 10.1158/0008-5472.CAN-03-2678
Bernstein JL, Bernstein L, Thompson WD, Lynch CF, Malone KE, Teitelbaum SL, Olsen JH, Anton-Culver H, Boice JD, Rosenstein BS, Borresen-Dale AL, Gatti RA, Concannon P, Haile RW: WECARE Study Collaborative Group. ATM variants 7271T>G and IVS10–6T>G among women with unilateral and bilateral breast cancer. Br J Cancer 2003, 89: 1513–1516. 10.1038/sj.bjc.6601289
Henriksson K, Olsson H, Kristoffersson U: The need for oncogenetic counselling. Ten years' experience of a regional oncogenetic clinic. Acta Oncol 2004, 43: 637–649. 10.1080/02841860410018520
Einbeigi Z, Bergman A, Kindblom LG, Martinsson T, Meis-Kindblom JM, Nordling M, Suurkula M, Wahlstrom J, Wallgren A, Karlsson P: A founder mutation of the BRCA1 gene in Western Sweden associated with a high incidence of breast and ovarian cancer. Eur J Cancer 2001, 37: 1904–1909. 10.1016/S0959-8049(01)00223-4
Arver B, Claro A, Langerod A, Borresen-Dale AL, Lindblom A: BRCA1 screening in patients with a family history of breast or ovarian cancer. Genet Test 1999, 3: 223–226.
Goshen R, Chu W, Elit L, Pal T, Hakimi J, Ackerman I, Fyles A, Mitchell M, Narod SA: Is uterine papillary serous adenocarcinoma a manifestation of the hereditary breast-ovarian cancer syndrome? Gynecol Oncol 2000, 79: 477–481. 10.1006/gyno.2000.6003
Lorenzo Bermejo J, Hemminki K: Familial association of histology specific breast cancers with cancers at other sites. Int J Cancer 2004, 109: 430–435. 10.1002/ijc.11713
Acknowledgements
The authors are grateful to Monica Emanuelsson, Elisabeth Stenman and Eva Holmberg for valuable assistance and to the Swedish Cancer Society and the Swedish Society of Medicine for funding.
The South Swedish Oncogenetic Study Group consists of Karin Henriksson, Niklas Loman, Ulf Kristoffersson, Håkan Olsson and Oscar Jóhansson.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
von Wachenfeldt, A., Lindblom, A., The South Swedish Oncogenetic Study Group. et al. A hypothesis-generating search for new genetic breast cancer syndromes - a national study in 803 Swedish families. Hered Cancer Clin Pract 5, 17 (2007). https://doi.org/10.1186/1897-4287-5-1-17
Published:
DOI: https://doi.org/10.1186/1897-4287-5-1-17