Abstract
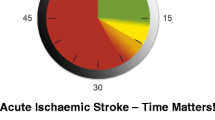
The role for prehospital thrombolysis for ST-elevation acute myocardial infarction and time-critical stroke transfers in the northern Norway aeromedical retrieval system as well as the aero-evacuation impact of increased Arctic expedition tourism could benefit from further discussion by Norum and Elsbak. Close ECG surveillance for ST elevation and retrieval thrombolysis en route to the accepting hospital could be of benefit for acute coronary syndrome patients in northern Norway who require prolonged aeromedical transfer. For patients who remain within a reasonable time frame for stroke thrombolysis (up to 4.5 h after symptom onset), expedited transfer for neuroimaging to determine eligibility is recommended.
Similar content being viewed by others
Letter to the Editors
Norum and Elsbak describe the clinical and transfer characteristics of fixed and rotary wing aeromedical retrievals carried out in northern Norway for the 10 years 1999-2009 [1]. Acute cardiovascular diagnoses were encountered in 76/345 (22%) of the transported cohort [1, 2], although it is not stated which, if any, of these patients suffered high-risk acute coronary syndromes (ACS) and/or ST elevation acute myocardial infarction (STEMI). With one in five of the transported cohort potentially having a STEMI or high-risk ACS, a lengthy 3 h 33 min one-way transfer time [1] and attendant delays to accessing primary percutaneous reperfusion, Norum and Elsbak's study could have discussed the role of early recognition of ST elevation and prehospital thrombolysis. Prehospital ECG recognition of STEMI is reliable [3], and prehospital thrombolysis is safe [4] and acutely as clinically beneficial as primary angioplasty if transfer times are anticipated to exceed 120 min from onset of chest pain [5–7], a situation that applies to Norum and Elsbak's study cohort. Furthermore, in high-risk ACS, close ECG surveillance for attainment of lysis criteria followed by timely prehospital thrombolysis could mitigate further ST elevation (and the extent of myocardial injury) during transport [8].
Despite the apparent absence of neurological/stroke patients in their 10-year retrieval registry, Norum and Elsbak's [1] emphasis on urgent aeromedical transfer to identify stroke patients suitable for thrombolysis is to be applauded. Stroke lysis with intravenous alteplase remains beneficial when administered at up to 4.5 h after symptom onset [9, 10], a time range that remains relevant within the approximately 3.5 h mean transfer time encountered in the northern Norwegian aeromedical system. That rapidly aging adult populations in advanced economies will give rise to increased stroke burden is borne out by the transport of 69 stroke patients among 504 patients (14%) recently retrieved by a single agency German aeromedical service [11].
Norum and Elsbak [1] speculate that increasing expedition ship tourist traffic to Arctic Norway could lead to an increased need for aeromedical evacuation. However, most expedition ships operating in the Arctic are currently physician-staffed, with non-life or limb-threatening respiratory, gastrointestinal, dermatological, musculoskeletal complaints as well as minor trauma being the most frequently encountered health complaints [12]. Cardiovascular and neurological events, emergency evacuation, need for hospitalization as well as unexpected deaths are rarely encountered despite travelers being older, suggesting effective pre-trip medical screening [12]. At this stage it remains uncertain whether more Arctic tourism will necessarily increase aeromedical workload; this has been my experience as ship's physician in Svalbard in July and August 2009, when there was only one case of shipboard IV rehydration required for non-specific enteritis.
Abbreviations
- ACS:
-
acute coronary syndromes
- STEMI:
-
ST elevation acute myocardial infarction.
References
Norum J, Elsbak TM: Air ambulance services in the Arctic: a Norwegian study. Int J Emerg Med 2011, 4: 1. [http://www.intjem.com/content/4/1/1] 10.1186/1865-1380-4-1
Norum J: Cardiovascular disease (CVD) in the Norwegian Arctic: Air ambulance operations 1999–2009 and future challenges in the region. Int Marit Health 2010, 62: 117–22.
Barbagelata A, Perna ER, Clemmensen P, Uretsky BF, Canella JP, Califf RM, Granger CB, Adams GL, Merla R, Birnbaum Y: Time to reperfusion in acute myocardial infarction. It is time to reduce it! J Electrocardiol 2007, 40: 257–64. 10.1016/j.jelectrocard.2007.01.007
Welsh RC, Travers A, Senaratne M, Williams R, Armstrong PW: Feasibility and applicability of paramedic-based prehospital thrombolysis in a large North American center. Am Heart J 2006, 152: 1007–14. 10.1016/j.ahj.2006.06.022
Steg PG, Bonnefoy E, Chabaud S, Lapostolle F, Dubien BY, Cristofini P, Leizorovisz A, Touboul P, for the Comparison of Angioplasty and Prehospital Thrombolysis in acute Myocardial infarction (CAPTIM) Investigators: Impact of time to treatment on mortality after prehospital fibrinolysis or primary angioplasty: data from the CAPTIM randomized clinical trial. Circulation 2003, 108: 2851–6. 10.1161/01.CIR.0000103122.10021.F2
Danchin N, Blanchard D, Steg PG, Sauval P, Hanania G, Goldstein P, Cambou JP, Gueret P, Vaur L, Boutalbi Y, Genes N, Lablanche JM, USIC 2000 Investigators: Impact of prehospital thrombolysis for acute myocardial infarction on 1-year outcome: results from the French Nationwide USIC 2000 Registry. Circulation 2004, 110: 1909–15. 10.1161/01.CIR.0000143144.82338.36
Morrison LJ, Verbeek PR, McDonald AC, Sawadsky BV, Cook DJ: Mortality and prehospital thrombolysis for acute myocardial infarction: A meta-analysis. JAMA 2000, 283: 2686–92. 10.1001/jama.283.20.2686
Lamfers EJ, Hooghoudt TE, Hertzberger DP, Schut A, Stolwijk PW, Verheugt FW: Abortion of acute ST segment elevation myocardial infarction after reperfusion: incidence, patients' characteristics, and prognosis. Heart 2003, 89: 496–501. 10.1136/heart.89.5.496
Lees KR, Bluhmki E, von Kummer R, Brott TG, Toni D, Grotta JC, Albers GW, Kaste M, Marler JR, Hamilton SA, Tilley BC, Davis SM, Donnan GA, Hacke W, for the ECASS EPITHET rt-PA Group Investigators: Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet 2010, 375: 1695–1703. 10.1016/S0140-6736(10)60491-6
Hacke W, Kaste M, Bluhmki E, Brozman M, Davalos A, Guidetti D, Larrue V, Lees KR, Medeghri Z, Machnig T, Schneider D, von Kummer R, Wahlgren N, Toni D, for the European Cooperative Acute Stroke Study (ECASS) Investigators: Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. New Engl J Med 2008, 359: 1317–29. 10.1056/NEJMoa0804656
Sand M, Bollenbach M, Sand D, Lotz H, Thrandorf C, Cirkel C, Altmeyer P, Bechara FG: Epidemiology of aeromedical evacuation: An analysis of 504 cases. J Travel Med 2010, 17: 405–9. 10.1111/j.1708-8305.2010.00454.x
Shaw MTM, Leggat PA: Illness and injury to travellers on a premium expedition to Iceland. Travel Med Infectious Disease 2008, 6: 148–51. 10.1016/j.tmaid.2008.02.003
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
JT declares that he fulfils all three criteria for authorship: (1) contribution to design, (2) involved in drafting and critically revising manuscript, and (3) approved the final version of manuscript for publication, if accepted.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Ting, J.Y. Letter to the editors: the potential role for prehospital thrombolysis and time-critical stroke transfers in the northern Norway aeromedical retrieval system; In response to: Norum J, Elsbak TM: Air ambulance services in the Arctic: a Norwegian study. Int J Emerg Med 2011, 4:1. Int J Emerg Med 4, 45 (2011). https://doi.org/10.1186/1865-1380-4-45
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1865-1380-4-45