Abstract
Background
Substantial heterogeneity in HIV prevalence has been observed within sub-Saharan Africa. It is not clear which factors can explain these differences. Our aim was to identify risk factors that could explain the large differences in HIV-1 prevalence among pregnant women in Harare, Zimbabwe, and Moshi, Tanzania.
Methods
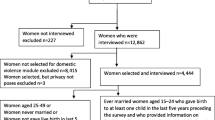
Cross-sectional data from a two-centre study that enrolled pregnant women in Harare (N = 691) and Moshi (N = 2654) was used. Consenting women were interviewed about their socio-demographic background and sexual behaviour, and tested for presence of sexually transmitted infections and reproductive tract infections. Prevalence distribution of risk factors for HIV acquisition and spread were compared between the two areas.
Results
The prevalence of HIV-1 among pregnant women was 26% in Zimbabwe and 7% in Tanzania. The HIV prevalence in both countries rises constantly with age up to the 25-30 year age group. After that, it continues to rise among Zimbabwean women, while it drops for Tanzanian women. Risky sexual behaviour was more prominent among Tanzanians than Zimbabweans. Mobility and such infections as HSV-2, trichomoniasis and bacterial vaginosis were more prevalent among Zimbabweans than Tanzanians. Reported male partner circumcision rates between the two countries were widely different, but the effect of male circumcision on HIV prevalence was not apparent within the populations.
Conclusions
The higher HIV-1 prevalence among pregnant women in Zimbabwe compared with Tanzania cannot be explained by differences in risky sexual behaviour: all risk factors tested for in our study were higher for Tanzania than Zimbabwe. Non-sexual transmission of HIV might have played an important role in variation of HIV prevalence. Male circumcision rates and mobility could contribute to the rate and extent of spread of HIV in the two countries.
Similar content being viewed by others
Background
There is substantial heterogeneity in HIV-1 prevalence within sub-Saharan Africa, a region that contains more than a third of the world's HIV-1 infections [1]. Sub-Saharan Africa's epidemics vary significantly from country to country in both scale and scope. Adult national HIV prevalence is less than 2% in countries of west and central Africa, and in 2007, it exceeded 15% in southern African countries [2].
Zimbabwe and Tanzania are examples of sub-Saharan countries that show large variations in HIV prevalence. Zimbabwe is severely affected by the HIV and AIDS epidemic. The country is experiencing a decline in HIV prevalence, but the figures are still very high. Among pregnant women (15-49 years), HIV prevalence declined from 32% in 2000 to 26% in 2002 and 18% in 2006 [3]. In the general population, HIV prevalence in Zimbabwe was estimated to be 27% in 2001, 19% in 2005, 16% in 2007 [3] and 14% in 2009 [4]. The prevalence of the infection in Tanzania is relatively low when compared with that of Zimbabwe, and was estimated to be 12% in 1999 and 7% in 2003/04 [5]. The HIV prevalence rate among Tanzanian antenatal clinic attendees in 2005/06 was 8%, and in 2008, it was estimated to be 6% [6].
A lot of resources have been invested to identify plausible risk factors of HIV that may explain why certain areas experience very high HIV-1 prevalences [7–9]. A number of biologic, behavioural and demographic factors have been suggested as influences on the large differences in HIV prevalence in sub-Saharan Africa. These include patterns of sexual networking, other sexually transmitted infections (STIs), reproductive tract infections (RTIs), time of introduction of the virus into the general population, migration, mobility, individual differences in susceptibility to HIV, virus subtypes and male circumcision rates [8, 10–12]. However, to date, there are still questions and not answers about what might be fuelling the epidemic in some countries and not in others. Comparisons of factors that determine the rate of spread of HIV in different regions is hampered by lack of comparable data [7].
A clear understanding and explanation of the striking HIV-1 differences may aid in identification of effective intervention strategies. A previous study of about 800 women in Zimbabwe and Tanzania found significant differences in HIV prevalence and called for more research to find factors that accelerate the rate of HIV acquisition or contribute to the difference in prevalence patterns [9].
This paper makes use of data from a large two-centre study done in Harare, Zimbabwe, and Moshi, Tanzania. The data were collected using the same protocol by members of the study group called Better Health for the African Mother and Child. We present here a comparison of the distribution of risk factors of HIV acquisition between the two countries. The objectives of this study are to compare underlying socio-demographic characteristics, sexual behaviour and other STIs and/or RTIs among pregnant women in Zimbabwe and Tanzania, and come up with possible explanations for the contrasting HIV-1 prevalence.
Methods
Study area and population
Methodology of the two centre study has been described in detail elsewhere [13, 14]. Data from cross-sectional studies of pregnant women enrolled consecutively at 36 weeks of gestation between 2002 and 2004 were used; these women were enrolled at two antenatal clinics in peri-urban Moshi in Tanzania, where there is a relatively low HIV prevalence, and three antenatal clinics in the peri-urban parts of Harare in Zimbabwe, where there is a high HIV prevalence. The same protocol was used in both centres. A questionnaire was administered by interviewers to solicit information on socio-demographic background, sexual behaviour, and current and past medical history. A doctor or a midwife carried out an overall physical and gynecological examination of the women. The women were tested for HIV-1, syphilis, HSV2, Trichomonas vaginalis, bacterial vaginosis and candidiasis.
Statistical analysis
Data were entered and analyzed using STATA Version 10 from StataCorp, Texas, USA. Distribution of risk factors for HIV infection between the two countries were compared using Student's t test for continuous variables and Pearson-chi square test for categorical variables. Unadjusted odds ratios and their 95% confidence intervals were presented for the various risk factors of HIV seropositivity for each country. Promising factors, i.e., those with a p value of less than 0.25 in univariate analysis, were investigated in multivariate analysis. Factors with a p < 0.10 were maintained in the final multivariate model, using a stepwise backward likelihood ratio procedure.
Ethical approval
The studies were approved by the Medical Research Councils of the respective countries, as well as the Norwegian Ethical Committee. Every woman who consented to taking part in the study was given a numeric identifier, which was used throughout the study on all documentation to maintain patient confidentiality. The women gave written informed consent to take part in the study.
Results
In total, 177 (25.6%) of the 691 pregnant women in Harare, Zimbabwe and 184 (6.9%) of the 2654 pregnant women in Moshi, Tanzania were HIV-1 positive. Figure 1 compares the age-specific HIV prevalence for the two countries. HIV-1 prevalence rises with age for the two countries up to the age group of 25-29 years. Thereafter, the prevalence of HIV in Zimbabwe continues to rise while that for Tanzania drops slightly for women who are older than 30 years.
Table 1 shows a comparison of the distribution of key risk factors between the two countries. Rates of risky sexual behaviour and alcohol consumption were consistently higher in Tanzania than in Zimbabwe. Sexually transmitted infections and reproductive tract infections are more common in Zimbabwe than in Tanzania. About 92% of the male partners of the Zimbabwean women are not circumcised, while circumcision is common (98%) in Tanzania in this study. Mobility is more common in Zimbabwe (7.7% for women and 41% for their partners) than in Tanzania (1.5% for women and 26% for their partners). A history of schistosomiasis was more often reported by the women in Zimbabwe than those in Tanzania (18% vs. 4%)
Table 2 shows the risk of being HIV positive within populations, separately for data from Zimbabwe and Tanzania respectively. In both countries, several risk factors for HIV positivity were identified in the univariate analysis. In multivariate analysis for the separate countries, age, higher number of lifetime sexual partners, HSV-2 infection, bacterial vaginosis and having a genital ulcer were consistently and independently associated with HIV-1 positivity.
Independent risk factors for HIV that were identified in Tanzania only were early age of sexual debut, being in a polygamous marriage, having children with different men, syphilis infection and having a partner who travels. These factors did not reach statistical significance in multivariate analysis in Zimbabwe, but were significant risk factors in univariate analysis, except for early age of sexual debut and having a partner who travels frequently. Having genital warts was independently associated with HIV infection in Zimbabwe, but this association was shown only in univariate analysis for Tanzania. Having a partner who is circumcised showed a tendency towards protection from HIV infection in Tanzania, but this was not statistically significant, while in Zimbabwe this factor showed the reverse association in univariate analysis and was also not significant in the multivariate analysis.
Discussion
We saw significant differences in the HIV prevalence for women attending antenatal clinics in Harare, Zimbabwe (25.6%) and in Moshi, Tanzania (6.9%), consistent with earlier reports [9]. The HIV prevalence for both countries rises constantly with age, but while it continues to rise among Zimbabwean women older than 30 years, the graph for Tanzanian women tails off. Mobility and biological risk factors for HIV, such as STIs and RTIs, notably HSV-2, trichomoniasis and bacterial vaginosis, were more prominent among Zimbabweans than Tanzanians. Risky sexual behaviour and male circumcision were more prominent among Tanzanians than Zimbabweans. In both countries, age, higher number of lifetime sexual partners, HSV-2 and bacterial vaginosis infections and having a genital ulcer were consistently and independently associated with HIV-1 positivity.
An unexpected phenomenon was seen in the sexual behaviour data: women in Tanzania reported more risky sexual behaviour than women in Zimbabwe, which is opposite to what is reflected in the HIV prevalence. Prevalence of risky sexual behaviour characteristics, such as having had a casual sexual partner in the previous 12 months, having had more than one lifetime sexual partner, early sexual debut, being in a polygamous relationship and having siblings by different fathers, were all higher for Tanzania. Alcohol consumption, which increases the tendency to engage in risky sexual behaviour [15], was also more common in Tanzania than in Zimbabwe. Clearly, sexual behaviour only cannot explain the observed differences in HIV prevalence between the two countries. How then can we explain this paradox?
The data collected from 2002 to 2004 in Moshi and Harare are cross-sectional and thus describe the situation close to the time of data collection, whereas the HIV prevalence data are the result of exposure to risk factors over periods of a decade or more. During this time, the prevalence of some of the key risky sexual behaviours is likely to be reduced, particularly where epidemics are severe [8]. It is possible that at the time of data collection, sexual risk behaviour for the women in Zimbabwe was decreasing in response to the alarming prevalence that had caused so much morbidity and mortality.
A longitudinal study conducted in the Manicaland province, Zimbabwe, has shown an improvement in sexual risk behaviour, e.g., men reporting fewer casual sexual partners than before [16]. In some parts of Tanzania, meanwhile, studies have shown that sexual risk behaviour is not decreasing because people see themselves as not being at risk of HIV infection [17]. However, the results of 1999 and 2005 demographic and health surveys done in the two countries have consistently shown that risky sexual behaviour is more prominent in Tanzania than in Zimbabwe. This is in terms of having: extramarital sexual partners; higher risk sexual intercourse; higher percentages of both men and women not using condoms; and higher percentages of men who reported visiting a commercial sex worker [18–21].
Lower risk sexual behaviour in Zimbabwe than in Tanzania could also be a result of under-reporting of socially unacceptable sexual behaviour by Zimbabwean women. Differences in social desirability bias could be a major contributing factor to the quality of sexual behaviour data [22]. Discrepancy in risky sexual behaviour and HIV prevalence were, however, reported in other studies of heterogeneity in HIV prevalence in African countries in which data collection methods were highly standardized and included triangulation [23].
From the "Four Cities Study", behavioural factors found to be more common in the two high HIV prevalence cities were young age at first sexual intercourse (women), young age at first marriage and large age differences between spouses. However, high rate of partner change, sex with sex workers, concurrent partnerships, and larger age difference between non-spousal partners were not more common in the two high HIV prevalence cities [23].
Apart from age mixing i.e sexual partners with large age differences, a study by Chapman et al [22], which used adolescent data from Zimbabwe, South Africa and Tanzania, found that "behaviours assumed a priori to be higher risk were not found to be more common in populations with higher HIV prevalence. In some cases, risk behaviours were much more prevalent in lower HIV prevalence studies. For example, the lowest levels of having had sex, oldest age of debut and the lowest proportion of multiple partners were reported in Zimbabwe, although that country had the highest HIV prevalence" [22].
Prevalence of HSV-2 and trichomoniasis was moderately higher in Zimbabwe than in Tanzania, but HIV prevalence in Zimbabwe was almost four times higher than that in Tanzania. With regards to the interaction between STIs and HIV infection, there is convincing evidence that STIs substantially enhance the vulnerability of non-HIV-infected individuals and the infectiousness of HIV-infected individuals [24, 25]. The prevalence of women with genital warts and genital ulcers was also higher in Zimbabwe than in Tanzania. It has been shown in several studies that the presence of sores on the genital tract facilitates entry of HIV [26, 27].
However, the causes of the higher prevalences of STIs and genital symptoms in Zimbabwe, given the observed much lower degree of risk behaviour compared with women in Tanzania, remains questionable. In 1999, the prevalence of STIs among women in Moshi and Harare were reported to be similar, except for large HIV prevalence differences, again showing higher prevalence in Harare [9]. This suggests that the higher STI prevalences in Zimbabwe compared with Tanzania during the study period, 2002 to 2004, were caused by HIV prevalence differences that existed over time.
Male circumcision among regular or current sexual partners was reported by almost 98% of the women in Tanzania and by only about 8% of the Zimbabwean women. Three randomized controlled trials, in Uganda, Kenya and South Africa, have shown that male circumcision is associated with a decreased risk of acquisition of HIV infection by men [28–30]. Reviews by van Howe [31] and Weiss et al [32] show that male circumcision might be protective against other STIs as well.
In the Ugandan randomized controlled trial, the prevalence of self-reported symptoms of STIs was lower in the circumcised arm than in the control arm. Obviously, women in areas where male circumcision is common get an indirect advantage due to the protective effect for their partners and the corresponding lower HIV prevalence in the population. Even though the rates of circumcision match the HIV prevalences in our study, the protective effect of male circumcision is not visible in the data within each country. Data from Tanzania show an insignificant protective effect, which might be due to the small number of men who are not circumcised. In Zimbabwe, those who are circumcised might possess other risky characteristics, possibly cultural, which render the protective effect of male circumcision insignificant.
Some studies point to the role of mobility and schistosomiasis infection rates in HIV acquisition in sub-Saharan Africa [12, 33, 34]. In our study, mobility was more common among Zimbabwean women and their partners than among those in Tanzania. However, the individual-level analysis did not show any association of mobility and HIV infection, except for male partners of Tanzanian women. With regard to schistosomiasis infection, our study results show marked differences in the prevalence between the two countries, but this infection was not at all associated with HIV seropositivity within both countries.
Another possible explanation for the contrasting HIV epidemics could be the role played by non-sexual transmission of HIV that might have occurred more in Zimbabwe in the early years of the epidemic. Figure 1 shows that HIV prevalence in our results continues to increase for the Zimbabwean women who are 30 years and older, while the rate for women in Tanzania stabilizes or even decreases with age. These women grew up in the 1980 s, when a number of studies reported HIV-positive children with HIV-negative mothers [35–39].
Some studies challenge the conventional hypothesis that sexual transmission is responsible for more than 90% of adult HIV infections in Africa [40]. A study in Zimbabwe in the 1990 s found a 2.1% HIV prevalence among 933 women with no reported sexual experience [41]. If adults and adolescents with no sexual exposures are found to be HIV positive, this suggests that a proportion of the HIV in those who are sexually exposed also comes from non-sexual transmission [40].
It is, however, important to highlight the possible weakness of sexual behaviour surveys in failing to detect true differences in risk. Another vital point is that some variables may not be fully investigated. For example, in this study the phrase, "ever used condom", is used rather than the more useful, "condom use at last sexual encounter". Further, the data collected age of sexual debut in categories, not the actual age of debut, making it difficult to estimate the median value. The role of other factors, such as age mixing and concurrency in driving the HIV prevalence in different ways, should also be investigated.
Conclusions
From our data and available information, we conclude that differences in sexual behaviour alone cannot explain the much higher HIV prevalence in Harare, Zimbabwe, than in Moshi, Tanzania. The large HIV prevalence differences may be a result of the fact that non-sexual transmission of HIV occurred at a relative larger scale in Zimbabwe in the early years of the epidemic. Male circumcision might be responsible for the low prevalence of STIs and HIV in Tanzania relative to Zimbabwe, but we could not confirm the role of male circumcision within the populations. More comparable sexual behaviour surveys that are capable of investigating risk factors fully and correctly in different countries are needed.
References
UNAIDS: 2008 Report on the global AIDS epidemic. UNAIDS; 2008.
UNAIDS: 2008 Status of the Global HIV Epidemic: sub-Saharan Africa. UNAIDS; 2008.
United Nations General Assembly (UNGASS): [http://data.unaids.org/pub/Report/2008/zimbabwe_2008_country_progress_report_en.pdf] Zimbabwe Report for HIV and AIDS. January 2006-December 2007. Accessed on 21 October 2010
ANC HIV estimates technical working group, Ministry of Health and Child Welfare (MOHCW): [http://ochaonline.un.org/OchaLinkClick.aspx?link=ocha&docId=1121703] Final Report for the Zimbabwe national HIV and AIDS estimates 2009. Accessed on 21 October 2010
Ministry of Health and Social Welfare, National Aids Control Programme, Tanzania: Surveillance of HIV and syphilis infections among antenatal clinic attendees 2005/6. Ministry of Health and Social Welfare; 2006.
United Nations General Assembly (UNGASS): [http://data.unaids.org/pub/Report/2008/tanzania_2008_country_progress_report_en.pdf] Mainland Tanzania Country Report of HIV and AIDS. January 2006-December 2007. Accessed on 21 October 2010
Buve A, Carael M, Hayes RJ, Auvert B, Ferry B, Robinson NJ, Anagonou S, Kanhonou L, Laourou M, Abega S, Akam E, Zekeng L, Chege J, Kahindo M, Rutenberg N, Kaona F, Musonda R, Sukwa T, Morison L, Weiss HA, Laga M, Study Group on Heterogeneity of HIV Epidemics in African Cities: Multicentre study on factors determining differences in rate of spread of HIV in Sub-Saharan Africa: methods and prevalence of HIV infection. AIDS 2001, 15 (Suppl 4) : S5-S14.
Boerma JT, Gregson S, Nyamukapa C, Urassa M: Understanding the uneven spread of HIV within Africa: comparative study of biologic, behavioral, and contextual factors in Rural Populations in Tanzania and Zimbabwe. Sex Transm Dis 2003, 30: 779–787.
Mbizvo EM, Msuya S, Hussain A, Chirenje M, Mbizvo M, Sam N, Stray-Pedersen B: HIV and sexually transmitted infections among women presenting at urban primary health care clinics in two cities of sub-Saharan Africa. Afr J Reprod Health 2005, 9: 88–98.
Buve A, Carael M, Hayes R, Robinson NJ: Variations in HIV prevalence between urban areas in sub-Saharan Africa: do we understand them? AIDS 1995, 9 (Suppl A) : S103-S109.
Grosskurth H, Gray RH, Hayes RJ, Mabey D, Wawer M: Control of sexually transmitted diseases for HIV-1 prevention: understanding the implications of the Mwanza and Rakai trials. Lancet 2000, 355: 1981–1987.
Voeten HACM, Vissers DCJ, Gregson S, Zaba B, White RG, de Vlas SJ, Habbema JD: Strong association between in-migration and HIV prevalence in urban sub-Saharan Africa. Sex Transm Dis 2009, in press.
Kurewa EN, Munjoma MW, Chirenje ZM, Rusakaniko S, Hussain A, Stray-Pedersen B: Compliance and loss to follow up of HIV negative and positive mothers recruited from a PMTCT programme in Zimbabwe. Cent Afr J Med 2007, 53: 25–30.
Msuya SE, Mbizvo E, Hussain A, Uriyo J, Sam NE, Stray-Pedersen B: HIV among pregnant women in Moshi Tanzania: the role of sexual behavior, male partner characteristics and sexually transmitted infections. AIDS Res Ther 2006, 3: 27.
Norris AH, Kitali AJ, Worby E: Alcohol and transactional sex: how risky is the mix? Soc Sci Med 2009, 69: 1167–1176.
Gregson S, Garnett GP, Nyamukapa CA, Hallett TB, Lewis JJ, Mason PR, Chandiwana SK, Anderson RM: HIV decline associated with behavior change in Eastern Zimbabwe. Science 2006, 311: 664–666.
Mwaluko G, Urassa M, Isingo R, Zaba B, Boerma JT: Trends in HIV and sexual behavior in a longitudinal study in a rural population in Tanzania, 1994–2000. AIDS 2003, 17: 2645–2651.
Central Statistical Office [Zimbabwe] and Macro International Inc: Zimbabwe Demographic and Health Survey 1999. Calverton, Maryland: Central Statistical Office and Macro International Inc; 2000.
National Bureau of Statistics [Tanzania] and Macro International Inc: Tanzania Reproductive and Child Health Survey 1999. Calverton, Maryland: National Bureau of Statistics and Macro International Inc; 2000.
Central Statistical Office [Zimbabwe] and Macro International Inc: Zimbabwe Demographic and Health Survey 2005–06. Calverton, Maryland: Central Statistical Office and Macro International Inc; 2007.
National Bureau of Statistics [Tanzania] and ORC Macro: Tanzania Demographic and Health Survey 2004–05. Dar es Salaam, Tanzania: National Bureau of Statistics and ORC Macro; 2005.
Chapman R, White RG, Shafer LA, Pettifor A, Mugurungi O, Ross D, Pascoe S, Cowan FM, Grosskurth H, Buve A, Hayes RJ: Do behavioural differences help to explain variations in HIV prevalence in adolescents in sub-Saharan Africa? Trop Med Int Health 2010, 15 (5) : 554–566.
Buve A, Carel M, Hayes RJ, Auvert B, Ferry B, Robinson NJ, Anagonou S, Kanhonou L, Laourou M, Abega S, Akam E, Zekeng L, Chege J, Kahindo M, Rutenberg N, Kaona F, Musonda R, Sukwa T, Morison L, Weiss HA, Laga M, Study Group on Heterogeneity of HIV Epidemics in African Cities: The multicentre study on factors determining the differential spread of HIV in four African cities: summary and conclusions. AIDS 2001, 15 (Suppl 4) : S127-S131.
Fleming DT: From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted disease to sexual transmission of HIV infection. Sex Transm Inf 1999, 75: 3–17.
Steen R, Wi TE, Kamali A, Ndowa F: Control of sexually transmitted infections and prevention of HIV transmission: mending a fractured paradigm. Bull World Health Organ 2009, 87 (11) : 858–865.
Keet IPM, Lee FK, van Griensven GJ, Lange JM, Nahimias A, Coutinho RA: Herpes simplex virus type 2 and other genital ulcerative infections as a risk factor for HIV-1 acquisition. Genitourin Med 1990, 66: 330–333.
Chen CY, Ballard RC, Beck-Sague CM, Dangor Y, Radebe F, Schimid S, Weiss JB, Tshabalala V, Fehler G, Htun Y, Morse SA: Human immunodeficiency virus infection and genital ulcer disease in South Africa: the herpetic connection. Sex Transm Dis 2000, 27: 21–29.
Bailey RC, Moses S, Parker CB, Agot K, Maclean I, Krieger JN, Williams CF, Campbell RT, Ndinya-Achola JO: Male circumcision for HIV prevention in young men in Kisimu, Kenya: a randomised controlled trial. Lancet 2007, 369: 643–656.
Gray RH, Kigozi G, Serwadda D, Makumbi F, Watya S, Nalugoda F, Kiwanuka N, Moulton LH, Chaudhary MA, Chen MZ, Sewankambo NK, Wabwire-Mangen F, Bacon MC, Williams CF, Opendi P, Reynolds SJ, Laeyendecker O, Quinn TC, Wawer MJ: Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet 2007, 369: 657–666.
Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A: Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS Med 2005, 2: e298.
van Howe SR: Genital ulcerative disease and sexually transmitted urethritis and circumcision: a meta-analysis. Int J STD AIDS 2007, 18: 799–809.
Weiss HA, Thomas SL, Munabi SK, Hayes RJ: Male circumcision and risk of syphilis, chancroid, and genital herpes: a systematic review and meta-analysis. Sex Transm Infect 2006, 82: 101–110.
Kishamawe C, Vissers DC, Urassa M, Isingo R, Mwaluko G, Borsboom GJ, Voeten HA, Zaba B, Habbema JD, de Vlas SJ: Mobility and HIV in Tanzanian couples: both mobile persons and their partners show increased risk. AIDS 2006, 20: 601–608.
Rolinson D: A wake up call for urinary schistosomiasis: reconciling research effort with public health importance. Parasitology 2009, 136: 1593–1610.
Mann JM, Francis H, Davachi F, Baudoux P, Quinn TC, Nzilambi N, Bosenge N, Colebunders RL, Piot P, Kabote N: Risk factors for immunodeficiency virus seropositivity among children 1–24 months old in Kinshasha, Zaire. Lancet 1986, 11: 654–657.
Lepage P, Van de Perre P, Carael M, Butzler JP: Are medical injections a risk factor for HIV infection in children? Lancet 1986, 11: 1103–1104.
Commenges D, Alioum A, Lepage P, Van de Perre P, Msellati P, Dabis F: Estimating the incubation period of paediatric AIDS in Rwanda. AIDS 1992, 6: 1515–1520.
Prazuck T, Tall F, Nacro B, Rochereau A, Traore A, Sanou T, Malkin JE, Apaire-Marchais V, Masson D, Dublanchet A: HIV infection and severe malnutrition: a clinical and epidemiological study in Burkina Faso. AIDS 1993, 7: 103–108.
De Cock KM, Zadi F, Adjorlolo G, Diallo MO, Sassan-Morokro M, Ekpini E, Sibailly T, Doorly R, Batter V, Brattegaard K: Retrospective study of maternal HIV-1 and HIV-2 infections and child survival in Abijan, Côte d'Ivoire. Br Med J 1994, 308: 441–442.
Gisselquist D, Rothenberg R, Potterat J, Drucker E: HIV infections in sub-Saharan Africa not explained by sexual or vertical transmission. Int J STD AIDS 2002, 13: 657–666.
Zaba BW, Carpenter LM, Boerma JT, Gregson S, Nakiyingi J, Urassa M: Adjusting antenatal clinic data for improved estimates of HIV prevalence among women in sub-Saharan Africa. AIDS 2000, 14: 2741–2750.
Acknowledgements
We gratefully acknowledge the women who participated in this study and the study support staff. Special thanks go to the Letten Foundation for funding the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
Letten F Saugstad is the founder of the Letten Foundation, which sponsored the study in Zimbabwe and Tanzania. The other authors have no conflicts of interest to declare.
Authors' contributions
MPM drafted the manuscript, analyzed data and interpreted results. SJDV contributed to drafting of the manuscript and interpretation of results. ENK, MWM, SM and NS participated in data collection. MZC supervised data collection. RS participated in data analysis. LFS participated in protocol development and interpretation of results. BSP developed the protocol, participated in drafting of the manuscript and interpretation of results. All authors read and approved the final version of the manuscript.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Mapingure, M.P., Msuya, S., Kurewa, N.E. et al. Sexual behaviour does not reflect HIV-1 prevalence differences: a comparison study of Zimbabwe and Tanzania. JIAS 13, 45 (2010). https://doi.org/10.1186/1758-2652-13-45
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1758-2652-13-45