Abstract
Background
Metastasis-associated in colon cancer 1 (MACC1) is demonstrated to be up-regulated in several types of cancer, and can serve as biomarker for cancer invasion and metastasis. To investigate the relations between MACC1 and biological processes of ovarian cancer, MACC1 specific small hairpin RNA (shRNA) expression plasmids were used to investigate the effects of MACC1 inhibition on ovarian carcinoma OVCAR-3 cells.
Methods
Expressions of MACC1 were detected in different ovarian tissues by immunohistochemistry. MACC1 specific shRNA expression plasmids were constructed and transfected into OVCAR-3 cells. Then, expressions of MACC1 were examined by reverse transcription polymerase chain reaction (RT-PCR) and Western blot. Cell proliferation was observed by MTT and monoplast colony formation assay. Flow cytometry and TUNEL assay were used to measure cell apoptosis. Cell migration was assessed by wound healing and transwell migration assay. Matrigel invasion and xenograft model assay were performed to analyze the potential of cell invasion. Activities of Met, MEK1/2, ERK1/2, Akt, cyclinD1, caspase3 and MMP2 protein were measured by Western blot.
Results
Overexpressions of MACC1 were detected in ovarian cancer tissues. Expression of MACC1 in OVCAR-3 cells was significantly down-regulated by MACC1 specific small hairpin RNA. In OVCAR-3 cells, down-regulation of MACC1 resulted in significant inhibition of cell proliferation, migration and invasion, meanwhile obvious enhancement of apoptosis. As a consequence of MACC1 knockdown, expressions of Met, p-MEK1/2, p-ERK1/2, cyclinD1 and MMP2 protein decreased, level of cleaved capase3 was increased.
Conclusions
RNA interference (RNAi) against MACC1 could serve as a promising intervention strategy for gene therapy of ovarian carcinoma, and the antitumor effects of MACC1 knockdown might involve in the inhibition of HGF/Met and MEK/ERK pathways.
Similar content being viewed by others
Background
Ovarian cancer is one of malignant tumors in female genital system, but is the leading cause of death from gynecological cancer in the world [1]. Despite improvements in the application of aggressive cytoreductive surgery and combination chemotherapy, ovarian cancer has the most unfavorable prognosis due to its insidious onset, diagnosis at late stage, dissemination, relapse, and tendency to develop chemotherapy resistance. Though considerable efforts aim at elucidating the tumorigenesis of ovarian carcinoma, its molecular mechanism has not been completely explained.
Recently, MACC1 has been identified as a prognosis biomarker for colon cancer, which promotes proliferation, invasion and hepatocyte growth factor (HGF)-induced scattering of colon cancer cells in vitro and in vivo [2]. MET, which encodes Met protein, has been proven to be a transcriptional target of MACC1. MACC1 controls the activity and expression of MET, and regulates HGF/Met signal pathway [2]. HGF/Met pathway plays key roles in carcinogenesis, aberrant activation of Met leads to enhancement of cell proliferation, invasion and metastasis, and Met is essential for metastatic potential of many malignances [3]. Once activated by HGF, Met transmits intracellular signals and activates downstream Ras-mitogen-activated protein kinase (MAPK) and phosphoinositide 3-kinase (PI3K)/Akt pathways, which promote cell survival, migration, invasion, and suppress apoptosis [4].
MACC1 was demonstrated to be associated with poor prognosis and high risk of metastasis in colon cancer, gastric carcinoma, lung cancer, and hepatocellular carcinoma [5–8]. However, the mechanism of MACC1 implicates in ovarian cancer is still unclear. Small interfering RNA can specifically silence particular genes, and is used as a powerful tool to research gene functions and as a genetic therapy strategy for carcinoma [9]. In present study, expressions of MACC1 were detected in different ovarian tissues by immunohistochemistry, effects of MACC1 inhibition on OVCAR-3 cells were observed by RNA interference, and the possible antitumor mechanisms of MACC1 knockdown in ovarian carcinoma cells were discussed.
Materials and methods
Immunohistochemistry and evaluation
Paraffin-embedded 20 specimens of normal ovary, 19 specimens of benign ovarian tumor and 52 specimens of ovarian cancer tissues were obtained from Department of Pathology of Zhengzhou University. Rabbit-anti-human polyclonal MACC1 antibody (Sigma, USA) was used for immunohistochemistry assay, which was performed following the protocol of Universal SP kit (Zhongshan Goldenbridge Biotechnology, Peking, China). Positive staining of MACC1 protein presents brown in cytoplasm, partly in nucleus. Semi-quantitative counting method was used to determine positive staining described as following: Selected 10 visual fields under high power lens (× 400) randomly, counted the numbers of positive cells in 100 cells per field, calculated the average positive rate. Positive rate less than 1/3 scored as 1, more than 1/3 and less than 2/3 scored as 2, more than 2/3 scored as 3, without positive cell scored as 0. Cells without brown staining scored as 0, with mild brown staining scored as 1, with moderate brown staining scored as 2, with intense brown staining scored as 3. The final positive scores = positive rate score × staining intensity score, 0 score was negative staining (-), 1~4 scores were positive staining (+), more than 4 scores was strong positive (++).
ShRNAs synthesis and plasmids construction
Single shRNA strands were 5'-GATCCCC-N21-TTCAAGAGA-N'21-TTTTTGGA-AA-3' (sense) and 5'-AGCTTTTCCAAAAA-N21-TCTCTTGAAN'21-GGG-3' (antisense). N21 was the sense sequence of MACC1 target oligonucleotides, N'21 was antisense sequence of MACC1 target oligonucleotides. Three different template oligonucleotides targeting MACC1 [GeneBank, NM_182762.3] were as follow: MACC1-s1, 5'-AAAGACAGAAGGAGAAAGGAA-3'; MACC1-s2, 5'-AATCAAC-
TGTCTGCTTCTAAC-3'; MACC1-s3, 5'-AATTATATGCCAGGACAGCTT-3'. As a negative control, one scrambled sequence 5'-AACAGTTATCTATGCGACAGT-3' (corresponding to MACC1-s3) was designed. These sequences were submitted to BLAST against human genome sequence to ensure that only MACC1 gene was targeted. All single shRNA strands were synthesized at Sangon Biotechnology Co., Ltd (Shanghai, China), and were annealed and ligated into the BglII and HindIII sites of linearized psuper-EGFP plasmid. The four shRNAs inserted vectors were named as psuper-EGFP-s1, psuper-EGFP-s2, psuper-EGFP-s3, and psuper-EGFP-NC respectively.
Cell transfection
Human ovarian carcinoma OVCAR-3 cells (with high level of MACC1 expression measured in our preliminary study) were purchased from Chinese Academy of Sciences Cell Bank (Shanghai, China), and cultured in DMEM medium (HyClone, USA) supplemented with 10% fetal bovine serum (FBS), 100 U/ml penicillin and 100 mg/ml streptomycin at 37°C with 5% CO2. Cells were harvested in logarithmic phase of growth for all experiments described below. Cell transfection was performed following the protocol of Lipofectamine 2000 (Invitrogen, USA). The untransfected cells, empty vector (psuper-EGFP-neo) transfected cells, and nonspecific shRNA (psuper-EGFP-NC) transfected cells were used as controls. Stably transfected OVCAR-3 cells were selected with 800 μg/ml G418 (Sigma, USA) after tansfection 48 h. After 12 days, resistant colonies were trypsinized and cultured in selective medium. Names of the stably transfected cells were OVCAR-3-neo, OVCAR-3-NC, OVCAR-3-s1, OVCAR-3-s2, and OVCAR-3-s3 respectively.
RT-PCR
Cell total RNA was isolated using Trizol Reagent (Invitrogen, USA), and first strand cDNA was synthesized from 1 μg total RNA according to the protocol of RevertAid first strand cDNA synthesis kit (Fermentas, EU). Primers used in RT-PCR were as follow: MACC1, 5'-CCTTCGTGGTAATAATGCTTCC-3' (sense) and 5'-AGGGCTTCCATTGTATTGAGGT-3' (antisense); β-actin, 5'-ACGCACC- CCAACTACAACTC-3' (sense) and 5'-TCTCCTTAATGTCACGCACGA-3' (antisense). PCR cycling parameters (19 cycles) were: denaturation (94°C, 30s), annealing (56°C, 30s) and extension (72°C, 30s). Equal amounts of PCR products were electrophoresed on 1.2% agarose gels and visualized by ethidium bromide staining. The specific bands of PCR products were analyzed by Image-Pro Plus 6.0 system, β-actin was used as a control for normalization. RT-PCR was performed for three times independently.
Western blot
Primary antibodies used in Western blot, following manufacturer's protocols, were anti-MACC1 (Sigma, USA), anti-Met, anti-p-MEK1/2(ser212/ser218), anti-MEK1/2, anti-p-ERK1/2(Thr202/Tyr204), anti-ERK1/2 and anti-MMP2 (Santa Cruz, USA), anti-Akt, anti-p-Akt(Thr308), anti-cyclinD1, anti-cleaved caspase3 and anti-β-actin (Beyotime Biotechnology, Jiangsu, China). Total protein was extracted using Cell Lysis Buffer for Western and IP (Beyotime Biotechnology, Jiangsu, China), and protein concentration was determined using Bradford assay. Equal amounts of protein (30 μg) were separated by 10% SDS-PAGE and transferred onto PVDF membranes. The detection of hybridized protein was performed by enhanced chemiluminescence kit (Zhongshan Goldenbridge Biotechnology, Peking, China), β-actin was used as a control for normalization. The specific bands were analyzed by Image-Pro Plus 6.0 system.
MTT assay
Planted 2 × 104 cells per well into 96-well plates, and added 100 μl medium containing 10% FBS into each well. Five duplicate wells were set up for each group. Cultured cells continuously for 7 days, added 20 μl MTT reagent (5 mg/ml, Sigma, USA) into each well, incubated for another 4 h then aspirated former medium and added 150 μl DMSO. The absorbance of sample was measured by Microplate spectrophotometer (Thermo, USA) at 492 nm. All experiments were done in triplicate. Cell growth curve was plotted versus time by origin 8 software.
Monoplast colony formation assay
Prepared single cell suspension, seeded about 50, 100, 200 cells of each group into 6-well plates respectively. Added 2 ml medium containing 10% FBS into each well, cultured cells continuously for one week. Fixated cells with methanol for 5 min, stained cells by hematoxylin for 30 min, counted the numbers of colony (more than 10 cells per colony) under low power lens (× 100) of inverted microscope (OLYMPUS, IX71, Japan), and calculated the rate of colony formation.
Flow cytometry analysis
About 1 × 106 cells were treated into single cell suspension with PBS solution, and were prepared following manufacture's protocol of Annexin V-FITC Apoptosis Detection Kit (Beyotime Biotechnology, Jiangsu, China). Then, rates of apoptosis were analyzed with FACScan system (BD, USA).
TUNEL assay
Dripped single cell suspension onto microscopic slides, incubated cells for 4 h till cells were adherent. Three duplicate slides were set up for each group. Fixated cells by 4% paraformaldehyde for 30 min, blocked cells by 0.3% H2O2 for 30 min, incubated cells with 0.1% Triton X-100 for 2 min, then performed following manufacture's protocol of In situ cell death detection kit (Roche, German). Selected five visual fields under high power lens (× 400) randomly, counted the numbers of apoptotic body in 100 cells, calculated the rate of apoptosis.
Wound healing assay
About 5 × 104~1 × 105 cells were seeded into each well of 6-well plates, three duplicate wells were set up for each group, monolayer cells were obtained after cells confluence. Scratched monolayer cells with 200 μl pipette tip, washed cells 3 times with PBS, and added 2 ml medium without FBS into each well. The values of scratch were measured at 0 h and 24 h after scratching by Image Pro-Plus 6.0 system.
Transwell migration assay
Transwell chambers (8 μm pore size; Millipore, USA) were also used to measure cell migration. Seeded 2 × 105 cells into each upper chamber with 200 μl fresh medium without FBS, added 500 μl medium with 20% FBS into each lower chamber, three duplicate wells were set up for each group. After 12 h, fixated cells with methanol for 5 min, and stained cells by hematoxylin for 30 min. Cleaned upper chamber and inverted the chamber, counted cell numbers on the lower membrane under high power lens (× 400) in five random visual fields.
Matrigel invasion assay
Transwell chamber (8 μm pore size; Millipore, USA) covered with 100 μl of 1 mg/ml Matrigel (BD, USA) was used to measure cell invasive ability. Seeded 1 × 105 cells into each upper chamber with 200 μl fresh medium without FBS, added 500 μl medium with 20% FBS into each lower chamber, three duplicate wells were set up for each group. After 12 h, fixated cells with methanol for 5 min, and stained cells by hematoxylin for 30 min. Cleaned upper chamber and inverted the chamber, counted cell numbers on the lower membrane under high power lens (× 400) in five random visual fields.
Xenograft model assay
The experimental protocol was approved by Zhengzhou University Ethics Committee for Animal Experimentation. Female BALB/c nu/nu mice (4-5 weeks old, 13-17 g) were purchased from Vital River Laboratory Animal Technology Co., Ltd (Peking, China), and were randomly assigned into four groups with 4 mice per group. About 1 × 107 cells were suspended in 0.2 ml PBS and injected subcutaneously into one mouse. The tumors were monitored every 5 days beginning at day 5 by measuring two perpendicular diameters with a caliper. The mice were sacrificed on the 35th day after injection, tumors were dissected and measured, and tumor volume in mm3 was calculated by the formula: volume = (width)2 × length/2 [10].
Statistical analysis
Average values were expressed as mean ± standard deviation (SD). Count data were analyzed by χ2 test. Measurement data were analyzed by one-way ANOVA and Bonferroni test using SPSS 17.0 software package. Difference was considered significant when P value was less than 0.05.
Results
Overexpressions of MACC1 in ovarian cancer tissues
The positive rates of MACC1 in normal ovary, benign ovarian tumor and ovarian cancer tissues were detected by immunohistochemistry (Table 1). Compared to normal ovary and benign ovarian tumor, expressions of MACC1 were obviously up-regulated in ovarian cancer tissues (Figure 1), which showed abnormal expression of MACC1 might be associated with ovarian cancer.
Immunohistochemistry analysis of MACC1 expression in different ovarian tissues. Normal ovary (A) and benign ovarian tumor (B) showed a lower staining of MACC1, but ovarian cancer (C) showed higher density staining (DAB staining, × 400). (D): Bar graphs show the positive rates of MACC1 protein. *P < 0.05 versus normal and benign ovarian tissues.
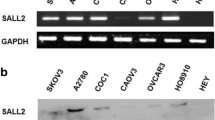
Down-regulation of MACC1 expressions by RNAi
After transfection 48 h, transfected cells with green fluorescence under fluorescence microscopy were observed (Figure 2). Expressions of MACC1 in stably transfected cells, which were selected by G418, were measured by RT-PCR and Western blot. Compared to control cells, levels of MACC1 mRNA and protein were significantly down-regulated in OVCAR-3-s1, OVCAR-3-s2 and OVCAR-3-s3 cells, especially in OVCAR-3-s3 cells (Figure 3). According to these results, OVCAR-3-s3 cells which showed the highest inhibitory rate of MACC1 were used for further assay described below.
Transfection of MACC1-shRNA into ovarian carcinoma OVCAR-3 cells. (A): Normal OVCAR-3 cells under incandescent light (× 200). (B): After transfection 24 h, OVCAR-3-s3 cells under fluorescent light (× 100). (C): Monoplast colony of OVCAR-3-s3 cells selected by G418 for three weeks (× 200). (D): G418 resistant OVCAR-3-s3 cell line (× 100).
Down-regulation of MACC1 by MACC1-shRNA in ovarian carcinoma cells. The best inhibitory effects of MACC1 were identified in OVCAR-3-s3 cells by RT-PCR (A) and Western blot (C), which were both performed for three times independently. Bar graphs show the relative expression levels of MACC1 mRNA (B) and protein (D).*P < 0.05 versus control groups.
Inhibition of cell proliferation and colony formation by MACC1 RNAi
According to Figure 4, the proliferation of OVCAR-3-s3 cells was obviously inhibited from the second day, when compared with control cells. There were no differences among OVCAR-3, OVCAR-3-neo and OVCAR-3-NC cells. In addition, OVCAR-3-s3 cells had lower rate of colony formation than control groups as shown in Figure 5. Thus, knockdown of MACC1 by RNAi could inhibit the growth of ovarian carcinoma cells.
MACC1-shRNA inhibited the monoplast colony formation of ovarian carcinoma cells. Monoplast colony in 50-cells wells of each group. (A): OVCAR-3 cells. (B): OVCAR-3-neo cells. (C): OVCAR-3-NC cells. (D): OVCAR-3-s3 cells (Hematoxylin staining, × 100). Bar graphs show the average rates of monoplast colony formation.*P < 0.05 versus control groups.
Apoptosis induced by MACC1 RNAi
Cell apoptosis rate measured by flow cytometer (Figure 6) in OVCAR-3-s3 cells was markedly increased to 24.13%, higher than 3.37% for OVCAR-3, 7.82% for OVCAR-3-neo, and 7.19% for OVCAR-3-NC cells (P < 0.05). Furthermore, TUNEL assay showed numbers of apoptosis body were increased in OVCAR-3-s3 cells (Figure 7). The results of apoptosis assay indicated the inhibitory effect of cell growth might due to the enhancement of apoptosis by MACC1 RNAi.
MACC1-shRNA increased the apoptosis rate of ovarian carcinoma cells. TUNEL assay was used to measure the apoptosis rate in OVCAR-3 cells (A), OVCAR-3-neo cells (B), OVCAR-3-NC cells (C), and OVCAR-3-s3 cells (D). DAB staining, × 400. Bar graphs show the rates of apoptosis.*P < 0.05 versus control groups.
Suppression of migration by MACC1 RNAi
Compared with control groups, OVCAR-3-s3 cells showed suppressed capacity of impaired migration (Figure 8 and 9). Moreover, numbers of cell adherent on lower membranes of transwell chamber were sharply decreased in OVCAR-3-s3 group, which were shown in Figure 10. These results suggested MACC1 RNAi could suppress migration capability of ovarian carcinoma cells.
Inhibition of MACC1 by RNAi suppressed the migration ability of ovarian carcinoma cells. Transwell migration assay was used for cell migration ability assay. (A): OVCAR-3 cells. (B): OVCAR-3-neo cells. (C): OVCAR-3-NC cells. (D): OVCAR-3-s3 cells (Hematoxylin staining, × 400). Each bar represents the cell numbers adherent on lower membrane.*P < 0.05 versus control groups.
Activity of invasion retarded by MACC1 RNAi
The numbers of cell, assessed in Matrigel invasion assay, were remarkably decreased in OVCAR-3-s3 group (Figure 11). On the other hand, the volumes of xenograft tumors removed from nude mice were retarded apparently in OVCAR-3-s3 group after 35 days. As shown in Figure 12, the growth of xenograft tumors in OVCAR-3-s3 group obviously fell behind other groups. Results of invasion assay indicated invasive potential of ovarian carcinoma cells could be retarded by MACC1 RNAi.
Inhibition of invasion by MACC1 RNAi in ovarian carcinoma cells. Cell invasive ability was assessed by Matrigel invasion assay. (A): OVCAR-3 cells. (B): OVCAR-3-neo cells. (C): OVCAR-3-NC cells. (D): OVCAR-3-s3 cells (Hematoxylin staining, × 400). Each bar represents the cell numbers adherent on lower membrane.*P < 0.05 versus control groups.
Down-regulation of Met and MEK/ERK pathways activity by MACC1 RNAi
Expressions of Met, MEK1/2, p-MEK1/2, ERK1/2, p-ERK1/2, Akt and p-Akt were measured by Western blot in OVCAR-3, OVCAR-3-neo, OVCAR-3-NC and OVCAR-3-s3 cells. As a result of MACC1 knockdown, significant reductions of Met and p-MEK1/2 and p-ERK1/2 expression were observed in OVCAR-3-s3 cells. However, none obvious changes were detected on levels of total MEK1/2, total ERK1/2, total Akt and p-Akt (Figure 13 and 14). In addition, expressions of cyclinD1 and MMP2 decreased, level of cleaved caspase3 was increased after MACC1 inhibition (Figure 15).
Discussion
Among gynecological cancers, more than 75% of ovarian carcinoma patients are suffered with advanced disease, and the majority will relapse and die of their disease [11, 12]. Despite major efforts in diagnosis and improvements in the treatment of epithelial ovarian cancer, current therapies for advanced ovarian cancer are not effective enough and total survival rate of subjects with ovarian carcinoma has not changed appreciably.
MACC1 is closely associated with several types of cancer, and can serve as poor prognosis and metastatic biomarker for colon cancer, gastric carcinoma, lung cancer, and hepatocellular carcinoma [5–8]. In this study, we detected high levels of MACC1 in ovarian cancer tissues by immunohistochemistry, which showed abnormal expression of MACC1 might be associated with ovarian carcinoma. However, the relations between abnormal expression of MACC1 and ovarian carcinoma had not yet been reported.
Thus, we designed and synthesized three specific shRNAs against MACC1 gene to investigate the effects of MACC1 inhibition on ovarian carcinoma OVCAR-3 cells in present study. Results of RT-PCR and Western blot showed specific MACC1-shRNAs could effectively knockdown expression of MACC1 in OVCAR-3 cells. We also successfully obtained OVCAR-3 cell line with the best inhibitory effects of MACC1 expression for further analysis. As a consequence of MACC1 gene knockdown, the proliferation, migration and invasion of OVCAR-3 cells were obviously inhibited, but the apoptosis rate was significantly increased. These results showed inhibition of MACC1 could suppress the growth and metastatic potential of ovarian carcinoma cells in vitro and in vivo, which suggested MACC1 might implicate in the growth and metastasis of ovarian carcinoma.
MACC1 binds to a 60 bp proximal fragment of endogenous MET promoter, where contains a specific Sp1 binding site which is essential for MACC1-induced activation of MET and subsequent HGF/Met signaling consequences [13]. Once activated, Met can result in activation of several downstream signaling cascades, such as MAPK and PI3K/Akt pathways [14]. MACC1 protein contains several domains which can participate in MAPK signaling, and MACC1 can be up-regulated by MAPK pathway which has been identified to be essential for HGF-induced scattering [15–17]. In colon cancer cells, MAPK signaling could be hyperactive by transfection of MACC1, and HGF-induced cell scattering mediated by MACC1 could be abrogated by MEK specific inhibitors, whereas not by PI3K specific inhibitors [2].
After inhibition of MACC1 by RNAi in ovarian carcinoma OVCAR-3 cells, we observed that level of Met protein was down-regulated significantly, as well as expressions of p-MEK1/2 and p-ERK1/2 protein, but expression of p-Akt was uninfluenced. Therefore, we presumed that inhibition of MACC1 by RNAi might suppress the malignant behavior of ovarian carcinoma cells via HGF/Met and MEK/ERK pathways, at least in part. Furthermore, increased level of cleaved caspase3 and decreased levels of cyclinD1 and MMP2 protein were detected in ovarian carcinoma cells after RNA interference against MACC1, which suggested cyclinD1, caspase3 and MMP2 should be associated with MACC1 mediated downstream signaling.
HGF/Met signaling plays an important role in cellular growth, epithelial-mesenchymal transition, angiogenesis, cell motility, invasiveness and metastasis [18]. Deregulated HGF/C-met signaling has been observed in many tumors, including ovarian carcinoma, and been proved to contribute to tumor dissemination and metastasis [19]. MAPK and PI3K/Akt pathways have been demonstrated to implicate in cell survival, anti-apoptosis, invasion, metastasis and angiogenesis of malignancies, including ovarian carcinoma [20–22]. Because of these cascades play key roles in carcinogenesis, some specific antibodies and small molecules to neutralize or block the key regulators of these pathways have been used to inhibit tumor growth and metastasis, which exploit effective intervention strategies for malignancies [19, 23, 24]. According to previous reports and the results described above, we considered that MACC1, as a key regulator and upstream signaling of these pathways, could be a potential therapeutic target for ovarian cancer.
Conclusions
In summary, our data showed that MACC1 might implicate in growth and metastasis of ovarian carcinoma. In ovarian carcinoma cells, the antitumor effects of MACC1 RNAi might involve in the inhibition of HGF/Met and MEK/ERK pathways. As a key regulator of HGF/Met signaling, RNA interference against MACC1 could serve as a promising intervention strategy for gene therapy of ovarian carcinoma.
Abbreviations
- ERK:
-
extracellular signal-regulated kinase
- HGF:
-
hepatocyte growth factor
- MACC1:
-
metastasis-associated in colon cancer 1
- MAPK:
-
mitogen-activated protein kinase
- MEK:
-
mitogen-activated protein kinase kinase
- Met:
-
hepatocyte growth factor receptor
- PI3K:
-
phosphoinositide 3-kinase
- RNAi:
-
RNA interference
- shRNA:
-
small hairpin RNA.
References
Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ: Cancer statistics, 2009. CA Cancer J Clin. 2009, 59: 225-249. 10.3322/caac.20006.
Stein U, Walther W, Arlt F, Schwabe H, Smith J, Fichtner I, Birchmeier W, Schlag PM: MACC1, a newly identified key regulator of HGF-MET signaling, predicts colon cancer metastasis. Nat Med. 2009, 15: 59-67. 10.1038/nm.1889.
Toschi L, Jänne PA: Single-agent and combination therapeutic strategies to inhibit hepatocyte growth factor/MET signaling in cancer. Clin Cancer Res. 2008, 14: 5941-5946. 10.1158/1078-0432.CCR-08-0071.
Bottaro DP, Rubin JS, Faletto DL, Chan AM, Kmiecik TE, Vande Woude GF, Aaronson SA: Identification of the hepatocyte growth factor receptor as the c-met proto-oncogene product. Science. 1991, 251: 802-804. 10.1126/science.1846706.
Shirahata A, Shinmura K, Kitamura Y, Sakuraba K, Yokomizo K, Goto T, Mizukami H, Saito M, Ishibashi K, Kigawa G, Nemoto H, Hibi K: MACC1 as a marker for advanced colorectal carcinoma. Anticancer Res. 2010, 30: 2689-2692.
Shirahata A, Sakata M, Kitamura Y, Sakuraba K, Yokomizo K, Goto T, Mizukami H, Saito M, Ishibashi K, Kigawa G, Nemoto H, Hibi K: MACC 1 as a marker for peritoneal-disseminated gastric carcinoma. Anticancer Res. 2010, 30: 3441-3444.
Shimokawa H, Uramoto H, Onitsuka T, Chundong G, Hanagiri T, Oyama T, Yasumoto K: Overexpression of MACC1 mRNA in lung adenocarcinoma is associated with postoperative recurrence. J Thorac Cardiovasc Surg. 2011, 141: 895-898.
Shirahata A, Fan W, Sakuraba K, Yokomizo K, Goto T, Mizukami H, Saito M, Ishibashi K, Kigawa G, Nemoto H, Sanada Y, Hibi K: MACC 1 as a marker for vascular invasive hepatocellular carcinoma. Anticancer Res. 2011, 31: 777-780.
Yu JY, DeRuiter SL, Turner DL: RNA interference by expression of short interfering RNAs and hairpin RNAs in mammalian cells. Proc Natl Acad Sci USA. 2002, 99: 6047-6052. 10.1073/pnas.092143499.
Osborne CK, Hobbs K, Clark GM: Effect of estrogens and antiestrogens on growth of human breast cancer cells in athymic nude mice. Cancer Res. 1985, 45: 584-590.
Heintz AP, Odicino F, Maisonneuve P, Quinn MA, Benedet JL, Creasman WT, Ngan HY, Pecorelli S, Beller U: Carcinoma of the ovary. FIGO 26th Annual Report on the Results of Treatment in Gynecological Cancer. Int J Gynaecol Obstet. 2006, 95 (Suppl 1): 161-192.
Edwards BK, Brown ML, Wingo PA, Howe HL, Ward E, Ries LA, Schrag D, Jamison PM, Jemal A, Wu XC, Friedman C, Harlan L, Warren J, Anderson RN, Pickle LW: Annual report to the nation on the status of cancer, 1975-2002, featuring population-based trends in cancer treatment. J Natl Cancer Inst. 2005, 97: 1407-1427. 10.1093/jnci/dji289.
Stein U, Smith J, Walther W, Arlt F: MACC1 controls Met: what a difference an Sp1 site makes. Cell Cycle. 2009, 8: 2467-2469. 10.4161/cc.8.15.9018.
Ponzetto C, Bardelli A, Zhen Z, Maina F, dalla Zonca P, Giordano S, Graziani A, Panayotou G, Comoglio PM: A multifunctional docking site mediates signaling and transformation by the hepatocyte growth factor/scatter factor receptor family. Cell. 1994, 77: 261-271. 10.1016/0092-8674(94)90318-2.
Kokoszyńska K, Kryński J, Rychlewski L, Wyrwicz LS: Unexpected domain composition of MACC1 links MET signaling and apoptosis. Acta Biochim Pol. 2009, 56: 317-323.
Li SS: Specificity and versatility of SH3 and other proline-recognition domains: structural basis and implications for cellular signal transduction. Biochem J. 2005, 390: 641-653.
Potempa S, Ridley AJ: Activation of both MAP kinase and phosphatidylinositide 3-kinase by Ras is required for hepatocyte growth factor/scatter factor-induced adherens junction disassembly. Mol Biol Cell. 1998, 9: 2185-2200.
Mazzone M, Comoglio PM: The Met pathway: master switch and drug target in cancer progression. FASEB J. 2006, 20: 161116-161121.
Zhou HY, Pon YL, Wong AS: HGF/MET signaling in ovarian cancer. Curr Mol Med. 2008, 8: 469-480. 10.2174/156652408785747933.
Cantley LC: The phosphoinositide 3-kinase pathway. Science. 2002, 296: 1655-1657. 10.1126/science.296.5573.1655.
Seger R, Krebs EG: The MAPK signaling cascade. FASEB J. 1995, 9: 726-735.
Nicosia SV, Bai W, Cheng JQ, Coppola D, Kruk PA: Oncogenic pathways implicated in ovarian epithelial cancer. Hematol Oncol Clin North Am. 2003, 17: 927-943. 10.1016/S0889-8588(03)00056-X.
Montagut C, Settleman J: Targeting the RAF-MEK-ERK pathway in cancer therapy. Cancer Lett. 2009, 283: 125-134. 10.1016/j.canlet.2009.01.022.
Wu P, Hu YZ: PI3K/Akt/mTOR pathway inhibitors in cancer: a perspective on clinical progress. Curr Med Chem. 2010, 17: 4326-4341. 10.2174/092986710793361234.
Acknowledgements
We thank Qinxian Zhang who was from Department of Organization and Embryology of Basic Medical College of Zhengzhou University for providing us plasmid psuper-EGFP as a kind gift for free.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
ZR participated in design of the study, carried out molecular genetic studies, drafted manuscript and performed statistical analysis. SH participated in design of the study and reviewed manuscript. CZ, RF and HH carried out immunohistochemistry and participated in statistical analysis. WQ participated in design of the study and helped to draft manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Zhang, R., Shi, H., Chen, Z. et al. Effects of metastasis-associated in colon cancer 1 inhibition by small hairpin RNA on ovarian carcinoma OVCAR-3 cells. J Exp Clin Cancer Res 30, 83 (2011). https://doi.org/10.1186/1756-9966-30-83
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1756-9966-30-83