Abstract
Background
Co-administration of anti-tuberculosis and antiretroviral therapy is often inevitable in high-burden countries where tuberculosis is the most common opportunistic infection associated with HIV/AIDS. Concurrent use of rifampicin and several antiretroviral drugs is complicated by pharmacokinetic drug-drug interaction.
Method
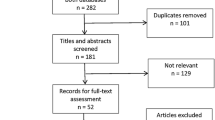
Pubmed and Google search following the key words tuberculosis, HIV, emtricitabine, tenofovir efavirenz, interaction were used to find relevant information on each drug of the fixed dose combination AtriplaR
Results
Information on generic name, trade name, pharmacokinetic parameter, metabolism and the pharmacokinetic interaction with Anti-TB drugs of emtricitabine, tenofovir, and efavirenz was obtained.
Conclusion
Fixed dose combination of emtricitabine/tenofovir/efavirenz (ATRIPLAR) which has been approved by Food and Drug Administration shows promising results as far as safety and efficacy is concerned in TB/HIV co-infection patients, hence can be considered effective and safe antiretroviral drug in TB/HIV management for adult and children above 3 years of age.
Similar content being viewed by others
Background
Human immunodeficiency virus (HIV) and tuberculosis (TB) are overlapping epidemics that cause an immense burden of disease. Sub-Sahara Africa is a region most affected by both diseases including Tanzania [1]. Literatures show that more than 75% of TB patients have also HIV, and possibly more than half of worldwide patients infected with HIV will also develop TB [2, 3]. Furthermore TB contributed to 27% of all AIDS diagnoses [4]. For TB the currently used combination drug regimens produce cure rates that exceed 95%, given good patient adherence during the multiple months' treatment period [5]. Also for HIV many regimens are available; however optimal treatment regimens for TB/HIV co-infection are not yet clearly defined.
As therapy for HIV disease becomes more available, physicians need to know how to treat these two diseases effectively while minimizing the risk of drug interactions and maintaining the shortest possible duration of treatment for TB. Current treatment of mycobacterium tuberculosis in most resource limited settings is comprised of a four-drug initial anti-tuberculosis regimen for 2 months (rifampicin, isoniazid, pyrazinamide and ethambutol), followed by two-drugs continuation phase of anti-tuberculosis regimen for 4 months (rifampicin and isoniazid). For TB/HIV co-infected patients the guidelines which exist [6] have shown many challenges.
Combining drug therapies for dual infection TB and HIV is made complex by alterations in the activity of the hepatic Cytochrome P450 (CYP) system, high pill burdens, shared drug toxicities, drug-drug and drug-disease interactions, immune reconstitution inflammatory syndrome, co-morbid diseases and drug resistance in both bacillus and virus [7, 8]. The CYP isoform enzymes are responsible for many interactions [9] (especially those involving rifampicin and isoniazid) during drug biotransformation (metabolism) in the liver and/or intestine, due to it is enzyme induction effect.
Presentation of the hypothesis
Adherence to a complex regimen is often a significant barrier to treatment success. Following the current guideline where a patient has to take 4-fixed dose combination for TB and the complex triple combination therapy selected for HIV treatment. The consequence of many pills reduce compliance and hence adherence to the treatment regimen leading to suboptimal TB and HIV treatment, hence increasing the possibility of drug resistance and shared drug toxicities [10]. These toxicities may necessitate therapy discontinuation, which exacerbates immune suppression and predisposes to other opportunistic infections.
TB/HIV co-infection simultaneous treatment have shown pharmacokinetic interactions produced with mainly rifampicin [(a cornerstone in TB treatment) and the non nucleoside reverse transcriptase inhibitors (NNRTIs)]. Enzyme inducer decreases elimination halve life of nevirapine [11]. When rifampicin and nevirapine are given together there is an observed 31% to 58% decrease in plasma levels of nevirapine due to rifampicin induction effect [12–15]. Available literatures explain that rifampicin combination with efavirenz there is reduction of serum levels of 13-33% [16], however no virological failure reported to be significant [17]. HIV-infected patients achieve somewhat lower concentrations of the orally administered first-line anti-tubercular drugs [18, 19]. The effect of rifampicin on the concentrations of Protease Inhibitors (PI) is well elaborated in a study of Moreno et al. [20].
Immune reconstitution inflammatory syndrome (IRIS), which is due to dysregulated immune recovery [21], occurs in severely immune-suppressed HIV patients normally 1 to 4 weeks after ART initiation [22, 23]. In tuberculosis-related IRIS which is an inflammatory reaction is directed towards mycobacterial antigens [24], resulting in worsening pulmonary infiltrates. Risk factors for TB-IRIS include low baseline CD4 count, high baseline viral load, short duration between TB and ART initiation and disseminated tuberculosis [22, 25], making difficult to determine the optimal time to initiate ART in severely immune-suppressed TB patients [26, 27].
Immune reconstitution is based on the patient's ability to respond to treatment. For the most part, in patients with CD4 counts of 200-350 cells/mm3 who start treatment, their immune systems still have the ability to be activated to produce more CD4 cells [28]. In contrast, in patients with low CD4 counts (< 100 cells/mm3), it may be more difficult to activate their immune systems to produce many CD4 cells because of existing damage from the virus.
In the management of TB/HIV co-infection directly observed therapy and other adherence promoting strategies should be used in all patients with HIV-related TB [29]. Whenever possible, the care for HIV-related TB should be provided by or in consultation with experts in management of both TB and HIV. The care for persons with HIV-related TB should include close attention to the possibility of TB treatment failure, antiretroviral treatment failure, paradoxical reactions, side effects for all drugs used, and drug toxicities associated with increased serum concentrations of rifampicin.
Due to these accompanied complications, selecting an appropriate antiretroviral therapeutic regimen is warranted. This involves addressing multiple interdependent issues, including patient adherence, pharmacokinetic properties of the drugs (including food effects and drug-drug interactions), drug resistance, and overlapping adverse effects. On 12 July 2006 Bristol-Myers Squibb and Gilead Sciences announced that the US Food and Drug Administration (FDA) had cleared AtriplaR, their fixed-dose combination tablet. AtriplaR is a complete regimen in a single, fixed-dose combination tablet that contains: efavirenz 600 mg, emtricitabine 200 mg and tenofovir disoproxil fumarate 300 mg. It is a novel co formulation drugs from two different classes, simplifying administration and increasing adherence too [30].
Testing the hypothesis
A new formulation combining fixed doses of the nucleoside reverse transcriptase inhibitors emtricitabine (200 mg) and tenofovir disoproxil fumarate (tenofovir DF; 300 mg) with the non-nucleoside reverse transcriptase inhibitor efavirenz (600 mg) represents the first once-daily, one-tablet antiretroviral regimen. Co-formulated efavirenz/emtricitabine/tenofovir DF demonstrated excellent potency, tolerability and favorable safety profile [31].
Co administration of co-formulated efavirenz/emtricitabine/tenofovir DF with rifampicin based TB regimen clinical trials is going on in TB/HIV patients of Tanzania, therefore is important to have knowledge of each individual drug. Also a once-daily regimen of efavirenz, emtricitabine and tenofovir DF (administered as individual agents) was superior to once-daily efavirenz plus twice-daily co-formulated lamivudine/zidovudine in terms of virological suppression, immunological recovery and adverse events [32]. Individually, these agents have long half-life that allow for once-daily dosing.
Emtricitabine emtrivaR a cytosine analogue is the newest of the nucleoside reverse transcriptase inhibitor (NRTI) drugs. It was well tolerated in clinical trials where most adverse events were consistent with the NRTI class. Moreover, emtricitabine based regimens were as well tolerated as those with lamivudine [33]. Emtricitabine has no currently known phase I (glucuronidation) or phase II (cytochrome P450 and others) interactions [34]. It may be taken with or without food [35]. Emtricitabine displays dose-proportional pharmacokinetics. Bioavailability is not affected by food intake. Mean steady-state Cmax, Tmax and AUC values were 1.7 mg/L, 2 h, and 10 mg/L.h respectively in 6 patients with HIV infection. Plasma elimination half-life is 8-10 h, but the intracellular half-life of the active compound, emtricitabine-triphosphate is much longer: 39 h which support the once daily dosing.
Tenofovir disoproxil fumarate VireadR is an analogue of adenosine five monophosphate. It is a nucleotide analogue and consequently its mechanism of action differs from that of nucleoside analogues. It is a prodrug, therefore after absorption the drug is hydrolyzed and the active compound tenofovir-diphosphate is released. It has a longer serum half-life than most other NRTIs allowing a once daily dosing. The plasma half-life is 14.4 h, but the intracellular elimination half-life of the active compound, tenofovir-diphosphate is much longer > 49 h.
This drug has broad tissue distribution, aided by its small molecular size and very low protein binding, and is eliminated as unchanged drug in the urine through glomerular filtration and active tubular secretion. Because of this latter characteristic, dosage adjustments are required in patients with renal insufficiency [36]. 70-80% of a dose is recovered unchanged in the urine, suggesting minimal influence of hepatic metabolism. Tenofovir mean steady-state Cmax, Tmax and AUC were 0.33 mg/L, 2.3 h, and 3.0 mg/L.h respectively in patients infected with HIV. Adverse reactions are relatively uncommon, and nausea is the most often reported symptom [37]. The bioavailability of tenofovir disoproxil fumarate is increased in the presence of a high fat diet (40%-50%), and the drug should be taken with food, [38, 39]
Tenofovir disoproxil fumarate is not a substrate, inhibitor, or inducer of the P450 system, within the class of antiretroviral agents, an increase in the bioavailability of didanosine has been described, leading to the recommendation that the dose of didanosine be reduced when used in combination with tenofovir. Tenofovir can be used without adjustments with other nucleoside and nonnucleoside reverse transcriptase inhibitors. Equally, tenofovir seems to have no effect on the pharmacokinetics of protease inhibitors although these latter agents may produce a slight increase in the bioavailability of tenofovir, which seems to be of little clinical relevance.
Efavirenz SustivaR is a NNRTI which is principally metabolized by cytochrome P450, more precisely isoenzymes CYP2B6 and CYP3A4. No active metabolites are formed. Efavirenz has a long terminal half-life of 40-55 h after multiple dosing. Neuropsychiatric symptoms are the common side effects observed. Fumaz et al. [40], in a randomized, prospective, two-arm controlled study compared quality of life and neuropsychiatric side effects in patients receiving an efavirenz-containing regimen versus a group whose treatment did not include efavirenz. They found that the group receiving an efavirenz-containing regimen reported a better quality of life, particularly because their regimen was easier. They found, however, that 13% of their patients reported "character change". Meals of normal composition have no appreciable effect on the pharmacokinetics of efavirenz. The bioavailability is increased following a high fat meal. Time to peak plasma concentration is 3-5 h. Steady state concentrations are achieved after 6-7 days. Mean steady state Cmax, Cmin and AUC(0-24 h) were 4.1 mg/L, 1.8 mg/L and 58.1 h*mg/L respectively after multiple dosing of 600 mg efavirenz once daily.
Several pharmacokinetic studies have been conducted showing the interaction of rifampicin with efavirenz. Lopez-Cortez et al. [16] in Spain did on 24 patients with concomitant infections of HIV and tuberculosis. It was nonblinded study where group A (n = 16) received antituberculosis drugs without rifampicin but with added efavirenz 600 mg/day ARV regimen. The patients were then switched to a standard antituberculosis regimen containing rifampicin with efavirenz 600 mg/day (group A1; n = 8) or efavirenz 800 mg/day (group A2; n = 8). The result showed that levels of AUC, Cmax, and Cmin of efavirenz decreased respectively by 24%, 25%, and 22%, after addition of rifampicin to the efavirenz of 600 mg/day group. Significant association of body weight, dose of efavirenz and its pharmacokinetic parameters was observed and the dose increase to 800 mg/day when efavirenz is used with rifampicin was recommended.
Manosuthi et al. [17, 41] conducted a non-blinded randomized clinical trial to Thai patients and they were given rifampicin for more than 1 month with regimen containing efavirenz 600 mg/day (n = 42), or efavirenz 800 mg/day (n = 42). The plasma concentrations of efavirenz were determined for both groups 12 h after drug administration and on day 14. Both groups had 12-h efavirenz concentrations (C12) of same value (median 3.0 mg/L vs 3.3 mg/L); but the upper C12 levels were higher in the group receiving efavirenz at the dosage of 800 mg/day (21.3 mg/L) in comparison with the group on 600 mg/day (12.2 mg/L). The study concluded that efavirenz with a dose of 600 mg/day is adequate for the majority of HIV-infected patients in Thailand (as their body weight is around 50 kg) but more studied should be performed to other ethnic groups. This is in line with a recent study by Orrell [42] which showed that 600 mg dose of efavirenz is adequate.
Another study was conducted aiming at determining the effects of higher body weights and differing ethnicities on exposure to efavirenz. 9 patients with body weights of over 50 kg were enrolled in the study [43]. The patients received an antiretroviral regimen containing efavirenz 800 mg/day and antituberculosis therapy containing rifampicin. Plasma concentrations of efavirenz were monitored for 2 years. All patients had sub-therapeutic trough concentrations of efavirenz (median 11.7 mg/L; range 5.37-19.6 mg/L). The expected therapeutic range of trough concentrations of efavirenz were between 1.2 and 4.0 mg/L. Seven out of the 9 patients with HIV/TB co-infection had toxicity (6 of them black and 1 caucasian). Around 20% of ethnic Black Africans possess homologous G516T alleles versus 3% of Caucasians [44]. This CYP2B6 polymorphism is associated with exposure to higher concentrations of efavirenz.
Existence of a wide variability in efavirenz concentrations among black Africans was observed in the study of Friedland et al. [45]. This study indicated that inter-subject variability in efavirenz concentrations was greater when the drug was administered with rifampicin (coefficient of variation [CV] 157%) compared with the inter-subject variability after discontinuation of rifampicin (58%), with much of consistent intra-subject variation over time (CV 24%). However, Cmin was not significantly different during versus post TB therapy.
Regarding metabolism studies have shown that CYP2B6 genetic polymorphisms influence very much efavirenz elimination [46–48]. CYP2B6 polymorphisms have been associated with altered PK of efavirenz in HIV-infected adults and children [49–51] resulting in a higher efavirenz exposure and an increase in central nervous system side effect [44, 46]. CYP2B6 patients are poor metabolizer of the drug and dose reduction has been proposed to people with this genotype [52, 53]. Of note: is the high prevalence of efavirenz related CYP2B6 polymorphisms in patients of African region which represent the majority of the HIV-infected population in the world [54–58]. This indicates the need for prospective clinical studies to evaluate the utility of dose adjustments in these populations.
Use of efavirenz in children
The use of efavirenz as a component of first-line antiretroviral therapy in adult and children above 3 years has been accepted worldwide [59], however safety and efficacy of efavirenz in children less than 3 years of age has not been performed [60–63] and the data on the efavirenz exposure in mothers and their breastfed infants is also limited [64]
Despite the report that efavirenz is highly effective and well tolerated in the majority of pediatric patients [65], efavirenz plasma concentrations have been reported to be suboptimal in a large proportion of children and adolescents dosed according to current pediatric guidelines [60, 61] Also interindividual variability has been observed in paediatric population [66].
Recently data on population pharmacokinetics (PK) of efavirenz in children predicts sub-therapeutic efavirenz exposure in a significant proportion on children with the currently recommended efavirenz dose [61, 67]. Authors in ARROW study which was done recently in Uganda and Zimbabwe [68] suggested the use of higher paediatric efavirenz doses, as per WHO 2010 recommendations, however they concluded that children with toxic level of efavirenz concentration may be increased. Also efavirenz pharmacokinetics was shown to demonstrate significant age effects with apparent clearance much greater in young infants than older children. High efavirenz dose requirements and pharmacokinetic variability in infants will require additional pharmacokinetic studies to determine appropriate efavirenz dosing strategies. Therefore priorities should be made to access the developmental changes of efavirenz exposure in children and adolescents and application of therapeutic drug monitoring to the settings where the facility is available.
Implication of the hypothesis
HAART regimens have contained very high pill burdens, complex dosing schedules, and specific food requirements. The management of HIV-related tuberculosis disease seems to be complex although the treatment of TB in persons with HIV is essentially the same as for patients without HIV. A major concern in treating TB in HIV-infected persons is the interaction of rifampin with certain antiretroviral agents, PIs and NNRTIs [69, 70]. Rifabutin, which has fewer drug interactions, may be used as an alternative to rifampicin but is expensive and not available in resource limited area.
Pharmacokinetic data which are present indicate that rifampicin can be combined with efavirenz [16, 17].or nevirapine,[14] although for TB/HIV co-infected patients who got 600 mg rifampicin, adverse events were reported to be higher in nevirapine based regimen compared to efavirenz based regimen [71]. Non-boosted PIs cannot be administered with rifampicin because of considerable decreases in plasma concentrations of PIs, which may cause sub-therapeutic concentrations except ritonavir[72, 73]. Ritonavir is a strong inhibitor of CYP3A4 and P-glycoprotein, and when it is low dose is combined with other PIs an important increase in their plasma concentrations is achieved, however this is not a solution as substantial decreases in plasma concentrations of indinavir,[74] lopinavir [75] and atazanavir [76] have been observed when co-administered with rifampicin, even when small doses of ritonavir are given. Another promising PI is saquinavir although in a study of Ribera et al. [77] a decrease of 40%, 35% and 49% in the median saquinavir AUC0-24, Cmax and Ctrough, respectively, were observed.
In vitro study reveals the benefit from the use of combination therapy achieved with Atripla in terms of the emtricitabine and tenofovir intracellular drug concentration [78]. However in this study patients were HIV positive only hence more data are needed from TB/HIV co-infected patient.
HIV fusion inhibitors represent a novel class of antiretroviral drugs and enfuvirtide is the first drug within this class to be approved [79]. When combined with active ARV drugs, different studies reported findings of substantial improvements in virological, immunological and clinical outcomes [80–83]. It has little potential for drug-drug interactions as far as coadministration with TB drugs is concerned [79, 84, 85]. The major limitation of this drug is the twice daily dosing which may interfere with the treatment adherence. Injection-site reactions occurred almost universally in its recipients, although did not necessitate stopping treatment.
Co-formulated atriplaR (emtricitabine/tenofovir/efavirenz) have demonstrated excellent potency, tolerability and favorable safety profile. The drug is now available in most of the limited-resources countries. The drug is given once per day simplifying administration and increasing adherence too, hence may be recommended as a way to jointly treat these two diseases.
Abbreviations
- ARV:
-
Antiretroviral therapy
- CYP:
-
Cytochrome 450 system
- FDA:
-
Food and drug administration
- HAART:
-
Highly active antiretroviral therapy
- HIV:
-
Human immunodeficiency virus
- IRIS:
-
Immune reconstitution inflammatory syndrome
- NNRTIs:
-
Nonnucleoside reverse transcriptase inhibitors
- NRTIs:
-
Nucleoside reverse transcriptase inhibitors
- PIs:
-
Protease inhibitors
- TB:
-
Tuberculosis.
References
Harries AD, Zachariah R, Lawn SD: Providing HIV care for co-infected tuberculosis patients: a perspective from sub-Saharan Africa. Int J Tuberc Lung Dis. 2009, 13: 6-16.
Bowen EF, Rice PS, Cooke NT, Whitfield RJ, Rayner CF: HIV seroprevalence by anonymous testing in patients with Mycobacterium tuberculosis and in tuberculosis contacts. Lancet. 2000, 356: 1488-1489. 10.1016/S0140-6736(00)02876-2.
Msamanga GI, Fawzi WW: The double burden of HIV infection and tuberculosis in sub-Saharan Africa. N Engl J Med. 1997, 337: 849-851. 10.1056/NEJM199709183371210.
Rose AM, Sinka K, Watson JM, Mortimer JY, Charlett A: "An estimate of the contribution of HIV infection to the recent rise in tuberculosis in England and Wales: should all tuberculosis patients be routinely HIV tested?". Thorax. 2002, 57: 442-445. 10.1136/thorax.57.5.442.
Budha Nageshwar, Lee Richard, Meibohm Bernd: Biopharmaceutics, pharmacokinetics pharmacodynamics of antituberculous drugs. Curr Med Chem. 2008, 15 (8):
Updated guidelines for the use of ryfamycins for the treatment of tuberculosis among HIV-infected patients taking protease inhibitors or nonnucleoside reverse transcriptase inhibitors. accessed June 25th 2009, [http://www.cdc.gov/nchstp/tb/tb_hiv_drugs/toc.htm]
Rattan A, et al: Multi-drug-resistant Mycobacterium tuberculosis: molecular perspectives. Emerg Infect Dis. 1998, 4: 195-209. 10.3201/eid0402.980207.
Turner D, Wainberg MA: HIV transmission and primary drug resistance. AIDS REV. 2006, 8: 17-23.
Niemi Mikko, Backman Janne, Fromm Martin, et al: Pharmacokinetic interactions with Rifampicin: clinical relevance. Clin pharmacokinet. 2003, 42: 819-850. 10.2165/00003088-200342090-00003.
Dean GL, Edwards SG, Ives NJ, Matthews G, Fox EF, Navaratne L, Fisher M, Taylor GP, Miller R, Taylor CB, de Ruiter A, Pozniak AL: Treatment of tuberculosis in HIV-infected persons in the era of highly active antiretroviral therapy. AIDS. 2002, 16: 75-83. 10.1097/00002030-200201040-00010.
Pepper DJ, Meintjes GA, McIlleron H, Wilkinson RJ: Combined therapy for tuberculosis and HIV-1: the challenge for drug discovery. Drug Discov Today. 2007, 12: 980-989. 10.1016/j.drudis.2007.08.001.
Robinson , et al: Pharmacokinetic interactions between nevirapine and rifampin. World AIDs conference Geneva Switzerland. 1998
Oliva J, Moreno S, Sanz J, et al: Coadministration of rifampin and nevirapine in HIV-infected patients with TB. AIDS. 2003, 17: 637-638.
Ribera E, Pou L, Lopez RM, et al: Pharmacokinetic interaction between nevirapine and rifampicin in HIV-infected patients with tuberculosis. J Acqui Immune Defic Syndr. 2001, 28: 450-453.
Cohen K, van CG, Boulle A, et al: Effect of rifampicin-based antitubercular Therapy on nevirapine plasma concentrations in South African adults with HIV-associatedtuberculosis. J Antimicrob Chemother. 2008, 61 (2): 389-393.
Lopez-Cortes LF, Ruiz-Valderas R, Viciana P, et al: Pharmacokinetic interactions between efavirenz and rifampicin in HIV-infected patients with tuberculosis. Clin Pharmacokinet. 2002, 41: 681-690. 10.2165/00003088-200241090-00004.
Manosuthi W, Sungkanuparph S, Thakkinstian A, et al: Efavirenz levels and 24-week efficacy in HIV-infected patients with tuberculosis receiving highly active antiretroviral therapy and rifampicin. AIDS. 2005, 19: 1481-1486. 10.1097/01.aids.0000183630.27665.30.
Gurumurthy P, Ramachandran G, Hemanth Kumar AK, et al: Decreased bioavailability of rifampin and other antituberculosis drugs in patients with advanced human immunodefficiency virus disease. Antimicrob Agents chemother. 2004, 48: 4473-4475. 10.1128/AAC.48.11.4473-4475.2004.
McIlleron H, Wash P, Burger A, Norman J, Folb PI, Smith P: Determinants of rifampicin, isoniazid, pyrazinamide, and ethambutol pharmacokinetics in a cohort of tuberculosis patients. Antimicrob Agents Chemother. 2006, 50: 1170-7. 10.1128/AAC.50.4.1170-1177.2006.
Moreno , et al: Antiretroviral therapy in AIDS patients with tuberculosis. AIDs Rev. 2006, 8: 115-124.
French MA, et al: Immune restoration disease after the treatment of immunodeficient HIV-infected patients with highly active antiretroviral therapy. HIV Med. 2000, 1: 107-115. 10.1046/j.1468-1293.2000.00012.x.
Breton G, et al: Determinants of immune reconstitution inflammatory syndrome in HIV Type 1-Infected patients with tuberculosis after initiation of antiretroviral therapy. Clin Infect Dis. 2004, 39: 1709-1712. 10.1086/425742.
Narita M, et al: Paradoxical worsening of tuberculosis following antiretroviral therapy in patients with AIDS. Am J Respir Crit Care Med. 1998, 158: 157-161.
Bourgarit A, et al: Explosion of tuberculin-specific Th1-responses induce immune restoration syndrome in tuberculosis and HIV co-infected patients. AIDS. 2006, F1-F7.
Shelburne SA, et al: Incidence and risk factors for immune reconstitution inflammatory syndrome during highly active antiretroviral therapy. AIDS. 2005, 19: 399-406. 10.1097/01.aids.0000161769.06158.8a.
Dean GL, et al: Treatment of tuberculosis in HIV-infected persons in the era of highly active antiretroviral therapy. AIDS. 2002, 16: 75-83. 10.1097/00002030-200201040-00010.
Burman WJ, et al: Comparative pharmacokinetics and pharmacodynamics of the rifamycin antibacterials. Clin Pharmacokinet. 2001, 40: 327-341. 10.2165/00003088-200140050-00002.
Piacenti FJ: An update and review of antiretroviral therapy. Pharmacotherapy. 2006, 26: 111-1133.
Friedland G, Abdool KS, Abdool KQ, Lalloo U, Jack C, Gandhi N, El Sadr W: Utility of tuberculosis directly observed therapy programs as sites for access to and provision of antiretroviral therapy in resource-limited countries. Clin Infect Dis. 2004, 38 (Suppl 5): S421-S428.
Long MC, King JR, Acosta EP: Pharmacological aspects of new antiretroviral drugs. Curr HIV/AIDS Rep. 2009, 6: 43-57. 10.1007/s11904-009-0007-y.
Coicoechea M, Best B: Efavirenz/emtricitabine/tenofovir disoproxil fumaratefixed dose combination, first line therapy for all. Expert Opin Pharmacotherapy. 2007, 8: 371-382. 10.1517/14656566.8.3.371.
Frampton JE, Croom KF: Efavirenz/emtricitabine/tenofovir disoproxil fumarate: triple combination tablet. Drugs. 2006, 66: 1501-1512. 10.2165/00003495-200666110-00012.
Bang LM, Scott LJ: Emtricitabine: an antiretroviral agent for HIV infection. Drugs. 2003, 63: 241-242.
Saag MS: Emtricitabine, a new antiretroviral agent with activity against HIV-1 and hepatitis B virus. Clin Infect Dis. 2006, 42: 126-131. 10.1086/498348.
Emtriva_ package insert, Gilead Sciences. Foster City. 2004
Droste J, Kearney B, Van Horssen P, Burger D: Lack of clinically relevant drug-drug interaction between tenofovir DF and rifampin in healthy volunteers. 5th International Workshop on clinical pharmacology of HIV therapy. Rome, Italy. April 1-3, 2004. 2004, Abstract 4.11.
Viread_package insert, Gilead Sciences. 2001, Foster City, Calif
Grim SA, Romanelli F: Tenofovir disoproxil fumarate. Ann Pharmacother. 2003, 37: 849-859.
Kearney BP, Flaherty JF, Shah J: Tenofovir disoproxil fumarate: clinical pharmacology and pharmacokinetics. Clin Pharmacokinet. 2004, 43: 595-612. 10.2165/00003088-200443090-00003.
Fumaz CR, Tuldra A, Ferrer MJ, et al: Quality of life, emotional status, and adherence of HIV-1-infected patients treated with efavirenz versus protease inhibitor-containing regimens. J Acquir Immune Defic Syndr. 2002, 29: 244-253.
Manosuthi W, Kiertiburanakul S, Sungkanuparph S, Ruxrungtham K, Vibhagool A, Rattanasiri S, et al: Efavirenz 600 mg/day versus efavirenz 800 mg/day in HIV-infected patients with tuberculosis receiving rifampicin: 48 weeks results. AIDS. 2006, 20: 131-2. 10.1097/01.aids.0000196181.18916.9b.
Orrell C, Cohen K, Conradie F, Zeinecker J, Ive P, Sanne I, Wood R: Efavirenz and rifampicin in the South African context: is there a need to dose-increase efavirenz with concurrent rifampicin therapy?. Antivir Ther. 2011, 16: 527-534. 10.3851/IMP1780.
Brennan-Bonson P, Lyus R, Harrison T, Pakianathan M, Macallan D: Pharmacokinetic interactions between efavirenz and rifampicin in the treatment of HIV and tuberculosis: one size does not fit all. AIDS. 2005, 19: 1541-1543. 10.1097/01.aids.0000183519.45137.a6.
Haas DW, Ribaudo HJ, Kim RB, Tierney C, Wilkinson GR, Gulick RM, et al: Pharmacogenetics of efavirenz and central nervous system side effects:an Adults AIDS Clinical Trial Group Study. AIDS. 2004, 18: 2391-400.
Friedland G, Khoo S, Jack C, Lallo U: Administration of efavirenz (600 mg/day) with rifampicin results in highly variable level but excellent clinical outcomes in patients treated for tuberculosis and HIV. Antimicrob Agents Chemother. 2006, 58: 1299-302. 10.1093/jac/dkl399.
Desta Z, Saussele T, Ward B, et al: Impact of CYP2B6 polymorphism on hepatic efavirenz metabolism in vitro. Pharmacogenomics. 2007, 8 (6): 547-558. 10.2217/14622416.8.6.547.
Ward BA, Gorski JC, Jones DR, et al: The cytochrome P450 2B6 (CYP2B6) is the main catalyst of efavirenz primary and secondary metabolism: implication for HIV/AIDS therapy and utility of efavirenz as a substrate marker of CYP2B6 catalytic activity. J Pharmacol Exp Ther. 2003, 306: 287-300. 10.1124/jpet.103.049601.
Bumpus NN, Kent UM, Hollenberg PF: Metabolism of efavirenz and 8-hydroxyefavirenz by P450 2B6 leads to inactivation by two distinct mechanisms. J Pharmacol Exp Ther. 2006, 318: 345-351. 10.1124/jpet.106.102525.
Tsuchiya K, Gatanaga H, Tachikawa N, et al: Homozygous CYP2B6 *6 (Q172H and K262R) correlates with high plasma efavirenz concentrations in HIV-1 patients treated with standard efavirenz-containing regimens. Biochem Biophys Res Commun. 2004, 319: 1322-1326. 10.1016/j.bbrc.2004.05.116.
Klein K, Lang T, Saussele T, et al: Genetic variability of CYP2B6 in populations of African and Asian origin: allele frequencies, novel functional variants, and possible implications for anti-HIV therapy with efavirenz. Pharmacogenet Genomics. 2005, 15 (12): 861-873. 10.1097/01213011-200512000-00004.
Heine Robter, et al: A pharmacokinetic and pharmacogenetic study of efavirenz in children; dosing guidelines can result in sub-therapeutic concentrations. Antivir Therapy. 2008, 13: 779-787.
Cabrera SE, Santos D, Valverde MP, et al: Influence of the cytochrome P450 2B6 genotype on population pharmacokinetics of efavirenz in human immunodeficiency virus patients. Antimicrob Agents Chemother. 2009, 53: 2791-2798. 10.1128/AAC.01537-08.
Arab-Alameddine M, Di Iulio J, Buclin T, et al: Pharmacogenetics-based population pharmacokinetic analysis of efavirenz in HIV-1-infected individuals. Clin Pharmacol Ther. 2009, 85: 485-494. 10.1038/clpt.2008.271.
Nyakutira C, Roshammar D, Chigutsa E, et al: High prevalence of the CYP2B6 516 G-- > T(*6) variant and effect on the population pharmacokinetics of efavirenz in HIV/AIDS outpatients in Zimbabwe. Eur J Clin Pharmacol. 2008, 64: 357-365. 10.1007/s00228-007-0412-3.
Wang J, Sonnerborg A, Rane A, et al: Identification of a novel specific CYP2B6 allele in Africans causing impaired metabolism of the HIV drug efavirenz. Pharmacogenet Genomics. 2006, 16: 191-198.
Ngaimisi E, Mugusi S, Minzi O, Sasi P, Riedel KD, Suda A, Ueda N, Janabi M, Mugusi F, Haefeli WE, Bertilsson L, Burhenne J, Aklillu E: Effect of rifampicin and CYP2B6 genotype on long-term efavirenz autoinduction and plasma exposure in HIV patients with or without tuberculosis. Clin Pharmacol Ther. 2011, 90: 406-413. 10.1038/clpt.2011.129.
Uttayamakul S, Likanonsakul S, Manosuthi W, Wichukchinda N, Kalambaheti T, Nakayama EE, Shioda T, Khusmith S: Effects of CYP2B6 G516T polymorphisms on plasma efavirenz and nevirapine levels when co-administered with rifampicin in HIV/TB co-infected Thai adults. AIDS Res Ther. 2010, 7: 8-10.1186/1742-6405-7-8.
Kwara A, Lartey M, Sagoe KW, Xexemeku F, Kenu E, Oliver-Commey J, Boima V, Sagoe A, Boamah I, Greenblatt DJ, Court MH: Pharmacokinetics of efavirenz when co-administered with rifampin in TB/HIV co-infected patients: pharmacogenetic effect of CYP2B6 variation. J Clin Pharmacol. 2008, 48: 1032-1040. 10.1177/0091270008321790.
Scherpbier HJ, Bekker V, et al: Once daily highly active antiretroviral therapy for HIV-1 infected children: safety and efficacy of an efavirenz containing regimen. Pediatrics. 2007, 119: 705-715. 10.1542/peds.2006-1367.
von Hentig N, Koenigs C, Elanjikal S, et al: Need for therapeutic drug monitoring in HIV-1 infected children receiving efavirenz doses according to international guidelines. Eur J Med Res. 2006, 11: 377-380.
Ren Y, Nuttall JJ, Egbers C, et al: High prevalence of subtherapeutic plasma concentrations of efavirenz in children. J Acquir Immune Defic Syndr. 2007, 45: 133-136. 10.1097/QAI.0b013e31805c9d52.
Saitoh A, Fletcher CV, Brundage R, et al: Efavirenz pharmacokinetics in HIV-1-infected children are associated with CYP2B6-G516T polymorphism. J Acquir Immune Defic Syndr. 2007, 45: 280-285.
Fletcher CV, Brundage RC, Fenton T, et al: Pharmacokinetics and pharmacodynamics of efavirenz and nelfinavir in HIV-infected children participating in an area-under-the-curve controlled trial. Clin Pharmacol Ther. 2008, 83: 300-306. 10.1038/sj.clpt.6100282.
Schneider S, Peltier A, Gras A, et al: Efavirenz in human breast milk, mothers', and newborns' plasma. J Acquir Immune Defic Syndr. 2008, 48: 450-454. 10.1097/QAI.0b013e31817bbc21.
Teglas JP, Quartier P, Treluyer JM, et al: Tolerance of efavirenz in children. AIDS. 2001, 15: 241-243. 10.1097/00002030-200101260-00014.
Viljoen M, Gous H, Kruger HS, Riddick A, Meyers TM, Rheeders M: Efavirenz plasma concentrations at 1, 3, and 6 months post-antiretroviral therapy initiation in HIV type 1-infected South African children. AIDS Res Hum Retroviruses. 2010, 26: 613-619. 10.1089/aid.2009.0200.
Hirt D, Urien S, Olivier M, et al: Are recommended dose of efavirenz optimal in young West African HIV-infected children? (ANRS 12103). Antimicrob Agents Chemother. 2009, *Important report on suboptimal efavirenz exposure in African children
Fillekes Q, et al: Pediatric under-dosing of efavirenz: a pharmacokinetic study in Uganda. Advance online edition JAIDS. 2011
De Jong BC, Israelski DM, Corbett EL, et al: Clinical management of tuberculosis in the context of HIV infection. Annu Rev Med. 2004, 55: 283-301. 10.1146/annurev.med.55.091902.103753.
Pozniak AL, Miller R, Ormerod LP: The treatment of tuberculosis in HIV-infected persons. AIDS. 1999, 13: 435-45. 10.1097/00002030-199903110-00001.
Manosuthi W, Mankatitharm W, Lueangnivomkul A, et al: Standard dose efavirenz vs standard dose nevirapine in antiretroviral regimens among HIV-1 and tuberculosis co-infected patients who receive rifampicin. HIV Med. 2008, 9: 294-299. 10.1111/j.1468-1293.2008.00563.x.
Pozniak AL, Miller R, Ormerod LP: The treatment of tuberculosis in HIV-infected persons. AIDS. 1999, 13: 435-45. 10.1097/00002030-199903110-00001.
Moreno S, Podzamczer D, Blazquez R, et al: Treatment of tuberculosis in HIV-infected patients: safety and antiretroviral efficacy of the concomitant use of ritonavir and rifampin. AIDS. 2001, 15: 1185-1187. 10.1097/00002030-200106150-00018.
Justesen US, Andersen AB, Klitgaard NA, et al: Pharmacokinetic interaction between rifampin and the combination of indinavir and low-dose ritonavir in HIV-infected patients. Clin Infect Dis. 2004, 38: 426-429. 10.1086/380794.
La Porte CJ, Colbers EP, Bertz R, et al: Pharmacokinetics of adjusted-dose lopinavir-ritonavir combined with rifampin in healthy volunteers. Antimicrob Agents Chemother. 2004, 48: 1553-60. 10.1128/AAC.48.5.1553-1560.2004.
Burger DM, Agarwala S, Child M, et al: Effect of rifampin on steady-state pharmacokinetics of atazanavir with ritonavir in healthy volunteers. Antimicrob Agents Chemother. 2006, 50: 3336-42. 10.1128/AAC.00461-06.
Ribera E, Azuaje C, Lopez RM, et al: Pharmacokinetic interaction between rifampicin and the once-daily combination of saquinavir and low-dose ritonavir in HIV-infected patients with tuberculosis. J Antimicrob Chemother. 2007, 59: 690-697. 10.1093/jac/dkl552.
Bousquet L, Pruvost A, Guvut AC, et al: Combination of tenofovir and emtricitabine plus efavirenz in vitro modulation of ABC transporter and intracellular drug accumulation. Antimicrob agent Chemother. 2009, 53: 896-902. 10.1128/AAC.00733-08.
Hardy H, Skolnik PR: Enfuvirtide, a new fusion inhibitor for therapy of humanimmunodeficiency virus infection. Pharmacotherapy. 2004, 24: 198-211. 10.1592/phco.24.2.198.33141.
Lalezari JP, Henry K, O'Hearn M, Montaner JS, Piliero PJ, Trottier B, et al: Enfuvirtide, an HIV-1 fusion inhibitor, for drug resistant HIV infection in North and South America. N Engl J Med. 2003, 348: 2175-2185. 10.1056/NEJMoa035026.
Lazzarin A, Clotet B, Cooper D, Reyness J, Arasteh K, Nelson M, et al: Efficacy of enfuvirtide in patients infected with drug resistance HIV-1 in Europe and Australia. N Engl J Med. 2003, 348: 2175-2185. 10.1056/NEJMoa035026.
Nelson M, Arasteh K, Clotet B, Cooper DA, Henry K, Katlama C, et al: Durable efficacy of enfuvirtide over 48 weeks in heavily treatment-experienced HIV-1 infected patients in the T-20 versus optimized background regimen only 1 and 2 clinical trials. J Acquir Immune Defic Syndr. 2005, 40: 404-412. 10.1097/01.qai.0000185314.56556.c3.
Youle M, Staszweski S, Clotet B, Arribas JR, Blaxhult A, Carosi G, et al: Concomitant use of an active boosted protease inhibitor with enfuvirtide in treatment-experienced HIV-1 infected individuals: recent data and consensus recommendations. HIV lin trials. 2006, 7: 86-96. 10.1310/2XVK-PBGL-735N-WH72.
Ruxrungtham K, Boyd M, Bellibas SE, et al: Lack of interaction between enfuvirtide and ritonavir or ritonavir-boosted saquinavir in HIV-1-infected patients. J Clin Pharmacol. 2004, 44: 793-803. 10.1177/0091270004266489.
Boyd MA, Zhang X, Dorr A, Ruxrungtham K, et al: Lack of enzyme-inducing effect of rifampicin on the pharmacokinetics of enfuvirtide. J Clin Pharmacol. 2003, 43: 1382-1391. 10.1177/0091270003259220.
Acknowledgements
The authors gratefully acknowledge the Kilimanjaro Clinical Research Institute for Internet facility.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
GK gave an idea based on the fact that a phase II clinical trial is going on in our institute where TB/HIV co-infected patients are given AtriplaR in combination with 4FDC tuberculosis drugs, so knowing the detail of the drug involved is important. HS contributed in writing the manuscript. Both authors read and approved the final manuscript.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Semvua, H.H., Kibiki, G.S. AtriplaR/anti-TB combination in TB/HIV patients. Drug in focus. BMC Res Notes 4, 511 (2011). https://doi.org/10.1186/1756-0500-4-511
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1756-0500-4-511