Abstract
Introduction
Gastric variceal bleeding due to splenic vein thrombosis is a life-threatening situation and is often difficult to manage by endoscopy. In the worst cases, an emergency splenectomy may be required to stop variceal bleeding.
Case presentation
We report the case of a 60-year-old Caucasian woman with bleeding gastric varices secondary to splenic vein thrombosis treated by splenic artery embolization. Successful embolization was performed by depositing coils into the splenic artery resulting in cessation of variceal bleeding. After embolization there was no recurrence of bleeding.
Conclusion
Splenic artery embolization can be an effective and definite treatment for variceal bleeding secondary to splenic vein thrombosis.
Similar content being viewed by others
Introduction
In recent years new endoscopic techniques for the management of active variceal hemorrhage have been introduced [1, 2]. Although advances have been made in the treatment of bleeding varices, bleeding from gastric varices can be a life-threatening situation in patients with portal hypertension [3]. Gastric varices are challenging due to the difficulty of endoscopic approach and high recurrence rate [4]. This high recurrence rate is associated with poor prognosis and decreased survival. The cumulative mortality of gastric varices is as high as around 50% at one year [3, 5]. The optimal treatment of gastric variceal bleeding remains controversial [6, 7]. Different treatment options for gastric variceal bleeding secondary to splenic vein thrombosis have been discussed. Splenectomy was considered the best treatment in the past [8, 9]. Recently, splenic artery embolization has been suggested to be an effective method for the treatment of bleeding from gastric varices and portal hypertension [10].
This case report concerns a 60-year-old Caucasian woman with bleeding gastric varices secondary to splenic vein thrombosis treated by partial splenic artery embolization.
Case presentation
A 60-year-old Caucasian woman was admitted to our hospital because of severe upper gastrointestinal bleeding. An endoscopy was performed, revealing bleeding from gastric varices in the subcardial region. Due to the large variceal size, endoscopic therapy with variceal ligation could not be performed. She was transferred to our intensive care unit (ICU).
She had a history of similar episode of massive gastrointestinal bleeding from gastric varices six years previously. Evaluation at that time with liver function tests, portal venous flow and magnetic resonance angiography did not reveal an identifiable cause.
On admission to the ICU our patient initially showed no signs of hypovolemic shock. Laboratory results again did not indicate impaired liver function. Esophagogastroduodenoscopy again revealed bleeding from subcardial gastric varices in the absence of evidence of esophageal varices (Figure 1).
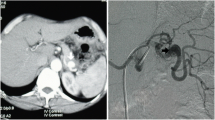
Endoscopic treatment with histoacryl glue only resulted in a temporary reduction of the bleeding. To reduce the portal venous pressure the vasopressin analog terlipressin was administered. Despite this therapy, there was another severe episode of upper gastrointestinal bleeding with signs of shock. In all, 10 units of red blood cell concentrate and four units of fresh frozen plasma were transfused. Sufficient endoscopic therapy could not be achieved. An abdominal sonograph showed she had an enlarged spleen (15.9 × 5.4 cm; liver size and structure were normal, with normal flow in the portal vein). A computed tomography (CT) scan showed total occlusion of the splenic vein. Despite the limited data on urgent splenic artery embolization, she was subsequently referred for interventional radiological procedures. A successful splenic artery embolization was performed via the transcatheter approach, depositing coils into the splenic artery resulting in immediate cessation of variceal bleeding (Figure 2).
No recurrence of bleeding was noted post-embolization. After embolization, our patient complained of mild left upper abdominal discomfort, which was effectively relieved by routine analgesics.
At two weeks after admission our patient was fully recovered and was released from our department. There were no further bleeding complications for 18 months. Follow-up endoscopy was performed two months and eight months after the intervention, showing only mild gastric varices without signs of bleeding.
Conclusions
Our case illustrates that splenic artery embolization can be a quick and effective method of controlling gastric variceal bleeding in patients with portal hypertension associated with splenic vein thrombosis. Splenic artery embolization results in a restriction of blood flow to the spleen and a reduction of transmural pressure and size of gastric varices.
Splenic embolization has the advantage of being a non-operative intervention that can be performed under local anesthesia. Splenic artery embolization has been shown to be an effective alternative to splenectomy with reduced morbidity and mortality [11]. Post-embolization syndrome is the most common side effect of splenic artery embolization [12]. It is a self-limiting, benign phenomenon that usually consists of left abdominal pain, fever, malaise, and gastrointestinal symptoms. Serious complications of this therapeutic method, such as splenic abscess and septicemia, are very rare [13].
In summary, splenic artery embolization can be a quick and effective method of controlling gastric variceal bleeding in patients with portal hypertension associated with splenic vein thrombosis.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
Tripathi D, Hayes PC: Endoscopic therapy for bleeding gastric varices: to clot or glue?. Gastrointest Endosc. 2008, 68: 883-886. 10.1016/j.gie.2008.04.040.
Liu J, Petersen BT, Tierney WM, Chuttani R, Disario JA, Coffie JM, Mishkin DS, Shah RJ, Somogyi L, Song LM: Endoscopic banding devices. Gastrointest Endosc. 2008, 68: 217-221. 10.1016/j.gie.2008.03.1121.
McCormick PA, O'Keefe C: Improving prognosis following a first variceal haemorrhage over four decades. Gut. 2001, 49: 682-685. 10.1136/gut.49.5.682.
Bendtsen F, Krag A, Moller S: Treatment of acute variceal bleeding. Dig Liver Dis. 2008, 40: 328-336. 10.1016/j.dld.2007.12.005.
Kim T, Shijo H, Kokawa H, Tokumitsu H, Kubara K, Ota K, Akiyoshi N, Iida T, Yokoyama M, Okumura M: Risk factors for hemorrhage from gastric fundal varices. Hepatology. 1997, 25: 307-312. 10.1002/hep.510250209.
Ryan BM, Stockbrugger RW, Ryan JM: A pathophysiologic, gastroenterologic, and radiologic approach to the management of gastric varices. Gastroenterology. 2004, 126: 1175-1189. 10.1053/j.gastro.2004.01.058.
Spaander MC, Murad SD, van Buuren HR, Hansen BE, Kuipers EJ, Janssen HL: Endoscopic treatment of esophagogastric variceal bleeding in patients with noncirrhotic extrahepatic portal vein thrombosis: a long-term follow-up study. Gastrointest Endosc. 2008, 67: 821-827. 10.1016/j.gie.2007.08.023.
Bernades P, Baetz A, Levy P, Belghiti J, Menu Y, Fekete F: Splenic and portal venous obstruction in chronic pancreatitis. A prospective longitudinal study of a medical-surgical series of 266 patients. Dig Dis Sci. 1992, 37: 340-346. 10.1007/BF01307725.
Evans GR, Yellin AE, Weaver FA, Stain SC: Sinistral (left-sided) portal hypertension. Am Surg. 1990, 56: 758-763.
Covarelli P, Badolato M, Boselli C, Noya G, Cristofani R, Mosca S, Tei F: Splenic vein thrombosis complicated by massive gastric bleeding: treatment with arterious embolization. Am Surg. 2008, 74: 184-186.
Shah R, Mahour GH, Ford EG, Stanley P: Partial splenic embolization. An effective alternative to splenectomy for hypersplenism. Am Surg. 1990, 56: 774-777.
Tajiri T, Onda M, Yoshida H, Mamada Y, Taniai N, Kumazaki T: Long-term hematological and biochemical effects of partial splenic embolization in hepatic cirrhosis. Hepatogastroenterology. 2002, 49: 1445-1448.
Sakai T, Shiraki K, Inoue H, Sugimoto K, Ohmori S, Murata K, Takase K, Nakano T: Complications of partial splenic embolization in cirrhotic patients. Dig Dis Sci. 2002, 47: 388-391. 10.1023/A:1013786509418.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
BS wrote the case report. JG was the physician who performed embolization. VP wrote the case report. RMS wrote the case report and gave final approval. WH wrote the case report, was the physician in charge of the ICU and performed the endoscopy. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Saugel, B., Gaa, J., Phillip, V. et al. Splenic artery embolization in a woman with bleeding gastric varices and splenic vein thrombosis: a case report. J Med Case Reports 4, 247 (2010). https://doi.org/10.1186/1752-1947-4-247
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1752-1947-4-247