Abstract
Background
Objectives of the study were to document the impact of some management factors on the occurrence of clinical mastitis in primiparous dairy cows and to identify common udder pathogens of clinical mastitis in freshly calved heifers and multiparous cows on the day of calving.
Methods
A one-year study was conducted during 2004 and 2005 in 11 selected Estonian dairy herds. Data consisted of 68 heifers with clinical mastitis and 995 heifers without clinical mastitis on the day of calving. Multivariable logistic regression with a random herd effect was used to investigate any association between housing system or the time interval from movement of heifers to the calving facility and day of calving on occurrence of clinical mastitis. Milk samples for bacteriological analysis were collected from affected heifers and multiparous cows on the day of calving
Results
Clinical mastitis occurrence in the study population of freshly calved heifers equalled 6.1 %. Housing system was not a significant risk factor for clinical mastitis of freshly calved heifers.
Moving heifers to the cowbarn less than two weeks before calving in tiestall farms increased risk (OR = 5.9 p = 0.001) for clinical mastitis at parturition. The most frequently isolated udder pathogens among heifers were Escherichia coli (22.1%), Streptococcus uberis (19.1%) and coagulase-negative staphylococci (8.8%). In comparison, the main pathogen in multiparous cows with clinical mastitis at parturition was Staphylococcus aureus (11.2%).
Conclusion
Moving heifers to the calving facilities too late in tiestall farms increased risk for clinical mastitis at parturition. The isolated udder pathogens did not differ significantly in tiestall farms compared to freestall farms in heifers, but differences were found between heifers and multiparous cows at parturition.
Similar content being viewed by others
Background
Mastitis is an economically important disease for dairy cattle production worldwide. Although replacement heifers are generally expected to have good udder health, many studies have identified a high risk of their developing subclinical mastitis during early lactation and reported that the prevalence of intramammary infections (IMI) is high in the peripartum period [1–7], mainly depending on infectious species [8]. At the same time, published reports on clinical mastitis incidence in freshly calved heifers are scarce and controversial. A nested case-control study in Norway showed that 5 % (6,410 out of 128,027) cases of clinical mastitis was treated in first calving heifers [9]. In Finland, the frequency of treatments for heifer mastitis from one week before to one week after calving was 3.9% for Ayrshires and 5.6% for Frisians [10]. In a study conducted in Netherlands the rate of clinical mastitis around parturition was found to be higher in heifers (>30%) compared to older cows (13%) [11].
Coagulase negative staphylococci (CNS), Streptococcus dysgalactiae (Str. dysgalactiae) and coliforms have been the most commonly identified pathogens of clinical mastitis during the periparturient period in heifers [12, 13]. However, in the studies conducted in Norway, Staphylococcus aureus (S. aureus) was the most frequently isolated micro-organism, followed by Str. dysgalacatiae and CNS [14]. At the same time, differences have been found in occurrence of staphylococcal mastitis between primiparous and multiparous cows, where CNS was more prevalent among cows and S. aureus in freshly calved heifers [15]. Some studies have suggested that udder pathogens found in heifers close to parturition are similar to mammary pathogens found in lactating cows [1, 12]. On the other hand, the risk of S. aureus IMI was influenced by the amount of time the heifers were housed with older cows and by the proportion of S. aureus- infected cows in the herd [16]. In Estonia, the most common pathogens of clinical mastitis are S. aureus (20.5% of isolated bacteria), CNS (11%), Streptococcus agalactiae (Str. agalactiae) (10.7%) and Streptococcus uberis (Str. uberis) (10.5%) [17]. No data are available on udder health in freshly calved heifers and multiparous cows in Estonia, although clinical mastitis has frequently been observed at parturition. Management factors at the herd level, including housing, feeding and milking systems, affect the incidence of clinical mastitis [18–21]; whereas at the individual cow level, milk leakage, teat and udder oedema and blood in the milk are associated with mastitis incidence [22]. Both types of associations are dependent upon species of udder pathogens that are present [23]. The transition phase, typically defined as the period from 3 weeks before to 3 weeks after parturition, is viewed as a critical time in the lactation cycle of a dairy cow. During this period, the cow experiences a series of nutritional, physiological and social changes which render her more vulnerable to infectious and metabolic diseases [24].
The aims of this study were:
-
1)
to study whether mastitis occurrence in first calving heifers differs between farms with different housing systems and whether it is affected by the time interval between movement of heifers to their calving facility and their day of calving.
-
2)
to identify common udder pathogens of clinical mastitis in first-calving heifers and multiparous cows on the day of calving in Estonia
Methods
Study population and experimental design
The one year study was carried out during 2004 and 2005. Eleven large-scale Estonian dairy herds was used in this study. These herds were selected from among the herds who received regular herd health visits by the university large animal clinic (in total 25 herds). The herds having more than 100 cows and 50 replacement heifers calving per year were included into the study. In Table 1, the main characteristics of the selected herds are presented. All heifers that calved during the observation period (n = 1,063) were eligible for inclusion. Heifers with clinical mastitis on the day of calving were included as cases (n = 68), and the remaining freshly calved heifers (n = 995) were controls. Heifers on each farm were moved from their rearing facility to the milking farm according to the availability of space. The number of days between the day of transfer of the heifer to the cowshed and the day of calving was recorded.
Data collection in cases of clinical mastitis
Local trained veterinarians collected milk samples during the first milking from all freshly calved heifers and multiparous cows on the day of calving. If milk from a quarter had abnormal viscosity (watery, thicker than normal), color(yellow, blood-tinged) or consistency(flakes or clots), clinical mastitis was diagnosed, and samples from diseased udder quaters were collected for bacteriological examination [25]. Before collection, the teat end was cleaned with 70%-ethanol swabs and allowed to dry. After discarding a few streams of milk, samples (2 to 4 ml) were collected into sterile 10 ml plastic tubes, either frozen at -20°C or cooled to +4°C and transported to the Estonian Veterinary and Food Laboratory. All bacteriological examinations of milk samples were performed according to the standards of the National Mastitis Council [26].
Data analysis
Logistic regression with a random herd effect for controlling clustering was used to analyze the effect of housing system (freestall, tiestall with short stall-length or tiestall with long stall-length) and length of time before calving that the heifers had been moved to the calving facility on the occurrence of clinical mastitis. To simplify the modelling, the continuous variable, number of days from moving heifers to the calving facility and expected parturition, was transformed to a dichotomous variable (≤14 days vs. >14 days classes) in the model. Odds ratios (OR) with a 95% confidence interval (95% CI) were calculated. Statistical significance was assumed at p ≤ 0.005. These analyses were conducted using Stata 9.2 [27]. A two-sample proportion test was used to estimate statistical significance of differences in occurrence of udder pathogens between first-calving heifers and multiparous cows. These analyses were conducted using statistical software Statistix for Windows 2.0.
Results
Approximately 40% (423) of the first-calving heifers were in tiestall farms and approximately 60% (640) were in freestall farms. The overall occurrence of clinical mastitis at calving of the heifers was 6.4% (n = 68), being 9.7% (n = 41) in tiestall farms compared with 4.1 % (n = 27) in freestall farms. The range of days from moving heifers to the calving facility and expected parturition were from 0 to76, where the median day was 26. The results of logistic regression analysis are shown in Table 2. Housing system only was not a significant risk factor for clinical mastitis of freshly calved heifers. In tiestall farms heifers moved to the calving facility less than two weeks before expected parturition had a higher risk (OR = 5.9 p = 0.001) to develop clinical mastitis at calving than heifers moved more than 14 days before calving.
In total, 303 clinical mastitis cases were identified on the day of parturition in 2,355 multiparous cows (12.8%). Udder pathogens were isolated from 49 (72%) out of 68 cases of clinical mastitis in freshly calved heifers and from 185 (61%) out of 303 cases in multiparous cows.
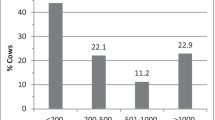
Bacteriological findings are shown in Table 3. The most frequently isolated bacteria from milk samples of freshly calved heifers were E.coli and Str. uberis. No clinical mastitis caused by Str. agalactiae or Corynebacterium spp. was discovered, and only one case of S. aureus mastitis was found in heifers. In contrast, S. aureus was the most common bacterium isolated from milk of affected multiparous cows, followed by Str. uberis and Escherichia coli(E. coli). Occurrence differences between heifers and cows were statistically significant for Str. uberis (p = 0.037), coliforms (p = 0.0002) and S. aureus (p = 0.019).
Figure 1 shows the distribution in tiestall vs. freestall housing systems of udder pathogens isolated from quarter milk samples with clinical mastitis in freshly calved heifers.
In tiestall herds, 36.6% (n = 15) of the samples were bacteriologically negative or mixed cultures, while the corresponding proportion in freestall herds was 14.8% (n = 4). The most common udder pathogens in both housing systems were Str. uberis, E. coli and CNS. Occurrence of colimastitis was higher in freestall farms than in tiestall farms, but Str. uberis was more frequent in tiestall farms than freestall farms. The differences were not statistically significant.
Discussion
In 11 large herds using traditional Estonian dairy management, two housing systems did not differ significantly in clinical mastitis occurrence of first-calving heifers. Others, however, have reported higher incidence of clinical mastitis in tiestall than in freestall housing [21, 28–30]. In tiestall farms, the main risk factors for clinical mastitis are teat injuries, short stalls and shortage of bedding material [31, 32], especially during the periparturient period [33]. In one Swedish report, the incidence of clinical mastitis decreased across 18 months, after the management system was changed from the tiestall to the freestall system [34]. We did identify an association at the tie-stall farms between time of movement of close-to-term heifers to the milking farm and the occurrence of clinical mastitis. Stress and sudden changes in environmental and management conditions during the peripartum period could weaken natural defence mechanisms in animals, making them more susceptible to clinical mastitis. In tiestall systems, an increased frequency of lying down and rising may lead to increased risk of teat tramping, leading to increased clinical mastitis incidence [35]. Contrarily, in loose-housing systems, cows have sufficient space for lying down and standing up in a more natural way during parturition. The results of the present study reflect the situation in large commercial dairy herds in Estonia. However, the number of herds in the study was limited and because sample sizes were small in some herds, these results should be interpreted with caution. A larger study of longer duration and with more herds is needed for more reliable conclusions.
In the relatively few reports on clinical mastitis in heifers, occurrence of clinical mastitis has been variable. In Finnish studies by Myllys [10], the treatment of clinical mastitis in heifers from one week before through one week after calving increased from 1.8% to 4.4% between 1983 and 1991. In the USA, the incidence of clinical mastitis in heifers was 12.3%, and mostly coliforms and streptococci were isolated [36]. In 1,040 heifers, 1361 clinically affected quarters were found in a large-scale Norwegian study [14]. As to the present investigation, the occurrence of clinical mastitis in freshly calved heifers was a modest 6.1%.
Environmental bacteria dominated in our study. Mainly E.coli (22.1%), Str.uberis (19.1%) and CNS (9.2%) were isolated in cases of clinical mastitis of the freshly calved heifers. Similar results have been reported by others, in which common bacteria isolated after parturition were CNS, coliforms and streptococci [12, 13, 36].
In a Danish study, the most frequently isolated organism was S. aureus [14]. Our investigation did not show S. aureus clinical mastitis in freshly calved heifers, although S. aureus was the main pathogen among the multiparous cows. Despite that, the spread of this infection should not be underestimated. Comparing tiestall and freestall farms, the bacterial findings on the day of parturition were generally the same. Coliform infection was more common among loose-housed heifers, where the primary source of infection is bovine faeces and where the secondary multiplication of bacteria to high numbers in bedding and manure is often a risk factor [38]. Prevalence of Str. uberis infections depends on udder and calving hygiene, but immune response in the lower udder gland also plays an important role [37]. That might explain the higher prevalence of clinical mastitis in heifers. Altough more CNS infections were found in tiestall farms, we could not draw clear conclusions due to the small number of samples. Our findings confirmed that S. aureus could be the main pathogen causing mastitis in multiparous cows at the time of parturition in Estonia. The importance of environmental bacteria may increase if management systems evolve towards higher intensity of production.
Conclusion
Moving heifers to the calving fascilities too late in tiestall farms, increased risk for clinical mastitis at parturition. The isolated udder pathogens did not differ significantly in tiestall farms compared to freestall farms in heifers, but differences were found between heifers and multiparous cows at parturition.
References
Oliver S, Mitchell BA: Intramammary infection in primigravid heifers near parturition. J Dairy Sci. 1983, 66: 1180-
Trinidad P, Nickerson SC, Alley TK: Prevalence of intramammary infection and teat canal colonisation in unbred and primigravid dairy heifers. J Dairy Sci. 1990, 73: 107-
Pankey JW, Drechsler PA, Wildeman EE: Mastitis prevalence in primigravid heifers at parturition. J Dairy Sci. 1991, 74: 1550-1552.
Oliver SP, Lewis MJ, Gillespie BE, Dowlen HH: Influence of prepartum antibiotic therapy on intramammary infections in primigravid heifers during early lactation. J Dairy Sci. 1992, 75: 406-408.
Roberson JR, Fox LG, Hancock DD, Gay CC, Besser TE: Coagulase-positive Staphylococcus intramammary infections in primiparous dairy cows. J Dairy Sci. 1994, 77: 958-969.
Nickerson SC, Owens E, Boddie RL: Symposium: mastitis in dairy heifers. Mastitis in dairy heifers: initial studies on prevalence and control. J Dairy Sci. 1995, 78: 1607-167.
De Vliegher S, Barkema HW, Stryhn H, Opsomer G, De Kruif A: Impact of early lactation somatic cell count in heifers on milk yield over the first lactation. J Dairy Sci. 2005, 88: 938-947.
Aarestrup FM, Jensen NE: Prevalence and duration of intramammary infection in Danish heifers during the peripartum period. J Dairy Sci. 1997, 80: 307-312.
Waage S, Sviland S, Ødegaard SA: Identification of risk factors for clinical mastitis in dairy heifers. J Dairy Sci. 1998, 81: 1275-1284.
Myllys V, Rautala H: Characterization of clinical mastitis in primiparous heifers. J Dairy Sci. 1995, 78: 538-545.
Barkema HW, Schukken YH, Lam TJ, Beiober GM, Wilmink ML, Benedictus G, Brand A: Incidence of clinical mastitis in dairy herds grouped in three catergories by bulk milk somatic cell counts. J Dairy Sci. 1998, 81: 411-419.
Jonsson P, Olsson SO, Olofson AS, Fätlh C, Holmberg O, Funke H: Bacteriological investigation of clinical mastitis in heifers in Sweden. J Dairy Research. 1991, 58: 179-
Myllys V: Staphylocci in heifer mastitis before and after parturition. J Dairy Sci. 1995, 62: 51-60.
Waage S, Mørk T, Røros A, Aasland D, Hunshamar A, Ødegaard SA: Bacteria associated with clinical mastitis in dairy heifers. J Dairy Sci. 1999, 82: 712-719.
Matthews KR, Harmon RJ, Langlois BE: Prevalence of Staphylococcus species during the periparturient period in primiparous and multiparous cows. J Dairy Sci. 1992, 75: 1835-1837.
Bassel L, Kelton D, Godkin A, Leslie K, Lissemore K: Risk factors for intramammary infection at first calving in Ontario dairy heifers. Proceedings of the 36th Ann Conv. AABP, Columbus, Ohio, United States of America. 2003, 177-178.
Estonian Veterinary and Food Laboratory: Annual report. Tartu. 2004
Aland A: Lüpsikarja tervise seiremudel ning selle rakendamine loomade tervise hindamisel ja parandamisel. PhD thesis. Estonian Agricultural University, Tartu. 2003
Schukken YH, Grommers FJ, Van de Geer D, Erb HN, Brand A: Risk factors for clinical mastitis with a low bulk milk somatic cell count: I. Data and risk factors in all cases. J Dairy Sci. 1990, 73: 3463-3471.
Barkema HW, Van der Ploeg JD, Schukken YH, Lam TJ, Benedictus G, Brand A: Management style and its association with bulk milk somatic cell count and incidence rate of clinical mastitis. J Dairy Sci. 1999, 82: 1655-1663.
Valde JP, Hird DW, Thurmond MC, Österås O: Comparison of ketosis, clinical mastitis, somatic cell count, and reproductive performance between free stall and tie stall barns in Norwegian dairy herds with automatic feeding. Acta Vet Scan. 1997, 38: 181-192.
Waage S: Case -control study of risk factor for clinical mastitis in postpartum dairy heifers. J Dairy Sci. 2001, 84: 392-399.
Barkema HW, Shaken YH, Lam TJ, Briber GM, Benedict's G, Brand A: Management practices associated with the incidence rate of clinical mastitis. J Dairy Sci. 1999, 82: 1643-1654.
Goff JP, Horts RL: Physiological changes at parturition and their relationship to metabolic disorders. J Dairy Sci. 1997, 80: 1260-1268.
Bulletin of the International Dairy Federation. No.217. Brussels. 1987
Hogan JS, Gonzales RN, Harmon RJ, Nickerson SC, Oliver SP, Smith KL: Laboratory Handbook on Bovine Mastitis. National Mastitis Council Inc, Madison, WI. 1987
Stata 9.2. 2005 Stata® Statacorp LP, College Station, USA.
Ekesbo I: Disease incidence in tied and loose housed dairy cattle. Acta Agric Scan. 1966, Thesis, Suppl 15
Matzke P, Holzer A, Deneke J: The effect of enviromental factors on the occurence of udder diseases. Tierartztliche Praxis. 1992, 20: 21-23.
Bakken G, Røn I, Østerås O: Clinical disease in dairy cows in relation to housing systems. In the Proceedings of the 6th Int Congr Anim Hygiene Sweden, Skara. 1988, 18-
Koskiniemi K: Observation on the incidence of teat injuries in different cowshed. Nordisk Veterinaermedicin. 1982, 34: 13-19.
Bendixen PH, Wilson B, Ekesbo I: Disease frequencies in dairy cows in Sweden. V. Tramped teat. Preventive Veterinary Medicine. 1988, 6: 17-25. 10.1016/0167-5877(88)90022-0.
Elbers ARW, Miltenburg JD, De Lange, De Crauwels APP, Barkema HW, Shukken YH: Risk factors for clinical mastitis in a random sample of dairy herds from the southern part of the Netherlands. J Dairy Sci. 1997, 87: 3358-3374.
Hultgren J: Foot/leg and udder health in relation to housing changes in Swedish dairy herds. Preventive Veterinary Medicine. 2002, 53: 167-189. 10.1016/S0167-5877(01)00279-3.
Oltenacu PA, Bendixen PH, Vilson B, Eksebo I: Tramped teats-clinical mastitis disease complex in tied cows. Enviromental risk factors and interrelationships with other diseases. Acta Vet Scan. 1990, 31: 471-478.
Gröhn YT, Wilson DJ, González RN, Hertl JA, Schulte H, Bennett G, Schukken YH: Effect of pathogen-specific clinical mastitis on milk yield in dairy cows. J Dairy Sci. 2004, 87: 3358-3374.
Andrews AH, Blowey RW, Boyd H, Eddy RG: Bovine Medicine. Diseases and Husbandry of Cattle. 2004, Blackwell Science Ltd, Second
Acknowledgements
The authors are grateful to Estonian State Veterinary Laboratory. This study was financially supported by Estonian Ministry of Agriculture and Estonian Science Foundation (ETF) grant no 5733.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
PK carried out the study, compiled the results and drafted the manuscript. AV participated in the designing the study and analysis of the data. BA coordinated data collection, and KK coordinated the study. All authors were significantly involved in designing the study, intepreting of data and composing the manuscript.
Piret Kalmus, Arvo Viltrop, Birgit Aasmäe and Kalle Kask contributed equally to this work.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Kalmus, P., Viltrop, A., Aasmäe, B. et al. Occurrence of clinical mastitis in primiparous Estonian dairy cows in different housing conditions. Acta Vet Scand 48, 21 (2006). https://doi.org/10.1186/1751-0147-48-21
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1751-0147-48-21