Abstract
Background
Apigenin (4′,5,7-trihydroxyflavone, AP), an active component of many medicinal Chinese herbs, exhibits anticancer properties in vitro and in vivo. This study aims to investigate the genotoxic, cytostatic, and cytotoxic effects of AP and time course changes in the levels of anti- and pro-apoptotic proteins involved in the DNA damage response in HepG2 cells.
Methods
The genotoxic potential of AP was determined by sister chromatid exchanges (SCEs) and chromosomal aberrations (CAs) analysis. The levels of cytostaticity and cytotoxicity were evaluated by the proliferation rate and mitotic indices, respectively. MTT was used to study cytotoxicity, while the induction of apoptosis and the expression of apoptosis-related proteins were determined by ELISA.
Results
At concentrations greater than 10 μM, AP decreased cell survival in a dose- (48 h: 10 vs. 20 μΜ, P < 0.001 and 20 vs. 50 μΜ, P = 0.005; 72 h: 10 vs. 20 μΜ, P < 0.001 and 20 vs. 50 μΜ, P = 0.001) and time-dependent manner (20 μΜ: 24 vs. 48 h, P < 0.001 and 48 vs. 72 h, P = 0.003; 50 μΜ: 24 vs. 48 h, P < 0.001 and 48 vs. 72 h, P < 0.001; 100 μΜ: 24 vs. 48 h, P < 0.001 and 48 vs. 72 h, P < 0.001). SCEs rates, cell proliferation, and mitotic divisions were also affected in a dose-dependent manner (P < 0.001). There was no change in the frequency of aberrant cells (1 μΜ ΑP: P = 0.554; 10 μM AP: P = 0.337; 20 μΜ AP: P = 0.239). Bcl-2 levels were reduced 3 h after AP administration (P = 0.003) and remained reduced throughout the 48 h observation period (6 h, P = 0.044; 12 h, P = 0.001; 24 h, P = 0.042; 48 h, P = 0.012). Bax and soluble Fas exhibited a transient upregulation 24 h after AP treatment. The Bax/Bcl-2 ratio was also increased at 12 h and remained increased throughout the 48 h observation period.
Conclusion
AP exhibited dose-dependent genotoxic potential in HepG2 cells. The protein levels of sFas, Bcl-2, and Bax were affected by AP to promote cell survival and cell death, respectively.
Similar content being viewed by others
Background
Complementary and alternative medicine has potential to provide new drugs for cancer treatment [1–3]. Plant-derived anticancer agents have already been used in the clinical practice, while many synthetic chemotherapeutics are analogs of natural products [3]. Apigenin (AP) is a bioflavone found in many Chinese medicinal herbs, such as Wedelia chinensis, Ixeris chinensis, Apium graveolens var. dulce, Scutellaria barbata, Andrographis paniculata, Chrysanthemum morifolium, and Ginkgo biloba[1, 4–10]. In vitro and in vivo studies have demonstrated that AP possesses antioxidant [11, 12], anti-inflammatory [13], and anticancer [14–16] properties, inhibiting tumor growth and inducing cell cycle arrest and apoptosis [17–20]. The anticancer properties of AP are associated with its pro-oxidant activity, with concentrations depending upon cell type [21–23]. AP promoted oxidative stress at 15 μΜ in human cervical carcinoma HeLa cells [21], at 50 μΜ in human promyelocytic leukemia HL-60 cells [22], and at 25 μΜ in Chang liver cells [23].
AP induced apoptosis in the hepatic parenchyma [24–29], and exhibited antiproliferative and apoptotic properties in HepG2, Hep3B and PLC/PRF/5 human liver cancer cell lines [25–28]. Its antiproliferative and apoptotic effects might be mediated through a p53-dependent pathway by p53 accumulation, induction of p21 expression, and downregulation of CDK4 expression [25, 29]. Generation of reactive oxygen species (ROS) might also play an important role in AP-induced apoptosis by transcriptionally downregulating catalase activity and increasing hydrogen peroxide levels [27, 28]. Cell death induction has also been associated with Bax/Bcl-2 ratio changes, cytochrome c release, and Apaf-1 induction, leading to caspase activation and PARP-cleavage in leukemia, prostate carcinoma, lung cancer, and cervical carcinoma cells [19, 30–33].
Although the properties of AP against various pro-oxidant and clastogenic agents have been studied [11, 34–36], there is little information on the genotoxic potential of this particular flavonoid. AP was highly clastogenic in Chinese hamster V79 cells and induced micronuclei formation in human peripheral lymphocytes in a dose-dependent manner [37, 38]. Other reports mentioned that AP could intercalate into both calf thymus DNA and RNA [39, 40]. The generation of DNA single-strand (SSBs) and double-strand breaks (DSBs) by DNA-crosslinking agents [41, 42], could lead to sister chromatid exchanges (SCEs) or chromosomal aberrations (CAs) [43]. An in vivo and in vitro study demonstrated that AP can remodel chromatin by inhibiting class I histone deacetylases. This affects regulation, expression, and activation of various DNA damage response genes, which results in cell cycle arrest, and apoptosis. These affected genes include ATM and ATR, which participate in DSBs repair via homologous recombination [44, 45].
The SCEs assay is a sensitive, simple, and rapid method to detect DNA damage and repair at low concentrations of potential genotoxic or anti-genotoxic agents [43, 46–49]. SCEs represent a useful tool in monitoring and improving chemotherapeutic strategies in vitro and in vivo[48, 50–54]. The efficacy of potential antitumor agents in inducing SCEs formation in vitro and in vivo correlates positively with the in vivo tumor’s response to these agents [55, 56]. CAs analysis is another genotoxic endpoint [43, 46]. A high frequency of CAs can lead to cell death, and it has been associated with increased overall cancer risk [43, 46, 57, 58].
AP’s ability to intercalate into DNA, remodel chromatin, and upregulate p53 and p21 proteins [25, 39, 40, 44, 59–61] directed us to study the genotoxic potential of this flavonoid in HepG2 cells. We also investigated the proliferation rate index (PRI) and the mitotic index (MI), markers of the cytostatic and cytotoxic properties of chemical and physical agents, respectively [49]. The time course changes in the levels of anti- and pro-apoptotic proteins involved in the DNA damage response were also investigated.
Methods
Chemicals
Apigenin (4′,5,7-trihydroxyflavone) was purchased from Calbiochem (San Diego, CA, USA). Bovine serum albumin, Bradford reagent, dimethyl sulfoxide (DMSO), and 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT) were purchased from Sigma (St. Louis, MO, USA). 5-bromodeoxyuridine and bisbenzimide H33258 were purchased from AppliChem (Darmstadt, Germany). High glucose Dulbecco’s modified Eagle’s medium (DMEM), trypsin-EDTA solution, colcemid, fetal bovine serum (FBS), and penicillin/streptomycin solution (10,000:10,000) were purchased from GIBCO (Carlsbad, CA, USA). Cell death detection ΕLISAPlus kit was purchased from Roche (Mannheim, Germany). Human sFas and human sFas ligand ELISA kits were purchased from R&D systems (Minneapolis, MN, USA). Human Bax ELISA kit was purchased from Assay Designs, Inc. (Ann Arbor, MI, USA) and human Bcl-2 ELISA kit was purchased from Bender Medsystems (Vienna, Austria).
Cell cultures
HepG2 cells were maintained in DMEM supplemented with 10% FBS and 1% penicillin/streptomycin solution, in a 37°C humidified incubator under an atmosphere of 5% CO2. On attaining 75–80% confluency the cells were subcultured by trypsinization and then seeded in appropriate cell numbers depending on the type of the experiments. All experiments took place 24 h after seeding.
Cytotoxicity assay
The cytotoxic potential of AP was evaluated at 24, 48, and 72 h by the MTT method. HepG2 cells were seeded in 96-well plates at a density of 104 cells per well in 100 μL of complete culture medium. Cells were incubated with 0.1, 1, 5, 10, 20, 50, and 100 μΜ of AP or 0.1% DMSO (vehicle control). AP stock solution was prepared in DMSO and diluted in complete culture medium to the desired concentrations (0.1, 1, 5, 10, 20, 50, and 100 μΜ). At each time point, eight replicate cultures for each concentration were studied in three independent experiments. At the end of the specified incubation period (24, 48, and 72 h), the medium was discarded and each well received 200 μL of fresh medium containing 20 μL of MTT solution (5 mg/ml in phosphate buffered saline) for 4 h. MTT crystals were dissolved by adding 100 μL 0.04 M HCL/isopropanol, for fifteen minutes at 37°C. Absorbance was determined at 570 nm by an ExpertPlus microplate reader (ASYS Hitech GmbH, Austria). Absorbance was normalized to vehicle-treated control cultures (equivalent to 100% cell viability).
SCEs and CAs analysis
For SCEs and CAs determination, 2 × 105 cells were treated with 1, 10, 20, and 50 μΜ of AP and 5 μg/mL of 5-bromodeoxyuridine for 72 h. Colcemid was added to all cultures 24 h before metaphase harvesting. At the end of the incubation period, the cells were scraped and centrifuged (Z300, Hermle Labortechnik GmbH, Germany) at 200 × g for 10 min. Pelleted cells were then treated with 5 mL of hypotonic KCl solution (0.075 M), at 37°C for 25 min. Fixative solution (3:1, methanol:acetic acid) was added to the cell suspension and was followed by another centrifugation at 200 × g for 10 min. The pellet was washed three times in fixative solution and stored at -20°C until further assayed. All treatments were examined in three independent experiments.
Fluorescence plus Giemsa
SCEs were visualized by a modified fluorescence plus Giemsa (FPG) technique [62]. Metaphase spreads were incubated in bisbenzimide H33258 solution (0.1 mg/mL) for 20 min at room temperature. A few drops of McIlivaine’s buffer (pH 8; 0.1 M citric acid and 0.2 M disodium phosphate) were applied to each slide and overlaid with a coverslip. After that, the slides were exposed to UV light for 90 min and stained with 7% Giemsa solution in Gurr buffer (pH 6.8).
Since the number of chromosomes in HepG2 cells varies from 50 to 60 (modal number: 55), the SCEs/chromosome rate was estimated. SCEs were evaluated in more than 60 well-spread second-division metaphases for each treatment. CAs were evaluated in 300 first division metaphases for each treatment. The criteria to classify different types of aberrations were in accordance with the recommendations of IPCS guidelines [43]. CAs were classified as chromatid gaps (chtg), chromatid breaks (chtb), chromosome gaps (chrg), chromosome breaks (chrb), ring (r), and dicentric chromosomes (d). Gaps were not included in the determination of total aberrant cells per treatment. Scoring was performed in a blind fashion.
PRI and MI assessment
For PRI and MI determinations, more than 450 cells and 4,500 nuclei were scored for each treatment, respectively. The proportion of cells in the first, second, third, or subsequent mitotic division was evaluated to determine the PRI. PRI was established according to the following formula:
where ΣM1 is the sum of cells in the first mitotic division, ΣM2 in the second and ΣM3+ in the third or subsequent mitotic divisions, while N is the total number of cells scored [63]. MI was expressed as the number of cells at metaphase per 1,000 analyzed nuclei (‰).
Assessment of apoptosis
As an index of apoptosis, cytoplasmic histone-associated DNA fragments were photometrically determined by the Cell Death Detection ΕLISAPlus kit according to the manufacturer’s instructions. Ten thousand cells per well were seeded in 96-well plates and treated with AP (20 μΜ) for 24 h (six replicate cultures). Cells were lysed and centrifuged at 130 × g. Supernatants were transferred into a streptavidin-coated microplate and simultaneously incubated with a monoclonal mouse biotinylated anti-histone antibody (clone H11-4) and a monoclonal mouse peroxidase-conjugated anti-DNA antibody (clone MCA-33) at room temperature for 2 h. DNA-histone complex was used as a positive control. Absorbance was determined at 405 nm by an ExpertPlus microplate reader. Background values were subtracted from the measurements.
Determination of sFas, mFasL, sFasL, Bcl-2, and Bax protein levels
Protein levels of soluble Fas (sFas), membrane-bound Fas-Ligand (mFasL), soluble Fas-Ligand (sFasL), Bcl-2, and Bax were determined by ELISA according to the manufacturers’ instructions. HepG2 cells were treated with 20 μM of AP for 1, 3, 6, 12, 24, and 48 h. Soluble Fas, sFasL, and mFasL protein levels were evaluated in the supernatant or cell lysate of 1 × 106 cells/mL. Bcl-2 and Bax protein levels were determined in 5 × 105 cells/mL and 62,500 cells/mL cell lysates, respectively. Bradford protein assay was used for total protein determination. Protein levels were interpolated from the corresponding standard reference calibration curves. Three independent experiments took place at all time points.
Statistical analysis
Data were expressed as mean ± standard deviation (SD). SCEs and CAs values were logarithmically transformed before further analysis because data were not normally distributed. Statistical analysis was performed by Student’s t-test for individual comparisons between control and apigenin-treated cultures. Multiple comparisons among various AP treatments were carried out by one-way ANOVA followed by Bonferroni’s post hoc test. Linear regression analysis was used to determine dose–response relationships. Pearson’s correlation coefficient was also determined. All statistical analyses were performed by SPPS version 16 (IBM, USA). All tests were two-tailed and P values less than 0.05 were considered statistically significant. For Student’s t-test, significance levels were adjusted to 0.01 to reduce the overall Type I error.
Results and discussion
AP concentrations ranging from 10 to 50 μΜ at 48 and 72 h showed a dose–response relationship of cell survival (48 h: 10 vs. 20 μΜ, P < 0.001 and 20 vs. 50 μΜ, P = 0.005; 72 h: 10 vs. 20 μΜ, P < 0.001 and 20 vs. 50 μΜ, P = 0.001), while AP concentrations ranging from 20–100 μΜ showed a time-dependent decrease (20 μΜ: 24 vs. 48 h, P < 0.001 and 48 vs. 72 h, P = 0.003; 50 μΜ: 24 vs. 48 h, P < 0.001 and 48 vs. 72 h, P < 0.001; 100 μΜ: 24 vs. 48 h, P < 0.001 and 48 vs. 72 h, P < 0.001) (48 h: IC50 = 34.58 μΜ; 72 h: IC50 = 18.80 μΜ) (Figure 1A). Similar results were reported by Chiang et al.[25] and Choi et al.[27], who studied the antiproliferative effect of AP in HepG2 cells. In agreement with Khan et al.[26], AP induced apoptosis at 24 h, eliciting an 11-fold increase in cytoplasmic histone-associated DNA fragments (P < 0.001) (Figure 1B).
AP (100 μΜ) induced DNA damage in Chinese hamster V79 cells and increased the frequency of micronuclei and CAs (concentrations higher than 37 μM) in human peripheral lymphocytes [34, 36–38, 64, 65]. In our study, we observed no effect on the frequency of aberrant cells (Table 1) but we noticed an increase in the frequency of SCEs at much lower concentrations (10 and 20 μΜ). However, 50 μΜ of AP was highly cytotoxic, making SCEs evaluation impossible (Table 2). This could be attributed to the high sensitivity of the SCEs method for detecting DNA damage and repair at doses that have little or no effect on CAs frequency [46–49, 66]. Moreover, the independent mechanisms leading to SCEs and CAs formation [46, 67–69] and the use of different cell systems could account for the differences. HepG2 cells have a polymorphic genetic profile with a variety of structural and numerical chromosomal abnormalities [70–72]. Sixty-seven breakpoints were identified in liver cancer cell lines including HepG2 cells [72]. Zimonjic et al.[71] performed comparative genomic hybridization analysis in 18 liver cancer cell lines and reported that regions exhibiting gain or loss, ranged from whole chromosome arms to a medium band of a 400-band ideogram. These previous findings could justify the high frequency of aberrant cells found in the control groups in the present study.
Linear regression analysis revealed a dose–response relationship between AP and SCEs frequencies, cell proliferation, and mitotic divisions (R = 0.798, R2 = 0.636, P < 0.001; R = -0.883, R2 = 0.781, P < 0.001; R = -0.820, R2 = 0.672, P < 0.001, respectively). AP concentration was positively correlated with the first and second mitotic division metaphases (R = 0.837, R2 = 0.700, P < 0.001; R = 0.768, R2 = 0.589, P < 0.001, respectively), while the third and subsequent mitotic division metaphases were negatively correlated (R = -0.867, R2 = 0.751, P < 0.001) with AP (Table 3). The flavonoid’s genotoxic potential was correlated with increased cytostaticity (SCEs vs. PRI: R = -0.582, R2 = 0.339, P = 0.018) and cytotoxicity (SCEs vs. MI: R = -0.573, R2 = 0.329, P = 0.032).
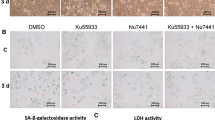
DSBs are repaired by homologous recombination, in which SCEs play an important role [73–75]. Iijima et al.[76] reported that NBS1, a protein involved in cellular responses to DSBs [77], regulated Bax activation in DNA damage-induced apoptosis. Furthermore, pro-apoptotic BAX could comprise a p53 downstream target gene through the direct binding of p53 to cofactors ASPP1 and ASPP2 [78, 79]. Bcl-2 could protect cells against cell death induced by ionizing radiation, alkylating agents, and various chemotherapeutic drugs [80–83]. Formation of DSBs by severe DNA damage triggered Bcl-2 decline and activated caspase-9 and caspase-3 [84]. In our study, AP treatment affected both Bcl-2 and Bax protein levels. Bcl-2 expression was downregulated at 3–48 h (Figure 2B). Bax levels were significantly lower in apigenin-treated cells at 1 and 3 h (P = 0.003 and P < 0.001, respectively) (Figure 2C). At 24 h, Bax expression was significantly upregulated compared with the corresponding vehicle-treated cultures (P = 0.005) and the respective 12 h of treatment (P = 0.001). Bax’s upregulation was transient and significantly reduced to the corresponding control cultures levels after 48 h. The Bax/Bcl-2 ratio, which is indicative of the mitochondrial induced apoptotic potential, exhibited a noticeable increase from 12–48 h of treatment (Figure 2D). Similar changes in the Bax/Bcl-2 ratio were observed in human lung A549 cancer cells and human prostate carcinoma DU145 cells [32, 33].
The effect of apigenin on apoptosis-related proteins. A. The effect of apigenin (20 μΜ) treatment on sFas protein levels. Control cultures: 6 vs. 12 h, P = 0.005; 12 vs. 24 h, P = 0.001. Apigenin treatment: 3 vs. 6 h, P = 0.021; 6 vs. 12 h, P = 0.001; 12 vs. 24 h, P = 0.001; 24 vs. 48 h, P = 0.001. B. The effect of apigenin (20 μΜ) treatment on Bcl-2 protein levels. C. The effect of apigenin (20 μΜ) treatment on Bax protein levels. D. The effect of apigenin (20 μΜ) treatment on Bax/Bcl-2 ratio. According to linear regression analysis: Time intervals 1–12 h, R = 0.960, R2 = 0.921, P = 0.040; Time intervals 12–48 h, R = -0.957, R2 = 0.915, P = 0.188. The star (*) indicates statistical significance compared with the respective control cultures.
Genotoxic agents could lead to cell death through the Fas/FasL mediated apoptotic pathway [85, 86]. In the present study, mFasL and sFasL were undetectable at all time points in all cultures. Nevertheless, sFas increased in a time-dependent manner in untreated and treated cultures (Control cultures: 6 vs. 12 h, P = 0.005; 12 vs. 24 h, P = 0.001. Apigenin treatment: 3 vs. 6h, P = 0.021; 6 vs. 12 h, P = 0.001; 12 vs. 24 h, P = 0.001; 24 vs. 48 h, P = 0.001) (Figure 2A). AP increased sFas levels at 1 and 24 h, compared with the corresponding control cultures (P = 0.002 and P = 0.001, respectively). Upregulation of sFas at 24 h, was transient and significantly reduced at 48 h, compared with the respective 24 h treatment (P = 0.001) and the corresponding control cultures (P = 0.001). There are no previous reports on the effect of AP on alternatively spliced FAS. Fas-mediated signaling is not limited to inducing cell death, and its expression in various cell types does not always correlate with susceptibility to the Fas-mediated apoptotic pathway [86, 87]. Alternatively, spliced FAS variants, which encode soluble forms of the receptor, could inhibit apoptosis [88–90]. Because of the sharp Bcl-2 downregulation at 12 h, sFas upregulation might represent a rescuing mechanism as a means to prevail over cell death signals. Filippov et al.[91] reported that cells in response to exogenous stress, such as the effect of a genotoxic agent, regulated the expression of specific splicing factors, altering the splicing profile of target genes such as CD44 and FAS. Since ROS induce alternative splicing, it is possible that free oxygen radical generation by AP could justify the induction of sFas expression [27, 92, 93]. AP’s intercalation into DNA/RNA might have also contributed to these changes in the expression of FAS.
Conclusion
AP exhibited dose-dependent genotoxic potential that led to changes in sFas, Bcl-2, and Bax protein levels in HepG2 cells.
Abbreviations
- AP:
-
Apigenin
- CAs:
-
Chromosomal aberrations
- chrb:
-
Chromosome break chrg, chromosome gap
- chtb:
-
Chromatid break
- chtg:
-
Chromatid gap
- d:
-
Dicentric chromosome
- DMEM:
-
Dulbecco’s modified Eagle’s medium
- DMSO:
-
Dimethyl sulfoxide
- DSBs:
-
Double-strand breaks
- f:
-
Fragment
- FBS:
-
Fetal bovine serum
- mFas:
-
Membrane-bound Fas
- mFasL:
-
Membrane-bound Fas-Ligand
- MI:
-
Mitotic index
- MTT:
-
3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide
- PRI:
-
Proliferation rate index
- r:
-
Ring chromosome
- ROS:
-
Reactive oxygen species
- SCEs:
-
Sister chromatid exchanges
- SD:
-
Standard deviation
- sFas:
-
Soluble Fas
- sFasL:
-
Soluble Fas-Ligand
- SSBs:
-
Single-strand breaks.
References
Wang Z, Wang N, Chen J, Shen J: Emerging glycolysis targeting and drug discovery from Chinese medicine in cancer therapy. Evid Based Complement Alternat Med. 2012, 2012: 873175-
Carmady B, Smith CA: Use of Chinese medicine by cancer patients: a review of surveys. Chin Med. 2011, 6: 22-10.1186/1749-8546-6-22.
Cragg GM, Newman DJ: Plants as a source of anti-cancer agents. J Ethnopharmacol. 2005, 100: 72-79. 10.1016/j.jep.2005.05.011.
Kim DI, Lee TK, Lim IS, Kim H, Lee YC, Kim CH: Regulation of IGF-I production and proliferation of human leiomyomal smooth muscle cells by Scutellaria barbata D. Don in vitro: isolation of flavonoids of apigenin and luteolin as acting compounds. Toxicol Appl Pharmacol. 2005, 205: 213-224. 10.1016/j.taap.2004.10.007.
Cao Y, Chu Q, Fang Y, Ye J:Analysis of flavonoids in Ginkgo biloba L. and its phytopharmaceuticals by capillary electrophoresis with electrochemical detection. Anal Bioanal Chem. 2002, 374: 294-299. 10.1007/s00216-002-1436-2.
Zheng QS, Sun XL, Xu B, Li G, Song M: Mechanisms of apigenin-7-glucoside as a hepatoprotective agent. Biomed Environ Sci. 2005, 18: 65-70.
Tsai CH, Lin FM, Yang YC, Lee MT, Cha TL, Wu GJ, Hsieh SC, Hsiao PW: Herbal extract of Wedelia chinensis attenuates androgen receptor activity and orthotopic growth of prostate cancer in nude mice. Clin Cancer Res. 2009, 15: 5435-5444. 10.1158/1078-0432.CCR-09-0298.
Chao WW, Lin BF: Isolation and identification of bioactive compounds in Andrographis paniculata (Chuanxinlian). Chin Med. 2010, 5: 17-10.1186/1749-8546-5-17.
Lu XY, Sun DL, Chen ZJ, Chen T, Li LP, Xu ZH, Jiang HD, Zeng S: Relative contribution of small and large intestine to deglycosylation and absorption of flavonoids from Chrysanthemun morifolium extract. J Agric Food Chem. 2010, 58: 10661-10667. 10.1021/jf102992r.
Chen Z, Kong S, Song F, Li L, Jiang H: Pharmacokinetic study of luteolin, apigenin, chrysoeriol and diosmetin after oral administration of Flos Chrysanthemi extract in rats. Fitoterapia. 2012, 83: 1616-1622. 10.1016/j.fitote.2012.09.011.
Kuo ML, Lee KC, Lin JK: Genotoxicities of nitropyrenes and their modulation by apigenin, tannic acid, ellagic acid and indole-3-carbinol in the Salmonella and CHO systems. Mutat Res. 1992, 270: 87-95. 10.1016/0027-5107(92)90119-M.
Myhrstad MC, Carlsen H, Nordstrom O, Blomhoff R, Moskaug JO: Flavonoids increase the intracellular glutathione level by transactivation of the gamma-glutamylcysteine synthetase catalytical subunit promoter. Free Radic Biol Med. 2002, 32: 386-393. 10.1016/S0891-5849(01)00812-7.
Liang YC, Huang YT, Tsai SH, Lin-Shiau SY, Chen CF, Lin JK: Suppression of inducible cyclooxygenase and inducible nitric oxide synthase by apigenin and related flavonoids in mouse macrophages. Carcinogenesis. 1999, 20: 1945-1952. 10.1093/carcin/20.10.1945.
Wei H, Tye L, Bresnick E, Birt DF: Inhibitory effect of apigenin, a plant flavonoid, on epidermal ornithine decarboxylase and skin tumor promotion in mice. Cancer Res. 1990, 50: 499-502.
Birt DF, Mitchell D, Gold B, Pour P, Pinch HC: Inhibition of ultraviolet light induced skin carcinogenesis in SKH-1 mice by apigenin, a plant flavonoid. Anticancer Res. 1997, 17: 85-91.
Van Dross R, Xue Y, Knudson A, Pelling JC: The chemopreventive bioflavonoid apigenin modulates signal transduction pathways in keratinocyte and colon carcinoma cell lines. J Nutr. 2003, 133 (Supp 1): 3800-3804.
McVean M, Xiao H, Isobe K, Pelling JC: Increase in wild-type p53 stability and transactivational activity by the chemopreventive agent apigenin in keratinocytes. Carcinogenesis. 2000, 21: 633-639. 10.1093/carcin/21.4.633.
Wang W, Heideman L, Chung CS, Pelling JC, Koehler KJ, Birt DF: Cell-cycle arrest at G2/M and growth inhibition by apigenin in human colon carcinoma cell lines. Mol Carcinog. 2000, 28: 102-110. 10.1002/1098-2744(200006)28:2<102::AID-MC6>3.0.CO;2-2.
Zheng P-W, Chiang L-C, Lin C-C: Apigenin induced apoptosis through p53-dependent pathway in human cervical carcinoma cells. Life Sci. 2005, 76: 1367-1379. 10.1016/j.lfs.2004.08.023.
Patel SD, Shukla S, Gupta S: Apigenin and cancer chemoprevention: Progress, potential and promise (Review). Int J Oncol. 2007, 30: 233-245.
Xu Y, Xin Y, Diao Y, Lu C, Fu J, Luo L, Yin Z: Synergistic effects of apigenin and paclitaxel on apoptosis of cancer cells. PLoS One. 2011, 6: e29169-10.1371/journal.pone.0029169.
Miyoshi N, Naniwa K, Yamada T, Osawa T, Nakamura Y: Dietary flavonoid apigenin is a potential inducer of intracellular oxidative stress: the role in the interruptive apoptotic signal. Arch Biochem Biophys. 2007, 466: 274-282. 10.1016/j.abb.2007.07.026.
Crespo I, García-Mediavilla MV, Almar M, González P, Tuñón MJ, Sánchez-Campos S, González-Gallego J: Differential effects of dietary flavonoids on reactive oxygen and nitrogen species generation and changes in antioxidant enzyme expression induced by proinflammatory cytokines in Chang Liver cells. Food Chem Toxicol. 2008, 46: 1555-1569. 10.1016/j.fct.2007.12.014.
Jeyabal PVS, Syed MB, Venkataraman M, Sambandham JK, Sakthisekaran D: Apigenin inhibits oxidative stress-induced macromolecular damage in N-nitrosodiethylamine (NDEA)-induced hepatocellular carcinogenesis in Wistar albino rats. Mol Carcinog. 2005, 44: 11-20. 10.1002/mc.20115.
Chiang L-C, Ng LT, Lin I-C, Kuo P-L, Lin C-C: Anti-proliferative effect of apigenin and its apoptotic induction in human HepG2 cells. Cancer Lett. 2006, 237: 207-214. 10.1016/j.canlet.2005.06.002.
Khan TH, Sultana S: Apigenin induces apoptosis in HepG2 cells: possible role of TNF-a and IFN-a. Toxicology. 2006, 217: 206-212. 10.1016/j.tox.2005.09.019.
Choi SI, CS J, Cho SY, YS L: Mechanisms of apoptosis induced by apigenin in HepG2 human hepatoma cells: Involvement of reactive oxygen species generated by NADPH oxidase. Arch Pharm Res. 2007, 30: 1328-1335. 10.1007/BF02980274.
Valdameri G, Trombetta-Lima M, Worfel PR, Pires AR, Martinez GR, Noleto GR, Cadena SM, Sogayar MC, Winnischofer SM, Rocha ME: Involvement of catalase in the apoptotic mechanism induced by apigenin in HepG2 human hepatoma cells. Chem Biol Interact. 2011, 193: 180-189. 10.1016/j.cbi.2011.06.009.
Shukla S, Gupta S: Apigenin: A promising molecule for cancer prevention. Pharm Res. 2010, 27: 962-978. 10.1007/s11095-010-0089-7.
Wang IK, Lin-Shiau SY, Lin JK: Induction of apoptosis by apigenin and related flavonoids through cytochrome c release and activation of caspase-9 and caspase-3 in leukaemia HL-60 cells. Eur J Cancer. 1999, 35: 1517-1525. 10.1016/S0959-8049(99)00168-9.
Shukla S, Gupta S: Molecular mechanisms for apigenin-induced cell-cycle arrest and apoptosis of hormone refractory human prostate carcinoma DU145 cells. Mol Carcinog. 2004, 39: 114-126. 10.1002/mc.10168.
Shukla S, Gupta S: Apigenin-induced prostate cancer cell death is initiated by reactive oxygen species and p53 activation. Free Radic Biol Med. 2008, 44: 1833-1845. 10.1016/j.freeradbiomed.2008.02.007.
Lu HF, Chie YS, Tan TW, Wu SH, Ma YS, Ip SW, Chung JG: Apigenin induces caspase-dependent apoptosis in human lung cancer A549 cells through Bax- and Bcl-2-triggered mitochondrial pathway. Int J Oncol. 2010, 36: 1477-1484.
Rithidech KN, Tungjai M, Whorton EB: Protective effect of apigenin on radiation-induced chromosomal damage in human lymphocytes. Mutat Res. 2005, 585: 96-104. 10.1016/j.mrgentox.2005.04.003.
Khan TH, Jahangir T, Prasad L, Sarwat S: Inhibitory effect of apigenin on benzo(a) pyrene-mediated genotoxicity in Swiss albino mice. J Pharm Pharmacol. 2006, 58: 1655-1660. 10.1211/jpp.58.12.0013.
Siddique YH, Ara G, Beg T, Afzal M: Anticlastogenic effect of apigenin in human lymphocytes treated with ethinylestradiol. Fitoterapia. 2010, 81: 590-594. 10.1016/j.fitote.2010.02.003.
Snyder RD, Gillies PJ: Evaluation of the clastogenic, DNA intercalative, and topoisomerase II-interactive properties of bioflavonoids in Chinese hamster V79 cells. Environ Mol Mutagen. 2002, 40: 266-276. 10.1002/em.10121.
Noel S, Kasinathan M, Rath SK: Evaluation of apigenin using in vitro cytochalasin blocked micronucleus assay. Toxicol in Vitro. 2006, 20: 1168-1172. 10.1016/j.tiv.2006.03.007.
Nafisi S, Hashemi M, Rajabi M, Tajmir-Riahi HA: DNA adducts with antioxidant flavonoids: morin, apigenin, and naringin. DNA Cell Biol. 2008, 27: 433-442. 10.1089/dna.2008.0735.
Kanakis CD, Nafisi S, Rajabi M, Shadaloi A, Tarantilis PA, Polissiou MG, Bariyanga J, Tajmir-Riahi HA: Structural analysis of DNA and RNA interactions with antioxidant flavonoids. Spectroscopy. 2009, 23: 29-43. 10.1155/2009/154321.
Ross WE, Bradley MO: DNA double-strand breaks in mammalian cells after exposure to intercalating agents. Biochim Biophys Acta. 1981, 654: 129-134. 10.1016/0005-2787(81)90145-3.
Pommier Y, Schwartz RE, Zwelling LA, Kohn KW: Effects of DNA intercalating agents on topoisomerase II induced DNA strand cleavage in isolated mammalian cell nuclei. Biochemistry. 1985, 24: 6406-6410. 10.1021/bi00344a014.
Albertini RJ, Anderson D, Douglas GK, Hagmar L, Hemminki K, Merlo F, Natarajan AT, Norppa H, Shuker DE, Tice R, Waters MD, Aitio A: IPCS guidelines for the monitoring of genotoxic effects of carcinogens in humans. Mutat Res. 2000, 463: 111-172. 10.1016/S1383-5742(00)00049-1.
Pandey M, Kaur P, Shukla S, Abbas A, Fu P, Gupta S: Plant flavone apigenin inhibits HDAC and remodels chromatin to induce growth arrest and apoptosis in human prostate cancer cells: in vitro and in vivo study. Mol Carcinog. 2012, 51: 952-962. 10.1002/mc.20866.
Thurn KT, Thomas S, Moore A, Munster PN: Rational therapeutic combinations with histone deacetylase inhibitors for the treatment of cancer. Future Oncol. 2011, 7: 263-283. 10.2217/fon.11.2.
Morris SM, Casciano DA, Casto BC: Detection of carcinogens based in in vitro mammalian cytogenetic tests. Handbook of carcinogen testing. Edited by: Milman HA, Weisburger EK. 1994, New Jersey: Noyes Publications, 100-115. 2
Solomon E, Bobrow M: Sister chromatid exchanges-a sensitive assay of agents damaging human chromosomes. Mutat Res. 1975, 30: 273-278.
Nakanishi Y, Schneider EL: In vivo sister-chromatid exchange: a sensitive measure of DNA damage. Mutat Res. 1979, 60: 329-337. 10.1016/0027-5107(79)90023-X.
Das BC: Factors that influence formation of sister chromatid exchanges in human blood lymphocytes. Crit Rev Toxicol. 1988, 19: 43-86. 10.3109/10408448809040817.
Marzano C, Bettio F, Baccichetti F, Trevisan A, Giovagnini L, Fregona D: Antitumor activity of a new platinum (II) complex with low nephrotoxicity and genotoxicity. Chem Biol Interact. 2004, 148: 37-48. 10.1016/j.cbi.2004.04.002.
Lialiaris T, Lyratzopoulos E, Papachristou F, Simopoulou M, Mourelatos C, Nikolettos N: Supplementation of melatonin protects human lymphocytes in vitro from the genotoxic activity of melphalan. Mutagenesis. 2008, 23: 347-354. 10.1093/mutage/gen020.
Lialiaris TS, Kotsiou E, Pouliliou S, Kareli D, Makrinou H, Kouskoukis A, Papachristou F, Koukourakis M: Cytoprotective activity of amifostine on cultured human lymphocytes exposed to irinotecan. Food Chem Toxicol. 2009, 47: 2445-2449. 10.1016/j.fct.2009.06.042.
Lialiaris TS, Papachristou F, Mourelatos C, Simopoulou M: Antineoplastic and cytogenetic effects of chlorpromazine on human lymphocytes in vitro and on Ehrlich ascites tumor cells in vivo. Anti Cancer Drugs. 2009, 20: 746-751. 10.1097/CAD.0b013e32832f567b.
Turkez H, Tatar A, Hacimuftuoglu A, Ozdemir E: Boric acid as a protector against paclitaxel genotoxicity. Acta Biochim Pol. 2010, 57: 95-97.
Tofilon P, Basic I, Milas L: Prediction of in vivo tumour response to chemotherapeutic agents by the in vitro SCE assay. Cancer Res. 1985, 45: 2025-2030.
Denn DF, Kendall LA, Marton LJ, Tofilon P: Prediction of human tumour cell chemosensitivity using the SCE assay. Cancer Res. 1986, 46: 1599-1602.
Swierenga SHH, Heddle JA, Sigal EA, Gilman JPW, Brillinger RL, Douglas GR, Nestmann ER: Recommended protocols on a survey of current practice in genotoxicity testing laboratories, IV. Chromosome aberrations and sister chromatid exchanges in Chinese Hamster Ovary V79. Chinese Hamster lung and human lymphocyte cultures. Mutat Res. 1991, 246: 301-322. 10.1016/0027-5107(91)90050-X.
Hagmar L, Bonassi S, Stromberg U, Brøgger A, Knudsen LE, Norppa H, Reuterwall C: European study group on cytogenetic biomarkers and health: chromosomal aberration in human lymphocytes predict human cancer: a report from the European study group on cytogenetic biomarkers and health (ESCH). Cancer Res. 1998, 58: 4117-4121.
El-Deiry WS: Regulation of p53 downstream genes. Semin Cancer Biol. 1988, 8: 345-357.
Kastan MB, Onyekwere O, Sidransky D, Vogelstein B, Craig RW: Participation of p53 protein in the cellular response to DNA damage. Cancer Res. 1991, 51: 6304-6311.
Clarke AR, Gledhill S, Hooper ML, Bird CC, Wyllie AH: p53 dependence of early apoptotic and proliferative responses within the mouse intestinal epithelium following gamma-irradiation. Oncogene. 1994, 9: 1767-1773.
Perry P, Wolff S: New Giemsa method for the differential staining of sister chromatids. Nature. 1974, 251 (5471): 156-158. 10.1038/251156a0.
Lamberti L, Bigatti Ponzetto P, Ardito G: Cell kinetics and sister chromatid exchange frequency in human lymphocytes. Mutat Res. 1983, 120: 193-199. 10.1016/0165-7992(83)90163-X.
Galloway SM, Wolff S: The relation between chemically induced sister-chromatid exchanges and chromatid breakage. Mutat Res. 1979, 61: 297-307. 10.1016/0027-5107(79)90135-0.
Ikushima T: Role of sister chromatid exchanges in chromatid aberration formation. Nature. 1977, 268: 235-236. 10.1038/268235a0.
Gebhart E: Sister chromatid exchange (SCE) and chromosome aberrations in mutagenicity testing. Hum Genet. 1981, 58: 235-254. 10.1007/BF00294917.
Latt SA: Sister chromatid exchanges, indices of human chromosome damage and repair: detection by fluorescence and induction by mitomycin C. Proc Natl Acad Sci USA. 1974, 71: 3162-3166. 10.1073/pnas.71.8.3162.
Siddique YH, Beg T, Afzal M: Antigenotoxic effect of apigenin against anti-cancerous drugs. Toxicol in Vitro. 2008, 22: 625-631. 10.1016/j.tiv.2007.12.002.
Begum N, Prasad NR, Kanimozhi G, Hasan AQ: Apigenin ameliorates gamma radiation-induced cytogenetic alterations in cultured human blood lymphocytes. Mutat Res. 2012, 747: 71-76. 10.1016/j.mrgentox.2012.04.001.
Simon D, Aden DP, Knowle BB: Chromosomes of human hepatoma cell lines. Int J Cancer. 1982, 30: 27-33. 10.1002/ijc.2910300106.
Zimonjic DB, Keck CL, Thorgeirsson SS, Popescu NC: Novel recurrent genetic imbalances in human hepatocellular carcinoma cell lines identified by comparative genomic hybridization. Hepatology. 1999, 29: 1208-1214. 10.1002/hep.510290410.
Wong N, Lai P, Pang E, Leung TW-T, Lau JW-Y, Johnson PJ: A comprehensive karyotypic study on human hepatocellular carcinoma by spectral karyotyping. Hepatology. 2000, 32: 1060-1068. 10.1053/jhep.2000.19349.
Dronkert ML, Kanaar R: Repair of DNA interstrand cross-links. Mutat Res. 2001, 486: 217-247. 10.1016/S0921-8777(01)00092-1.
Helleday T: Pathways for mitotic homologous recombination in mammalian cells. Mutat Res. 2003, 532: 103-115. 10.1016/j.mrfmmm.2003.08.013.
Johnson DR, Jasin M: Sister chromatid gene conversion is a prominent double-strand break repair pathway in mammalian cells. EMBO J. 2000, 19: 3398-3407. 10.1093/emboj/19.13.3398.
Iijima K, Muranaka C, Kobayashi J, Sakamoto S, Komatsu K, Matsuura S, Kubota N, Tauchia H: NBS1 regulates a novel apoptotic pathway through Bax activation. DNA Repair. 2008, 7: 1705-1716. 10.1016/j.dnarep.2008.06.013.
Berkovich E, Monnat RJ, Kastan MB: Roles of ATM and NBS1 in chromatin structure modulation and DNA double-strand break repair. Nat Cell Biol. 2007, 9: 683-690. 10.1038/ncb1599.
Bergamaschi D, Samuels Y, Jin B, Duraisingham S, Crook T, Lu X: ASPP1 and ASPP2: common activators of p53 family members. Mol Cell Biol. 2004, 24: 1341-1350. 10.1128/MCB.24.3.1341-1350.2004.
Rozan LM, El-Deiry WS: p53 downstream target genes and tumor suppression: a classical view in evolution. Cell Death Differ. 2007, 14: 3-9. 10.1038/sj.cdd.4402058.
Strasser A, Harris AW, Jacks T, Cory S: DNA damage can induce apoptosis in proliferating lymphoid cells via p53-independent mechanisms inhibitable by Bcl-2. Cell. 1994, 79: 329-339. 10.1016/0092-8674(94)90201-1.
Chao DT, Linette GP, Boise LH, White LS, Thompson CB, Korsmeyer SJ: Bcl-xL and Bcl-2 repress a common pathway of cell death. J Exp Med. 1995, 182: 821-828. 10.1084/jem.182.3.821.
Meikrantz W, Bergom MA, Memisoglu A, Samson L: O6-Alkylguanine DNA lesions trigger apoptosis. Carcinogenesis. 1998, 19: 369-372. 10.1093/carcin/19.2.369.
Zhang J, Reedy MC, Hannun YA, Obeid LM: Inhibition of caspases inhibits the release of apoptotic bodies: Bcl-2 inhibits the initiation of formation of apoptotic bodies in chemotherapeutic agent-induced apoptosis. J Cell Biol. 1999, 145: 99-108. 10.1083/jcb.145.1.99.
Ochs K, Kaina B: Apoptosis induced by DNA Damage O -Methylguanine is Bcl-2 and Caspase-9/3 regulated and Fas/Caspase-8 independent. Cancer Res. 2000, 60: 5815-5824.
Friesen C, Herr I, Krammer PH, Debatin KM: Involvement of the CD95 (APO-1/Fas) receptor/ligand system in drug-induced apoptosis in leukemia cells. Nat Med. 1996, 2: 574-577. 10.1038/nm0596-574.
Mueller M, Strand S, Hug H, Heinemann E-M, Walczak H, Hofmann WJ, Stremmel W, Krammer PH, Galle PR: Drug-induced apoptosis in hepatoma cells is mediated by the CD95 (APO-1/Fas) receptor/ligand system and involves activation of wild-type p53. J Clin Inves. 1997, 99: 403-413. 10.1172/JCI119174.
Leithäuser F, Dhein J, Mechtersheimer G, Koretz K, Brüderlein S, Henne C, Schmidt A, Debatin K-M, Krammer PH, Moller P: Constitutive and induced expression of APO-1, a new member of the nerve growth factor/tumor necrosis factor receptor superfamily, in normal and neoplastic cells. Lab Invest. 1993, 69: 415-429.
Cheng J, Zhou T, Liu C, Shapiro JP, Brauer MJ, Kiefer MC, Barr PJ, Mountz JD: Protection from Fas-mediated apoptosis by a soluble form of the Fas molecule. Science. 1994, 263: 1759-1762. 10.1126/science.7510905.
Cascino I, Fiucci G, Papoff G, Ruberti G: Three functional soluble forms of the human apoptosis-inducing Fas molecule are produced by alternative splicing. J Immunol. 1995, 154: 2706-2713.
Cascino I, Papoff G, Eramo A, Ruberti G: Soluble Fas/Apo-1 splicing variants and apoptosis. Front Biosci. 1996, 1: d12-d18.
Filippov V, Schmidt EL, Filippova M, Duerksen-Hughes PJ: Splicing and splice factor SRp55 participate in the response to DNA damage by changing isoform ratios of target genes. Gene. 2008, 420: 34-41. 10.1016/j.gene.2008.05.008.
Izquierdo JM, Majós N, Bonnal S, Martínez C, Castelo R, Guigó R, Bilbao R, Valcárcel J: Regulation of Fas alternative splicing by antagonistic effects of TIA-1 and PTB on exon definition. Molec Cell. 2005, 19: 475-484. 10.1016/j.molcel.2005.06.015.
Busa R, Geremia R, Sette C: Genotoxic stress causes the accumulation of the splicing regulator Sam68 in nuclear foci of transcriptionally active chromatin. Nucleic Acids Res. 2010, 38: 3005-3018. 10.1093/nar/gkq004.
Acknowledgements
The authors would like to thank Assoc. Prof. G. Kolios, Department of Pharmacology, Medical School, Democritus University of Thrace, Alexandroupolis, Greece for kindly providing the HepG2 cell line and Katherine Bahk for language editing.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
CS, EC and AKT designed and supervised the study. FP wrote the manuscript and conducted the experiments. AtP, IK, NK, and AlP assisted experimentally and drafted parts of the manuscript. GT and FP performed the statistical analysis. All authors read and approved the final version of the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Papachristou, F., Chatzaki, E., Petrou, A. et al. Time course changes of anti- and pro-apoptotic proteins in apigenin-induced genotoxicity. Chin Med 8, 9 (2013). https://doi.org/10.1186/1749-8546-8-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1749-8546-8-9