Abstract
Background
To compare the RapidArc plan for primary hepatocellular carcinoma (HCC) with 3-D conformal radiotherapy (3DCRT) and intensity-modulated radiotherapy (IMRT) plans using dosimetric analysis.
Methods
Nine patients with unresectable HCC were enrolled in this study. Dosimetric values for RapidArc, IMRT, and 3DCRT were calculated for total doses of 45~50.4 Gy using 1.8 Gy/day. The parameters included the conformal index (CI), homogeneity index (HI), and hot spot (V107%) for the planned target volume (PTV) as well as the monitor units (MUs) for plan efficiency, the mean dose (Dmean) for the organs at risk (OAR) and the maximal dose at 1% volume (D1%) for the spinal cord. The percentage of the normal liver volume receiving ≥ 40, > 30, > 20, and > 10 Gy (V40 Gy, V30 Gy, V20 Gy, and V10 Gy) and the normal tissue complication probability (NTCP) were also evaluated to determine liver toxicity.
Results
All three methods achieved comparable homogeneity for the PTV. RapidArc achieved significantly better CI and V107% values than IMRT or 3DCRT (p < 0.05). The MUs were significantly lower for RapidArc (323.8 ± 60.7) and 3DCRT (322.3 ± 28.6) than for IMRT (1165.4 ± 170.7) (p < 0.001). IMRT achieved a significantly lower Dmean of the normal liver than did 3DCRT or RapidArc (p = 0.001). 3DCRT had higher V40 Gy and V30 Gy values for the normal liver than did RapidArc or IMRT. Although the V10 Gy to the normal liver was higher with RapidArc (75.8 ± 13.1%) than with 3DCRT or IMRT (60.5 ± 10.2% and 57.2 ± 10.0%, respectively; p < 0.01), the NTCP did not differ significantly between RapidArc (4.38 ± 2.69) and IMRT (3.98 ± 3.00) and both were better than 3DCRT (7.57 ± 4.36) (p = 0.02).
Conclusions
RapidArc provided favorable tumor coverage compared with IMRT or 3DCRT, but RapidArc is not superior to IMRT in terms of liver protection. Further studies are needed to establish treatment outcome differences between the three approaches.
Similar content being viewed by others
Background
Hepatocellular carcinoma (HCC) is the fifth most common malignancy and the third most common cause of cancer-related death in the world [1]. Surgical resection has been proven as the major treatment modality for HCC. However, most patients with HCC have unresectable disease at diagnosis. These patients are treated with other treatment modalities, such as percutaneous ethanol injection (PEI), radiofrequency ablation (RFA) therapy, transcatheter arterial chemoradiotherapy (TACE), or sorafenib, but the response to treatment is limited [2–6].
The use of radiation therapy (RT) for the treatment of HCC was first investigated more than 40 years ago, but the early trials reported poor results due to the low tolerance of the whole liver to radiation and severe hepatic toxicity, or radiation-induced liver disease (RILD) caused by whole liver irradiation [7, 8]. RILD, a clinical syndrome characterized by ascites, anicteric hepatomegaly, and impaired liver function, is developed in 5% of patients who received 30~33 Gy whole liver irradiation and usually occurs 2 weeks to 4 months after completion of RT. RILD usually resolves after supportive care. Unfortunately, severe RILD may develop into hepatic failure and even death [9, 10]. The low hepatic tolerance to radiation also limits the application of higher radiation doses to the tumor. In 1991, Emami et al. reported that the TD5/5 (the tolerance dose leading to a 5% complication rate at 5 years) for 1/3, 2/3, and the whole liver at 1.8~2 Gy/day were 50 Gy, 35 Gy, and 30 Gy, respectively [11]. Dawson et al used the normal tissue complication probability (NTCP) of the Lyman model to describe the relationship between irradiated liver volume and radiation dose and they demonstrated that a higher radiation dose could be delivered safely to liver tumors, with better outcomes, if only part of the liver was irradiated [12]. As image-based treatment planning and engineering has advanced, three-dimensional conformal radiotherapy (3DCRT) was developed to irradiate the tumor accurately while minimizing the dose to the normal liver. A number of studies have demonstrated encouraging results showing that a radiation dose could be safely increased to part of the liver using 3DCRT [13]. For example, Park et al. reported a significant relationship between the total dose to the liver tumor and the tumor response (< 40 Gy, 40-50 Gy, and > 50 Gy giving responses of 29.2%, 68.6%, and 77.1%, respectively) without significant toxicity (rate of liver toxicity: 4.2%, 5.9%, and 8.4%, respectively).
Despite improvements to 3DCRT, dose distribution remains suboptimal in some cases. In the early 2000s, the development of inverse planning systems and multileaf collimators (MLCs) culminated in a more sophisticated technique, intensity-modulated radiotherapy (IMRT). Using an inverse planning algorithm to generate multiple nonuniform-intensity beams, IMRT can potentially deliver a higher dose to the tumor while delivering a relatively lower dose to the normal liver as compared with 3DCRT. Cheng et al. suggested that IMRT might be able to preserve acceptable target coverage and potentially reduce NTCP values (IMRT = 23.7% and 3DCRT = 36.6%, p = 0.009) compared with 3DCRT [14]. Fuss et al. reported that IMRT allowed a dose escalation to 60 Gy, in which range 3DCRT had to reduce the total dose to decrease the probability of RILD to acceptable levels [15].
The RapidArc technique, developed by Varian Medical Systems about 2 years ago, is a volumetric intensity-modulated arc therapy that accurately and efficiently delivers a radiation dose to the target using a one-or two-arc gantry rotation by simultaneously modulating the MLC motion and the dose rates. RapidArc has been shown to be equivalent or superior to IMRT for some malignancies, including head and neck cancer and prostate cancer [16–18], but there has been no study to determine the feasibility of using RapidArc for the treatment of primary HCC. The purpose of our study was to compare the RapidArc radiation treatment plans for patients with HCC with 3DCRT and IMRT plans using dosimetric analysis. The PTV coverage and critical organ sparing for each technique were determined using dose-volume histograms (DVH) and the NTCP model.
Methods
Patient Characteristics
From April 2008 to July 2010, we enrolled nine patients who had primary HCC diagnosed at China Medical University Hospital. All patients underwent alpha-fetoprotein (AFP) examination, contrast-enhanced computed tomography (CT), and ultrasonography to confirm the diagnosis. All patients were male and the median age was 57 years (range, 38-81 years). Five patients had Child-Pugh score A cirrhosis and 4 had Child-Pugh score B cirrhosis. Eight (88.9%) patients had American Joint Committee on Cancer (6th edition) stage III disease, and 1 (11.1%) patient had stage IV disease.
Immobilization, Simulation, and Target Delineation
The patients were immobilized using vacuum casts in a supine position with both arms raised above their heads. Non-contrast CT simulation was performed with a 5-mm slice thickness and included whole liver and bilateral kidney scans. Respiratory control and abdominal compression were not used. After simulation, the CT images were transferred into the Eclipse treatment planning system (Version 8.6.15, Varian Medical System, Inc., Palo Alto, CA, US), and target delineation was performed with the aid of the contrast-enhanced CT images.
We defined the gross tumor volume (GTV) as the volume of primary tumor evident on contrast-enhanced CT images. The clinical target volume (CTV) was delineated on the basis of the GTV expanded by 5 mm. The planning target volume (PTV) was defined as the CTV with a 5-mm radial expansion and a 10-mm craniocaudal expansion to account for errors caused by the daily setup process and internal organ motion. The normal liver volume was defined as the total liver volume minus the GTV. All of the contours were drawn by the same physician.
Treatment Planning and Dose Delivery
In our study, we prescribed 95% of total dose to cover ≥ 95% of the PTV coverage in daily 1.8-Gy fractions while keeping the minimum dose ≥ 93% of total dose and maximum dose ≤ 107% of total dose and normalized all plans to the mean dose of PTV. The guidelines for dose prescription were as follows. When the normal liver volume irradiated with > 50% of the isocenter dose was < 25%, 25-50%, or 50-75%, the total dose prescribed was > 59.4 Gy, 45-54 Gy, and 41.4 Gy, respectively [19]. No patient received whole liver irradiation. The constraints for the organs at risk (OARs), can be seen in Table 1. These were imposed in terms of the TD5/5 to ensure that the maximal tolerated doses to the normal liver, stomach, kidneys, and spinal cord were not exceeded [11]. Six-or 10-MV photon beams were used, depending on the tumor location, and the same energy was used for each patient and for all three methods.
For each patient, three different plans (3DCRT, IMRT, and RapidArc) were calculated using the Eclipse planning system with the 120-leaf multi-leaf collimator (MLC) (Varian Medical Systems). For the 3DCRT and IMRT plans, all the gantry angles and numbers of radiation fields (range, 4-5) were manually selected on the basis of the morphological relationship between the PTV and OARs to cover at least 95% of the PTV and spare the OARs. A dose rate of 400 MU/min was used. For RapidArc, the plans were optimized using the two-arc technique with gantry angle running counterclockwise from 179° to 181° and clockwise from 181° to 179° and with the dose rate varied between 0 MU/min and 600 MU/min (upper limit). The optimization constraints for OARs using RapidArc were the same as the constraints in Table 1.
Plan Evaluation
1. PTV coverage
-
The dose to the PTV was evaluated using DVHs with the following parameters:
-
a.
Vx% means the volume receiving ≥ x% of the prescribed dose. For example, the V100% of the PTV was used to prescribe the PTV coverage, and V107% was used to represent the hot spot in the PTV.
-
b.
The conformity index (CI) = (VPTV/TVPV)/(TVPV/VTV) = VPTV × VTV/TVPV 2, where VPTV is the volume of the PTV, TVPV is the portion of the VPTV within the prescribed isodose line, and VTV is the treated volume of the prescribed isodose line [17, 20]. The CI represented the dose fit of the PTV relative to the volume covered by the prescribed isodose line. The smaller and closer the value of CI is to 1, the better the conformity of the PTV.
-
c.
The homogeneity index (HI) = D5%/D95%, where D5% and D95% are the minimum doses delivered to 5% and 95% of the PTV [17, 21]. HI is a ratio that is used to evaluate the homogeneity of the PTV. The smaller and closer the value of HI is to 1, the better the homogeneity of the PTV.
-
a.
2. OARs sparing
-
a.
VnGy is the percentage of organ volume receiving ≥ n Gy. In this study, V40 Gy was the percentage of the normal liver volume receiving ≥ 40 Gy, which represents high-dose exposure for the normal liver. In contrast, V10 Gy was the percentage of the normal liver volume receiving ≥ 10 Gy, which represented low-dose exposure for the normal liver.
-
b.
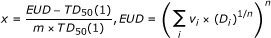
We used the normal tissue complication probability (NTCP), from the Lyman model, to measure the probability of RT complications in the normal liver [22]. In the NTCP model,
 (1)
(1)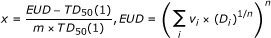 (2)
(2)
where EUD is the equivalent uniform dose, converted from the dose-volume pairs [D i , v i ], to describe the dose which, if delivered uniformly to the entire organ, would achieve the same effect as the given heterogeneous dose distribution demonstrated by the DVH. The TD50(1) is the dose to the whole liver that would result in a 50% probability of toxicity. The parameter "m" is the steepness of the dose-complication curve for a fixed partial volume. The parameter "n" is the slope of the complication probability, which determines the dose-volume relationship for the irradiated normal liver. In this study, the following values for the parameters were used: n = 0.32, m = 0.15, and TD50(1) = 40 Gy [23].
Statistical Analyses
The dosimetric differences among the three treatments for the nine patients were analyzed using the Friedman test. When a significant difference (p < 0.05) was found, the difference between two treatments for each effect was further examined by Wilcoxon signed-rank test. All analyses were performed using SPSS software, version 15.0 (SPSS Inc., Chicago, IL).
Results
PTV Coverage, CI, and HI
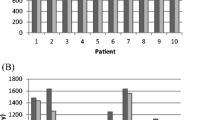
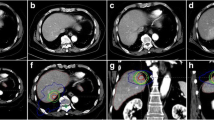
The mean gross tumor volume (GTV) was 979.3 ± 497.2 cm3 (range, 346.5-2019.3 cm3). The mean planned tumor volume (PTV) was 1734.2 ± 923.0 cm3 (range, 859.6-3253.4 cm3). The mean normal liver volume was 1632.4 ± 539.0 cm3 (range, 933.7-2270.6 cm3). None of the PTVs included the whole liver. The prescribed total dose was 49.4 ± 1.9 Gy (range, 45-50.4 Gy). The dose rate of RapidArc varied between 0 MU/min and 461 MU/min. The typical dose distributions and dose-volume histograms (DVH) for PTV and OARs are shown in Figure 1 and 2, respectively. In Figure 1C, RapidArc achieved better conformality to the 95% isodose line of the PTV than did 3DCRT and IMRT. In addition, RapidArc also achieved better spinal cord sparing to the 50% isodose line than did 3DCRT and IMRT. However, RapidArc resulted in higher coverage at the 30% isodose line in the normal liver as compared with 3DCRT (Figure 1A) or IMRT (Figure 1B), which means higher low-dose exposure occur for the normal liver with RapidArc. In Figure 2, the right DVH showed that all of the PTVs were fixed between V95% and V107%, without any significant differences. The left DVH showed that the low-dose distribution in the normal liver was greater for RapidArc than for 3DCRT or IMRT, and the high-dose distribution was greater for 3DCRT than for IMRT or RapidArc.
The comparison of isodose distributions of PTV and OAR in 3DCRT, IMRT and RapidArc. A: 3DCRT, B: IMRT and C: RapidArc. RapidArc achieved better conformality to the 95% isodose line (red line) of the PTV and better spinal cord sparing to the 50% isodose line (yellow line) as compared with 3DCRT and IMRT. However, RapidArc obtained higher 30%-isodose coverage (blue line) of volume of the normal liver than did 3DCRT and IMRT.
The comparison of DVHs for PTV and normal liver in 3DCRT, IMRT and RapidArc. Right figure = DVHs of PTV. These three techniques produced similar homogeneity of the PTV. Left figure = DVHs of normal liver. RapidArc obtained the higher low-dose distribution in the normal liver compared with 3DCRT and IMRT. On the other hand, 3DCRT obtained the high-dose distribution in the normal liver compared with IMRT and RapidArc.
Table 2 summarizes the results for the investigated DVH-parameters, including CTV coverage, PTV coverage, monitor unit (MU) dose and OAR dose for the 9 patients. Table 3 shows the differences among the three methods with regard to the DVH parameters. For target coverage, all V95% of CTV for these three techniques gave at least 99% of the prescribed dose without any significant difference (p = 1.00). For the PTV coverage, the mean CI of RapidArc (1.12 ± 0.05) was significantly lower than that of IMRT (1.19 ± 0.06) and 3DCRT (1.286 ± 0.11) (p < 0.05). The V95%, and V100% valus for PTVs and HI were 95.50 ± 2.41, 76.81 ± 5.95 and 1.13 ± 0.05 (3DCRT), 95.27 ± 1.99, 77.88 ± 4.27 and 1.13 ± 0.04 (IMRT), and 95.31 ± 1.64, 77.47 ± 2.64 and 1.12 ± 0.03 (RapidArc), respectively, with no significant differences among methods (p = 1.00, 1.00 and 0.69, respectively). For the hot spot sparing, the mean V107% of the PTV was significantly highest for 3DCRT (7.49 ± 7.92) and the lowest was RapidArc (1.74 ± 2.82); this indicates that there was better hot-spot sparing of the PTV with RapidArc than with IMRT or 3DCRT (p < 0.05).
OARs Sparing
The mean doses to the normal liver for each method were 21.58 ± 3.01 Gy (3DCRT), 19.31 ± 2.89 Gy (IMRT), and 21.97 ± 2.61 Gy (RapidArc), with a significantly lower mean dose to the normal liver with IMRT than with 3DCRT or RapidArc (p < 0.05). The high-dose regions of the normal liver were higher for V40 Gy and V30 Gy with 3DCRT (23.05 ± 4.06 and 32.10 ± 6.80) than with IMRT (18.61 ± 4.13 and 26.23 ± 5.87) (p < 0.01) or RapidArc (18.85 ± 3.97 and 27.77 ± 5.34) (p < 0.05). The low-dose region of the normal liver was higher for V10 Gy with RapidArc (75.77 ± 13.13) than with IMRT (57.24 ± 10.02) (p < 0.01) or 3DCRT (60.55 ± 10.24) (p < 0.05). In Table 3, the NTCP value for 3DCRT (7.57 ± 4.36) was significantly higher than that for IMRT (3.98 ± 3.00) (p < 0.01) or RapidArc (4.38 ± 2.69) (p < 0.05), but there was no significant difference in the NTCP between IMRT and RapidArc (p = 0.26). For the other OARs, there were no significant differences in dose among the three methods, except for a lower mean dose to the stomach and left kidney, respectively, with IMRT (20.63 ± 15.26 Gy and 8.36 ± 4.60 Gy) than with 3DCRT (23.16 ± 16.50 Gy and 11.37 ± 6.62 Gy) (p < 0.05). The maximum dose to the spinal cord (D1%) was equal for all three methods.
Efficiency Analysis
IMRT had three times the MUs (1165.44 ± 170.68) of RapidArc (323.78 ± 60.65) and 3DCRT (322.33 ± 28.62) (p < 0.01). There was no significant difference in the numbers of MUs between 3DCRT and RapidArc (p = 0.859).
Discussion
Historically, the role of RT in HCC has been limited because of the risk of RILD caused by whole liver irradiation. Improved knowledge of partial liver RT has created renewed in using RT with HCC and, furthermore, technical advancements in 3DCRT have allowed higher doses to targeted to the tumors while minimizing exposure of surrounding liver tissue. Recently, more and more types of conformal RT have been developed to deliver highly conformal treatment with minimal damage to surrounding normal liver parenchyma, including IMRT, image-guided radiotherapy (IGRT) and stereotactic body radiotherapy (SBRT) [24]. RapidArc is a novel form of volumetric intensity-modulated RT that has the advantages of a short treatment time, fewer MUs and the availability of highly conformal treatment plans. Several investigations have demonstrated the advantages of RapidArc. Verbakel et al. demonstrated that RapidArc achieved similar PTV coverage and OAR sparing but lower MUs than IMRT in patients with head and neck cancers. Besides, double arc plans yielded better PTV coverage than single arc or IMRT [16]. Palma et al. reported that variable dose rate volumetric modulated arc therapy achieved better dose distribution and lower MUs than IMRT in patients with prostate cancers. This work was a pilot study to investigate the dosimetric difference of a RapidArc plan for HCC compared to 3DCRT and IMRT plans.
In our study, the homogeneity of the PTV provided by all three techniques was similar, but the RapidArc was able to achieve better conformity and hot-spot sparing of the PTV compared to IMRT or 3DCRT (p < 0.05). For OARs sparing, the three methods showed comparable results in terms of the mean dose to the stomach and kidneys and maximum dose to the spinal cord. For the normal liver, 3DCRT provided the worst dose distribution, with significantly worse Dmean, V40 Gy, V30 Gy, and NTCP values than RapidArc or IMRT. Compared with IMRT, RapidArc provided comparable V40 Gy, V30 Gy, and NTCP values for the normal liver, but RapidArc achieved significantly higher Dmean, V20 Gy and V10 Gy values for the normal liver.
The Lyman NTCP model has been widely used to predict or estimate the probability of normal tissue complication. This model supposed there is a sigmoid relationship between a uniform radiation dose given to a part of the volume in an organ and the probability of complication. More and more authors have used this model to predict RILD. Burman et al. assigned the parameters to be as follows, n as 0.32, m as 0.15, and TD50(1) as 40 Gy, in a model that predict the risked of RILD [23]. Cheng et al. applied the values of n = 0.35, m = 0.35 and TD50(1) = 49.4 Gy in another model [25]. Dawson et al. further modified the parameter TD50(1) to 39.8 Gy for hepatobiliary cancer and to 45.8 Gy for liver metastasis (n = 0.97 and m = 0.12) [26]. Although different values for the parameters have been applied to the Lyman NTCP model by different authors, they demonstrated the feasibility of partial liver irradiation. If the TD50 is kept constant, the NTCP value is represented as a function of partial volume. This organ demonstrates a "threshold type behavior" and the NTCP value will rise only if a certain volume is irradiated. Furthermore, the NTCP value of the partial volume depends on the dose. Therefore, we believe that the V40 Gy and V30 Gy influence the NTCP values of the normal liver more than V20 Gy and V10 Gy do. In addition, Dawson et al. also addressed whether those who had impaired liver function might not be suitable for the Lyman NTCP model and whether a better understanding of the mechanism of RILD may improve the accuracy of Lyman model in the future.
In addition to value used for NTCP, the V30 Gy and Dmean of the normal liver play important roles in predicting the risk of RILD. Dawson et al. demonstrated that the Dmean of normal liver was associated with the risk of RILD [26]. Yamada et al. reported a deterioration in the Child-Pugh Score in 5 out of 6 patients with a V30 Gy > 40%, vs. 2 of 13 patients with a V30 Gy < 40% (p < 0.01) [27].
Another issue that should be kept in mind is the higher low-dose irradiation to normal liver compared with 3DCRT or IMRT when RapidArc is used. Shueng et al. published a case of cholangiocarcinoma with bone metastasis who had received palliative RT for bone pain who developed radiation pneumonitis [28]. They demonstrated that, in this case, although the V5 Gy of the normal lung was only 20%, this still potentially induced radiation pneumonitis. One of the possible causes is an interaction between radiation-induced inflammation within the previously irradiated field and chemotherapy. Yamashita et al. has reported that the incidence of lung toxicity will become higher if large amount of low dose radiation is delivered [29]. In addition to the dosimetric impact, several investigators reported that some biological factors are associated with RILD. For example, Cheng et al. reported that the HBV carriers or cases with Child-Pugh B cirrhosis were correlated with the risk of RILD after 3D-CRT [25]. Xu et al. also reported that the Child-Pugh classification was associated with RILD [30]. In the current study, the potential risk of RILD caused by low-dose irradiation is unclear, but HCC patients in Taiwan usually have hepatitis B or C infection and liver cirrhosis and they usually received TACE, PEI or targeted therapy before RT. Radiation oncologists should be aware of the potential risk of higher low-dose exposure to the normal liver when RapidArc is used.
From the view of dosimetric comparison, one of the reasons that RapidArc is not better than IMRT for liver protection may be that HCC is always surrounded by normal liver parenchyma, which is the major concern when using the volumetric RapidArc technique. In our study, we found that RapidArc increased the V10 Gy, V20 Gy and Dmean of the normal liver compared to IMRT and, therefore, we suggest that the RapidArc should be used more carefully when treating HCC cases even if both RapidArc and IMRT achieve equivalent V30 Gy for the normal liver and have similar NTCP values.
Another advantage of RapidArc over IMRT were the reduction in the number of MUs. Several studies have reported that the disadvantages of IMRT include higher MUs, longer delivery times, and more low-dose exposure of organs at risk (OARs), all of which increase the risk of a radiation-induced second malignancy. Hall reported that IMRT, as compared with 3DCRT, might double the incidence of solid cancers in long-term survivors, especially children [31]. Zwahlen studied the cancer risk after IMRT for cervical and endometrial cancer and reported that cumulative second cancer risks (SCR) relative to 3DCRT for 6-MV and 18-MV IMRT plans were +6% and +26%, respectively [32]. There is no sufficient data to demonstrate that the lower MUs associated with RapidArc might reduce the risk of radiation-induced second malignancy. Furthermore, radiation-induced second malignancy occurs only in those who have long-term survival after treatment. Xu et al. reported that the 5-year survival rate for HCC patients receiving TACE plus RT was only 13% with a median survival time of 18 months [33]. Thus this advantage of RapidArc may have little influence on the prevention of radiation-induced second malignancy for HCC patients. Verbakel WF et al. [16] and Wagner et al. [34] compared RapidArc with IMRT for different malignancies and concluded that the major advantages of RapidArc over IMRT were the lower MUs and the shorter treatment time, which can be beneficial to the reduction of intra-fractional movement, improving patient comfort, and higher patient throughput.
Although RapidArc has been demonstrated the advantages on the treatment of other kinds of malignancies, the dosimetric advantage of RapidArc in our study is not always better than IMRT. Therefore it is not convincing that IMRT should be replaced by RapidArc when treating HCC. The limitations of our study include small patient numbers, relatively coarse 5 mm-slice thickness and a lack of respiratory control or abdominal compression. These limitations would possibly cause some errors in the dose calculation and analysis. Clinical trials and long-term follow-up are required to draw more definite conclusions. Therefore, we suggest that if PTV conformity and percentages of NTCP, Dmean, V30 Gy and V10 Gy of the normal liver are acceptable, RapidArc may be selected on the basis of fewer MUs. If PTV coverage is not adequate or each of the above parameters related to liver toxicity is too high with RapidArc, then IMRT should be used.
In conclusion, RapidArc obtained favorable tumor coverage compared with IMRT and both RapidArc and IMRT achieved significantly better quality in terms of treatment plan when compared with 3DCRT. However, RapidArc is not superior to IMRT for liver protection. Nonetheless, RapidArc is a new technique, and optimization of its algorithm is still in its early stages (about 2 years of clinical experience), whereas 3DCRT and IMRT have been well-investigated and routinely used for more than 10 years. It is expected that more comprehensive planning systems for RapidArc are being developed and these might advance the optimization process in the future.
References
Bosch FX, Ribes J, Diaz M, Cleries R: Primary liver cancer: worldwide incidence and trends. Gastroenterology 2004, 127: S5-S16. 10.1053/j.gastro.2004.09.011
Ohto M, Yoshikawa M, Saisho H, Ebara M, Sugiura N: Nonsurgical treatment of hepatocellular carcinoma in cirrhotic patients. World J Surg 1995, 19: 42-46. 10.1007/BF00316978
Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S, Kim JS, Luo R, Feng J, Ye S, Yang TS, Xu J, Sun Y, Liang H, Liu J, Wang J, Tak WY, Pan H, Burock K, Zou J, Voliotis D, Guan Z: Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol 2009, 10: 25-34. 10.1016/S1470-2045(08)70285-7
Kuvshinoff BW, Ota DM: Radiofrequency ablation of liver tumors: influence of technique and tumor size. Surgery 2002, 132: 605-612. 10.1067/msy.2002.127545
Camma C, Schepis F, Orlando A, Albanese M, Shahied L, Trevisani F, Andreone P, Craxi A, Cottone M: Transarterial chemoembolization for unresectable hepatocellular carcinoma: meta-analysis of randomized controlled trials. Radiology 2002, 224: 47-54. 10.1148/radiol.2241011262
Tateishi R, Shiina S, Teratani T, Obi S, Sato S, Koike Y, Fujishima T, Yoshida H, Kawabe T, Omata M: Percutaneous radiofrequency ablation for hepatocellular carcinoma. An analysis of 1000 cases. Cancer 2005, 103: 1201-1209. 10.1002/cncr.20892
Stillwagon GB, Order SE, Guse C, Klein JL, Leichner PK, Leibel SA, Fishman EK: 194 hepatocellular cancers treated by radiation and chemotherapy combinations: toxicity and response: a Radiation Therapy Oncology Group Study. Int J Radiat Oncol Biol Phys 1989, 17: 1223-1229. 10.1016/0360-3016(89)90530-0
Lawrence TS, Robertson JM, Anscher MS, Jirtle RL, Ensminger WD, Fajardo LF: Hepatic toxicity resulting from cancer treatment. Int J Radiat Oncol Biol Phys 1995, 31: 1237-1248. 10.1016/0360-3016(94)00418-K
Tse RV, Guha C, Dawson LA: Conformal radiotherapy for hepatocellular carcinoma. Crit Rev Oncol Hematol 2008, 67: 113-123. 10.1016/j.critrevonc.2008.01.005
Dawson LA, McGinn CJ, Normolle D, Ten Haken RK, Walker S, Ensminger W, Lawrence TS: Escalated focal liver radiation and concurrent hepatic artery fluorodeoxyuridine for unresectable intrahepatic malignancies. J Clin Oncol 2000, 18: 2210-2218.
Emami B, Lyman J, Brown A, Coia L, Goitein M, Munzenrider JE, Shank B, Solin LJ, Wesson M: Tolerance of normal tissue to therapeutic irradiation. Int J Radiat Oncol Biol Phys 1991, 21: 109-122.
Dawson LA, Ten Haken RK: Partial volume tolerance of the liver to radiation. Semin Radiat Oncol 2005, 15: 279-283. 10.1016/j.semradonc.2005.04.005
Park HC, Seong J, Han KH, Chon CY, Moon YM, Suh CO: Dose-response relationship in local radiotherapy for hepatocellular carcinoma. Int J Radiat Oncol Biol Phys 2002, 54: 150-155.
Cheng JC, Wu JK, Huang CM, Liu HS, Huang DY, Tsai SY, Cheng SH, Jian JJ, Huang AT: Dosimetric analysis and comparison of three-dimensional conformal radiotherapy and intensity-modulated radiation therapy for patients with hepatocellular carcinoma and radiation-induced liver disease. Int J Radiat Oncol Biol Phys 2003, 56: 229-234. 10.1016/S0360-3016(03)00091-9
Fuss M, Salter BJ, Herman TS, Thomas CR Jr: External beam radiation therapy for hepatocellular carcinoma: potential of intensity-modulated and image-guided radiation therapy. Gastroenterology 2004, 127: S206-217. 10.1053/j.gastro.2004.09.035
Verbakel WF, Cuijpers JP, Hoffmans D, Bieker M, Slotman BJ, Senan S: Volumetric intensity-modulated arc therapy vs. conventional IMRT in head-and-neck cancer: a comparative planning and dosimetric study. Int J Radiat Oncol Biol Phys 2009, 74: 252-259. 10.1016/j.ijrobp.2008.12.033
Yoo S, Wu QJ, Lee WR, Yin FF: Radiotherapy treatment plans with RapidArc for prostate cancer involving seminal vesicles and lymph nodes. Int J Radiat Oncol Biol Phys 2010, 76: 935-942. 10.1016/j.ijrobp.2009.07.1677
Palma D, Vollans E, James K, Nakano S, Shaffer R, Mckenzie M, Morris J, Otto K: Volumetric modulated arc therapy for delivery of prostate radiotherapy: comparison with intensity-modulated radiotherapy and three-dimensional conformal radiotherapy. Int J Radiat Oncol Biol Phys 2008, 72: 996-1001. 10.1016/j.ijrobp.2008.02.047
Seong J, Park HC, Han KH, Chon CY: Clinical results and prognostic factors in radiotherapy for unresectable hepatocellular carcinoma: a retrospective study of 158 patients. Int J Radiat Oncol Biol Phys 2003, 55: 329-336. 10.1016/S0360-3016(02)03929-9
Cahlon O, Hunt M, Zelefsky MJ: Intensity-modulated radiation therapy: supportive data for prostate cancer. Semin Radiat Oncol 2008, 18: 48-57. 10.1016/j.semradonc.2007.09.007
Wang X, Zhang X, Dong L, Liu H, Gillin M, Ahamad A, Ang K, Mohan R: Effectiveness of noncoplanar IMRT planning using a parallelized multiresolution beam angle optimization method for paranasal sinus carcinoma. Int J Radiat Oncol Biol Phys 2005, 63: 594-601. 10.1016/j.ijrobp.2005.06.006
Warkentin B, Stavrev P, Stavreva N, Field C, Fallone BG: A TCP-NTCP estimation module using DVHs and known radiobiological models and parameter sets. J Appl Clin Med Phys 2004, 5: 50-63. 10.1120/jacmp.26.149
Burman C, Kutcher GJ, Emami B, Goitein M: Fitting of normal tissue tolerance data to an analytic function. Int J Radiat Oncol Biol Phys 1991, 21: 123-135.
Wulf J, Guckenberger M, Haedinger U, Oppitz U, Mueller G, Baier K, Flentje M: Stereotactic radiotherapy of primary liver cancer and hepatic metastases. Acta Oncol 2006, 45: 838-847. 10.1080/02841860600904821
Cheng JC, Wu JK, Lee PC, Liu HS, Jian JJ, Lin YM, Sung JL, Jan GJ: Biological susceptibility of hepatocellular carcinoma patients treated with radiotherapy to radiation-induced liver disease. Int J Radiat Oncol Biol Phys 2004, 60: 1502-1509. 10.1016/j.ijrobp.2004.05.048
Dawson LA, Normolle D, Balter JM, McGinn CJ, Lawrence TS, Ten Haken RK: Analysis of radiation-induced liver disease using the Lyman NTCP model. Int J Radiat Oncol Biol Phys 2002, 53: 810-821. 10.1016/S0360-3016(02)02846-8
Yamada K, Izaki K, Sugimoto K, Mayahara H, Morita Y, Yoden E, Matsumoto S, Soejima T, Sugimura K: Prospective trial of combined transcatheter arterial chemoembolization and three-dimensional conformal radiotherapy for portal vein tumor thrombus in patients with unresectable hepatocellular carcinoma. Int J Radiat Oncol Biol Phys 2003, 57: 113-119. 10.1016/S0360-3016(03)00434-6
Shueng PW, Lin SC, Chang HT, Chong NS, Chen YJ, Wang LY, Hsieh YP, Hsieh CH: Toxicity risk of non-target organs at risk receiving low-dose radiation: case report. Radiat Oncol 2009, 4: 71. 10.1186/1748-717X-4-71
Yamashita H, Nakagawa K, Nakamura N, Koyanagi H, Tago M, Igaki H, Shiraishi K, Sasano N, Ohtomo K: Exceptionally high incidence of symptomatic grade2–5radiation pneumonitis after stereotactic radiation therapy for lung tumors. Radiat Oncol 2007, 2: 21. 10.1186/1748-717X-2-21
Xu ZY, Liang SX, Zhu J, Zhu XD, Zhao JD, Lu HJ, Yang YL, Chen L, Wang AY, Fu XL, Jiang GL: Prediction of radiation-induced liver disease by Lyman normal-tissue complication probability model in three-dimensional conformal radiation therapy for primary liver carcinoma. Int J Radiat Oncol Biol Phys 2006, 65: 189-195. 10.1016/j.ijrobp.2005.11.034
Hall EJ: Intensity-modulated radiation therapy, protons, and the risk of second cancers. Int J Radiat Oncol Biol Phys 2006, 65: 1-7. 10.1016/j.ijrobp.2006.01.027
Zwahlen DR, Ruben JD, Jones P, Gagliardi F, Millar JL, Schneider U: Effect of intensity-modulated pelvic radiotherapy on second cancer risk in the postoperative treatment of endometrial and cervical cancer. Int J Radiat Oncol Biol Phys 2009, 74: 539-545. 10.1016/j.ijrobp.2009.01.051
Xu LT, Zhou ZH, Lin JH, Chen Z, Wang K, Wang P, Zhu XY, Shen YH, Meng ZQ, Liu LM: Clinical study of transarterial chemoembolization combined with 3-dimensional conformal radiotherapy for hepatocellular carcinoma. Eur J Surg Oncol 2011, 37: 245-251.
Wagner D, Christiansen H, Wolff H, Vorwerk H: Radiotherapy of malignant gliomas: comparison of volumetric single arc technique (RapidArc), dynamic intensity-modulated technique and 3D conformal technique. Radiother Oncol 2009, 93: 593-596. 10.1016/j.radonc.2009.10.002
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
YCK and HWY contributed significantly to study design and concept. YCK also contributed to manuscript writing and study coordinator. YMC and CWC contributed to statistical analysis. WPS and WCL contributed significantly to the acquisition of data and optimization of treatment plans. PFW and JJH contributed to final revision of manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Kuo, YC., Chiu, YM., Shih, WP. et al. Volumetric intensity-modulated Arc (RapidArc) therapy for primary hepatocellular carcinoma: comparison with intensity-modulated radiotherapy and 3-D conformal radiotherapy. Radiat Oncol 6, 76 (2011). https://doi.org/10.1186/1748-717X-6-76
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1748-717X-6-76