Abstract
Background
Free radical mediated oxidative stress is mainly involved in the pathogenesis of diabetic complications. Proteins and lipids are among the prime targets for oxidative stress. In the present study, we evaluated the oxidative stress in chronic IDDM patients by estimating the lipid peroxidation, protein oxidation, and antioxidants status.
Subjects and design
A total of 35 (15 IDDM + 20 normal healthy) children were examined in the study and estimated the lipid peroxidation, protein oxidation, and antioxidants – vitamin A (β-carotene, retinol), vitamin C, vitamin E and enzymatic antioxidants and nitric oxide.
Results
A statistically significant higher values of protein carbonyl groups and MDA as lipid peroxides were observed in diabetic patients with slight reduction in the synthesis of nitric oxide. It is interesting to note that there was a decrease in the antioxidant levels with corresponding increased protein and lipid oxidation. On PAGE under native conditions, we observed decreased levels of proteins – albumin, transferrin, ceruloplasmin and heptoglobulins and variable GC globulin fractions in IDDM compared to normal healthy controls.
Conclusion
Hyperglycemia induces the overproduction of oxygen free radicals and consequently increases the protein oxidation and lipid oxidation. A significance difference in the mean plasma concentration of total antioxidant status was observed in IDDM patients. The findings of the present study suggest that diabetes in an altered metabolic state of oxidation-reduction and that it is convenient to give therapeutic interventions with antioxidants.
Similar content being viewed by others
Background
Free radicals are very reactive chemical species, can cause oxidation injury to the living beings by attacking the macromolecules like lipids, carbohydrates, proteins and nucleic acids. Under normal physiological conditions, there is a critical balance in the generation of oxygen free radicals and antioxidant defense systems used by organisms to deactivate and protect themselves against free radical toxicity [1, 2]. Impairment in the oxidant/antioxidant equilibrium creates a condition known as oxidative stress. Oxidative stress is known to be a component of molecular and cellular tissue damage mechanisms in a wide spectrum of human diseases [3–5].
Diabetes is associated with a number of metabolic alterations and principal among these is hyperglycemia. The precise mechanism by which hyperglycemia may contribute to the development of coronary heart disease (CHD) is a matter of some controversy. Known sequelae of hyperglycemia such as cellular damage, increased extra cellular matrix production and vascular dysfunction have all been implicated in the pathogenesis of vascular disease in type I and type II diabetes [3, 5–10]. Mechanisms involved in the increased oxidative stress in diabetes include not only oxygen free radical generation due to nonenzymatic glycosylation (glycation), autooxidation of glycation products, but also changes in the tissue content and activity of antioxidant defense systems. Increased levels of the products of oxidative damage to lipids have been detected in serum of diabetic patients, and their presence correlates with the development of complications [6, 10–15]. A variety of natural antioxidants exist to scavenge oxygen free radicals and prevent oxidative damage to biological membranes. One group of these antioxidants is enzymatic (intracellular), which include super oxide dismutase, glutathione peroxidase and catalase. In addition to enzymatic antioxidants, the major natural antioxidants, most of them derived from natural sources by dietary intake are vitamin A, vitamin C and vitamin E and carotenoids. Also, numerous small molecules are synthesized or produced within the body that has antioxidant capacity (e.g. glutathione and uric acid) [3, 6, 14–18].
There are several studies evaluated the free radical induced lipid peroxidation and the antioxidants in diabetic patients. Many of these studies assessed individual antioxidants that act cooperatively in vivo to provide greater protection to the organism against free radical damage than could be provided by any single antioxidant acting alone. Controversial reports have been reported concerning the antioxidant status in diabetic patients [17, 19–21]. Protein oxidation, in contrast to lipid peroxidation, does not have the features of chain reactions. The plasma proteins destructed by peroxidation have a quite long period. Therefore, the evaluation of protein oxidation (PCG) in plasma is a respected marker of free radical intensity. There are only a few reports regarding the protein oxidation in various other pathogenic conditions and no reports are available for that processes along with antioxidants in type I diabetic patients. The aim of the present study was to evaluate the free radical reaction intensity in chronic diabetic IDDM patients on basis of protein carbonyl groups of proteins, lipid peroxidation and the status of antioxidants in plasma.
Subjects and methods
Subjects
A total of 35 (15 IDDM + 20 normal healthy) children were examined in the study. Based on preliminary survey, all 15 patients are treated but controlled who had the high levels of blood glucose and glycosylated hemoglobin (Gly-Hb), well above the normal ranges, were selected for the study. These children were treated with insulin, had no other medications and they had no supplemental intake of vitamins or other nutrients. The remaining 20 age-matched healthy children were chosen from the community and used as control subjects. Non-fasting heparinized venous blood samples were collected from each subject with their/parental prior consent.
The total plasma proteins were measured by biuret method, plasma albumin was measured by a colorimetric method based on the bromocresol green dye at pH 4.2 giving a colored complex [22]. Protein Oxidation was evaluated by measuring carbonyl group content in plasma proteins is a marker of free radical activity. It was measured with use of Levine method [23]. 100 μl of plasma was incubated with a 100 μl of 20 mM 2, 4-dinitrophenylhydrazine (DNPH) for 60 min. Subsequently, the protein was precipitated from the solution with the use of 20 % trichloroaceticacid. Then it was washed three times in the solution of ethanol and ethylacetate and dissolving in 1 ml of 6 M guanidine HCl in 60°C. The carbonyl group content was evaluated in a spectrophotometer at wavelength 360 nm. The results were expressed as μmol/mg of protein. The lipid peroxidation in terms of MDA was estimated by using TBARS method [24].
From all subjects, 5 – 8 ml of blood was collected in heparinized tubes at 8.00 AM after an overnight fast and immediately centrifuged at 1500 × g for 15 min at 4 C. Plasma and pelleted RBC were separated stored in eppendorf tubes and kept at -80 C until analysis. We measured SOD, GPx and catalase activity in plasma according to the methods of Beutler [25], Flohe and Gunzler [26] and Renu et al. [27]. The vitamin A and β-carotene, ascorbic acid, α-tocopherol and glutathione spectrophotometrically determined by Carr-Price reaction, DNP method and TLC methods [24]. Nitric oxide estimated in plasma by the method of Moshage et al. [28]. Electrophoresis was carried out in 10% polyacrylamide slab gels, according to the method of Laemmli [29].
Statistical analysis
Statistical analysis was performed by Minitab software. Subjects with IDDM were compared with healthy controls. Means and standard error of means were calculated and differences between means were student's t-test. The strength of association between pairs of variables was assessed by Pearson correlation coefficient. The level of significance was set at p < 0.05.
Results
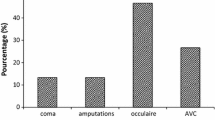
The biochemical particulars of the study subjects including IDDM and non-diabetic controls are given in table 1. The subjects with diabetes had duration of the disease ranged from 5 – 10 years. They all were being treated with insulin. Despite of their treatment, they had hyperglycemia having blood glucose levels more than 3-fold higher than in healthy subjects. The lipid profile of IDDM is statistically insignificant changes with nondiabetics. However, the TBARS (lipid peroxidation) levels increased by 4 fold in diabetics compared to healthy controls (table 2). No significant differences were found between patients with type 1 diabetes and control subjects in the concentration of total, HDL, and LDL cholesterol and triglycerides in age and in BMI.
The protein oxidation (PCG) in IDDM subjects was increased 3.5 fold with decreasing the plasma levels of total protein, albumin, globulin and their ratio compared to non-diabetic subjects. In native PAGE (not shown), the diabetic children had also decreased plasma levels of ceruloplasmin, ceruloglobulin and retinol binding protein (RBP), which are the carrier proteins for copper and vitamin A, respectively and also observed the decreased levels of proteins – albumin, transferrin, and heptoglobulins and variable GC globulin fractions in IDDM compared to normal healthy controls. Table 3 shows a significant decrease in the activities Cu-Zn super oxide dismutase, glutathione peroxidase and catalase in children with IDDM compared to controls. The glutathione peroxidase in the whole blood was also decreased in diabetic children, but their differences with those of the non-diabetic counterparts were not statistically significant. The antioxidant activity containing vitamins retinol, β-carotene, vitamin C and vitamin E were significantly decreased in plasma by 25 – 50 % respectively in diabetic children.
Discussion
Diabetes mellitus is a chronic, systemic, metabolic disease defined by hyperglycemia and characterized by alterations in the metabolism of carbohydrate, protein and lipid. Oxidative stress thought to be increased in a system where the rate of free radical production is increased and/or the antioxidant mechanisms are impaired. In recent years, the oxidative stress-induced free radicals have been implicated in the pathology of IDDM [14, 19, 30–34].
The present study was examined the changes in both extra and intracellular antioxidants and oxidant status in a children suffering from IDDM. The diabetic children were treated with insulin and yet they were hyperglycemic. Prolonged exposure to hyperglycemia and consequent non-enzymatic posttranslational modification of proteins resulting from chemical reaction between glucose and primary amino groups of proteins – glycation, and also increased oxygen free radicals through auto oxidation of glucose [15, 33–36]. Our results are in accordance with those of previous finding clearly show the increased glucose levels induces diabetes, the overproduction of oxygen free radicals and consequently increases the protein oxidation and lipid oxidation (table 2). Plasma MDA and PCG levels were significantly higher, which would indicate that free radical mediated oxidative damage of lipids and proteins is produced at in diabetics [35, 42, 42]. To our knowledge, there are no reports in the literature concerning plasma PCG levels in IDDM patients in relation with antioxidant status. Carbonyl group formation is considered an early and stable marker for protein oxidation. Oxidized proteins constitute a substantial fraction of the catalytically inactive or less active forms of enzymes, which may have direct metabolic consequences [37–41]. According to Gliesner et al [35] showed no statistically significant differences were found for any of the oxidative stress markers (PCG) assessed between patients with DM1 and controls. In addition, weight, height, and routine metabolic tests, including creatininemia and cholesterol levels, were similar between the groups. The lack of significant differences between healthy controls and patients with DM1 suggested that treatment is able to counteract the increase in free radical production. Ahmed et al [41] observed profound increases in proteolytic products of glycated and oxidised proteins in diabetic patients, concurrent with much lower increases in protein glycation and oxidation adduct residues.
Nitric oxide (NO) is an important vascular target for ROS. Superoxide neutralizes NO, and the peroxynitrite formed is a source of hydroxyl radicals that can cause endothelial damage [43]. Increased levels of nitric oxide were observed in Type I DM (table 2). Astaneie et al [44] have shown the elevated levels of NO with total antioxidant power. Existence of increased total antioxidant power in the presence of normal lipid peroxidation in plasma of type I diabetic patients indicates the existence of oxidative stress. Oxidative stress therefore diminishes vessel endothelium-dependent relaxation, which is apparent in some experimental preparations even after acute exposure to hyperglycemia. Defective endothelium-dependent relaxation has been observed in chronic diabetic animals, and also in type 1 and type 2 diabetic subjects [41, 45, 46] and is an important potential target for antioxidant treatment.
The relationship between hyperglycemia and oxygen free radicals is supported by our results demonstrating an association between blood levels of glucose and enzymatic oxidants such as super oxide dismutase and glutathione peroxidase, only in children with IDDM (table 3). The decreased erythrocyte Cu/Zn-SOD and catalase activity in our young diabetic patients also supports the hypothesis of radical mediated injury in this disease. These results are in agreement with others [47–49]. Circulating RBC act as a sink for free radicals. Consequently, erythrocytes are subject to a continuous flux of O2 and H2O2. It is, therefore, possible that SOD may have an important physiological role in combating this process, since this enzyme can catalyze the dissimulation of two super oxide radicals into H2O2. In the present study, on native PAGE, the plasma concentration of ceruloplasmin in IDDM was significantly lower than those of controls. These results are in agreement with others [50] who reported a significant reduction in the plasma concentration of ceuloplasmin in type I diabetic patients. It has been reported that ceruloplasmin is immunologically altered with decrease in enzymatic oxidants. These results may explain the significant reduction in SOD activity in IDDM patients, since increased H2O2 and decreased ceruloplasmin [51]. Selenium-dependent glutathione peroxidase (GPx), which works in parallel with SOD, protects cell proteins and cell membranes against oxidative damage. In the present sudy, the GPx activity was decreased significantly compared to that of the controls and a negative correlation coefficient between GPx activity and blood glucose concentration was observed in these children (table 3). However, in the published lieterature, the GPx response to diabetes has been conflicting. Diabetics have been reported to be associated with increased [48, 52] decreased [53] or unchanged [54]. In lieu with GPx, the catalase activities were also decreased in diabetes compared to control subjects (table 3). The low GPx activity could be directly explained by either low GSH content or enzyme inactivation under sever oxidative stress.
In addition to antioxidant enzyme activities, the capacity of the antioxidant system to cope with or trap the free radicals generated under normal or pathological conditions was evaluated by measuring the level of total antioxidant status. It reflects the status of α-tocopherol, vitamin A, β-carotene, ascorbic acid, albumin, uric acid and other antioxidants [42, 49, 57]. These extracellular nonenzymatic antioxidants delay or inhibit the oxidative process. Enhanced lipid peroxidation increases the need for lipid soluble antioxidants, such as α-tocopherol and vitamin A and β-carotene. A significance difference in the mean plasma concentration of total antioxidant status was observed in IDDM patients (table 3). Low levels of vitamin E are associated with increased incidence of diabetes and some research suggests that people with diabetes have decreased levels of antioxidants [32, 42, 55]. People with diabetes may also have greater antioxidant requirements because of increased production of free radicals in hyperglycemia [56]. The results of Martin-Gallan et al [42] clearly show systemic peroxidative damage associated with insufficient defense mechanisms against ROS to be already present at clinical onset of type 1 diabetes mellitus in children and adolescents. The present study has also demonstrated a significantly lower plasma ascorbate children compared with their controls. A significant negative correlation coefficient between blood glucose and vitamin C has been observed. Patients with diabetes or the metabolic syndrome have low levels of the antioxidant vitamin C [58, 59] and also control the diabetes [33]. Chen et al [59] shown that high-dose oral vitamin C partially replenishes vitamin C levels in patients with Type 2 diabetes and low vitamin C levels but does not improve endothelial dysfunction or insulin resistance.
The findings of the present study suggest that diabetes in an altered metabolic state of oxidation-reduction and that it is convenient to give therapeutic interventions with antioxidants. The loss of antioxidant capacity is statistically associated with accelerated aging processes in diabetic patients, due to an increase in basal oxidation products of etrythrocytes associated with monosaccharide autooxidative glycation [4, 11, 18, 60]. Our present work takes into account the hypothesis involving the relation between individual components in the intact clinical model and the complex oxidant-antioxidant plasmatic systemic balance. We clearly identified antioxidant markers that were affected in the presence of IDDM; include SOD, plasma albumin, ascorbic acid and α-tocopherol. Theoretically, one should be able to reverse these effects through dietary supplementation, especially of vitamin C and E.
Abbreviations
- IDDM:
-
Insulin dependent diabetes mellitus
- PAGE:
-
Polyacrylamide gel electrophoresis
- MDA:
-
Melondialdehyde
- PCG:
-
Protein carbonyl groups
- TBARS:
-
Thiobarbutyricacid reactives species
- TLC:
-
Thin layer chromatography
- GPx:
-
Glutathione peroxidase
- NO:
-
Nitric oxide
- SOD:
-
Superoxide dismutase
References
Sies H: Oxidative stress: Oxidants and antioxidants. 1991, New York, Academic press
Halliwell B, Whiteman M: Measuring reactive species and oxidative damage in vivo and in cell culture: how should you do it and what do the results mean? [Review]. Br J Pharmacol. 2004, 142: 231-55. 10.1038/sj.bjp.0705776.
Halliwell B, Gutteridge JMC: Free radicals in biology and medicine. 1999, New York: Oxford University Press, 936-
Halliwell B: Role of free radicals in the neurodegenerative diseases: therapeutic implications for antioxidant treatment [Review]. Drugs Aging. 2001, 18: 685-716. 10.2165/00002512-200118090-00004.
Isabella Dalle-Donne, Rossi Ranieri, Colombo Roberto, Giustarini Daniela, Milzani Aldo: Biomarkers of Oxidative Damage in Human Disease. Clinical Chemistry. 2006, 52 (4): 601-623. 10.1373/clinchem.2005.061408.
Maritim AC, Sanders RA, Watkins JB: Diabetes, oxidative stress, and antioxidants: a review. J Biochem Mol Toxicol. 2003, 17: 24-38. 10.1002/jbt.10058.
Stephens Jeffrey, Gable David, Hurel Steven, Miller George, Cooper Jackie, Humphries Steve: Increased Plasma Markers of Oxidative Stress Are Associated with Coronary Heart Disease in Males with Diabetes Mellitus and with 10-Year Risk in a Prospective Sample of Males. Clinical Chemistry. 2006, 52 (3): 446-452. 10.1373/clinchem.2005.060194.
Ruderman NB, Williamson JR, Brownlee M: Glucose and diabetic vascular disease. FASEB J. 1992, 6 (11): 2905-14.
American Diabetic Association: Guidelines. Standards of medical care in Diabetes. Diabetes Care. 2005, 28 (Supplement 1): S4-36. 10.2337/diacare.28.suppl_1.S4.
Guillermo Zalba, Fortuño Ana, Díez Javier: Oxidative stress and atherosclerosis in early chronic kidney disease. Nephrol Dial Transplant. 2006, 21: 2686-2690. 10.1093/ndt/gfl398.
Wolff SP: Diabetes mellitus and free radicals. Free radicals, transition metals and oxidative stress in the etiology of diabetes mellitus and complications. Br Med Bull. 1993, 49: 642-652.
Brownlee M: Biochemistry and molecular cell biology of diabetic complications. Nature. 2001, 414: 813-820. 10.1038/414813a.
Wieruszwysocka B, Wysocki H, Byks H, Zozulinska D, Wykretowicz A, Kazierczak M: Metabolic control quality and free radical activity in diabetic patients, Diabetes Res. Clin Pract. 1995, 27: 193-197.
Heistad Donald: Oxidative Stress and VascularDisease. Arterioscler Thromb Vasc Biol. 2005, 26: 689-95. 10.1161/01.ATV.0000203525.62147.28.
Liu Xi Shang, Hou Fan Fan, Guo Jian Zhi, Nagai Ryoji, Zhang Ru Wei, Liu Qiang Zhi, Zhou Mei Zhan, Zhou Mei, Di Xie , Wang Bao Guo, Zhang Xun: Advanced Oxidation Protein Products Accelerate Atherosclerosis Through Promoting Oxidative Stress and Inflammation. Arterioscler Thromb Vasc Biol. 2006, 26: 1156-1162. 10.1161/01.ATV.0000214960.85469.68.
Azen SP, Qian D, Mack WJ, Sevanian A, Selzer RH, Liu CR, Liu CH, Hodis HN: Effect of supplementary antioxidant vitamin intake on carotid arterial wall intima-media thickness in a controlled clinical trial of cholesterol lowering. Circulation. 1996, 94: 2369-2372.
Heart Protection Study Collaborative Group: MRC/BHF Heart Protection Study of antioxidant vitamin supplementation in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002, 360: 23-33. 10.1016/S0140-6736(02)09328-5.
Engler MM, Engler MB, Malloy MJ, Chiu EY, Schloetter MC, Paul SM, Stuehlinger M, Lin KY, Cooke JP, Morrow JD, Ridker PM, Rifai N, Miller E, Witztum JL, Mietus-Snyder M: Antioxidant vitamins C and E improve endothelial function in children with hyperlipidemia: Endothelial Assessment of Risk from Lipids in Youth (EARLY) Trial. Circulation. 2003, 108: 1059-1063. 10.1161/01.CIR.0000086345.09861.A0.
Ashour M, Salem S, Hassaneen H, EL-Gadban H, Elwan N, Awad A, Basu TK: Antioxidant status and insulin dependent diabetes mellitus (IDDM). J Clin Biochem Nutr. 1999, 26: 99-107.
Marra Giampiero, Cotroneo Patrizia, Pitocco Dario, Manto Andrea, diLeo Mauro, Ruotolo Valeria, Caputo Salvatore, Giardina Bruno, Phirlanda Iovanni, Santini Stefano: Early Increase of Oxidative Stress and Reduced Antioxidant Defenses in Patients with Uncomplicated Type 1 Diabetes. Diabetes Care. 2002, 25: 370-375. 10.2337/diacare.25.2.370.
Rice-Evans C, Miller NJ: Total antioxidant status in plasma and body fluids. Methods Enzymol. 234: 279-293.
Doumas BT, Watson WA, Biggs HG: Albumin standards and the measurement of serum albumin with bromocresol green. Clin Chem Acta. 1971, 31: 87-10.1016/0009-8981(71)90365-2.
Levine RL, Garland D, Oliver CN, Amici A, Climent I, Lenz AG, Ahn BW, Shaltiel S, Stadman ER: Determination of carbonyl content in oxidatively modified proteins. Methods in Enzymology. Edited by: Pecker L, Glazer AN. 1990, New York, Academic, 186: 464-478.
Raghuramulu N, Madhavan Nair K, Kalyanasundaram S: A manual of laboratory techniques. 2003, National Institute of Nutrition, Hyderabad. India
Beutler E: Red cell metabolism. A manual of biochemical methods. 1984, New York, 3
Flohe L, Gunzler WA: Assays of glutathione peroxidase, Methods enzymol. 1984, 105: 114-121.
Renu AK, Timothy SK, Engerman RL: Abnormalities of retinol metabolism in diabetes or experimental galactosemia. Free radical Biol Med. 1997, 22 (4): 587-92.
Moshage H, Kok B, Huizenga JR, Jansen PLM: Nitrite and nitrate determinations in plasma: A critical evaluation. Clin Chem. 1995, 41/6: 892-896.
Laemmli UK: Cleavage of structural proteins during the assembly of the head bacteriophage T4. Nature. 1970, 227: 680-685. 10.1038/227680a0.
Maiese K, Morhan SD, Chong ZZ: Oxidative stress biology and cell injury during type 1 and type 2 diabetes mellitus. Curr Neurovasc Res. 2007, 4 (1): 63-71. 10.2174/156720207779940653.
Kaneto H, Katekami N, Kawamori D, Miyatsuka T, Sakamotot K, Matsuoka TA, Matsuhisa M: Involvement of oxidative stress in the pathogenesis of diabetes. Antioxid Redox Signal. 2007, 9: 355-66. 10.1089/ars.2006.1465.
Quilliot Didier, Walters Evelyne, Bonte Jean-Paul, Fruchart Jean-Charles, Duriez Patrick, Ziegler Olivier: Diabetes mellitus worsens antioxidant status in patients with chronic pancreatitis. Am J Clin Nutr. 2005, 81: 1117-25.
Ceriello A, Kumar S, Picon L, Esposito K, Giugliano D: Simultaneous control of hyperglycemia and oxidative stress normalizes endothelial function in type I diabetes. Diabetes care. 2007, 30: 649-54. 10.2337/dc06-2048.
Hsu WT, Tsai LY, Lin SK, Hsiao K, Chen BH: Effects of diabetes duration and glycemic control on free radicals in children with type 1 diabetes mellitus. Ann Clin Lab Sci. 2006, 36: 174-8.
Gleisner A, Martinez L, Pino R, Rojas IG, Martinez A, Asenjo S, Rudolph MI: Oxidative stress markers in plasma and urine of prepubertal patients with type 1 diabetes mellitus. J Pediatr Endocrinol Metab. 2006, 19: 995-1000.
Wolff SP, Jiang Z, Hunt J: Protein glycation and oxidative stress in diabetes mellitus and aging. Free Radical Biol Med. 1991, 10 (5): 339-352. 10.1016/0891-5849(91)90040-A.
Dominguez C, Ruiz E, Gussinye M, Carrascisa A: Oxidative stress at onset and in early stages of type I diabetes in children and adolescents. Diabetes care. 1998, 21: 1736-42. 10.2337/diacare.21.10.1736.
Hartnett ME, Stratton RD, Browne Rw, Rosner BA, Lanham RJ, Armstrong D: Serum markers of oxidative stress and severity of diabetic retinopathy. Diabetes Care. 2000, 23 (2): 234-40. 10.2337/diacare.23.2.234.
Matteucci E, Giampietro O: Oxidation stress in families of type I diabetic patients. Diabetic Care. 2000, 23 (8): 1182-6. 10.2337/diacare.23.8.1182.
Kalousova M, Skrha J, Zima T: Advanced glycation end products and advanced oxidation protein products in-patients with diabetes mellitus. Physio Res. 2002, 51: 597-604.
Ahmed N, Babaei-Jadidi R, Howell SK, Thornalley PJ, Beisswenger PJ: Glycated and oxidized protein degradation products are indicators of fasting and postprandial hyperglycemia in diabetes. Diabetes Care. 2005, 28: 2465-71. 10.2337/diacare.28.10.2465.
Martin-Gallan P, Carrascisa A, Gussinye M, Dominguez C: Estimation of lipoperoxidative damage and antioxidant status in diabetic children: relationship with individual antioxidants. Free Radic Res. 2005, 39: 933-42. 10.1080/10715760500156751.
Elliott TG, Cockcroft JR, Groop PH, Viberti GC, Ritter JM: Inhibition of nitric oxide synthesis in forearm vasculature of insulin-dependent diabetic patients: blunted vasoconstriction in patients with microalbuminuria. Clin Sci. 1993, 85: 687-693.
Astaneie F, Afshari M, Mojtahedi A, Mostafalou S, Zamani MJ, Larijani B, Abdollahi M: Total antioxidant capacity and levels of epidermal growth factor and nitric oxide in blood and saliva of insulin-dependent diabetic patients. Arch Med Res. 2005, 36: 376-81. 10.1016/j.arcmed.2005.03.007.
Beckman JS, Beckman TW, Chen J, Marshall PA, BA: Apparent hydroxyl radical production by peroxynitrite: implications for endothelial injury from nitric oxide and superoxide. Proc Natl Acad Sci USA. 1990, 87: 1620-1624. 10.1073/pnas.87.4.1620.
Seckin D, Ilhan N, Ilhan N, Ertugrul S: Glycaemic control, markers of endothelial cell activation and oxidative stress in children with type 1 diabetes mellitus. Diabetes Res Clin Pract. 2006, 73: 191-77. 10.1016/j.diabres.2006.01.001.
Kawamura N, Ookawara T, Suzuki K, Konishi K, Mino M, Taniguchi NC: Increased glycated Cu, Zn superoxide dismutase levels in erythrocytes of patients with insulin dependent diabetes mellitus. J Clin Endocrinol Metab. 1992, 74: 1352-1354. 10.1210/jc.74.6.1352.
Djordjevic A, Spasic S, Jovanovic-Galovic A, Djordjevic R, Grubor-Lajsic G: Oxidative stress in diabetic pregnancy: SOD, CAT and GSH-Px activity and lipid peroxidation products. J Matern Fetal Neonatal Med. 2004, 16: 367-72. 10.1080/14767050400018270.
Peuchant E, Brun JL, Rigalleau V, Dubourg L, Thomas MJ, Daniel JY, Leng JJ, Gin H: Oxidative and antioxidative status in pregnant women with either gestational or type 1 diabetes. Clin Biochem. 2004, 37: 293-98. 10.1016/j.clinbiochem.2003.12.005.
Asayama K, Uchida N, Nakan T, Dobaski K: Antioxidants in the serum of children with insulin dependent diabetes mellitus. Free Radical Biol Med. 1993, 15: 597-602. 10.1016/0891-5849(93)90162-N.
Diamon M, Susa S, Yamatani K, Manaka H, Hama K, Kimura M, Ohnuma H, Kato T: Hyperglycemia is a factor for an increase in serum ceruloplasmin in type II diabetes. Diabetes Care. 1997, 21 (9): 1525-28. 10.2337/diacare.21.9.1525.
Ndahimana J, Dorchy H, Vertongen EC: Erythrocyte and plasma antioxidant activity in type I diabetes mellitus. Press Med. 1996, 25: 188-192.
Dominguez C, Ruiz E, Gussinye M, Carrascisa A: Oxidative stress at onset and in early stages of type I diabetes in children and adolescents. Diabetes care. 1998, 21: 1736-42. 10.2337/diacare.21.10.1736.
Faure P, Benhamou PY, Perard A, Halimi S, Roussel AM: Lipid peroxidationin insulin dependent diabetic patients with early retina degenerative lesions: Effects of an oral zinc supplementation. Eur J Clin Nutr. 1995, 49: 282-288.
Polidori MC, Mecocci P, Stahl W, Parente B, Cecchetti R, Cherubini A, Cao P, Sies H, Senin U: Plasma levels of lipophilic antioxidants in very old patients with type 2 diabetes. Diabetes Metab ResRev. 2000, 16: 15-19. 10.1002/(SICI)1520-7560(200001/02)16:1<15::AID-DMRR71>3.0.CO;2-B.
Sharma A, Kharb S, Chugh SN, Kakkar R, Singh GP: Evaluation of oxidative stress before and after control of glycemia and after vitamin E supplementation in diabetic patients. Metabolism. 2000, 49: 160-162. 10.1016/S0026-0495(00)91117-X.
Ford Earl, Mokdad Ali, Giles Wayne, Brown David: The Metabolic Syndrome and Antioxidant Concentrations. Diabetes. 2003, 52: 2346-2352. 10.2337/diabetes.52.9.2346.
Will JC, Byers T: Does diabetes mellitus increase the requirement for vitamin C?. Nutr Rev. 1996, 54: 193-202.
Chen Hui, Karne Rajaram, Hall Gail, Campia Umberto, Panza Julio, Cannon Richard, Wang Yaohui, Katz Arie, Levine Mark, Quon Michael: High-dose oral vitamin C partially replenishes vitamin C levels in patients with Type 2 diabetes and low vitamin C levels but does not improve endothelial dysfunction or insulin resistance. Am J Physiol Heart Circ Physiol. 2006, 290: H137-H145. 10.1152/ajpheart.00768.2005.
Tiwari AK: Antioxidants: New generation therapeutic base for treatment of polygenic disorders. Current Science. 2004, 86 (8): 1092-1102.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Ramakrishna, V., Jailkhani, R. Evaluation of oxidative stress in Insulin Dependent Diabetes Mellitus (IDDM) patients. Diagn Pathol 2, 22 (2007). https://doi.org/10.1186/1746-1596-2-22
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1746-1596-2-22