Abstract
Background
Sufficient levels of physical activity provide cardio-protective benefit. However within developed society sedentary work and inflexible working hours promotes physical inactivity. Consequently to ensure a healthy workforce there is a requirement for exercise strategies adaptable to occupational time constraint. This study examined the effect of a 12 week aerobic exercise training intervention programme implemented during working hours on the cardiovascular profile of a sedentary hospital workforce.
Methods
Twenty healthy, sedentary full-time staff members of the North West London Hospital Trust cytology unit were randomly assigned to an exercise (n = 12; mean ± SD age 41 ± 8 years, body mass 69 ± 12 kg) or control (n = 8; mean ± SD age 42 ± 8 years, body mass 69 ± 12 kg) group. The exercise group was prescribed a progressive aerobic exercise-training programme to be performed 4 times a week for 8 weeks (initial intensity 65% peak oxygen consumption (VO2 peak)) and to be conducted without further advice for another 4 weeks. The control was instructed to maintain their current physical activity level. Oxygen economy at 2 minutes (2minVO2), 4 minutes (4minVO2), VO2 peak, systolic blood pressure (SBP), diastolic blood pressure (DBP), BMI, C-reactive protein (CRP), fasting glucose (GLU) and total cholesterol (TC) were determined in both groups pre-intervention and at 4 week intervals. Both groups completed a weekly Leisure Time Questionnaire to quantify additional exercise load.
Results
The exercise group demonstrated an increase from baseline for VO2 peak at week 4 (5.8 ± 6.3 %) and 8 (5.0 ± 8.7 %) (P < 0.05). 2minVO2 was reduced from baseline at week 4 (-10.2 ± 10.3 %), 8 (-16.8 ± 10.6 %) and 12 (-15.1 ± 8.7 %), and 4minVO2 at week 8 (-10.7 ± 7.9 %) and 12 (-6.8 ± 9.2) (P < 0.05). There was also a reduction from baseline in CRP at week 4 (-0.4 ± 0.6 mg·L-1) and 8 (-0.9 ± 0.8 mg·L-1) (P < 0.05). The control group showed no such improvements.
Conclusion
This is the first objectively monitored RCT to show that moderate exercise can be successfully incorporated into working hours, to significantly improve physical capacity and cardiovascular health.
Similar content being viewed by others
Background
It is widely accepted that cardiovascular disease (CVD) is the leading cause of death in developed countries [1]. Over the past decade it has become recognised that physical activity is an independent factor in the determination of over all CVD risk through the prevention of atherosclerosis and reduction of thrombotic risk [2, 3]. Evidence supports an inverse association between physical fitness and various CVD risk factors, including glucose tolerance [4], cholesterol [5], blood pressure [6], resting pulse rate [7] and obesity [8], and markers of systemic inflammation including C-reactive protein (CRP) [9], and TNFα [10]. It is suggested that such effects occur through a reduction in lipoprotein oxidation [11], improved endothelial function via the increased production of nitric oxide and prostacyclin [12], decreased atherogenic activity of blood mononuclear cells effecting the production of cytokines [13], and a reduced accumulation of collagen in the arterial wall [14]. Therefore guidelines recommend that individuals accrue 30 minutes of moderate physical activity on at least 5 days of the week [15, 16].
Despite the positive impact of physical fitness on CVD, developed societies have become more sedentary in both occupation and leisure time. A recent observational study of 2595 civil servants in Northern Ireland reported that almost two thirds failed to engage in regular, moderate physical activity, with females twice as likely to abstain from exercise than men [17]. In England it has been reported that a total of 24.2% of men and 19.8% of women meet the activity recommendations; a total that dropped to 17.6% and 13.0% when domestic activity was excluded [18]. Since most adults will spend more than half their waking hours within the workplace, worksite health promotion programs that influence employee behaviour by promoting physical activity could prove fundamental in addressing the growing problem of sedentary habit and cardiovascular risk.
A number of randomised-controlled trials assessing the benefit of workplace exercise interventions on health-related outcome measures (body composition, blood pressure, lipid profile, inflammatory markers) have been reported [19–21]. However, the conclusions from these trials have been based upon the subjective self-report of physical activity, without individualised prescription or monitoring of the exercise programme, and objective assessment. Therefore the relationship between improved physical capacity and health from workplace exercise remains inconclusive [21]. In view of this there is a necessity for further studies of strong methodological quality to examine corporate exercise strategies adaptable to occupational time constraints.
The aim of this pilot study was to investigate the efficacy of a structured, monitored 12-week aerobic exercise training intervention programme on modifying the cardiovascular risk profile of a sedentary National Health Service (NHS) workforce, and to evaluate whether it could be implemented during working hours.
Methods
Setting
The trial was conducted at the Olympic Medical Institute (OMI), Northwick Park and North West London Hospitals (NWLH) NHS Trust (Northwick Park site). The North West London Research Ethics Committee, NWLH NHS Trust approved the trial (REC 05/Q0405/122). All participants provided written informed consent before entering the study.
Study participants
Participants were full-time male and female personnel from the NWLH Trust cytology laboratory. Who as specialist medical and non-medical cytology staff, spend multiple hours per day seated for the microscopic assessment of cervical cytology slides. All subjects were defined "sedentary" from self-reported physical activity levels of less than 2 hours organised physical activity per week. Eligible participants were not admitted if they had known cardiac disease, uncontrolled hypertension, thyroid disease, diabetes, mental illness, infection, immune or endocrine abnormality or contraindications to exercise on the basis of an exercise stress test. All participants were required to complete a medical screening questionnaire (PAR-Q) before entering the study.
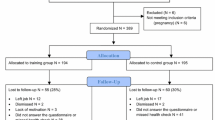
20 participants were recruited and randomly assigned to an exercise (n = 12) or control (n = 8) group using a random numbers table. Group assignment was revealed following baseline testing.
Experimental design
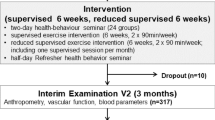
Physiological tests included blood pressure, body composition, peak oxygen uptake and blood screening, and were performed at pre-intervention and at 4 weekly intervals for a total of 12 weeks. After baseline assessment and at each 4 week reassessment, control subjects were instructed to maintain their current physical activity level, while the exercise group were provided with an individualised progressive exercise prescription of brisk walking or light jogging to be performed 4 times a week for the following 4 weeks (Figure 1.). At 8 weeks no further progression of the exercise training programme was provided, and participants were instructed to maintain the exercise as of week 8 for the final 4 weeks. This was to evaluate if there was any further physiological benefit, or if exercise adherence was affected in the absence of any additional training stimulus. Participants conducted all exercise sessions during their lunch, morning or afternoon breaks, to avoid disturbance to the normal laboratory working routine. Heart rate monitors (F4, Polar electro-oy, Kempele, Finland) were provided to monitor accurately the intensity of the exercise prescribed, and the average heart rate and exercise duration of each session was recorded in an exercise diary. The exercise intensity was initially set to correspond with 65 % of peak oxygen consumption (VO2 peak). Participants were instructed on an appropriate warm-up and cool-down procedure, and provided with a supervised exercise session during the initial week of each 4 week period. Progress was checked through personal contact on a weekly basis. At each exercise testing session all participants were provided with an evaluation of their results.
Both groups were provided with the Godin Leisure Time Questionnaire [22] to record in arbitrary units any additional physical activity or exercise that was above the prescribed programme. On entering the study participants were asked to complete a typical retrospective week of the same questionnaire. This was to ensure that all individuals from both groups participated in similar amounts of physical activity or exercise at baseline. The control group was offered the intervention at the end of the trial.
Outcomes
The primary outcomes were changes in peak oxygen consumption (VO2 peak), submaximal oxygen consumption at 2 minutes (2minVO2) and 4 minutes (4minVO2), and biological markers of inflammation (C-reactive protein, IL-6 and TNFα) between baseline and post intervention. Secondary outcomes were changes in time to exhaustion, resting heart rate, systolic and diastolic blood pressure. Secondary biological markers were fasting glucose and total cholesterol. Secondary physical outcomes were changes in body weight and body mass index (BMI). All outcome measures were taken after a 24 hour period of no exercise.
Biological outcomes
Fasting blood samples were collected in the morning, before any of the physiological tests. Whole blood samples were analysed for total cholesterol and glucose using an Abbott 8200 analyser (Abbott, Chicago, IL, USA). Cholesterol and glucose levels were measured using the cholesterol oxidase and hexokinase method respectively. Serum samples were used for CRP, TNFα, and IL-6. These were separated by low-speed centrifugation, and stored for later analysis at -70°C. The assays were performed using a semi-automated solid-phase, enzyme-labelled, chemiluminescent sequential immunometric assay (Euro/DPC, Gwynedd, UK), and measured using an IMMULITE 1000 analyser (Immulite, Gwynedd, UK). The lowest detection levels for IL-6, TNFα and CRP were 2 pg/mL, 1.7 pg/mL and 0.1 mg/L respectively. For the purpose of data analysis all values below the detection limit were coded as 1.9 pg/mL, 1.6 pg/mL and 0.05 mg/L respectively.
Blood pressure
Subjects remained in the supine position for 10 minutes. Blood pressure was measured manually, and recorded to the nearest 2 mm Hg. Each measurement was repeated three times then averaged.
Physical characteristics
Body composition was assessed indirectly through changes in body weight and body mass index. Body weight was assessed using an electronic scale (Seca, Vogel Halke, Germany). Standing height was determined without shoes. Body mass index was calculated as body mass (Kg) divided by height squared (m2).
Cardiopulmonary outcomes
Cardiopulmonary outcomes were evaluated using a progressive walking test (modified Bruce protocol) to volitional fatigue on a motorised treadmill. Speed (2.5, 3, 3.5 or 4 m·p-1· h-1) was predetermined by the participant's previous exercise history, and remained constant for the duration of the test, and for each subsequent test. The gradient was set at 2 % and increased by 1 % each minute. Heart rate data were recorded at 1-minute intervals. On the initial test this was used with VO2 data to determine the heart rate training intensity (65 % VO2 peak) of the exercise-training programme. This procedure was repeated at 4 and 8 weeks to ensure correct continuation of the heart rate training prescription. Participants were provided with standardized encouragement throughout the test.
Criteria for peak oxygen consumption included any two of the following: a peak or plateau for more than 1 minute in oxygen consumption; a respiratory exchange ratio ≥ 1.15; volitional exhaustion; and rating of perceived exertion greater than 19 (Borg, 1980). Exercise was terminated if participants developed severe dyspnea, dizziness, or chest pain, or had an abnormal heart rate response.
Expired gases were analysed every 5 seconds using an automated online gas analyser (Oxycon, Jaeger, Hoechberg, Germany). The system was calibrated for volume and gas concentrations before the start of each test. Peak oxygen consumption and oxygen consumption at 2 and 4-minute intervals were determined by taking the mean of twelve consecutive 5-second values at the end of each respective stage. Participants were asked to follow the same diet for the 24 hour period preceding each testing session.
Statistical analysis
Baseline characteristics between groups were compared using independent-samples t tests. Cardiopulmonary outcomes were normalized to baseline, and expressed as percentage change. Due to skewed distribution CRP data was log transformed. Repeated measures ANOVA were used to determine differences in outcomes between groups. Post hoc analysis was made within groups between each time-point. Where significant interaction effects were found, post hoc analysis was made at each time point between groups. SPSS version 14.0 (SPSS Inc, Chicago, IL, USA) was used for all statistical analyses. A P value < 0.05 was considered to be statistically significant. The results are reported as mean ± SD values.
Results
Baseline characteristics
Table 1 presents the baseline characteristics of the exercise (n = 12) and the control (n = 8) groups. There were no significant differences between groups for baseline characteristics.
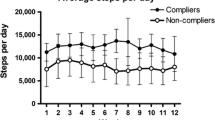
Adherence to the exercise training intervention
The exercise group completed 81 ± 14 % (13 ± 2), 84 ± 12 % (13 ± 2) and 70 ± 13 % (11 ± 2) of the 16 prescribed exercise sessions between week 1 and week 4, week 4 and week 8, and week 8 and week 12 respectively. Non-protocol related exercise was not significantly different between groups at any time point during the study (week 4 P = 0.893; week 8 P = 0.952; week 12 P = 0.941).
Changes in cardiopulmonary function
Table 2 and 3 present the cardiopulmonary outcomes. There was no significant time effect (F = 1.752; P = 0.167) in VO2 peak (L·min-1), but there was a significant interaction effect (F = 8.351; P = 0.000) and a treatment effect (F = 25.147; P = 0.000) between exercise and control groups. Post hoc analysis revealed that there were significant differences between exercise and control groups at all time points tested (P = 0.001; P = 0.001; P = 0.000). Furthermore, in the exercise group VO2 peak (L·min-1) significantly increased between week 0 and week 4 (P = 0.012), while in the control group it significantly decreased between week 0 and week 4 (P = 0.026), week 0 and week 8 (P = 0.004) and week 0 and 12 (P = 0.001) respectively. However, while there were no significant differences in peak heart rate (HRP) from baseline to any of the time points tested in the exercise group, HRP in the control group was significantly lower at all time points (P = 0.015; P = 0.032; P = 0.001). There was no significant time effect in time to exhaustion (TE) (F = 1.283; P = 0.334), but there were significant interaction and treatment effects between the exercise and the control conditions (F = 4.239; P = 0.006; F = 12.289; P = 0.002). Post hoc analysis between groups revealed significant differences at weeks 4 (P = 0.003), 8 (P = 0.002) and 12 (P = 0.036) respectively. Furthermore in the exercise group TE significantly increased from week 0 – week 4 (P = 0.005), week 0 – week 8 (P = 0.002) and week 0 – week 12 (P = 0.025), but no significant changes occurred in the control group at any time point.
There was a significant time (F = 12.099; P = 0.000), and treatment (F = 5.456; P = 0.031) effect in % change for absolute 2minVO2, but no significant interaction effect (F = 2.385; P = 0.079). Post hoc analysis between groups revealed that significant differences occurred at weeks 4 (P = 0.000), 8 (P = 0.003) and 12 (P = 0.001) respectively. While post hoc analysis within groups showed significant reductions in the exercise group between week 0 and week 4 (P = 0.006), week 4 and week 8 (P = 0.019), week 0 and week 8 (P = 0.000), and week 0 and week 12 (P = 0.000) in the exercise group, but no significant changes within the control group at any time point.
There were significant time (F = 4.004; P = 0.012) and treatment effects (F = 4.803; P = 0.042), but no significant interaction effect (F = 2.705; P = 0.054) in % change for absolute 4minVO2. Post hoc analysis between groups revealed that significant differences occurred at weeks 4 (P = 0.033) and 8 (P = 0.009), but not at week 12. Significant reductions occurred in the exercise group between week 4 and week 8 (P = 0.038), week 0 and week 8 (P = 0.002), week 8 and week 12 (P = 0.049) and week 0 and week 12 (P = 0.021), but not between week 0 and week 4. No significant changes occurred at any time point in the control group.
Changes in body composition and blood pressure
No significant time, treatment or interaction effects were observed for BMI (time F = 0.894; P = 0.364; treatment F = 0.468; P = 0.468; interaction F = 0.034; P = 0.857), weight (time F = 0.967; P = 0.389; treatment F = 0.501; P = 0.607; interaction F = 0.211; P = 0.652), systolic blood pressure (time F = 0.314; P = 0.746; treatment F = 1.657; P = 0.214; interaction F = 0.469; P = 0.641) or diastolic blood pressure (time F = 1.483; P = 0.229; treatment F = 0.293; P = 0.595; interaction F = 0.151; P = 0.929) over the 12 week intervention period.
Changes in blood parameters
Table 4 and 5 present blood parameter outcomes. No significant time, treatment or interaction effects were observed for total cholesterol (time F = 0.145; P = 0.932; treatment F = 0.049; P = 0.827; interaction F = 0.769; P = 0.516), glucose (time F = 0.209; P = 0.890; F = 0.049; P = 0.827; F = 0.615; P = 0.608), IL-6 (time F = 0.877; P = 0.429; F = 2.482; P = 0.133; F = 1.326; P = 0.278) or TNF-α (time F = 0.057; P = 0.982; treatment F = 0.002; P = 0.961; interaction F = 1.180; P = 0.326) over the 12 week intervention period. However while there was no significant time or treatment effect for CRP in exercise and control groups (time F = 1.703; P = 0.201; treatment F = 0.189; P = 0.669), there was a significant interaction effect (F = 3.309; P = 0.027). Post-hoc analysis revealed that there were no significant differences between exercise and control groups at any of the time points tested. However there were significant reductions in CRP within the exercise group between week 1 and week 4 (P = 0.013), week 4 and week 8 (P = 0.000), and between week 1 and week 8 (P = 0.010), while there was no significant change at any time point in the control group. There was a trend for a decrease in TNF-α from baseline within the exercise group compared to the control group.
Discussion
The data from the study confirmed that a moderate intensity aerobic exercise-training programme performed 4 times a week could be successfully implemented within the workplace during working hours. Furthermore, it was demonstrated that it was effective at reducing risk factors associated with cardiovascular disease, and at improving physiological capacity within previously sedentary individuals. Specifically, significant improvements were found in peak oxygen consumption (VO2 peak), economy of absolute oxygen utilization at both 2 minutes (2minVO2) and 4 minutes (4minVO2), and C-reactive protein (CRP) concentration. These results confirm previous reports showing that improved cardiovascular fitness, or physical activity level reduces cardiovascular risk, with a particular association with lower CRP levels [9, 23, 24]. This is the first report combining objective physiological outcome measures with objective monitoring of the training programme to demonstrate the type of exercise that can be effectively carried out during working hours, while still providing health related benefits.
At the end of the 8-week intervention period absolute VO2 peak increased significantly by 5 % in the exercise group, while it decreased significantly by 6 % in the control group. There was no significant change in peak heart rate in the exercise group, but there was a significant reduction in peak heart rate in the control group, suggesting that a decline in effort contributed to the observed fall in VO2 peak. Absolute 2minVO2 and 4minVO2 decreased significantly by 17 % and 11 % respectively in the exercise group, while there was no significant change in the control group. Furthermore, as the exercise group averaged the completion of 81 % and 84 % of the prescribed exercise sessions between week 1 and week 4, and week 4 and week 8 respectively, it can be concluded that the progressive aerobic exercise training programme was not only effective at improving the physical fitness of a sedentary group of adults, but was also successful at increasing physical activity levels.
However although cardiovascular fitness and physical activity are positively related, research indicates that it is the former that is more closely linked to cardiovascular disease risk factors and disease, than actual physical activity level [25, 26]. As a consequence it has been shown that it is only those individuals who increase their VO2 max, rather than their actual physical activity level that reduce their relative risk of cardiovascular disease risk factors [27]. This has been attributed to a reduction in large artery stiffness, which may be mediated by concomitant changes in high-density lipoprotein (HDL) cholesterol and body weight [28].
This holds relevance for the present study: after 8 weeks when the exercise group were not provided with any further progression or instruction to the exercise training programme VO2 peak decreased by 2 %. In view of the 70 % completion of the 16 sessions, and the significant improvement in absolute 4minVO2 (-7 %), it appears probable that the intensity of the exercise performed within this time period was too low to challenge VO2 peak. This is supported by evidence that indicates that VO2 max has a modest association with physical activity, but a much stronger association with the mean intensity of the exercise [29]. In view of this, and the cardio protective benefit of an increase in VO2 max future research should evaluate the implication of a higher intensity workplace exercise training programme on the modification of cardiovascular risk profile, while assessing whether it remains successful at ensuring exercise adherence.
It appears that supervision and progression of the exercise programme may influence adherence [30, 31]. In the present study, at 8 weeks when no further progression or supervision to the exercise training programme was provided a reduction in the adherence of the training sessions occurred; 81 % and 84 % were completed in week 1 to week 4 and week 4 to week 8, while only 70 % were completed in week 8 to week 12. This could further highlight the need for employers to ensure the provision of additional support and progression to the original training programme for optimal participation of employees, and success of the programme.
The exercise group demonstrated a significant decrease in CRP of -0.4 ± 0.6 mg/L between week 1 and week 4, and -1.0 ± 0.4 mg/L between week 4 and week 8. However while this is in accordance with previous research [24, 32], it should be noted that due to a mean baseline value indicating high risk for CVD (> 3.0 mg/L), that the reduction would still result in a mean value indicating average risk of CVD (2.2 mg/L) [33]. The mechanism behind such action remains unclear. It has been postulated that a reduction in CRP is attained via the positive benefit of exercise on BMI via modulation of the percentage of visceral fat and insulin receptor sensitivity [24]. However, within the present study there was no such positive effect on body composition, or fasting glucose. Another potential explanation is that among unfit individuals there is a greater generation of reactive oxygen species via normal metabolic processes, and unaccustomed muscle stretching. This leads to subliminal injury of the myocytes, that causes both cell and tissue oxidative damage, leading to an inflammatory response [34]. Evidence confirms that chronic exercise induces a mechanical resistance of the myocytes to stretching, and elevates endogenous antioxidant enzyme activity, which prevents excessive local inflammatory response [35]. As there were significant gains in aerobic capacity within the exercise group it is plausible that this explanation provides a mechanism of action for the observed results.
No significant change was observed in IL-6 at any time point during the study. However there was a significant reduction in TNF-α between week 1 and week 4 in the exercise group. As TNF-α directly impairs glucose uptake and metabolism via a direct effect on insulin signal transduction, a reduction holds positive benefit for prevention of CVD [10]. Thus despite the lack of a significant change in fasting glucose, there is still suggestive evidence that the training programme may accrue positive benefit for this specific risk factor.
Although the present study was successful at improving maximal and submaximal aerobic exercise capacity, it had no significant effect on fasting glucose or cholesterol, blood pressure or BMI. It is likely that the small sample size is responsible for such null findings. However it is also unsurprising for a number of reasons.
Firstly, although physical activity and exercise improves insulin sensitivity through a direct effect on the muscle (enhancement of insulin receptor autophsophorylation [36], increase in GLUT-4 content [37] and glucose transport-phosphorylation [38], and a reduction in visceral obesity [39], neither the exercise nor the control group exhibited impaired glucose tolerance (exercise = 5.04 ± 0.50; control = 5.11 ± 0.52 mmol/L) at baseline that would have required intervention modification. The same can be said for blood pressure, with all participants classified as normotensive (exercise = 118 ± 12/73 ± 10; control = 106 ± 10/69 ± 9) at baseline. Nevertheless, in view of the beneficial effect that exercise has on glucose tolerance, and evidence that those with low levels of physical fitness are shown to be at a relative risk of 1.52 for developing hypertension, when compared to highly fit individuals [6], the use of exercise in aiding glycemic control, and the maintenance of healthy blood pressure should still be encouraged.
Secondly, regarding BMI, it should be considered that the aim of the training programme was not to directly target weight loss for a reduction of cardiovascular risk, but instead to improve physiological capacity, and biomarkers of cardiovascular profile. In accordance with this, and in the absence of dietary modification, it would have been unlikely that the 4 × 30 minute sessions per week would have provided the necessary negative energy balance stimulus of 500 – 1000 kcal·d-1 to achieve gradual weight loss (ACSM, 2006). Given that a BMI ≥ 30 kg·m-2classifies obesity, concomitantly increasing the risk of hypertension, poor total cholesterol/HDL cholesterol ratio, coronary disease and mortality rate [40], there is a need for future work place health promotion programmes to evaluate whether an aerobic exercise training programme specifically targeting weight loss and management as its primary outcome can be successfully implemented within the workforce.
A limitation of the present study was the failure to examine lipoprotein subfractions; small low-density lipoproteins (LDLs), high-density lipoproteins (HDLs), high-density lipoprotein subfractions (HDL3 and HDL2), very low-density lipoproteins (VLDLs), and respective particle size, that better reflect CVD risk than absolute measures of cholesterol concentrations [41]. In a recent study, Halverstadt et al (2007) concluded that an aerobic exercise training program consisting of 20 minutes, 3 days a week, progressively building up to a duration of 40 minutes and an intensity of 70 % VO2 max for a period of 24 weeks, plus a weekend walk was successful at improving lipid subfraction profile and cardiovascular risk independent of diet and change in body fat. This is supported by several other studies, which also indicate an improved plasma lipoprotein profile with exercise training, exclusive of weight loss [5, 42].
Conclusion
Our pilot study provides objective and randomised controlled trial data demonstrating that regular supervised exercise increases physical activity for healthy individuals, and improves exercise capacity, with a concomitant cardioprotective benefit. As this can be achieved without disrupting the working day, this exercise programme provides a means of improving health at work. As the study was conducted within an NHS department, it may be of particular relevance to the NHS, as the single largest employer in Europe.
References
Roberts CK, Barnard RJ: Effects of exercise and diet on chronic disease. J Appl Physiol 2005,98(1):3–30. 10.1152/japplphysiol.00852.2004
Wilund KR: Is the anti-inflammatory effect of regular exercise responsible for reduced cardiovascular disease. Clin Sci 2007,112(11):543–55. 10.1042/CS20060368
Wannamethee SG, Lowe GD, Whincup PH, Rumley A, Walker M, Lennon L: Physical activity and hemostatic and inflammatory variables in elderly men. Circulation 2002,105(15):1785–1790. 10.1161/hc1502.107117
Eriksson KF, Lindgarde F: No excess 12-year mortality in men with impaired glucose tolerance who participated in the Malmo Preventive Trial with diet and exercise. Diabetologia 1998,41(9):1010–1016. 10.1007/s001250051024
Kraus WE, Houmard JA, Duscha BD, Knetzger KJ, Wharton MB, McCartney JS, Bales CW, Henes S, Samsa GP, Otvos JD, Kulkarni KR, Slentz CA: Effects of the amount and intensity of exercise on plasma lipoproteins. N Engl J Med 2002,347(19):1483–1492. 10.1056/NEJMoa020194
Blair SN, Goodyear NN, Gibbons LW, Cooper KH: Physical fitness and incidence of hypertension in healthy normotensive men and women. JAMA 1984,252(4):487–490. 10.1001/jama.252.4.487
Melo RC, Santos MD, Silva E, Quiterio RJ, Moreno MA, Reis MS, Verzola IA, Oliveira L, Martins LD, Gallo-Junior L, Catai AM: Effects of age and physical activity on the autonomic control of heart rate in healthy men. Braz J Med Biol Res 2005,38(9):1331–1338. 10.1590/S0100-879X2005000900007
Tate DF, Jeffery RW, Sherwood NE, Wing RR: Long-term weight losses associated with prescription of higher physical activity goals. Are higher levels of physical activity protective against weight regain? Am J Clin Nutr 2007,85(4):954–959.
Borodulin K, Laatikainen T, Salomaa V, Jousilahti P: Associations of leisure time physical activity, self-rated physical fitness, and estimated aerobic fitness with serum C-reactive protein among 3,803 adults. Atherosclerosis 2006,185(2):381–387. 10.1016/j.atherosclerosis.2005.06.015
Pedersen BK: The anti-inflammatory effect of exercise: its role in diabetes and cardiovascular disease control. Essays Biochem 2006, 42: 105–117. 10.1042/bse0420105
Vasankari TJ, Kujala UM, Vasankari TM, Ahotupa M: Reduced oxidized LDL levels after a 10-month exercise program. Med Sci Sports Exerc 1998,30(10):1496–1501. 10.1097/00005768-199810000-00005
Walther C, Gielen S, Hambrecht R: The effect of exercise training on endothelial function in cardiovascular disease in humans. Exerc Sport Sci Rev 2004,32(4):129–134. 10.1097/00003677-200410000-00002
Smith JK, Dykes R, Douglas JE, Krishnaswamy G, Berk S: Long-term exercise and atherogenic activity of blood mononuclear cells in persons at risk of developing ischemic heart disease. JAMA 1999,281(18):1722–1727. 10.1001/jama.281.18.1722
Kramsch DM, Aspen AJ, Rozler LJ: Atherosclerosis: Prevention by agents not affecting abnormal levels of blood lipids. Science 1981,213(4515):1511–1512. 10.1126/science.6792706
American College of Sports Medicine (ACSM): Guidelines for Exercise Prescription. 7th edition. Philadelphia; USA: Lippincott Williams and Wilkins; 2006.
The Chief Medical Officer. At least five a week: evidence on the impact of physical activity and its relationship to health 2004. [http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4080994]
Addley K, McQuillan P, Ruddle M: Creating healthy workplaces in Northern Ireland: evaluation of a lifestyle and physical activity assessment programme. Occup Med 2001,51(7):439–449. 10.1093/occmed/51.7.439
Stamatakis E, Hillsdon M, Primatesta P: Domestic physical activity in relationship to multiple CVD risk factors. Am J Prev Med 2007,32(4):320–327. 10.1016/j.amepre.2006.12.020
Murphy MH, Murtagh EM, Boreham CA, Hare LG, Nevill AM: The effect of a worksite based walking programme on cardiovascular risk in previously sedentary civil servants. BMC Public Health 2006, 6: 136. 10.1186/1471-2458-6-136
White K, Jacques PH: Combined diet and exercise intervention in the workplace: effect on cardiovascular disease risk factors. AAOHN J 2007,55(3):109–114.
Proper KI, Koning M, van der Beek AJ, Hildebrandt VH, Bosscher RJ, van Mechelen W: The effectiveness of worksite physical activity programs on physical activity, physical fitness, and health. Clin J Sport Med 2003,13(2):106–117. 10.1097/00042752-200303000-00008
Godin G, Shephard RJ: A simple method to assess exercise behavior in the community. Can J Appl Sport Sci 1985,10(3):141–146.
Kuo HK, Yen CJ, Chen JH, Yu YH, Bean JF: Association of cardiorespiratory fitness and levels of C-reactive protein: data from the National Health and Nutrition Examination Survey 1999–2002. Int J Cardiol 2007,114(1):28–33. 10.1016/j.ijcard.2005.11.110
Elosua R, Bartali B, Ordovas JM, Corsi AM, Lauretani F, Ferrucci L: Association between physical activity, physical performance, and inflammatory biomarkers in an elderly population: the InCHIANTI study. J Gerontol A Biol Sci Med Sci 2005,60(6):760–767.
Suzuki I, Yamada H, Sugiura T, Kawakami N, Shimizu H: Cardiovascular fitness, physical activity and selected coronary heart disease risk factors in adults. J Sports Med Phys Fitness 1998,38(2):149–157.
Lakka TA, Venalainen JM, Rauramaa R, Salonen R, Tuomilehto J, Salonen JT: Relation of leisure-time physical activity and cardiorespiratory fitness to the risk of acute myocardial infarction. N Engl J Med 1994,330(22):1549–1554. 10.1056/NEJM199406023302201
McMurray RG, Ainsworth BE, Harrell JS, Griggs TR, Williams OD: Is physical activity or aerobic power more influential on reducing cardiovascular disease risk factors? Med Sci Sports Exerc 1998,30(10):1521–1529. 10.1097/00005768-199810000-00009
Ferreira I, Twisk JW, Stehouwer CD, van Mechelen W, Kemper HC: Longitudinal changes in VO2max: associations with carotid IMT and arterial stiffness. Med Sci Sports Exerc 2003,35(10):1670–1678. 10.1249/01.MSS.0000089247.37563.4B
O'Donovan G, Owen A, Bird SR, Kearney EM, Nevill AM, Jones DW, Woolf-May K: Changes in cardiorespiratory fitness and coronary heart disease risk factors following 24 wk of moderate- or high-intensity exercise of equal energy cost. J Appl Physiol 2005,98(5):1619–1625. 10.1152/japplphysiol.01310.2004
Bendermacher BL, Willigendael EM, Teijink JA, Prins MH: Supervised exercise therapy versus non-supervised exercise therapy for intermittent claudication. Cochrane Database Syst Rev 2006,2(2):CD005263.
Olney SJ, Nymark J, Brouwer B, Culham E, Day A, Heard J, Henderson M, Parvatanei K: A randomized controlled trial of supervised versus unsupervised exercise programs for ambulatory stroke survivors. Stroke 2006,37(2):476–481. 10.1161/01.STR.0000199061.85897.b7
Albert MA, Glynn RJ, Ridker PM: Effect of physical activity on serum C-reactive protein. Am J Cardiol 2004,93(2):221–5. 10.1016/j.amjcard.2003.09.046
Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon RO, Criqui M: Markers of inflammation and cardiovascular disease: application to clinical and public health practice: A statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation 2003,108(1):499–511. 10.1161/01.CIR.0000052939.59093.45
Pansarasa O, Castagna L, Colombi B, Vecchiet J, Felzani G, Marzatico F: Age and sex differences in human skeletal muscle: role of reactive oxygen species. Free Radic Res 2000,33(3):287–293. 10.1080/10715760000301451
Elosua R, Molina L, Fito M, Arquer A, Sanchez-Quesada JL, Covas MI, Ordonez-Llanos J, Marrugat J: Response of oxidative stress biomarkers to a 16-week aerobic physical activity program, and to acute physical activity, in healthy young men and women. Atherosclerosis 2003,167(2):327–334. 10.1016/S0021-9150(03)00018-2
Youngren JF, Keen S, Kulp JL, Tanner CJ, Houmard JA, Goldfine ID: Enhanced muscle insulin receptor autophosphorylation with short-term aerobic exercise training. Am J Physiol Endocrinol Metab 2001,280(3):E528–33.
Hughes VA, Fiatarone MA, Fielding RA, Kahn BB, Ferrara CM, Shepherd P, Fisher EC, Wolfe RR, Elahi D, Evans WJ: Exercise increases muscle GLUT-4 levels and insulin action in subjects with impaired glucose tolerance. Am J Physiol 1993,264(6 Pt 1):E855–62.
Perseghin G, Price TB, Petersen KF, Roden M, Cline GW, Gerow K, Rothman DL, Shulman GI: Increased glucose transport-phosphorylation and muscle glycogen synthesis after exercise training in insulin-resistant subjects. N Engl J Med 1996,335(18):1357–1362. 10.1056/NEJM199610313351804
Short KR, Vittone JL, Bigelow ML, Proctor DN, Rizza RA, Coenen-Schimke JM, Nair KS: Impact of aerobic exercise training on age-related changes in insulin sensitivity and muscle oxidative capacity. Diabetes 2003,52(8):1888–1896. 10.2337/diabetes.52.8.1888
Hu G, Tuomilehto J, Silventoinen K, Barengo N, Jousilahti P: Joint effects of physical activity, body mass index, waist circumference and waist-to-hip ratio with the risk of cardiovascular disease among middle-aged Finnish men and women. Eur Heart J 2004,25(24):2212–2219. 10.1016/j.ehj.2004.10.020
Rosenson RS, Otvos JD, Freedman DS: Relations of lipoprotein subclass levels and low-density lipoprotein size to progression of coronary artery disease in the Pravastatin Limitation of Atherosclerosis in the Coronary Arteries (PLAC-I) trial. Am J Cardiol 2002,90(2):89–94. 10.1016/S0002-9149(02)02427-X
Thompson PD, Yurgalevitch SM, Flynn MM, Zmuda JM, Spannaus-Martin D, Saritelli A, Bausserman L, Herbert PN: Effect of prolonged exercise training without weight loss on high-density lipoprotein metabolism in overweight men. Metabolism 1997,46(2):217–223. 10.1016/S0026-0495(97)90305-X
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
JAH conceived the study design, carried out the testing, performed statistical testing and drafted the manuscript. MM carried out the immunoassays. GPW participated in the coordination of the study and drafting of the manuscript. KvS helped to draft the manuscript. TSL conceived of the study, and participated in its design and coordination, and helped to draft the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Hewitt, J.A., Whyte, G.P., Moreton, M. et al. The effects of a graduated aerobic exercise programme on cardiovascular disease risk factors in the NHS workplace: a randomised controlled trial. J Occup Med Toxicol 3, 7 (2008). https://doi.org/10.1186/1745-6673-3-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1745-6673-3-7