Abstract
Background
Angiotensin-converting enzyme inhibitors and the angiotensin-receptor blocker valsartan ameliorate ventricular remodeling after myocardial infarction (MI). Based on previous clinical trials, a maximum clinical dose is recommended in practical guidelines. Yet, has not been clearly demonstrated whether the recommended dose is more efficacious compared to the lower dose that is commonly used in clinical practice.
Method/Design
Valsartan in post-MI remodeling (VALID) is a randomized, open-label, single-blinded multicenter study designed to compare the efficacy of different clinical dose of valsartan on the post-MI ventricular remodeling. This study also aims to assess neurohormone change and clinical parameters of patients during the post-infarct period. A total of 1116 patients with left ventricular dysfunction following the first episode of acute ST-elevation MI are to be enrolled and randomized to a maximal tolerable dose (up to 320 mg/day) or usual dose (80 mg/day) of valsartan for 12 months in 2:1 ratio. Echocardiographic analysis for quantifying post-MI ventricular remodeling is to be conducted in central core laboratory. Clinical assessment and laboratory test are performed at fixed times.
Discussion
VALID is a multicenter collaborative study to evaluate the impact of dose of valsartan on the post-MI ventricular remodeling. The results of the study provide information about optimal dosing of the drug in the management of patients after MI. The results will be available by 2012.
Trial registration
Similar content being viewed by others
Background
Progressive enlargement of the heart chamber and deterioration of contractile function after myocardial infarction (MI), termed post-MI ventricular remodeling, is associated with development of heart failure and poor prognosis [1–3]. The magnitude of post-MI remodeling is influenced by several determinants, most notably infarct size [4], but also by ventricular wall stress [5], patency of infarct-related artery [6], and a number of neurohormonal factors [7]. Thus, the consequence of post-MI remodeling varies among patients with acute MI even in the era of reperfusion therapy [8]. Modification of neurohormonal acitivities, particularly the rennin-angiotensin-aldosterone system (RAAS), can significantly influence the process of ventricular remodeling after acute MI. Suppression of angiotensin activity either by inhibition of angiotensin-converting enzyme (ACE) [9–11] or by blockade of angiotensin II receptor [12] attenuates ventricular dilatation and improves clinical outcomes. Based on the results from major pivotal clinical trials, it is usually recommended in practical guidelines that the maximal clinical dose of ACE inhibitors used in those trials be given to patients after acute MI [13, 14]. A seminal finding that the neurohormone level is linearly related with mortality [15] in patients with heart failure also suggests the potential benefit of higher doses.
However, the optimal level of RAAS antagonism in the treatment of heart failure or post-MI remodeling is still a matter of debate. Although administration of higher dose of angiotensin-converting enzyme (ACE) inhibitor was more beneficial than lower dose in animal model of post-MI remodeling [16], results of clinical studies were not confirmatory. In the VALIANT study [17], addition of ARB valsartan to ACE inhibitor resulted in similar degree of post-MI left ventricular (LV) remodeling compared to either drug alone, although in the Val-HeFT study [18], LV remodeling in heart failure was more favorable in the combination therapy group. In several clinical studies that directly compared different doses of ACE inhibitors in patients with chronic heart failure, the results of clinical outcomes as well as neurohormonal responses were inconsistent, and sometimes irrelevant because of the impractical dosing of drugs chosen for the comparison. In the ATLAS study [19], patients receiving high-dose lisinopril (32.5-35.0 mg/day) had a nonsignificant (8%) lower risk of death and a significant (12%) lower rate of death and hospitalization compared with patients receiving low-dose lisinopril (2.5-5.0 mg/day). The CHIPS trial [20] compared low-dose (50 mg/day) with high-dose (100 mg/day) captopril therapy and demonstrated a nonsignificant trend toward less worsening heart failure and hospitalization in the high-dose group. In the NETWORK trial [21], there was no difference in the primary endpoint of combined death, heart failure-related hospitalization, and worsening of heart failure among the three groups of low dose (5 mg/day), medium dose (10 mg/day), and high dose (20 mg/day) enalapril therapy. Furthermore, the lower dose used in NETWORK (enalapril 5 mg/day) [21] was too small, and the higher dose used in ATLAS (lisinopril 35 mg/day) [19] was excessive for practical use. The recent publication of the Heart failure Endpoint evaluation of Angiotensin Antagonist Losartan trial (HEAAL) presented notable evidence of the superiority of 150 mg/day of losartan versus 50 mg per day on the primary outcomes of death or hospitalization in patients with systolic heart failure [22]. However, the study subjects were limited to patients who were intolerant to ACE inhibitors [22], precluding extrapolation of the result to general patients. Furthermore, the optimal dosing of ARB agents has not been explored in the population of post-MI. Thus, the question of whether submaximal dose of ARB, which are lower than those in major pivotal trials but typically used in clinical practice, can offer similar benefit in post-MI ventricular remodeling remains to be solved. This is more so in the Asian population, wherein moderate dose ARB has been shown to provide sufficient protection from cardiovascular risk [23]. Therefore, the primary objective of the VALsartan in post-mI remoDeling (VALID) study is to address this issue in Korean patients who suffered their first acute ST-elevation MI by comparing the impact of different doses of valsartan, an ARB demonstrated as effective as ACE inhibitor in post-MI patients [12], on echocardiographic variables of left ventricular remodeling during the follow-up period of 1 year. The comparison dose of valsartan will be 80 mg per day, as commonly prescribed after MI in Korea, versus 320 mg per day, a targeted dose in major clinical trials [12, 24].
Trial objectives
The primary hypothesis to be tested is whether high dose valsartan significantly reduces ventricular remodeling as measured by echocardiography in post-MI patients during a 12-month follow-up period, compared with the usual dose of control group.
Methods and Design
Study design
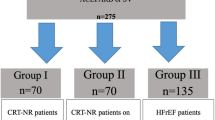
VALID is a prospective, multicenter, randomized, open-label, active controlled study with two parallel study groups. VALID is being conducted in 18 tertiary hospitals throughout South Korea. Participants are randomly allocated into the usual dose group and high dose group and followed-up for 12 months after discharge. Overall study algorithm is depicted in Figure 1. Baseline echocardiographic examination and neurohormonal assay are performed before discharge. Study approval was given by the institutional review board at each participating center, and consecutive, eligible patients are provided written informed consent.
Randomization
Randomization will take place following initial echocardiographic estimation of left ventricular ejection fraction, which is conducted after stabilization by reperfusion therapy or conservative treatment. Eligible patients are randomly assigned in a 1:2 ratio to receive the usual dose (valsartan 80 mg/day) or a high dose (valsartan up to 320 mg/day). Random allocation with stratified technique is generated automatically by a centralized web based tool (http://www.cnrres.co.kr/valid) so it cannot be influenced by researchers.
Approval
This study follows the Helsinki Declaration's principles, meaning that all patients sign a written informed consent stating that participation is voluntary and that participation can
be withdrawn at any time, without any negative consequences concerning their current or future medical treatment. This study protocol was approved by the institutional review board of Dong-A University hospital and each participating center.
Patient population
Men and women aged 18 years or older who suffer their first acute ST-elevation myocardial infarction with the sign of LV dysfunction are eligible for this study (Table 1). In the present study, LV dysfunction is defined as an ejection fraction < 50% using a modified Simpson's rule [25]. Enrollment criteria are intended to include patients in acute stage of infarction, within 10 days of symptom onset, who are typically treated under modern therapeutic strategy. Patients are recruited regardless of whether they received reperfusion therapy, either thrombolysis or primary percutaneous coronary intervention, or not. Pharmacological therapy other than study drug, including beta-adrenergic blockers, is allowed according to the discretion of attending physician. Patients who have contraindication to the study drug or major concomitant disease are excluded (Table 1).
Intervention and comparator descriptions
Eligible patients are randomly assigned in a 1:2 fashion to either the usual dose group (valsartan 80 mg/day) or the high dose group (valsartan up to 320 mg/day). In the usual dose group, valsartan 40 mg twice a day is administrated throughout the study period. For those in the high dose group, dose is up-titrated to 80 mg twice a day before hospital discharge and finally to 160 mg twice a day after 2 weeks during outpatient visits. The process of the trial conduct is illustrated in Figure 2. If up-titration is not clinically feasible, either because of hypotension or deepening azotemia, the previous dose is administered subsequently as maximal tolerable dose.
Titration scheme of study drug. In the usual dose group, valsartan 40 mg twice a day is administrated throughout the study period. For those in the high dose group, dose is up-titrated to 80 mg twice a day before hospital discharge and finally to 160 mg twice a day after 2 weeks during outpatient visits.
Outcomes measurement
The primary outcome of the study is the changes of the echocardiographic indices of LV remodeling, which is the LV volume index at end-systolic and end-diastolic time as measured by modified Simpson's rule [25], during the study period. Echocardiographic records from participating institute are sent to the core echocardiography laboratory for the analysis. Secondary outcomes include occurrence of predefined clinical events (all-cause death, cardiovascular death, hospitalization, revascularization), changes of plasma level of neurohormone (B-type natriuretic peptide, norepinephrine, aldosterone), and echocardiographic indices other than ventricular volume (ejection fraction, wall motion score index, mitral inflow, tissue Doppler index) at 12 months (Table 2). Neurohormone measurement will be conducted in a core laboratory.
Follow-up protocol
During the study period, study visits are scheduled at week -2 (high-dose group only), and 1, 3, 6, 9, 12 months. At each visit, patients undergo a complete physical examination, medical history-taking, and assessment of drug compliance. Investigators evaluate all clinical and laboratory adverse events at each visit. To monitor safety, serum creatinine and urea nitrogen concentrations are determined at every study visit. New York Heart Association (NYHA) functional class [26] and predefined clinical events are recorded at each clinical visit. Echocardiographic examination and neurohormonal assay are performed at 3 and 12 months after discharge. After a routine review with 50% of the patients enrolled, early cessation of the trial will be decided by the institutional review board and study sponsor when the trial appears to be futility or causing unexpected harm to participants.
Adverse effects
Analysis of safety related data is performed with respect to frequency of serious adverse events, stratified by causality and intensity of morbidity in both treatment groups.
Patients are interviewed at each visit about the occurrence of any adverse events, including the time of onset, duration, and severity; all information is recorded on a case report from. The causal relation to the study drug and the intensity of adverse events are evaluated by the investigators. Serious adverse events (SAE) have to be reported to the institutional review board and study sponsor by the principal investigator within 24 hours after the SAE becomes known.
Withdrawals
Patients are free to withdraw trial participation at their own request at any time and without giving reasons for their decision. Moreover, the primary investigator can withdraw study patients, if continuation of the trial would be detrimental to the patient's
well being. Withdrawals will be documented in the case report form and in the patient's medical records and all ongoing severe adverse event have to be followed up.
Sample size
The sample size calculation is based on the primary outcome and the primary analysis for the intention-to-treat population. In the VALIANT Echo study, [17] a sample size of 600 patients was determined necessary to detect, with a 90% power, a 7.6 mL difference in end-diastolic volume between the treatment groups. Because the present study enrolls more patients with mild degree (EF < 50%) LV dysfunction, we anticipate that the difference of ventricular volume between treatment groups will be smaller than the previous study. Thus, detection of 3.8 mL difference, with a two-sided level of significance α = 5% and a power of 1-β = 90%, in end-diastolic volume between treatment groups would require a sample size of 279 patients in a usual dose of valsartan group and 558 patients in a high dose valsartan group. Assuming 25% of patients are lost to follow-up or with missing data, as reported in the GISSI-3 study [27], the required sample size of this study will be a total of 1,116 patients. The study is likely to be underpowered in terms of assessing secondary outcomes if this size is employed. Variability data for the outcome measures could be used to inform design a subsequent larger-scale randomized controlled trial, if post hoc analysis reveals this study to be underpowered.
Statistical analyses
A consultant group of statisticians has been appointed to conduct the statistical work for this study, including data completion, interim analysis, application of statistical technique and final assessment. The principal analysis will be an intention-to-treatment basis. For baseline characteristics, continuous variables are assessed using the Student t test and discrete variables are compared using the chi-square test. The two-sided null-hypothesis for the primary outcome measure states that usual and high dose valsartan lead to the same expected change of ventricular remodeling during the 12 months after MI. This null-hypothesis will be tested by application of an analysis of covariance that adjusts for age, gender, and cardiovascular risk factors. Primary outcome will be compared using 2-sample t tests. Event-free cumulative survival rates are plotted using the Kaplan-Meier method and comparisons are made between patients with and those without clinical events using the log-rank test. A Cox proportional hazards model with the use of forward selection based on the likelihood ratio test will be implemented for multivariate analysis to determine which prognostic factors identified in the univariate analysis were significantly related to 12-month clinical events. Assessments for the change of neurohormone and other echocardiographic indices will be compared between treatment groups at 12-month follow-up using 2-sample t tests.
We will compare proportions of missing data using chi-square tests and agreement between data collection methods using Lin's Concordance Correlation Coefficient. Additionally, sensitivity analyses will be conducted using different patient populations (per protocol population excluding patients with relevant protocol violations), different imputation techniques for missing values, and different statistical methods for taking into account covariates. A value of p < 0.05 will be considered statistically significant.
Discussion
Despite the accepted roles of ACE inhibitors and the ARB agent valsartan in the treatment of post-MI LV dysfunction [9–12], the appropriate dose remains unclear. Although clinical guidelines recommend to prescribe the doses that have been shown to reduce the risk of cardiovascular events in clinical trials [13, 14], it is common practice for the patients to be maintained on doses appropriate for initiation of therapy rather than doses up-titrated to target doses used in the clinical trials. Concerns about patient's intolerance to higher doses might be an attributable factor for such practice. Although the recent HEAAL study demonstrated a superiority of higher dose over low dose losartan in ACE intolerant patients with heart failure, the evidence is still lacking for the setting of post-MI LV dysfunction and for general population. The VALID study has been designed to address the issue of optimal dosing of ARB valsartan in the post-MI patients by comparing the major echocardiographic outcome of post-MI LV remodeling, which is the LV volume index. Because the differences of clinical outcomes between high- versus low-dose therapy is expected to be considerably smaller than those of placebo-controlled landmark trials, quantitative measurement of post-MI ventricular remodeling can be a reasonable surrogate endpoint.
Conclusions
The enrollment criteria for the VALID is different from those of other major post-MI ACE inhibitor trials in that patients with milder systolic LV dysfunction (EF <50%) is eligible for VALID while more severe form of LV dysfunction (EF <35% or clinical sign of heart failure) was required for enrollment in previous major clinical trials [9–12]. Two factors have been considered when deciding the cut-off value for LV dysfunction. First, the majority of patients referred to the participating hospital receive reperfusion therapy in Korea [28], leading to substantial increment of the number of the patients with more preserved LV contractile function. Second, as the proportion of elderly population among the patients with acute MI is increasing, the pattern of post-MI remodeling may exhibit a different picture. Elderly patients seem to undergo LV remodeling more commonly than younger patients, even after smaller size acute MI. In the PREAMI study [29], ACE inhibitor (8 mg/day of perindopril) could reduce progressive LV remodeling in elderly patients who had a relatively preserved LV function with EF ≥40%. Thus, the increasing proportion of elderly population in acute MI cases in Korea [30] can make it feasible to examine the effect of ARB agent on post-MI remodeling in the presence of moderate LV dysfunction for the VALID study.
Abbreviations
- ACE:
-
Angiotensin-converting enzyme
- MI:
-
Myocardial infarction
- LV:
-
Left ventricle
- EF:
-
Ejection fraction
- RAAS:
-
Renin-angiotensin-aldosterone system
- VALID:
-
Valsartan in post-myocardial infarction remodeling
- βAR:
-
Beta-adrenergic blocker
- ARB:
-
Angiotensin II receptor blocker.
References
Pfeffer MA, Braunwald E: Ventricular remodeling after myocardial infarction. Experimental observation and clinical implications. Circulation. 1990, 81: 1161-1172. 10.1161/01.CIR.81.4.1161.
Gaudron P, Ellis C, Kugler I, Ertl G: Progressive left ventricular dysfunction and remodeling after myocardial infarction: potential mechanisms and early predictors. Circulation. 1993, 87: 755-763.
St John Sutton M, Pfeffer MA, Plapoert T: for the SAVE Investigators. Quantitative two-dimensional echocardiographic measurements are major predictor of adverse cardiovascular events after myocardial infarction. Circulation. 1994, 89: 68-75.
Pfeffer MA, Pfeffer JM, Fishbein MC, Fletcher PJ, Spadaro J, Kloner RA, Braunwald E: Myocardial infarction size and ventricular function in rats. Circ Res. 1979, 44: 503-512.
Hammerman H, Kloner RA, Alker KJ, Schoen FJ, Braunwald E: Effect of transient increased afterload during experimentally induced acute myocardial infarction in dogs. Am J Cardiol. 1985, 55: 566-570. 10.1016/0002-9149(85)90248-6.
Pfeffer MA, Lamas GA, Vaughan DE, Parisi AE, Braunwald E: Effect of captopril on progressive ventricular dilatation after anterior myocardial infarction. N Eng J Med. 1988, 11: 12-19.
Noda K, Sasaguri M, Ishida M, Ikeda M, Arakawa K: Role of locally formed angiotensin II and bradykinin in the reduction of myocardial infarct size in dogs. Cardiovas Res. 1993, 27: 334-340. 10.1093/cvr/27.2.334.
Giannuzzi P, Temporelli PG, Bosimini E Gentile F, Lucci D, Maggioni AP, Tavazzi L, Badano L, Stoian I, Piazza R, Heyman I, Levantesi G, Cervesato E, Geraci E, Nicolosi GL: Heterogeneity of left ventricular remodeling after acute myocardial infarction: results of the Gruppo Italiano per lo Studio della Sopravvivenze nell'Infarto Miocardico-3 Echo substudy. Am Heart J. 2001, 141: 131-138. 10.1067/mhj.2001.111260.
Pfeffer MA, Braunwald E, Moye LA: on the behalf of the SAVE Investigators. Effect of captopril of mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction: results of the Survival and Ventricular Enlargement Trial. N Engl J Med. 1992, 327: 685-691.
The Acute Infarction Ramipril Efficacy (AIRE) Study Investigators: Effect of ramipril on mortality and morbidity of survivors of acute myocardial infarction with clinical evidence of heart failure. Lancet. 1993, 342: 821-828.
Kober L, Torp-Pederson C, Carlsen E, Bagger H, Eliasen P, Lyngborg K, Videbaek J, Cole DS, Auclert L, Pauly NC: A clinical trial of the angiotensin-converting-enzyme inhibitor trandopril in patients with left ventricular dysfunction after myocardial infarction. Trandolapril Cardiac Evaluation (TRACE) Study Group. N Engl J Med. 1995, 233: 1670-1676.
Pfeffer MA, McMurray JJ, Velazquez EJ, Rouleau JL, Kober L, Maggioni AP, Solomon SD, Swedberg K, Van de Werf F, White H, Leimberger JD, Henis M, Edward S, Zelenkofske S, Sellers MA, Califf RM: For the Valsartan in Acute Myocardial Infarction Trial Investigators. Valsartan, captopril or both in myocardial infarction complicated by heart failure, left ventricular dysfunction or both. N Engl J Med. 2003, 349: 1893-1906. 10.1056/NEJMoa032292.
Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K, Oates JA, Rahko PS, Silver MA, Stevenson LW, Yancy CW, Antman EM, Smith SC, Adams CD, Anderson JL, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B, American College of Cardiology; American Heart Association Task Force on Practice Guidelines; American College of Chest Physicians; International Society for Heart and Lung Transplantation; Heart Rhythm Society: ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. Circulation. 2005, 112: e154-e235. 10.1161/CIRCULATIONAHA.105.167586.
Krum H: The Task Force for the diagnosis and treatment of CHF of the European Society of Cardiology. Guidelines for the diagnosis and treatment of chronic heart failure: full text (update 2005). Eur Heart J. 2005, 26: 1115-1140.
Francis GS, Cohn JN, Jonson G Rector TS, Goldman S, Simon A: Plasma norepinephrine, plasma renin acitivity, and congestive heart failure. Relation to survival and the effect of therapy in V-HeFT II. The V-HeFT VA Cooperative Study Group. Circulation. 1993, 87 (6 Suppl): VI40-VI48.
Yang Y, Zhang P, Song L Ruan Y, Xu X, Li Y, Zhou Y, Tian Y, Xu Y, Chen Z: Comparision of the doses of enalapril in preventing left ventricular remodeling after acute myocardial infarction in the rat. China Med J. 2002, 115: 347-351.
Solomon SD, Skali H, Anavekar NS, Bourgoun M, Barvik S, Ghali JK, Warnica W, Khrakovskaya M, Arnold MO, Schwarz Y, Velazquez EJ, Califf RM, McMurray JV, Pfeffer MA: Changes in ventricular size and function in patients treated with valsartan, captopril or both after myocardial infarction. Circulation. 2005, 111: 3411-3419. 10.1161/CIRCULATIONAHA.104.508093.
Wong M, Staszewsky L, Latini R, Bariera S, Volpi A, Chiang YT, Benza RL, Gottlieb SO, Kleemann TD, Rosconi F, Vandervoort PM, Cohn JN: Val-HeFT Heart Failure Trial Investigators. Valsartan benefits left venricular structure and function in heart failure; Val-Heft echocardiographic study. J Am Coll Cardiol. 2002, 40: 970-974. 10.1016/S0735-1097(02)02063-6.
Packer M, Poole-Wilson PA, Armstrong PW, Cleland JGF, Horowitz JD, Massie BM, Lyden L, Thygesen K, Uretsky BF: Comparative effect of low and high doses of the angiotension-converting enzyme inhibitor, lisinopril, on mortality and morbidity in chronic heart failure. Circulation. 1999, 100: 2312-2318.
Clement DL, De Buyzere M, Tomas M, Vanavermaete G: Long-term effects of clinical outcome with low and high dose in the Captopril in Heart Insufficient Patients Study (CHIPS). Acta Cardiol. 2000, 55: 1-7. 10.2143/AC.55.1.2005711.
The NETWORK Investigators: Clinical outcome with enalapril in symptomatic chronic heart failure; a dose comparison. Eur Heart J. 1998, 19: 481-489.
HEAAL Investigators: Effects of high-dose versus low-dose losartan on clinical outcomes in patients with heart failure (HEAAL study): a randomized, double-blind trial. Lancet. 2009, 374: 1840-1848. 10.1016/S0140-6736(09)61913-9.
Jikei Heart Study group: Valsartan in a Japanese population with hypertension and other cardiovascular disease (Jikei Heart Study): a randomized, open-label, blinded endpoint morbidity-mortality study. Lancet. 2007, 369: 1431-1439. 10.1016/S0140-6736(07)60669-2.
Cohn JN, Tognoni G: A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med. 2001, 345: 1667-1675. 10.1056/NEJMoa010713.
Lang RM, Bierig M, Devereux RB, flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ: American Society of Echocardiography's Guidelines and Standards Committee: European Association of Echocardiography. J Am Soc Echocardiogr. 2005, 18: 1440-1463. 10.1016/j.echo.2005.10.005.
The Criteria Committee of the New York Heart Association: Nomenclature and Criteria for Diagnosis. 1994, Boston, Little Brown, 9
Nicolosi GL, Latini R, Marino P, Maggioni AP, Barlera S, Franzosi MG, Geraci E, Santoro L, Tavazzi L, Toqnoni G, Vecchio C, Volpi A: The prognostic value of predischarge quantitative two-dimensional echocardiographic measurenets and the effects of early lisinopril treatment on left ventricular structure and function after acute myocardial infarction in the GISSI-3 Trial. Eur Heart J. 1996, 17: 1646-1656.
Lee KH, Jeong MH, Ahn YK, Kim JH, Chae SC, Kim YJ, Hur SH, Seong IW, Hong TJ, Choi DH, Cho MC, Kim CJ, Seung KB, Chung WS, Jang YS, Cho JG, Park SJ: Sex differences of the clinical characteristics and early management in the Korea Acute Myocardial Infarction Registry. Korean Circulation J. 2007, 37: 64-71. 10.4070/kcj.2007.37.2.64.
The PREAMI Investigators: Effect of angiotensin-converting enzyme inhibition with perindopril on left ventricular remodeling and clinical outcome. Results of the Randomized Perindopril and Remodeling in Elderly with Acute Myocardial Infarction (PREAMI) study. Arch Intern Med. 2006, 166: 659-666.
Moon HK, Kim YD, Yang DG, Kim SG, Cha KS, Kim MH, Kim JS, Cha TJ, Joo SJ, Lee JW, Hong TJ, Shin YW, Kim DI, Kim DS, Park JS, Shin DG, Kim YJ: Age and Gender Distribution of patients with acute myocardial infarction admitted to university hospitals during the period of 1990-1999. Korean Circulaiton J. 2003, 33: 92-96.
Acknowledgements
This study was financially supported by Novartis Korea, Seoul, Korea. As this is an investigator-initiated trial, the authors designed and conducted the study. Data collection has been managed by an independent clinical research center. The funding body does not interfere in the analysis and interpretation of the data. We would like to thank all members of present study group for their ideas, suggestions, participation and support.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
YDK is the Principle Investigator for the study, contributed to the study design and to drafting and revising the manuscript. YRC made significant contribution to concept of the study, drafting and reviewing manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Cho, YR., Kim, YD., Park, TH. et al. The impact of dose of the angiotensin-receptor blocker valsartan on the post-myocardial infarction ventricular remodeling: study protocol for a randomized controlled trial. Trials 12, 247 (2011). https://doi.org/10.1186/1745-6215-12-247
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1745-6215-12-247