Abstract
Background
The relationship between life stressors, coping and affective disorder is interesting when predicting onset of a affective disorder and relapse of mood episodes.
Methods
A litteratur review of cross-sectional and longitudinal studies concerning coping and affective disorder in adults including a Medline and Embase search was conducted.
Results
11 cross-sectional studies and 17 longitudinal studies concerning affective disorder and coping were found, among these, two studies include patients with bipolar disorder exclusively. Only four studies elucidate whether emotion-oriented and/or avoidance coping styles are associated with a higher risk of developing affective disorder, so this hypothesis remains unclear. Most studies shows that emotion-oriented and avoidance coping strategies are associated with relapse of depressive episodes. Conversely, problem-focused and task-oriented coping seem to be associated with a good outcome.
Conclusion
There is a gap between coping theory and clinical use of coping and the clinical relevance of coping is, though promising, still unclear. In future research it is recommended to concentrate on development of a semi-structured interview combining coping style, life events and personality traits.
Similar content being viewed by others
Introduction
Psychosocial stressors may precipitate depression [1, 2] and presumably also mania [3]. However, most persons exposed to stressful events do not develop psychiatric impairments [4]. This raises the question: why do some people experience an affective disorder in relation to a stressful life event and others do not? The answer is complex; it involves genetic loading, personality, prior experiences, parental style, social network and probably how individuals deal or cope with stress.
Coping and stress are aspects of life and coping style plays an important role in individual well-being. As formulated by H. Selye "that although we cannot avoid stress as long as we live, we can learn a great deal about how to keep its damaging side effects "distress" to a minimum" [5]. Freud's interest in defence mechanisms had a close connection to what today is named coping [6]. He believed some defence mechanisms to be healthier or less regressed than others in the same way that some coping styles seem to be associated with a healthier outcome. Synonyms for coping may be mastery, adaptation or behavioural style. Coping is defined in various ways: "any response to external life strains that serves to prevent, avoid or control emotional distress" [7], or as "constantly changing cognitive and behavioural efforts to manage specific external and/or internal demands that are appraised as taxing or exceeding the resources of the person" [8].
The failure of coping to deal adaptively with stress may lead to mental and physical illness. In general, people who rely more on approach coping tend to adapt better to life stressors and experience fewer psychological problems [9]. Approach and task-oriented coping are strategies involving problem solving, seeking information and attempts to alter the situation [10]. Conversely, avoidance and emotion-oriented coping strategies seem to be associated with psychological distress [11]. Avoidance coping describes activities aimed at avoiding the stressful situation and involves denial, wishful thinking and withdrawal [12]. Emotion-oriented coping describes emotional reactions that are self-orientated in order to reduce stress. These reactions involve emotional responses (individuals blaming themselves for being too emotional, becoming angry-, or tense) [13] and ruminative responses defined as: behaviours and thoughts that focus attention on depressive symptoms and on the implication of these symptoms (individuals thinking how tired they feel and why they get depressed, why others do not) [10].
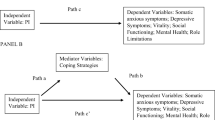
Many studies of coping examine the relationship between coping and somatic illness. Research on the relation of coping and depressive disorder has attracted attention, but in clinical psychiatry there is a gap between clinical practice and research [14, 15]. With changing treatment approaches for depressive and bipolar disorders such as interpersonal psychotherapy and cognitive-behavioural therapy coping may be important as a target for treatment. Therefore clinical studies involving coping and depressive and bipolar disorders in adults are reviewed in order to investigate two hypotheses; Are avoidance and emotion-oriented coping strategies associated with an increased risk of developing an affective disorder and with a higher risk of relapse of mood episodes?
Methods
Electronic searching in Embase and Medline using the combination of the following terms: Mood Disorders or Bipolar Disorder or Depression (MeSH-terms) Mania or Manic-depressive Illness (Text-words) and Coping (Text-word): 5864 hits Medline, 3016 hits Embase. Studies of coping and affective disorder were selected by reading headings and abstracts. The following studies were excluded; coping and somatic illness, coping in children and adolescents and studies of coping concerning individuals as employees, parents etc. Medline Index starts in 1968. The search was ended at March 2005.
Results
As seen from the Tables, 11 cross-sectional studies and 17 follow-up studies were identified. The studies are presented in three tables according to design and in historical order. Five studies investigated the same sample [16, 35, 36, 40, 43].
Cross-sectional studies
The 11 cross-sectional studies are presented in Table 1. The cross-sectional studies showed; Firstly, a relation between emotion-oriented and avoidance coping strategies and the prevalence and symptom severity of depression. Secondly, the cross sectional studies cannot show whether these strategies were associated with first episode or with relapse of a depressive or manic episode.
Short-term studies
The seven short-term studies are presented in table 2. Short-term studies are here defined as studies with a three- to six-month follow-up period. The short-term studies indicated: firstly, in four of the seven studies that emotion-oriented and ruminative coping style were state dependent [27, 29, 31, 32], secondly, in four studies these coping styles were related to the severity of the depressive symptoms [27, 29–31], thirdly, three studies showed that recovery from depression were associated with changes in coping style [27, 29, 31], accordingly, recovered patients relied less on inappropriate emotion-focused coping strategies and finally, two studies showed that emotion-oriented coping predicted the presence of depression at follow-up [28, 30]. Conversely one study showed that ruminative coping might be associated with a good outcome in depressed patients [33].
Long-term studies
The 10 long-term studies are presented in table 3. Long-term studies are here defined as studies with a follow-up period longer than six months. The long-term studies indicated: firstly, that adaptive coping strategies predicted increased remission and decreased risk of relapse in half of the studies [35, 37, 39, 41, 42]. One study concluded that depressed persons did not differ in amount of problem-focused coping compared to control persons [34]; another study did not find that problem-focused coping was a predictor of post-treatment symptoms [38]. Secondly, the use of passive and ruminative coping strategies and coping by avoiding other people was found to be related to a higher risk of relapse and of greater severity of depressive symptoms at follow-up in six of the ten studies [34, 35, 37, 39, 40, 42]. Thirdly, one study showed that a high level of stressors was connected with higher depression scores at follow-up [37]. Finally, the study on bipolar disorder showed that patients that used stimulating coping strategies more often had a manic episode [42]
Results summary
Regarding the two hypotheses none of the studies were capable of answering whether certain coping strategies are predictive of affective disorder. Most studies showed that in depressive disorder avoidance and emotion-oriented coping strategies seem to be related to recurrence/relapse of depressive episodes. These coping strategies might also be associated with an increased time to recovery. Only a few studies on bipolar disorder were identified, limiting the findings to depressive disorder mainly. In the cross-sectional and short-term studies it is difficult to make a clear distinction between coping processes and symptoms, and avoidance and emotion-oriented coping styles seemed to be state related, so the results of these studies are not able to answer our hypothesis.
Discussion
Study-design
Regarding the trait or state effect, the use of cross-sectional designs and designs with a short follow-up period can be problematically because of the possibility of measuring residual depressive symptoms. The coping style of an individual may change during a depresive or manic episode, as illustrated in the short-term studies. Possibly, the emotion-oriented coping style found especially in the cross-sectional studies could be explained by a state-dependent consequence of a depressed mood. One way to determine whether the anomalies are caused by the depressive or manic episode (state model) is to include a control group. Among the 28 studies, 12 included a control group. In the follow-up studies, the lack of a control group makes it difficult to distinguish whether the changes that occurred reflect normalization of coping over time or whether the changes reflect changes in affective symptoms. The best impression of the relation between coping and state comes from the follow-up studies that used repeated measures of affective symptoms, life events and coping behaviour and include a control group [34–37, 40, 43]. The studies with a long follow-up time [37, 40, 41, 43] illustrate the time-relation between coping and affective episodes: these studies support the hypothesis that emotion-oriented and avoidance coping strategies seem to be associated with increased risk of relapse. So, the controlled follow-up studies provided the most valid study design to comply with methodological problems.
Comparing results
It is difficult to compare studies involving heterogeneous samples and it is likely that selection bias influenced the results unpredictable. Most studies used clinical samples of unipolar patients. A general limitation is the lack of attention to confounding variables such as the duration and severity of the mood episodes and the number of previous episodes. Some studies investigated these parameters [21, 23, 28, 30, 39–41] and these results did not deviate substantially from those of other studies. The use of passive coping strategies predicted relapse of depression and stimulating coping strategies increased the relapse risk of mania but from the limited number of studies concerning bipolar disorder [20, 42] it is not possible to elucidate the relation between coping and bipolar disorder. The little attention to research into coping mechanisms and mania was already stressed in a case report in 1990 [45] and latest by the authors in a research report from 1999 where the development and validation of the coping inventory for prodomes of mania was described [46].
Participants were registered differently according to comorbid psychopathology. In one study the most common comorbid disorders were panic disorder, dysthymia and social phobia [26]. One study concentrated on comorbid agoraphobia [39] and one on comorbid personality disorder [44]. In some studies patients with comorbid psychopathology were excluded [16, 21, 22, 28, 29]. Although the relation of coping processes and risk for substance abuse is a defined area of coping research [47], only two studies [39, 43] adjusted for the possible effect of comorbid substance use as a part of a coping strategy. This may have affected the results so that some inappropriate coping strategies are not identified.
Coping measurements
As seen from the tables, the studies measured coping differently, which makes it difficult to compare across studies. The coping measures were based on self-reports and a variety of questionnaires were used without any golden standard. It is important to develop reliable and valid tools that assess how people cope with stressful situations and negative events. Therefore developing structured and easily scorable scales started in the 1960s [48] and during the 1980 and 1990s, – much research was conducted on self-reported measures of coping. Facing particularly stressful events, individuals are asked about the kind of coping behaviour(s) in which they have engaged [49]. This research used widely divergent strategies, techniques and measures; additionally some of the scales possess a variety of psychometrically drawbacks [13]. When examining the coping questionnaires, it is clear that substance use as a coping behaviour has virtually been ignored [13, 27, 50, 51]. The two studies concerning abuse showed that depressive symptoms were significantly associated with more drinking problems [43] and that improvement in functioning and well-being was associated with less alcohol consumption [39].
As discussed, in a critical review concerning the gap between coping theory and clinical intervention research [52], when using a coping checklist and thereby reducing coping to a summary score, a lot of information will be lost. The questions seem to be to general for the results to be valid and crucial aspects of timing, sequencing and appropriateness may be lost.
Coping and life events
There is a substantial and partially causal link between life-events and depression [53] and the occurrence of major life events signals a period of increased risk of developing a depressive episode [54]; several studies measured life events [17, 18, 21, 23, 24, 26, 27, 29, 34–37, 39, 43, 44]. A general problem in measuring coping in connection with life events is the time relation, as participants should recall a stressful situation and then reconstruct how they dealt with it. Firstly, there is recall bias and secondly, coping has a temporal aspect: an individual can cope before a stressful event occurs, while it is happening and afterwards [55]. The issue of timing is complex as there presumably may be an interaction between individual vulnerability, coping, life events and the risk of developing depression. Thus it is difficult to measure the coping process given the typical brief period between a severe life event and depression. Capturing the coping process represents a challenge [56] and it may require a more frequent monitoring of coping than is usually done in studies.
All coping measures are based on self-reports and participants are often asked in connection with hypothetical stressors e.g. the Coping Inventory for Stressful Situations [13] and it is difficult to know what kind of stressors were thought of. Many scales for coping are developed to assess overall coping strategies but it reasonable that human cope differently according to the nature of the event. Linking coping measures to recent actual stressors and attempting objective assessment of the stressful life event to avoid circularity is of main importance. The procedure of semi-structured interviews is time- and labour consuming and might be a reason for the consistent use of self-reports. The lacking use of coping in clinical assessment and treatment may be due to the rather confusing divergent coping scales. It can be rather meaningless to detect coping not knowing what kind of stressor the coping process relates to and the influence of personality traits cannot be ignored [56]. For advancing research and clinical focus on coping there is a need of developing an integrated semi-structured interview detecting personality traits, life events and coping together. Beside, a specific development of coping schedules capable of identifying prodomal symptoms of bipolar episodes as described by Wong et al. [46] would be of clinical use.
Coping and personality
Coping is closely related to personality and personality can affect coping measures and in coping as well as in personality research there is a distinction between trait and state variables. In the concept of coping responses [57], coping is seen as a response to specific stressful situations rather than a stable feature of personality. Another approach emphasizes the method of coping; whether a response entails primal cognitive or behavioural efforts [58]. One study [26] showed that less-adaptive coping strategies (emotion-oriented coping) were associated with neuroticism and depression, whereas the reverse association was found regarding adaptive coping strategies (task-orientated coping). These findings are replicated in studies of the general population [59, 60]. Finally, a study [61] from Japan found that task-oriented and avoidance coping were related to extraversion and that emotion-oriented coping was related to neuroticism. Personality traits are important in the assessment of coping and it is advisable to measure these traits when dealing with coping measures; however, only three studies have done so [26, 41, 44].
Coping and Gender
In most of the present studies more women were included reflecting the gender differences in the prevalence of depressive disorder. In some studies gender differences were found and the general tendency was that men tend to distract themselves using active coping strategies, whereas women use strategies involving expressing emotion [16, 21, 25]. Other studies found no gender differences [22, 30, 33]; however, most studies did not take gender into consideration in the analyses. According to the hypothesis of Nolen-Hoeksema [62] the increased vulnerability of women to developing depression is related to gender differences in coping; men's response to their dysphoria is more behavioural and dampens their depressive episodes, whereas women's response to their dysphoria is more ruminative and amplifies them. Accordable to a review [63] of gender differences in depression, it is possible that men tend to distract themselves from their mood by engaging in physical or instrumental activities, whereas women are less active and ruminate over the possible causes and implications of their depression. These hypotheses are compatible with findings from other studies [64–66] the latter study involving data covering representative population samples from six European countries. Conversely, an older prospective one-year study [67] of 100 healthy community-residing men and women, in which participants were interviewed seven times at four-week intervals, found no gender differences in emotion-focused coping. Another study [68] of couples that recently had experienced at least one threatening life event that was potentially depressonigenic for both showed that women had a greater risk than men of depressive episodes following the life event. The greater risk was restricted to episodes that followed events involving children, housing or reproductive problems. Women's greater risk was only present among those couples for whom there were clear gender differences in associated roles.
Coping and age
Age differs between the studies but most studies had a broader age range. How age influences the stress and coping process is not clear: The Normative Aging Study [69], a longitudinal study examined stress, appraisal and coping in three groups' middle-aged, young-old and old-old men. The study followed 2280 men for more than 30 years. A significant overall effect of age on coping strategies: instrumental action, cognitive reframing, social support and interpersonal hostile strategies were found and all coping strategies showed linear decrease with age. The relation between age and coping is complex and there is no clear answer as to whether persons cope better or worse as they age. In a recent study, the association between life events and onset of depression and mania was not found to change throughout life [70]
Coping and medical adherence
The episodic course of affective disorders presents a challenge to the clinician and the patient, in making and fulfilling a treatment plan. Effective treatment depends on medication adherence also when treating medical patients with comorbid depression. When treating affective disorder, doctors and patients have to deal with different problems: lack of insight, symptom-free intervals, residual affective symptoms and poor social support, which can complicate long-term treatment [71]. Identification of these factors may add to increase medication adherence as seen in a study [72] that investigated medication adherence in 32 patients with bipolar I disorder. Consistent with the hypothesis that acceptance coping would be positively associated and denial coping negatively associated with adherence to mood-stabilizing medication, it was found that low levels of acceptance and a high level of denial undermined medication adherence.
Clinical implications
Coping strategies could be a target for selective prevention targeting subgroups of the population whose risk of developing an affective disorder is higher than average. Further, a way to ameliorate the course in affective disorder is to help patients to identify prodomal symptoms and individual maladaptive coping strategies and try to change these, e.g. problem training as a treatment for depression [46, 73, 74] or intervention designed to improve coping. More recent literature supports the utility of individual cognitive behavioural and psycho-educational approaches, particular in enhancing medication adherence, so medication and psychotherapy are not only compatible but also synergistic [75] and a strong focus in psychological treatment involves structured attempts to teach patients new coping skills.
Conclusion
The gap between coping theory and clinical use of coping remains and the clinical relevance of coping is, though promising, still unclear. It is difficult to make a clear distinction between coping processes and symptoms. The complex interaction between life stressors, coping, personality and affective disorders need to be better understood before coping behaviour and changes in coping strategies can be included more systematically in patient treatment. Primary, there is a need to develop new valid and reliable measures combining assessment of coping, life events and personality in a semi-structured interview. Long-term high-risk studies capable of detecting coping before and after an onset of an mood disorder would provide new information of the relation between coping strategies and affective disorder.
References
Ellicott A, Hammen C, Gitlin M, Brown M, Jamison K: Life events and the course of bipolar disorder. Am J Psychiatry. 1990, 147: 1194-98.
Rudolp KD, Hammen C, Burge D: Toward an interpersonal life-stress model of depression: The development context of stress generation. Develop Psychopath. 2000, 12: 215-34.
Kessing LK, Agerbo E, Mortensen PB: Major stressful life events and first admission with mania. 2004, 6: 122-9.
Kessler RC: The effects of stressful events on depression. Ann Rev Psychol. 1997, 48: 191-214.
Seley H: The stress of life. The McGraw-Hill Companies, Inc. 1976, Revised
Bond M, Gardner ST, Christian J, Sigal JJ: Empirical study of self-rated defence styles. Arch Gen Psychiatry. 1983, 40: 333-38.
Pearlin LI, Schooler C: The structure of coping. J Health Soc Behav. 1978, 19: 2-21.
Lazarus RS, Folkman S: Stress, Appraisal and Coping. New York. 1984, Springer Publishing Company, 328-33.
Folkman S, Lazarus RS: The relationship between coping and emotion: implications for theory and research. Soc Sci Med. 1988, 26: 309-17.
Ray C, Lindop J, Gibson S: The concept of coping. Psychol Med. 1982, 12: 385-95.
Suls J, Fletcher B: Self attention, life stress and illness: a prospective study. Psychosom Med. 1985, 47: 469-81.
Folkman S, Lazarus RS: The relationship between coping and emotion: implications for theory and research. Soc Sci Med. 1988, 26: 309-17.
Endler NS, Parker JDA: CISS Coping Inventory for Stressful Situations. Manual second edition, Multi-Health Systems. 1999
Sommerfield MR, McCrae RR: Stress and coping research. Methodological challenges, theoretical advances and clinical applications. Am Psychol. 2000, 55: 620-25.
Lazarus RS: Toward better research on stress and coping. Am Psychol. 2000, 55 (6): 665-73.
Billings AG, Moss RH: Coping, stress and social resources among adults with unipolar depression. J Pers Soc Psychol. 1984, 46: 877-91.
Rosenberg SJ, Peterson RA, Hayes JR: Coping behaviours among depressed and nondepressed medical inpatients. J Psychosom Res. 1987, 31: 653-58.
McNaughton ME, Patterson TL, Irwin MR, Grant I: The relationship of life adversity, social support, and coping to hospitalisation with major depression. J Nerv Ment Dis. 1992, 180: 491-97.
Turner RA, King PR, Tremblay PF: Coping styles and depression among psychiatric outpatients. Pers Individ Diff. 1992, 13: 1145-47.
Lam D, Wong G: Prodromes, coping strategies, insight and social functioning in bipolar affective disorders. Psychol Med. 1997, 27: 1091-1100.
Dekker J, Ormel J: Depression and coping. Eur J Psychiatry. 1999, 13: 183-89.
Schouws S, Dekker J, Tuynman-Qua H, Kwakman H, Jonghe F: Relation between quality of life and coping and social behaviour in depression. Eur J Psychiatry. 2001, 15: 49-56.
Vossler A, Sommer G, Bühler KE, Haltenhof H: Soziale unterstützung and krankheitsverarbeitung bei 41 patienten mit depressiven störungen. Nervenheilkunde. 2001, 20: 17-21.
Ravindran AV, Matheson K, Griffiths J, Merali Z, Anisman H: Stress, coping, uplifts and quality of life in subtypes of depression: a conceptual frame and emerging data. J Affect Disord. 2002, 71: 121-30.
Lam D, Scuck N, Smith N, Farmer A, Checkley S: Response style, interpersonal difficulties and social functioning in major depressive disorder. J Affect Disord. 2003, 75: 279-83.
McWilliams AL, Cox BJ, Enns MW: Use of the coping inventory for stressful situations in a clinically depressed sample: Factor structure, personality correlates, and prediction of distress. J Clin Psychol. 2003, 59 (4): 423-37.
Parker GB, Brown LB: Coping behaviours that mediate between life events and depression. Arch Gen Psychiatry. 1982, 39: 1386-91.
Parker GB, Brown LB: Coping behaviours as predictors of the course of clinical depression. Arch Gen Psychiatry. 1986, 43: 561-65.
Schussler G, Grischke M, Ruger U: Coping with depressive disorders. Nervenartz. 1992, 63: 416-21.
Ravindran AV, Griffiths J, Waddell C, Anisman H: Stressful life events and coping styles in relation to dysthymia and major depressive disorders. Variations associated with alleviation of symptoms following pharmacotherapy. Prog Neuropsychopharmacol Biol Psychiatry. 1995, 19: 637-53.
Kuehner C, Weber I: Responses to depression in unipolar depressed patients: An investigation of Nolen-Hoeksema's response styles theory. Psychol Med. 1999, 29: 1323-33.
Uehara T, Sakado K, Sato T, Takizawa R: Coping measurement and the state effect of depression and anxiety in psychiatric outpatients. Psychopathology. 2002, 35: 48-51.
Yamada K, Nagayama H, Tsutiama K, Kitamura T, Furukawa T: Coping behaviour in depressed patients: a longitudinal study. Psychiatry Res. 2003, 121: 169-77.
Coyne JC, Aldwin C, Lazarus RS: Depression and coping in stressful episodes. J Abnorm Psychol. 1981, 90: 439-47.
Billings AG, Moos RH: Life stressors and social resources affect posttreatment outcomes among depressed patients. J Abnorm Psychol. 1985, 94: 140-53.
Billings AG, Moos RH: Psychosocial processes of remission in unipolar depression: comparing depressed patients with matched community controls. J Cons Clin Psychol. 1985, 53: 314-25.
Swindle RW, Cronkite RC, Moos RH: Life stressors, social resources, coping and the 4-year course of unipolar depression. J Abnorm Psychol. 1989, 4: 468-77.
Hoffart A, Martinsen EW: Coping strategies in major depression, agoraphobic and comorbid in-patients: A longitudinal study. Br J Med Psychol. 1993, 66: 143-55.
Sherbourne CD, Hayes RD, Wells KB: Personal and psychosocial risk factors for physical and mental health outcomes and course of depression among depressed patients. J Consul Clin Psychol. 1995, 63: 345-55.
Moos RH, Cronkite RC: Symptom-based predictors of a 10-year chronic course of treated depression. J Nerv Ment Dis. 1999, 187: 360-68.
Oldehinkel AJ, Ormel J, Neeleman J: Predictors of time to remission from depression in primary care patients: Do some people benefit more from positive life change than others. J Abnorm Psychol. 2000, 2: 299-307.
Lam DH, Wong G, Sham P: Prodromes, coping strategies and course of illness in bipolar affective disorder-a naturalistic study. Psychol Med. 2001, 31: 1397-1402.
Holahan CJ, Moos RH, Holahan CK, Cronkite RC: Drinking to cope and alcohol use in unipolar depression: a ten-year model. J Abnorm Psychol. 2003, 112: 159-65.
Szadoczky E, Rozsa S, Zambori J, Furedi J: Predictors of 2-year outcome of major depressive episode. J Affect Disord. 2004, 83 (1): 49-57.
Suresh TR, Srinivasan TN: Claimed simulation of insanity. Br J Psychiatr. 1990, 157: 603-5.
Wong G, Lam D: The development and validation of the coping inventory for prodomes of mania. J Affect Disord. 1999, 53: 57-65.
Wills TA, Hirky AE: Coping and substance abuse: a theoretical model and review of the evidence. Zeidner M, Endler NS, Handbook of Coping. 1996, 279-302.
Sidle A, Moos R, Adams J, Cady P, Alto P: Development of a coping scale. Gen Psychiatry. 1969, 20: 226-32.
Endler NS, Parker JDA: A factor analytic study of coping styles and the MMPI-2 content scales. J Clin Psychol. 1990, 49: 523-27.
Rosenbaum M: A schedule for assessing self-control behaviours: prelaminary findings. Behav Ther. 1980, 11: 109-21.
Porter LS, Stone AA: An approach to assessing daily coping. Edited by: Zeidner M. 1996, Endler NS: Handbook of Coping, 133-50.
Coyne JC, Racioppo MW: Never the Twain shall meet? Closing the gap between coping research and clinical intervention research. Am Psychol. 2000, 55: 655-64.
Brown GW, Harris T: Social origins of depression. 1978, University printing house, Cambridge
Paykel ES: Life events, social support and depression. Acta Psychiatr Scand. 1994, 337: 50-58.
Schwarzer R: Stress and coping from a social-cognitive perspective. Annals New York Academy Science. 1998, 851: 531-37.
Kessler RC, Price RH, Wortman CB: Social factors in psychopathology: stress, social support and coping processes. Annu Rev Psychol. 1985, 36: 531-72.
Coyne JC, Gottlieb BH: The mismeasure of coping by checklist. J Pers. 1996, 64: 959-91.
Moos RH, Holahan CJ: Dispositional and contextual perspectives on coping: toward an integrative framework. J Clin Psychol. 2003, 12: 1387-1403.
Cosway R, Endler NS, Sadler AJ, Deary IJ: The coping for stressful situations; Factorial structure and associations with personality traits and psychological health. J Applied Biobehav Res. 2000, 5: 121-43.
Saklofske DH, Kelly IW: Coping and personality. Psychol Rep. 1995, 77: 481-82.
Uehara T, Sakado K, Sato T, Takizawa R: Relationship between stress coping and personality in patients with major depressive disorder. Psychother Psychosom. 1999, 68: 26-30.
Nolen Hoeksema SH: Sex differences in unipolar depression: evidence and theory. Psychol Bull. 1987, 101: 259-82.
Piccinelli M, Wilkinson G: Gender differences in depression: Critical review. Br J Psychiatry. 2000, 177: 486-92.
Wilhelm K, Parker G: Sex differences in depressiogenic risk factors and coping strategies in a socially homogeneous group. Acta Psychiat Scand. 1993, 88: 205-11.
Bouhuys AL, Geerts E, Gordijn CM: Gender-specific mechanisms associated with outcome of depression: perception of emotions, coping and interpersonal functioning. Psychiatr Res. 1999, 85: 247-61.
Angst J, Gamma A, Gastpar M, Lépine JP, Mendlewicz J, Tylee A: Gender differences in depression. Eur Arch Psychiatr Clin Neuroscience. 2000, 252: 201-9.
Folkman S, Lazarus RS: An analysis of coping in a middle-aged community sample. J Health Soc Behav. 1980, 21: 219-39.
Nazroo JY, Edwards AC, Brown GW: Gender differences in the onset of depression following a shared life event: a study of couples. Psychol Med. 1997, 27: 9-19.
Aldwin CM, Sutton KJ, Chiara G, Spir A: Age differences in stress, coping, and appraisal: findings from the normative aging study. J Gerontol. 1996, 51: 177-88.
Kessing LK, Agerbo E, Mortensen PB: Does the impact of major stressful life events on the risk of developing depression change throughout life?. Psychol Med. 2003, 33: 1177-84.
Schuman C, Lenz G, Berghöfer A, Müller-Oerlinghausen B: Non-adherence with long-term prophylaxis: a 6-year naturalistic follow-up study of affectively ill patients. Psychiatr Res. 1999, 89: 247-57.
Greenhause WJ, Meyer B, Johnson SH: Coping and medication adherence in bipolar disorder. J Affect Disord. 2000, 59: 237-41.
Jané-Llopis E, Hosman C, Jenkins R, Anderson P: Predictors of efficacy in depression prevention programmes. Br J Psychiatry. 2003, 183: 384-97.
Fava GA, Kellner R: Prodomal symptoms in affective disorders. Am J Psychiatry. 1991, 148: 823-30.
Craighead WE, Miklowitz DJ: Psychosocial interventions for bipolar disorder. J Clin Psychiatry. 2000, 61: 58-64.
Acknowledgements
The Theodore and Vada Stanley Medical Research Institute and the Lundbeck Foundation supported the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Christensen, M.V., Kessing, L.V. Clinical use of coping in affective disorder, a critical review of the literature. Clin Pract Epidemiol Ment Health 1, 20 (2005). https://doi.org/10.1186/1745-0179-1-20
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1745-0179-1-20