Abstract
Background
Lead is a heavy metal and important environmental toxicant and nerve poison that can destruction many functions of the nervous system. Lead poisoning is a medical condition caused by increased levels of lead in the body. Lead interferes with a variety of body processes and is toxic to many organs and issues, including the central nervous system. It interferes with the development of the nervous system, and is therefore particularly toxic to children, causing potentially permanent neural and cognitive impairments. In this study, we investigated the relationship between lead poisoning and the intellectual and neurobehavioral capabilities of children.
Methods
The background characteristics of the research subjects were collected by questionnaire survey. Blood lead levels were detected by differential potentiometric stripping analysis (DPSA). Intelligence was assessed using the Gesell Developmental Scale. The Achenbach Child Behavior Checklist (CBCL) was used to evaluate each child’s behavior.
Results
Blood lead levels were significantly negatively correlated with the developmental quotients of adaptive behavior, gross motor performance, fine motor performance, language development, and individual social behavior (P < 0.01). Compared with healthy children, more children with lead poisoning had abnormal behaviors, especially social withdrawal, depression, and atypical body movements, aggressions and destruction.
Conclusion
Lead poisoning has adverse effects on the behavior and mental development of 2–4-year-old children, prescribing positive and effective precautionary measures.
Similar content being viewed by others
Background
Lead exists widely in the environment, and it is a heavy metal element with neurotoxic effects. In contrast to trace elements such as iron and zinc, lead has no know beneficial effects in the human body [1]. With the economic development of China in recent years, the concentration of lead in the environment has increased, and lead pollution has become a serious problem. Chinese people have begun to place greater scrutiny on the influence of lead exposure on human health, especially its impact on teenagers [2]. Lead poisoning can damage and produce irreversible harm to fetal growth, the growth of teenagers, and psychological, behavioral, and cognitive development [3, 4].
Because lead in the environment gradually accumulates in the body, lead is regarded as one of the most harmful environmental toxins to toddlers [5]. When the blood lead level reaches about 50 μg/L in the body of children, it can impair growth, memory, intelligence, and behavior, even when there is no obvious clinical manifestation. The most important untoward effect of lead exposure is the impairment of the intelligence of infants and the learning abilities of children. Most recent investigations have verified that [6–8] lead exposure can affect learning and memory, and the intelligence quotient of children is inversely proportional to their blood lead level. Because childhood lead poisoning is quite common in China at present, it should be given adequate attention.
Most international long-term follow-up investigations of the effects of lead exposure on neurological dysfunctions in children have reported that these effects of lead are persistent, especially lead exposure in 2-year-old children, an age that appears to be a critical period for a child’s later intelligence quotient and academic achievement [9]. There is very strong evidence clearly indicating that lead has a negative influence on children's intelligence and behavioral development. The subjects in this study were mainly Chinese children between 2 and 6 years of age. Because of the age of the subjects, the universal intelligence development diagnostic scale of China (Gesell Development Schedules) [10] was used to assess intelligence development, and the most commonly used Achenbach Child Behavior Checklist (CBCL) [11, 12] was used for the behavioral evaluations. In this study, we investigated the relationships between lead poisoning and intelligence and neurobehavioral changes in 2–4-year-old children, to provide a basis for clinical prevention and treatment measures.
Subjects and methods
Subjects
Ten children were randomly selected from each kindergarten in Xi’an. A total of 100 children were selected from ten kindergartens with an average age 2.8 years (SD = 1.45) and an age range of 2.2–3.9 years old. The exclusion criteria we used were (1) birthing problems such as delivery injuries or a low birth weight, (2) neonatal problems such as asphyxia, intracranial hemorrhage, hypoxic-ischemic encephalopathy, and severe jaundice, (3) acquired disabilities including poisoning, cerebral trauma, encephalitis, meningitis, encephalopathy and cerebral injuries following convulsions, and (4) potential factors influencing cognitive development such as malnutrition and inherited metabolic diseases. Based on these criteria, 96 children were selected to receive blood lead level detection tests.
Determination of blood levels of lead
Blood levels of lead were determined by differential potentiometric stripping analysis (DPSA). A pre-coated mercury film method was used. Mercury film was pre-plated on the working electrode three times before detection, accumulating to a thickness that enabled it to work for 4 consecutive hours. Pb2+ and Hg2+ were enriched in the mercury film in selected conditions. Amalgam was stripped in a static mode. The content of Pb2+ and Hg2+ was quantified according to the peak of the stripping curve. The samples were detected without digestion.
Blood samples of 40 μL were collected and placed into 4 mL of de-ionized water. The color of the sample changed from purplish red to yellow after addition of 1.0–1.2 mol/L of a hydrochloric acid solution and 2.0 mL of a 0.01 mol/L KMnO4 solution. The color faded after addition of 0.1 mL of 50 g/L ascorbic acid. After 20 min, 75 μL × 10-2 mol/L of a mercury solution was added to the sample in a three-electrode system, and the peak was recorded. A blank reagent was processed at the same time. The lead content in the blood sample and reagent blank was calculated by a standard addition method, and the absolute difference between the two samples was regarded as the lead content.
The diagnostic criterion for lead poisoning in children was updated by the Centers for Disease Control and Prevention (CDC) in 2012 to a blood lead value of ≥50 μg/L, whether or not there are corresponding clinical signs or other blood biochemical changes. The children in this study were divided into a control group (blood lead value < 50 μg/L) and lead poisoning group (blood lead value ≥ 50 μg/L) according to this criterion.
Questionnaire and behavioral assessments
The parents of the children in both groups were required to fill out a health questionnaire and CBCL for the children. The significance of this investigation and the project requirements were explained to the parents before they filled out the questionnaire, which was collected immediately. The content of the health questionnaire included approximately 40 questions related to source of exposure to lead, such as the family and social environment, life and health habit, and health conditions of the children. The main risk factors for high blood lead values could be assessed through questionnaire assignment analysis. A number of well-known instruments exist for assessing and categorizing the problem behavior of children. One of the most respected instruments in this area is the Child Behavior Checklist (CBCL; Achenbach, 1991). The CBCL is a paper-based questionnaire that presents caregivers with a series of 113 statements that relate to emotional and behavioral problems and competencies, using a 3-point response format to establish the frequency of problem behavior. Follow-up studies by the author of the CBCL (Achenbach, 1995; Achenbach & Howell, 1993) [13, 14] and hundreds of studies relying on this instrument have reported adequate reliability and validity of CBCL scores in various populations, although there have been some challenges to this instrument (e.g., Raadal, Milgrom, Cauce, & Mancl, 1994) [15]. This study used the child and teenager psychological test software 2.0 to input and analyze the CBCL scores, and to provide measures of social withdrawal, depression, sleep problems, atypical body actions, previous medical diagnoses, aggression, and destruction.
Intellectual development test
The development schedules used in this study were a set of four timetables devised by Arnold Gesell (1880–1961) at Yale University to evaluate the physical, emotional, and behavioral development of infants, toddlers, and preschoolers. They describe typical behavior at specific ages in the following areas: ability to adapt, motor functioning, use of language, and social interaction [16]. Here, the intellectual development test was conducted by professionals using the intelligence development diagnostic scale for children (0–6 years old) in subjects in both groups. A children’s intelligence development diagnostic scale called the Gesell Development Schedules as revised by the Beijing intelligence development group was used to assess the developmental quotients each child’s adaptive behavior, gross motor performance, fine motor movements, language development, and individual social behaviors.
Statistical methods
All numerical variables in this experiment are expressed as means, standard deviations, minimum values, and maximum values. Enumeration data are expressed by case number, rate, and constituent ratio. Blood lead values between the experimental and control groups were compared using a t-test after logarithmic transformation (meet normal distribution). The cognitive development diagnostic scale results of the two groups were compared by t-test, the comparison of the prevalence of abnormal behavior in the two groups was conducted by a χ2 test, and scores on each behavior factor and the total behavioral score were analyzed by the rank-sum test. SPSS11.5 statistical software was used to analyze all data, and P < 0.05 was taken as being significant statistical difference. All test conducted were two-tailed, and the test statistic and its correspondent P value are shown.
Results
The relationship between blood lead levels and cognitive development in children
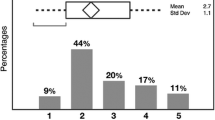
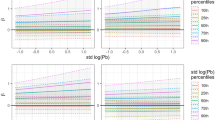
The blood lead value in 76 children was 4–246 μg/L, with the average blood lead value mean (±SD) of 88.39 (±67.92) μg/L. The log transformed blood lead values ranged 0.60–2.39, with an average blood lead logarithmic value mean (±SD) of 1.81 (±0.52). Scores on the child adaptive behavior developmental quotient, gross motor developmental quotient, fine motor movement developmental quotient, language developmental quotient, and individual- social behavior were 63–132, 69–135, 58–157, 59–138 and 68–136, respectively, with means (±SD) of 95.36 (±14.71), 96.03 (±14.68), 100.42 (±17.65), 92.08 (±16.95), and 107.54 (±14.15), respectively. Regression and correlation analysis (Table 1) showed that blood lead levels had an obvious negative correlation with the developmental quotients of child adaptive behavior, gross motor performance, fine motor movements, language development, and individual social behavior.
Compared with the control group, scores on the measure of developmental quotients of child adaptive behavior, gross motor performance, fine motor movements, language development, and individual social behavior lagged in the children previously exposed to lead, at 20.15, 13.28, 17.82, 20.99, and 14.75, respectively. The comparisons (Table 2) between the two groups showed that there were significant differences on these 5 developmental quotients.
The relationship between blood lead levels and behavior in children
The examination showed that there were 11 subjects with social withdrawal, 17 subjects with depression, 8 subjects with sleep problems, 6 subjects with atypical body actions, 34 subjects with aggressions, and 7 subjects with destructions among the 50 children in the lead poisoning group, and the rate of abnormal behavior was 27.7%. There were 7 subjects with social withdrawal, 4 subjects with melancholies, 5 subjects with sleep problems, 8 subjects with atypical body actions, 6 subjects with aggressions, and 5 subjects with destructions among the 50 children in the control group, and the rate of abnormal behavior was 11.7%. The rates of depression, aggressions, and abnormal behavior in the lead poisoning group were significantly higher than those in the control group (P < 0.01), and the rates of social withdrawal, sleep problems, aggressions, and destruction in the lead poisoning group were noticeably higher than those in the control group (P < 0.05). The prevalence of atypical body actions in the lead poisoning group was lower than that in control group (P > 0.05), and the prevalence of social withdrawal, sleep problems, atypical body actions, and destruction were significantly different between the two groups (P > 0.05) (Table 3).
Comparison of behavior factor scores between the two groups (Table 4) showed that depression, atypical body actions, aggressions, and total behavior scores in the children in the lead poisoning group were significantly different than in the children in the control group (P < 0.01), and the most significant differences (P < 0.05) were in social withdrawal and destruction, without obvious differences in sleep problems between the two group (P > 0.05).
Risk factor analysis of lead poisoning in children
Among the more than 40 factors we examined in the questionnaire, the risk factors for lead poisoning in children included poor living habits such as finger-sucking, nail-biting, putting foreign objects in the mouth, playing with plasticine, and using colored tableware frequently. They also included eating puffed food, preserved eggs, and canned food, smoking by a family member, living near a large road, and recent room decoration. Furthermore, the educational background of the parents was negatively correlated with elevated blood lead levels in children, and the statistical analysis indicated OR > 1, P < 0.05. Dietary protein was a protective factor against lead poisoning (B < 0, OR = 0.276 < 1, P < 0.05). The results of the logistic regression analysis are summarized in Table 5.
Discussion
Lead is a neurotoxin with no physiological functions in the human body, the ideal concentration of which in the blood is zero. However, because of the prevalence of lead in the environment, lead exists in the vast majority of human bodies. With the rapid development of industrialization, the production and use of lead, and its accumulative release, there has been a rapid increase in lead levels in the environment [17, 18]. Children are very sensitive to lead poisoning because of their metabolism and growth characteristics. Lead can easily penetrate the brains of children because their blood–brain barriers are not fully developed. Research has shown that the blood–brain barrier of newborn rats is highly permeable to lead, and that the younger the subject is, the greater is the permeability. The amounts of lead penetrating the blood–brain barriers of 16-day-old and 26-day-old rats were 2.42- and 2.05-times, respectively, that of adult rats under the same conditions [19]. Lead poisoning can have continuous damaging effects on children, influencing the development of nervous, cardiovascular, digestive, urological, reproductive, and endocrine systems, with the most sensitive to lead poisoning being the nervous system [20, 21].
That lead poisoning can impair the IQ of children has been verified by many Chinese and international scholars. Research by Schnass et al. [22] emphasized that the influence of blood lead levels in newborn children on a general cognitive index (GCI) gradually peaked at 1–3 years after birth, and this influence was most obvious on 4–5-year-olds. After studying 74 children at 4–14 years of age, Bellinger et al. [23] found that IQ is inversely proportional blood lead levels, and IQ values dropped about 6 points with every 100 μg/L increase in the level of lead in the blood. A high level of lead in the blood has adverse effects on intellectual development in children. A study by Miranda et al. implied that blood lead levels of 20–50 μg/L can impair the reading and math abilities of children [24]. Consistent with these results, we found that blood lead levels were significantly negatively correlated with the development quotients of children’s adaptive behavior, gross motor performance, fine motor performance, language development, and individual social behavior.
The earliest and most obvious influences of lead on the nervous system of children include neurobehavioral changes except for a decline in intelligence. It has been verified that lead exposure is associated with childhood behavior disorders [25]. Behavioral changes in 1–3-year-old children have been associated with low levels of lead exposure, which indicates that behavior disorders should be clinically monitored in children that have even low levels of lead exposure [26]. Lewendon et al. [27] found that blood levels of lead in children with behavior problems were higher than those in healthy children, and suggested that the blood lead content of children with behavior disorders should be monitored regularly. Mendola et al. [28] found low levels of perinatal lead exposure were associated with attention problems in children. Researchers also found recently that antisocial behavior, behavior disorders, and adolescent crime in childhood and adolescence are also related to lead exposure before and after birth [29–32]. The results of this study are consistent with those findings. There were significant differences between the scores for social withdrawal, depression, atypical body actions, aggressions, destructions, and total behavioral changes in children previously exposed to lead and the control group (P < 0.05), and there was no significant difference between these groups in sleeping problems. At present, most reports hold that blood lead levels have a relationship with behavior disorders in children, but no strong conclusions have been drawn yet as to which specific behaviors are influenced by lead exposure, which should be further studied [33, 34]. Human intakes lead mainly from food, water and respiration. The human body intakes 100–300 μg of lead every day from the gastrointestinal tract, and in adults, about 10% of this is absorbed into the body, whereas the absorption rate of children can reach 40%. The half-life of lead in blood and rapid-exchange soft tissue is less than one month, whereas the half-life of lead phosphate in skeleton can be 20 years [35].
Based on these collective findings, as an environmental pollutant, lead can be regarded as a “risk indicator” for the evaluation of IQ development [36]. The exact relationship between lead exposure and IQ changes remains uncertain. However, IQ is negatively correlated with blood lead levels. Moreover, we found more behavior disorders in children exposed to lead than in normal children, especially in terms of social withdrawal, depression, atypical body actions, aggressions, and destruction. Therefore, future studies should use multivariate analysis to elucidate the influence of lead poisoning on childhood intelligence and behavior, as this may clarify the mechanisms underlying the untoward effects of blood lead, and more importantly draw attention to comprehensive screening of lead poisoning in children. High blood lead levels and lead poisoning can be prevented. Because lead dust in the environment is the main source of lead poisoning in children, children’s food and tableware should be covered by dust shields. Furthermore, we should ensure the dietary balance and supply of various nutrients for children, and help children develop good eating habits. Prevention, early detection, and early intervention of childhood blood lead poisoning can be achieved through environmental interventions, health education, screening, and focused monitoring.
Consent
Written informed consent was obtained from the patient’s guardian/parent/next in keen for publication of this report and any accompanying images.
Abbreviations
- CBCL:
-
Child Behavior Checklist
- Cr2O3:
-
Chromium oxide
- CRM:
-
Certified Reference Material
- IQ:
-
Intelligence quotient
- PKC:
-
Protein kinase C
- MDA:
-
Malondialdehyde.
References
Zheng H, Lin WX, Hu HY, Huang JH, Huang MN, He YS: Effects of low-level Lead exposure on the neurobehavioral development of infants and early intervention. Zhonghua Yu Fang Yi Xue Za Zhi. 2008, 42 (3): 165-168.
Shen X, Wu S, Yan C: Impacts of low-level Lead exposure on development of children: recent studies in China. Clin Chim Acta. 2001, 313 (1–2): 217-20.
Carlisle JC, Dowling KC, Siegel DM, Alexeeff GV: A blood Lead benchmark for assessing risks from childhood Lead exposure. J Environ Sci Health A Tox Hazard Subst Environ Eng. 2009, 44 (12): 1200-8. 10.1080/10934520903139829.
Cleveland LM, Minter ML, Cobb KA, Scott AA, German VF: Lead hazards for pregnant women and children: part 2: more can still be done to reduce the chance of exposure to Lead in at-risk populations. Am J Nurs. 2008, 108 (11): 40-47. 10.1097/01.NAJ.0000339156.09233.de. quiz 47–8
Ferguson A, Bursac Z, Kern DF: Arkansas People Participating in Lead Education (APPLE): results of a Lead-safe training program. J Community Health. 2011, 36 (3): 367-374. 10.1007/s10900-010-9317-7.
Xu J, Yan CH, Yang B, Xie HF, Zou XY, Zhong L, Gao Y, Tian Y, Shen XM: The role of metabotropic glutamate receptor 5 in developmental Lead neurotoxicity. Toxicol Lett. 2009, 191 (2–3): 223-530.
Kasten-Jolly J, Heo Y, Lawrence DA: Central nervous system cytokine gene expression: modulation by lead. J Biochem Mol Toxicol. 2011, 25 (1): 41-54. 10.1002/jbt.20358.
Olympio KP, Gonçalves C, Günther WM, Bechara EJ: Neurotoxicity and aggressiveness triggered by low-level Lead in children: a review. Rev Panam Salud Publica. 2009, 26 (3): 266-275.
Chen A, Dietrich KN, Ware JH, Radcliffe J, Roqan WJ: IQ and blood Lead from 2 to 7 years of age: are the effects in older children the residual of high blood Lead concentrations in 2-year-olds?. Environ Health Perspect. 2005, 113 (5): 597-601. 10.1289/ehp.7625.
Ames LB: Arnold Gesell: Themes of His Work. 1989, New York: Human Sciences Press
Achenbach TM: Manual for the Child Behavior Checklist/4-18 and 1991 Profile. 1991, Burlington. VT: University of Vermont, Department of Psychiatry
Achenbach TM: Manual for the Teacher's Report form and 1991 Profile. 1991, Burllington, VT: University of Vermont, Department of Psychiatry
Achenbach TM: “Behavior problems in 5- to 11-year-old children from low-income families”: of norms and cutoffs. J Am Acad Child Adolesc Psychiatry. 1995, 34: 536-537. 10.1097/00004583-199505000-00003.
Achenbach TM, Howell CT: Are American children’s problems getting worse? A 13-year comparison. J Am Acad Child Adolesc Psychiatry. 1993, 32: 1145-1154. 10.1097/00004583-199311000-00006.
Raadal M, Milgrom P, Cauce AM, Mancl L: Behavior problems in 5- to 11-year-old children from low-income families. J Am Acad Child Adolesc Psychiatry. 1994, 33: 1017-1025. 10.1097/00004583-199409000-00013.
Cohen LG, Spenciner LJ: Assessment of Young Children. 1994, New York: Longman
Ray TK, Laskar AR: Lead intoxication in children: a global concern. Natl Med J India. 2004, 17 (6): 320-321.
Needleman H: Lead poisoning. Annu Rev Med. 2004, 55: 209-220. 10.1146/annurev.med.55.091902.103653.
Bellinger D, Leviton A, Waternaux C, Needleman H, Rabinowitz M: Longitudinal analyses of prenatal and postnatal Lead exposure and early cognitive development. N Eng J Med. 1987, 316 (17): 1037-43. 10.1056/NEJM198704233161701.
Oszlánczi G, Papp A, Szabó A, Nagymajtényi L, Sápi A, Kónya Z, Paulik E, Vezér T: Nervous system effects in rats on subacute exposure by Lead-containing nanoparticles via the airways. Inhal Toxicol. 2011, 23 (4): 173-181. 10.3109/08958378.2011.553248.
Burke MG, Miller MD: Practical guidelines for evaluating Lead exposure in children with mental health conditions: molecular effects and clinical implications. Postgrad Med. 2011, 123 (1): 160-168. 10.3810/pgm.2011.01.2256.
Schnaas L, Rothenberg SJ, Perroni E, Martínez S, Hernández C, Hernández RM: Temporal pattern in the effect of postnatal blood Lead level on intellectual development of young children. Neurotoxicol Teratol. 2000, 22 (6): 805-810. 10.1016/S0892-0362(00)00101-X.
Bellinger DC, Hu H, Kalaniti K, Thomas N, Rajan P, Sambandam S, Ramaswamy P, Balakrishnan K: A pilot study of blood Lead levels and neurobehavioral function in children living in Chennai, India. Int J Occup Environ Health. 2005, 11 (2): 138-143.
Miranda ML, Kim D, Galeano MA, Paul CJ, Hull AP, Morgan SP: The relationship between carly childhood blood Lead levels and performance on end-of-grade tests. Environ Health Perspect. 2007, 115 (8): 1242-1247. 10.1289/ehp.9994.
Gilbert SG, Weiss B: A rationale for lowering the blood Lead action level from 10 to 2 microg/dL. Neurotoxicology. 2006, 27 (5): 693-701. 10.1016/j.neuro.2006.06.008.
Mendelsohn AL, Dreyer BP, Fierman AH, Rosen CM, Legano LA, Kruger HA, Lim SW, Courtlandt CD: Low-level Lead exposure and behavior in early childhood. Pediatrics. 1998, 101 (3): E10-10.1542/peds.101.3.e10.
Lewendon G, Kinra S, Nelder R, Cronin T: Should children with developmental and behavioural problems be routinely screened for Lead?. Arch Dis Child. 2001, 85 (4): 286-288. 10.1136/adc.85.4.286.
Mendola P, Selevan SG, Gutter S, Rice D: Environmental factors associated with a sperctrum of neurodevelopmental deficits. Ment Retard Dev Disabil Res Rev. 2002, 8 (3): 188-197. 10.1002/mrdd.10033.
Nevin R: How Lead exposure relates to temporal changes in IQ, violent crime, and unwed pregnancy. Environ Res. 2000, 83 (1): 1-22. 10.1006/enrs.1999.4045.
Dietrich KN, Ris MD, Succop PA, Berger OG, Bornschein RL: Early exposure to Lead and juvenile delinquency. Neurotoxicol Teratol. 2001, 23 (6): 511-518. 10.1016/S0892-0362(01)00184-2.
Needleman HL, McFarland C, Ness RB, Fienberg SE, Tobin MJ: Bone Lead levels in adjucated delinquents A case control study. Neurotoxicol Teratol. 2002, 24 (6): 711-717. 10.1016/S0892-0362(02)00269-6.
Olympio KP, Oliveira PV, Naozuka J, Cardoso MR, Marques AF, Günther WM, Bechara EJ: Surface dental enamel Lead levels and antisocial behavior in Brazilian adolescents. Neurotoxicol Teratol. 2010, 32 (2): 273-279. 10.1016/j.ntt.2009.12.003.
Yeoh B, Woolfenden S, Wheeler D, Alperstein G, Lanphear B: Household interventions for prevention of domestic Lead exposure in children. Cochrane Database Syst Rev. 2008, 16 (2): CD006047-
Marchetti C: Molecular targets of Lead in brain neurotoxicity. Neurotox Res. 2003, 5 (3): 221-236. 10.1007/BF03033142.
Heath LM, Soole KL, McLaughlin ML, McEwan GT, Edwards JW: Toxicity of environmental Lead and the influence of intestinal absorption in children. Rev Environ Health. 2003, 18 (4): 231-50.
Jakubowski M: Low-level environmental Lead exposure and intellectual impairment in children–the current concepts of risk assessment. Int J Occup Med Environ Health. 2011, 24 (1): 1-7. 10.2478/s13382-011-0009-z.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
HSX and DYC carried out the studies and drafted the manuscript. YLF and LL designed the study and performed the statistical analysis. JPP and QN collected the questionnaires and conduct the analyses. DBJ and LXD conceived the study, participated in its design and coordination, and drafted the manuscript. WZL and ZG performed the experiments. All authors read and approved the final manuscript.
Shuangxing Hou, Lianfang Yuan contributed equally to this work.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Hou, S., Yuan, L., Jin, P. et al. A clinical study of the effects of lead poisoning on the intelligence and neurobehavioral abilities of children. Theor Biol Med Model 10, 13 (2013). https://doi.org/10.1186/1742-4682-10-13
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1742-4682-10-13