Abstract
Background
Most patients with chronic obstructive pulmonary disease (COPD) receive inhaled long-acting bronchodilators and inhaled corticosteroids. Conventional meta-analyses established that these drugs reduce COPD exacerbations when separately compared with placebo. However, there are relatively few head-to-head comparisons and conventional meta-analyses focus on single comparisons rather than on a simultaneous analysis of competing drug regimens that would allow rank ordering of their effectiveness. Therefore we assessed, using a network meta-analytic technique, the relative effectiveness of the common inhaled drug regimes used to reduce exacerbations in patients with COPD.
Methods
We conducted a systematic review and searched existing systematic reviews and electronic databases for randomized trials of ≥ 4 weeks' duration that assessed the effectiveness of inhaled drug regimes on exacerbations in patients with stable COPD. We extracted participants and intervention characteristics from included trials and assessed their methodological quality. For each treatment group we registered the proportion of patients with ≥ 1 exacerbation during follow-up. We used treatment-arm based logistic regression analysis to estimate the absolute and relative effects of inhaled drug treatments while preserving randomization within trials.
Results
We identified 35 trials enrolling 26,786 patients with COPD of whom 27% had ≥ 1 exacerbation. All regimes reduced exacerbations statistically significantly compared with placebo (odds ratios ranging from 0.71 (95% confidence interval [CI] 0.64 to 0.80) for long-acting anticholinergics to 0.78 (95% CI 0.70 to 0.86) for inhaled corticosteroids). Compared with long-acting bronchodilators alone, combined treatment was not more effective (comparison with long-acting beta-agonists: odds ratio 0.93 [95% CI 0.84 to 1.04] and comparison with long-acting anticholinergics: odds ratio 1.02 [95% CI 0.90 to 1.16], respectively). If FEV1 was ≤ 40% predicted, long-acting anticholinergics, inhaled corticosteroids, and combination treatment reduced exacerbations significantly compared with long-acting beta-agonists alone, but not if FEV1 was > 40% predicted. This effect modification was significant for inhaled corticosteroids (P = 0.02 for interaction) and combination treatment (P = 0.01) but not for long-acting anticholinergics (P = 0.46). A limitation of this analysis is its exclusive focus on exacerbations and lack of FEV1 data for individual patients.
Conclusion
We found no evidence that one single inhaled drug regimen is more effective than another in reducing exacerbations. Inhaled corticosteroids when added to long-acting beta-agonists reduce exacerbations only in patients with COPD with FEV1 ≤ 40%.
Similar content being viewed by others
Background
Chronic obstructive pulmonary disease (COPD) has become a leading cause of death worldwide and its management requires an enormous amount of human and financial resources [1, 2]. Reduction of exacerbation rates is one of the main treatment goals in COPD management since exacerbations bear heavily on the patient's health-related quality of life and prognosis as well as on COPD-related costs [3]. Several conventional meta-analyses provided evidence that long-acting beta-agonists, long-acting anticholinergics and inhaled corticosteroids reduce exacerbations in patients with COPD when compared with placebo [4–6]. The conventional meta-analyses are, however, less informative about the comparative effectiveness of long-acting beta-agonists and anticholinergics or about the additional value of inhaled corticosteroids when added to long-acting bronchodilators. The comparative effectiveness is of great interest to physicians because the predominant question in clinical practice is to choose between treatments rather than deciding whether to treat or not to treat [7, 8].
Opinions differ about whether a long-acting bronchodilator alone is sufficient or if an inhaled corticosteroid provides additional benefits at least for some patients [3, 9, 10]. Any added benefit of corticosteroids, if present, should outweigh the associated risk for adverse effects and their additional costs. Conventional meta-analyses [4–6, 11, 12] do not provide enough support to solve this debate because evidence from randomized head-to-head comparisons is often unavailable. Also, conventional meta-analyses cannot provide effect estimates for comparisons of more than two treatments at the same time, so that a ranking of competing treatments is not available. Finally, conventional meta-analyses cannot assess subgroup effects reliably [13] although such information is very valuable for clinicians. Theoretically, a single very large trial would overcome these three limitations of conventional meta-analysis. However, the sample size would need to be a multiple of that of the recently published TORCH trial [14] (more than 6000 patients) if subgroup effects were to be investigated.
Since such a trial is very unlikely to become available, a network meta-analysis or individual patient data meta-analysis can be very informative [15]. Such pooled analyses unify evidence from all randomized trials while fully preserving randomization [16–18]. Therefore, our aim was to assess the relative effectiveness of competing inhaled drug regimens for the prevention of exacerbations in patients with stable COPD in a pooled analysis of randomized comparisons. In addition, we assessed whether the effectiveness depend on the severity of COPD, treatment duration, or the definition of an exacerbation (event based or symptom based).
Methods
Data sources and selection
We searched the Cochrane Database of Systematic Reviews (Oxford, United Kingdom, 2007, Issue 2), the Database of Abstracts of Reviews of Effects (last search on November 20th 2007) and the Health Technology Assessment database (last search November on 20th 2007) for randomized trials included in existing systematic reviews (see Additional file 1 for systematic reviews used to identify relevant studies). We based our searches on existing systematic reviews in order to avoid unnecessary duplication of previous work. The existing systematic reviews used extensive search strategies that included several databases such as Medline, EMBASE, CINAHL and LILACS as well as websites of regulatory bodies. In addition, drug companies were approached for unpublished trials. We complemented these searches by entering all included studies into the 'related articles' function of PubMed (last search for trials on November 20th, 2007).
We included randomized trials without any language restrictions that were ≥ 4 weeks in duration, included patients with stable COPD, and assessed the effects of long-acting beta-agonists, long-acting anticholinergics, inhaled corticosteroids, or combination treatment (long-acting beta-agonists plus inhaled corticosteroids) on exacerbations with or without placebo control. We included all trials where the proportion of patients with at least one exacerbation during follow-up was reported. We did not include trials where only the mean number of exacerbations per patient year was reported because meta-analysis of such data is prone to bias without individual patient data [19].
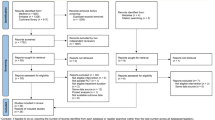
We retrieved all full reports of potentially eligible trials. Two reviewers (research fellows with medical doctor degrees and one and three years of research experience, respectively) independently assessed them and determined their inclusion or exclusion. If the two reviewers disagreed even after discussion, a third reviewer (epidemiologist with MD and PhD degree) arbitrated. Out of 56 trials identified initially, we excluded 20 (Figure 1, see also Additional file 2 for excluded studies). Another trial met the inclusion criteria but it could not be included in the analysis because the treatments (combination of long-acting beta-agonist, long-acting anticholinergic and inhaled corticosteroid versus one or two components), were dissimilar to those in the included trials [20]. We included the remaining 35 randomized trials in the analysis [14, 21–54]. One trial [35] was republished together with another trial [24]. We considered the data from both trials as published in the second report [24].
Study flow from database searches to inclusion oftrials. 40 trials were excluded after title and abstract screening because they obviously did not fulfill the inclusion criteria (not patients with COPD, patients with unstable COPD, short-acting bronchodilators, treatment duration < 4 weeks, no exacerbations ascertained). Reasons for exclusion for the 20 studies excluded after full text assessment are listed in Additional file 2.
Data extraction
We focused our analysis on exacerbations. For each trial arm (2 to 4, depending on the trial), one reviewer extracted the number of patients with at least one exacerbation during follow-up and the number of patients with no exacerbation during follow-up (2 × 2, 3 × 2, or 4 × 2 tables). A second and, in case of disagreement, third reviewer, checked the data extraction for correctness. We also recorded whether the studies' definition of exacerbation was event based (physician or emergency room visit, hospital admission) or symptom based (increase of dyspnea, sputum, or cough; for example according to Anthonisen et al [55]) and recorded the severity of exacerbation according to the Operational Classification of Severity of the European Respiratory and American Thoracic Societies (severe or mild to moderate exacerbation defined as requiring inpatient treatment or outpatient treatment, respectively) [9]. We recorded the drugs that were evaluated and classified them into the categories of placebo, long-acting beta-agonists (salmeterol, formoterol), long-acting anticholinergics (tiotropium bromide), and inhaled corticosteroids (budesonide, fluticasone, flunisolide, or beclomethasone), or combined treatment with a long-acting beta-agonist and an inhaled corticosteroid. Finally, we recorded treatment duration in weeks, the patient group's mean age, and mean FEV1.
Study reporting quality assessment
For each trial, two reviewers independently evaluated the quality of reporting for important components of internal validity (Additional file 3). We assessed the method of randomization, concealment of random allocation and whether inclusion criteria were specified in order to judge whether confounding was controlled for by randomization and/or restriction. We recorded blinding of treatment providers and patients to judge the presence of information bias and we recorded whether an intention-to-treat analysis was reported to assess if randomization was maintained throughout the analyses. We resolved discordant scores based on real differences in interpretation through consensus or third party arbitration. We used the quality assessment to judge the validity of the trial results.
Data synthesis and analysis
Based on 2 × 2 tables from each study (or 3 × 2 and 4 × 2 tables, respectively), we created as many data entries with respective coding for treatment and exacerbation (yes/no) as there were patients in the respective cell. For example, in the study of Brusasco et al [24] there were 156 patients in the placebo group with an exacerbation and 244 patients without an exacerbation, resulting in 156 (exacerbation = yes) and 244 (exacerbation = no) data entries for the 400 patients with placebo. For each of these entries we entered the mean age and FEV1 as covariates. For a detailed description of creating such a data set, see Additional file 4.
We performed a logistic regression arm-level analysis with the presence of exacerbation as dependent and the different treatment options as independent variables. We started with placebo treatment as the reference group followed by identical analyses where long-acting beta-agonists, long-acting anticholinergics and inhaled corticosteroids, respectively, served as reference group to which the other treatments were compared. To preserve randomization within each trial, we included a dummy variable for each of the studies. This dummy variable also adjusted for differences in risk profiles and study setup between trials. Second, we conducted stratified analyses to assess whether treatment duration or follow-up, respectively, disease severity (expressed by FEV1), or the definition of exacerbation influenced the (relative) treatment effects. We performed separate analyses for trials with a treatment duration of ≤ and > 6 months and≤and > 12 months, for trials with event- or symptom-based exacerbations, and for trials including patients with a mean post-bronchodilator FEV1 of ≤ and > 40% and 50% predicted (where available). We did not select 35% predicted as cut-off because there was only one trial [47] with such a low mean FEV1. To assess effect modification formally, we tested for interaction by introducing product terms between predictor variables and treatments into the logistic regression analysis. With a random coefficient model, we investigated the presence of any additional variation of the treatment effects due to differences across trials [56]. All analyses were conducted using STATA (STATA™ for Windows, version 9, Stata Corp; College Station, TX).
Role of the funding source
This work was supported by the Swiss National Science Foundation and The Helmut Horten Foundation. These funding sources did not have any influence on the planning, conduct and reporting of this study.
Results
Study characteristics
Table 1 (parts A-E) shows the characteristics of the 35 trials with 26,786 patients. Median sample size per trial was 545 (interquartile range, 253 to 976). On the patient level, median treatment duration was 25 weeks (interquartile range, 12 to 52), median age was 64 years (interquartile range, 63 to 65), and median FEV1 42% predicted (interquartile range, 40 to 46). A total of 26 trials (74%) with 23,245 patients used an event-based definition for exacerbations, and nine trials (26%) with 3541 patients had a symptom-based definition. 7201 patients (27%) suffered from at least one exacerbation. A total of 8312 patients received placebo (32 trials), 6357 received long-acting beta-agonists (21 trials), 4764 received a long-acting anticholinergic (11 trials), 3492 an inhaled corticosteroid (12 trials), and 3861 patients combination treatment (8 trials).
Quality of reporting
The median number of adequately reported aspects of study quality was 4 out of 6 (interquartile range 3–5, Additional file 1). This was largely influenced by the frequent reporting of inclusion criteria and blinding (94.1% of trials). However, the method of randomization (35.3%), concealment of random allocation (29.4%) and an intention to treat analysis (50.0%) were reported less frequently.
Comparisons of inhaled drug regimes
All treatments significantly reduced exacerbations when compared with placebo, with odds ratios ranging from 0.71 (95% confidence interval [CI] 0.64 to 0.80) for long-acting anticholinergics to 0.78 (95% CI 0.70 to 0.86) for inhaled corticosteroids (Figure 2). Comparing active drugs among each other, we found no significant differences between long-acting beta-agonists, long-acting anticholinergics, inhaled corticosteroids, and combination treatment. In particular, there were no significant differences between long-acting beta-agonists and long-acting anticholinergics (odds ratio, 0.91; 95% CI 0.81 to 1.03), or between combination treatment and long-acting beta-agonists (odds ratio, 0.93; 95% CI 0.84 to 1.04) or long-acting anticholinergics alone (odds ratio 1.02; 95% CI 0.90 to 1.16).
All comparisons among inhaled drug regimens. The forest plots show odds ratios (95% confidence intervals) indicating the odds of at least one exacerbation in patients with a drug treatment from the row as compared with treatment from the corresponding column. For example, the odds ratio of 0.91 (0.81 to 1.03) indicates that long-acting anticholinergics are more effective than long-acting beta-agonists, although not significantly so.
When we analyzed patients with FEV1 ≤ 40% (n = 9,434, mean FEV1 = 37% predicted), long-acting anticholinergics (odds ratio 0.83; 95% CI 0.71 to 0.98), inhaled corticosteroids (odds ratio 0.75; 95% CI 0.57 to 1.00), and combination treatment (odds ratio 0.79; 95% CI 0.67 to 0.93) reduced exacerbations significantly compared with long-acting beta-agonists alone (Figure 3). In patients with FEV1 > 40% predicted (n = 17,352, mean FEV1 = 46% predicted), there were no differences between treatments. Thus, the difference between point estimates in patients with FEV1 ≤ or > 40% was small for long-acting anticholinergics (0.09) but larger for inhaled corticosteroids (0.35) and combination treatment (0.26). This effect modification was confirmed when we tested for effect modification formally (P = 0.46 for long-acting anticholinergics, P = 0.02 for inhaled corticosteroids, and P = 0.01 for combination treatment). Effects of long-acting anticholinergics and combination treatment did not differ significantly (odds ratio 0.94; 95% CI 0.80 to 1.11). There was no effect modification when stratified for FEV1 ≤ or > 50%. In the other stratified analyses (stratified for treatment duration of ≤ and > 6 months and ≤ and > 12 months as well as for definition of exacerbation), we did not observe any influence of treatment duration or the definition of exacerbations on (relative) treatment effects.
The random coefficient model showed very similar point estimates and 95% CIs. Compared with the simpler logistic regression model, there was very small extra variability arising from differences of treatment effects across trials (point estimates of interstudy variances range from 10-6 to 10-9).
Discussion and conclusion
Based on 35 trials, our analysis showed that all inhaled drug regimens significantly reduced exacerbations but there were no significant differences between them. Thus, it appears that inhaled corticosteroids provide no additional value in reducing exacerbations when used concurrently with long-acting beta-agonists. However, combination treatment appeared to be more effective than beta-agonists alone in patients with low FEV1.
According to the recently published BOLD study, the prevalence of COPD with GOLD stage II to IV in populations over 40 years of age is around 10%, and approximately 80% of these patients have an FEV1 ≥ 50% predicted (GOLD stage II) [57]. For these patients, our study suggests that single treatment with long-acting beta-agonists or long-acting anticholinergics is not only the treatment of choice for symptom control but also for preventing exacerbations. Although common practice is to prescribe inhaled corticosteroids also [58, 59], our findings suggest that these patients do not need the additional medical therapy to reduce exacerbations.
In contrast, in patients with low FEV1 (below 40% predicted), long-acting anticholinergics appear to be the most attractive choice. They are as effective as combination treatment in reducing exacerbations but offer advantages in terms of costs and adverse effects [53]. The only head-to-head comparison of a long-acting anticholinergic and combination treatment, the recently published INSPIRE study, identified outcomes in agreement with these findings [53]. The INSPIRE study also showed no clinically relevant differences in health-related quality of life (< 4 points on St. Georges Respiratory Questionnaire). A significant reduction in 2-year mortality was observed with combination treatment (3%) compared with the long-acting anticholinergic (6%). However, this mortality analysis should be interpreted with caution because a closer look at how death was ascertained in the INSPIRE trials reveals that death was only recorded for patients who did not withdraw from treatment (65.5% with combined treatment and 58.3% with long-acting anticholinergic). Thus, it appears that one third of patients did not enter the mortality analysis. Unfortunately, little evidence is available about the combination of long-acting anticholinergics and inhaled corticosteroids; however, a recent Canadian trial indicated that this combination could be the most effective treatment for reducing exacerbations in patients with low FEV1 [20].
Exacerbation is not the only outcome that should inform the decision for or against adding inhaled corticosteroids to long-acting bronchodilators. Other outcomes should be considered as well. A recent systematic review found no risk reduction in terms of mortality if an inhaled steroid was added to a long-acting bronchodilator [11]. Health-related quality of life was statistically significantly better after combined treatment (difference of -1.64 units on St. Georges Respiratory Questionnaire; 95% CI -2.28 to -1) but the effects were well under the threshold representing a minimal important difference (4 units) [11]. Arguments for treating COPD solely with long-acting beta-agonists are the substantially lower costs and lower risk for adverse effects such as pneumonia, oral candidiasis, or loss of bone density compared with combination treatment [11, 14, 53, 60]. Integrating and presenting this complex information about benefits and downsides of inhaled drug treatments is challenging. One approach is to use decision aids that are particularly valuable for value-sensitive decisions where the balance of benefits and downsides is not straightforward. As the decision is, in the case of inhaled drug treatment for COPD, only between two treatment options (bronchodilator(s) versus combined treatment), information about the comparisons with placebo could now be excluded for simplicity, since offering no treatment is not in the best interest of the patient. However, whether patients benefit from such informed decision-making requires testing in additional trials.
Unlike previous meta-analyses based on comparisons of inhaled drugs with placebo or, in some instances, with another inhaled drug [4–6, 11, 12], we argue that the comparative effectiveness of available treatments are of greater interest to physicians [7, 8]. To provide estimates for this comparative effectiveness, we used a new analytical approach to pool evidence from all available randomized trials. Such analyses may be, in many instances, the only way to estimate comparative treatment effectiveness; head-to-head comparisons are unavailable, and the sample sizes required to detect small differences are unfeasibly large. For comparison of inhaled COPD drugs, for example, thousands of patients are required just for the main comparison, not even accounting for subgroup effects.
There are other approaches for indirect comparisons [16–18]. An early and important contribution emphasized the importance of preserving randomization [16]. However, that proposed approach only allows for a single head-to-head comparison and not for simultaneous comparison of all treatments under consideration. Two other approaches [17, 18] are available, but the complexity of their statistical methods may represent a barrier for their application and interpretation [61]. Our approach is particularly attractive because it is transparent and easily reproducible. The multivariable logistic regression analysis allows for an analysis like that used in any randomized trial while keeping intact the randomization of each trial. The comparisons with placebo showed the same results as those of the meta-analyses of the Clinical Practice Guideline of the American College of Physicians [6]. When the odds ratios are transformed to relative risks [62], the effect estimates are identical to those of a conventional meta-analysis.
A limitation of our study is that we focused on exacerbations and did not consider additional outcomes such as health-related quality of life or mortality. When we planned the current analyses the body of evidence on mortality was too small to provide precise effect estimates, even if pooled. The TORCH trial [14] published in 2007 was the first trial that was powered to assess the effects of inhaled drugs on mortality, but even this very large trial turned out to be too small. Therefore, we decided to postpone analyses on mortality to a point in time where more data would become available. Another limitation is that we performed only a few stratified analyses. For physicians, knowing more about profile-specific effect estimates would be very useful. For example, more detailed information about risk factors for exacerbations, such as previous exacerbations, would enhance understanding about who benefits from the addition of inhaled corticosteroids. Single trials are unlikely to provide such information because of the very large sample sizes they would require for sufficient power to detect effect modification. Individual patient data meta-analysis and pooled analyses may solve this problem to some extent. However, reporting of such patient characteristics is highly variable, and retrieval of individual patient data from primary studies is challenging [63].
A limitation of any approach to pool data on exacerbations is that (relative) treatment effects can only be estimated adequately based on the proportion of patients with at least one exacerbation. Analysis of exacerbation rates expressed as mean exacerbation rates per person-year would offer a more comprehensive use of the data and would be less dependent on the length of follow-up. However, such data cannot be pooled adequately without having access to adequate and fully reported analyses that took within- and between-patient variability in exacerbations into account. But as Suissa points out, most trials are not analyzed and reported adequately[19]. Ideally, an individual patient data meta-analysis would be conducted but it is very challenging to convince investigators of all relevant trials to share their data [63]. The advantage of using the proportion of patients with at least one exacerbation is the limited influence of few patients with many exacerbations on the results. Also, physicians may be more familiar with this format and respective estimates for treatment effects such as odds ratios or relative risks than with mean differences in exacerbation rates. However, there is little evidence on how effect estimates should be presented in order to facilitate the transfer from research into practice.
A common problem of systematic reviews in COPD is poor reporting of clinical and spirometric characteristics of patients enrolled in included trials. It is sometimes difficult to judge whether all patients had COPD, or if some patients had other lung disease such as asthma. Also, there is often no separate reporting for moderate and severe exacerbations, although it would be informative to estimate the effects of inhaled steroids stratified for the severity of exacerbations. COPD is a heterogeneous disease and it is important that future studies provide more information about their patients, including clinical characteristics, lung function data and also information on co-treatments.
The results of our study may support physicians in selecting inhaled drug treatments for patients with COPD. In general, long-acting beta-agonists or anticholinergics appear to be the treatment of choice to reduce exacerbation rates. Adding an inhaled corticosteroid does not provide additional protection from exacerbations. In patients with low FEV1, combination treatment and long-acting anticholinergics should be favored because they reduce the risk for exacerbations more than single treatment with a long-acting beta-agonist. Our analyses, together with the existing meta-analyses that considered additional outcomes, inform patients and physicians to balance the benefits and downsides of different inhaled drug treatments for COPD.
References
Barnes PJ: Chronic obstructive pulmonary disease: a growing but neglected global epidemic. PLoS Med. 2007, 4: e112.
Lopez AD, Shibuya K, Rao C, Mathers CD, Hansell AL, Held LS, Schmid V, Buist S: Chronic obstructive pulmonary disease: current burden and future projections. Eur Respir J. 2006, 27: 397-412.
Wedzicha JA, Seemungal TA: COPD exacerbations: defining their cause and prevention. Lancet. 2007, 370: 786-796.
Nannini L, Cates C, Lasserson T, Poole P: Combined corticosteroid and long-acting beta-agonist in one inhaler versus placebo for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2007, 4: CD003794.
Yang IA, Fong KM, Sim EH, Black PN, Lasserson TJ: Inhaled corticosteroids for stable chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2007, 2: CD002991.
Wilt TJ, Niewoehner D, Macdonald R, Kane RL: Management of stable chronic obstructive pulmonary disease: a systematic review for a clinical practice guideline. Ann Intern Med. 2007, 147: 639-653.
Tunis SR, Stryer DB, Clancy CM: Practical clinical trials: increasing the value of clinical research for decision making in clinical and health policy. Jama. 2003, 290: 1624-1632.
Rothman KJ, Michels KB: The continuing unethical use of placebo controls. New Engl J Med. 1994, 331: 394-398.
American Thoracic Society and European Respiratory Society: Standards for the diagnosis and treatment of patients with chronic obstructive pulmonary disease. 2007, [http://www.ers-education.org/pages/default.aspx?id=725]
Suissa S, McGhan R, Niewoehner D, Make B: Inhaled corticosteroids in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2007, 4: 535-542.
Nannini L, Cates C, Lasserson T, Poole P: Combined corticosteroid and long-acting beta-agonist in one inhaler versus long-acting beta-agonists for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2007, 4: CD006829.
Nannini L, Cates C, Lasserson T, Poole P: Combined corticosteroid and long-acting beta-agonist in one inhaler versus inhaled steroids for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2007, 4: CD006826.
Berlin JA, Santanna J, Schmid CH, Szczech LA, Feldman HI: Individual patient-versus group-level data meta-regressions for the investigation of treatment effect modifiers: ecological bias rears its ugly head. Stat Med. 2002, 21: 371-387.
Calverley PM, Anderson JA, Celli B, Ferguson GT, Jenkins C, Jones PW, Yates JC, Vestbo J: Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. New Engl J Med. 2007, 356: 775-789.
Caldwell DM, Ades AE, Higgins JP: Simultaneous comparison of multiple treatments: combining direct and indirect evidence. BMJ. 2005, 331: 897-900.
Bucher HC, Guyatt GH, Griffith LE, Walter SD: The results of direct and indirect treatment comparisons in meta-analysis of randomized controlled trials. J Clin Epidemiol. 1997, 50: 683-691.
Lu G, Ades AE: Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med. 2004, 23: 3105-3124.
Lumley T: Network meta-analysis for indirect treatment comparisons. Stat Med. 2002, 21: 2313-2324.
Suissa S: Statistical treatment of exacerbations in therapeutic trials of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2006, 173: 842-846.
Aaron SD, Vandemheen KL, Fergusson D, Maltais F, Bourbeau J, Goldstein R, Balter M, O'Donnell D, McIvor A, Sharma S, Bishop G, Anthony J, Cowie R, Field S, Hirsch A, Hernandez P, Rivington R, Road J, Hoffstein V, Hodder R, Marciniuk D, McCormack D, Fox G, Cox G, Prins HB, Ford G, Bleskie D, Doucette S, Mayers I, Chapman K, Zamel N, FitzGerald M, Canadian Thoracic Society/Canadian Respiratory Clinical Research Consortium: Tiotropium in combination with placebo, salmeterol, or fluticasone-salmeterol for treatment of chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med. 2007, 146: 545-555.
Beeh KM, Beier J, Buhl R, Stark-Lorenzen P, Gerken F, Metzdorf N: Efficacy of tiotropium bromide (Spiriva) in patients with chronic-obstructive pulmonary disease (COPD) of different severities. Pneumologie. 2006, 341-346.
Bourbeau J, Rouleau MY, Boucher S: Randomised controlled trial of inhaled corticosteroids in patients with chronic obstructive pulmonary disease. Thorax. 1998, 53: 477-482.
Boyd G, Morice AH, Pounsford JC, Siebert M, Peslis N, Crawford C: An evaluation of salmeterol in the treatment of chronic obstructive pulmonary disease (COPD). Eur Respir J. 1997, 10: 815-821.
Brusasco V, Hodder R, Miravitlles M, Korducki L, Towse L, Kesten S: Health outcomes following treatment for six months with once daily tiotropium compared with twice daily salmeterol in patients with COPD. Thorax. 2003, 58: 399-404.
Burge PS, Calverley PMA, Jones PW, Spencer S, Anderson JA, Maslen TK: Randomised, double blind, placebo controlled study of fluticasone propionate in patients with moderate to severe chronic obstructive pulmonary disease: The ISOLDE trial. BMJ. 2000, 320: 1297-1303.
Calverley P, Pauwels R, Vestbo J, Jones P, Pride N, Gulsvik A, Anderson J, Maden C: Combined salmeterol and fluticasone in the treatment of chronic obstructive pulmonary disease: a randomised controlled trial. Lancet. 2003, 361: 449-456.
Calverley PM, Boonsawat W, Cseke Z, Zhong N, Peterson S, Olsson H: Maintenance therapy with budesonide and formoterol in chronic obstructive pulmonary disease. Eur Respir J. 2003, 22: 912-919.
Calverley PM, Lee A, Towse L, van NJ, Witek TJ, Kelsen S: Effect of tiotropium bromide on circadian variation in airflow limitation in chronic obstructive pulmonary disease. Thorax. 2003, 58: 855-860.
Campbell M, Eliraz A, Johansson G, Tornling G, Nihlen U, Bengtsson T, Rabe KF: Formoterol for maintenance and as-needed treatment of chronic obstructive pulmonary disease. Respir Med. 2005, 99: 1511-1520.
Celli B, Halpin D, Hepburn R, Byrne N, Keating ET, Goldman M: Symptoms are an important outcome in chronic obstructive pulmonary disease clinical trials: results of a 3-month comparative study using the Breathlessness, Cough and Sputum Scale (BCSS). Respir Med. 2003, 97 (Suppl A): S35-43.
Chapman KR, Arvidsson P, Chuchalin AG, Dhillon DP, Faurschou P, Goldstein RS, Kuipers AF, International study group: The addition of salmeterol 50 mug bid to anticholinergic treatment in patients with COPD: A randomized, placebo controlled trial. Can Respir J. 2002, 3: 178-185.
Covelli H, Bhattacharya S, Cassino C, Conoscenti C, Kesten S: Absence of electrocardiographic findings and improved function with once-daily tiotropium in patients with chronic obstructive pulmonary disease. Pharmacotherapy. 2005, 25: 1708-1718.
Dahl R, Greefhorst LA, Nowak D, Nonikov V, Byrne AM, Thomson MH, Till D, Della CG, Formoterol in Chronic Obstructive Pulmonary D: Inhaled formoterol dry powder versus ipratropium bromide in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001, 164: 778-784.
Dusser D, Bravo M-L, Iacono P, on behalf the MISTRAL study group: The effect of tiotropium on exacerbations and airflow in patients with COPD. Eur Respir J. 2006, 27 (3): 547-555.
Donohue JF, Van Noord JA, Bateman ED, Langley SJ, Lee A, Witek TJ, Kesten S, Towse L: A 6-month, placebo-controlled study comparing lung function and health status changes in COPD patients treated with tiotropium or salmeterol. Chest. 2002, 1: 47-55.
Littner MR, Ilowite JS, Tashkin DP, Friedman M, Serby CW, Menjoge SS, Witek TJ: Long-acting bronchodilation with once-daily dosing of tiotropium (Spiriva) in stable chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000, 161: 1136-42.
Mahler DA, Donohue JF, Barbee RA, Goldman MD, Gross NJ, Wisniewski ME, Yancey SW, Zakes BA, Rickard KA, Anderson WH: Efficacy of salmeterol xinafoate in the treatment of COPD. Chest. 1999, 115: 957-965.
Mahler DA, Wire P, Horstman D, Chang C, Yates J, Fischer T, Shah T: Effectiveness of fluticasone propionate and salmeterol combination delivered via the Diskus device in the treatment of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2002, 166: 1084-1091.
Niewoehner DE, Rice K, Cote C, Paulson D, Cooper JA, Korducki L, Cassino C, Kesten S: Prevention of exacerbations of chronic obstructive pulmonary disease with tiotropium, a once-daily inhaled anticholinergic bronchodilator: a randomized trial. Ann Intern Med. 2005, 143: 317-326.
Paggiaro PL, Dahle R, Bakran I, Frith L, Hollingworth K, Efthimiou J: Multicentre randomised placebo-controlled trial of inhaled fluticasone propionate in patients with chronic obstructuve pulmonary disease. Lancet. 1998, 351: 773-780.
Paggiaro PL, Vagaggini B, Di FA, Zingoni M, Fano M, Biraghi M: Efficacy of nebulized flunisolide combined with salbutamol and ipratropium bromide in stable patients with moderate-to-severe chronic obstructive pulmonary disease. Respiration. 2006, 73 (5): 603-609.
Rossi A, Kristufek P, Levine BE, Thomson MH, Till D, Kottakis J, Della CG: Comparison of the efficacy, tolerability, and safety of formoterol dry powder and oral, slow-release theophylline in the treatment of COPD. Chest. 2002, 121: 1058-1069.
Stockley RA, Chopra N, Rice L: Addition of salmeterol to existing treatment in patients with COPD: a 12 month study. Thorax. 2006, 61: 122-128.
Szafranski W, Cukier A, Ramirez A, Menga G, Sansores R, Nahabedian S, Peterson S, Olsson H: Efficacy and safety of budesonide/formoterol in the management of chronic obstructive pulmonary disease. Eur Respir J. 2003, 21: 74-81.
van der Valk , Monninkhof E, van der PJ, Zielhuis G, van HC: Effect of discontinuation of inhaled corticosteroids in patients with chronic obstructive pulmonary disease: the COPE study. Am J Respir Crit Care Med. 2002, 166: 1358-1363.
Van Noord JA, De Munck DRAJ, Bantje T, Hop WCJ, Akveld MLM, Bommer AM: Long-term treatment of chronic obstructive pulmonary disease with salmeterol and the additive effect of ipratropium. Eur Respir J. 2000, 15 (5): 878-885.
Wadbo M, Lofdahl CG, Larsson K, Skoogh BE, Tornling G, Arwestrom E, Bengtsson T, Strom K, Swedish Society of Respiratory Medicine: Effects of formoterol and ipratropium bromide in COPD: a 3-month placebo-controlled study. Eur Respir J. 2002, 20: 1138-1146.
Baumgartner RA, Hanania NA, Calhoun WJ, Sahn SA, Sciarappa K, Hanrahan JP: Nebulized arformoterol in patients with COPD: a 12-week, multicenter, randomized, double-blind, double-dummy, placebo- and active-controlled trial. Clin Ther. 2007, 29: 261-278.
Briggs DD, Covelli H, Lapidus R, Bhattycharya S, Kesten S, Cassino C: Improved daytime spirometric efficacy of tiotropium compared with salmeterol in patients with COPD. Pulm Pharmacol Ther. 2005, 18: 397-404.
Casaburi R, Mahler DA, Jones PW, Wanner A, San PG, ZuWallack RL, Menjoge SS, Serby CW, Witek T: A long-term evaluation of once-daily inhaled tiotropium in chronic obstructive pulmonary disease. Eur Respir J. 2002, 19: 217-224.
Hanania NA, Darken P, Horstman D, Reisner C, Lee B, Davis S, Shah T: The efficacy and safety of fluticasone propionate (250 microg)/salmeterol (50 microg) combined in the Diskus inhaler for the treatment of COPD. Chest. 2003, 124: 834-843.
Kardos P, Wencker M, Glaab T, Vogelmeier C: Impact of salmeterol/fluticasone propionate versus salmeterol on exacerbations in severe chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2007, 175: 144-149.
Wedzicha JA, Calverley PM, Seemungal TA, Hagan G, Ansari Z, Stockley RA: The prevention of chronic obstructive pulmonary disease exacerbations by salmeterol/fluticasone propionate or tiotropium bromide. Am J Respir Crit Care Med. 2008, 177: 19-26.
Weir DC, Bale GA, Bright P, Sherwood Burge P: A double-blind placebo-controlled study of the effect of inhaled beclomethasone dipropionate for 2 years in patients with nonasthmatic chronic obstructive pulmonary disease. Clin Exp Allergy. 1999, 29 (Suppl 2): 125-128.
Anthonisen NR, Manfreda J, Warren CP, Hershfield ES, Harding GK, Nelson NA: Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med. 1987, 106: 196-204.
Akl EA, Grant BJ, Guyatt GH, Montori VM, Schunemann HJ: A decision aid for COPD patients considering inhaled steroid therapy: development and before and after pilot testing. BMC Med Inform Decis Mak. 2007, 7: 12.
Buist AS, McBurnie MA, Vollmer WM, Gillespie S, Burney P, Mannino DM, Menezes AM, Sullivan SD, Lee TA, Weiss KB, Jensen RL, Marks GB, Gulsvik A, Nizankowska-Mogilnicka E, BOLD Collaborative Research Group: International variation in the prevalence of COPD (the BOLD Study): a population-based prevalence study. Lancet. 2007, 370: 741-750.
Viejo-Banuelos JL, Pueyo-Bastida A, Fueyo-Rodriguez A: Characteristics of outpatients with COPD in daily practice: The E4 Spanish project. Respir Med. 2006, 100: 2137-2143.
Fritsch K, Jacot ML, Klarer A, Wick F, Bruggmann P, Krause M, Thurnheer R: Adherence to the Swiss guidelines for management of COPD: experience of a Swiss teaching hospital. Swiss Med Wkly. 2005, 135: 116-121.
Scanlon PD, Connett JE, Wise RA, Tashkin DP, Madhok T, Skeans M, Carpenter PC, Bailey WC, Buist AS, Eichenhorn M, Kanner RE, Weinmann G, Lung Health Study Research Group: Loss of bone density with inhaled triamcinolone in Lung Health Study II. Am J Respir Crit Care Med. 2004, 170: 1302-1309.
Pocock SJ: Safety of drug-eluting stents: demystifying network meta-analysis. Lancet. 2007, 370 (9605): 2099-2100.
Deeks JJ, Altman DG: Effect measures for meta-analysis of trials with binary outcomes. Systematic Reviews in Health Care. Edited by: Egger M, Smith G, Altman D. 2001, London: BMJ Publishing Group, 313-335. 2
Stewart LA, Tierney JF: To IPD or not to IPD? Advantages and disadvantages of systematic reviews using individual patient data. Eval Health Prof. 2002, 25: 76-97.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1741-7015/7/2/prepub
Acknowledgements
Dr Milo A Puhan's (grant no. 3233B0/115216/1) and Dr Lucas M Bachmann's work (grants no. 3233B0-103182 and 3200B0-103183) was supported by the Swiss National Science Foundation. The Helmut Horten Foundation supported Dr Milo A Puhan, Dr M Bachmann and Dr G ter Riet.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None of the authors has any competing interests related to the content of this paper. Dr. Kleijnen received restricted research grants from Pfizer Ltd.
Authors' contributions
All authors had full access to all of the data in the study. MAP takes responsibility for the integrity of the data and accuracy of the data analysis. MAP, LMB, JK, and AGK undertook Study concept and design. MAP, LMB and AGK were responsible for data acquisition. MAP, LMB, JK, GtR and AGK performed Analysis and interpretation of data. MAP, LMB and AGK drafted the manuscript. JK and GtR undertook critical revision of the manuscript for important intellectual content. MAP, LMB, GtR and AGK performed the statistical analysis. JK and AGK supervised the study. All authors have read and approved the final manuscript.
Electronic supplementary material
12916_2008_180_MOESM4_ESM.doc
Additional file 4: Appendix 4. Approach to create new data set with n data entries where n is the total number of included patients. (DOC 38 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Puhan, M.A., Bachmann, L.M., Kleijnen, J. et al. Inhaled drugs to reduce exacerbations in patients with chronic obstructive pulmonary disease: a network meta-analysis. BMC Med 7, 2 (2009). https://doi.org/10.1186/1741-7015-7-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1741-7015-7-2