Abstract
Peripheral blood eosinophilia and vascular occlusions are rare occurrences in patients with pleural mesothelioma whereas eosinophilia may associate with thrombosis. We describe a patient with mesothelioma who developed peripheral blood eosinophilia followed by deep vein thrombosis despite being on low molecular weight heparin prophylaxis. We discuss the genesis of peripheral blood eosinophilia and thrombosis in pleural mesothelioma.
Similar content being viewed by others
Introduction
The latest nationwide census from the occupational United Kingdom physicians identified pleural mesothelioma (PM) in 92% of lung cancers patients [1] whereas PM represented only 8% of histology proven lung cancers accrued from an area without heavy industrial exposure to asbestos [2]. Peripheral blood eosinophilia (PBE) has been detected in 0.5% to 1.7% of patients with malignancy [3]: it may occur in cancer of the lung, pancreas, uterus, liver, breast, kidney and thyroid [3, 4], in liposarcomas [5] in lymphomas and T-cell-leukemias [6, 7] but it is quite rare in PM [8–11]. PBE is associated with metastatic spread, predicts a poor prognosis [12, 13], may disappear with treatment of the malignancy and reappear with tumour relapse [6, 14]. We describe a patient who developed PBE almost coincidentally with PM followed by deep vein thrombosis despite low molecular weight heparin prophylaxis and in the absence of inherited thrombophilia.
Case report
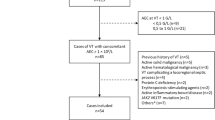
A 75-year old gentleman was admitted to the Oncology/Haematology Ward in early September 2007 for severe shortness of breath. He had been fully investigated for a pleural effusion one month earlier in a neighbouring hospital. At that time drained pleural fluid revealed reactive lymphocytes with neither neutrophils nor eosinophils. However peripheral blood esosinophils were raised at 1.6 × 109/L, C-reactive protein (CRP) at 33 mg/dl and fibrinogen at 568 mg/dl. Cultures for bacteria and stains for acid-fast bacilli were negative. Several stool examinations and serologic tests were negative for parasites as well as an autoimmune screen (antinuclear antibodies, antineutrophil-cytoplasmic antibodies, anti myeloperoxidase antibodies). A right pleural biopsy done in mid August 2007 revealed sheets of pleura infiltrated by malignant epithelioid cells that on immune staining expressed CK7 (cytokeratin) with focal expression of CK5/6 whereas staining for carcino-embriogenic antigen, BerEP4, thyroid transcription factor-1 mesothelin, Wilms' tumour -1, CK20 or prostate specific antigen was negative, confirming a diagnosis of epithelioid mesothelioma. A drain was inserted through the right chest wall and opiates started (morphine sulphate 30 modified release bd, oxycodone). During the current admission the drain was re-sited and fluid examination revealed only reactive lymphocytes and few neutrophils. His peripheral blood eosinophils had risen to 21 × 109/L, CRP was up at 88 mg/dl and fibrinogen at 880 mg/dl. The patient was started on a prophylactic dose of tinzaparin (3500 IU/day). On the fourth day after admission the patient developed a swollen calf, his D-dimer was greater than 1000 mg/dl (cut-off normal >280 mg/dl) and an ultrasound scan confirmed a fresh popliteal vein thrombosis. Tinzaparin was increased to therapeutic levels for five days until warfarin brought the international normalised ratio within therapeutic range. A thrombophilia screen (including factor V Leiden, prothrombin 20210, protein C, protein S, antithrombin, lupus anticoagulant and anticardiolipin antibodies) arranged before commencing warfarin came back normal. Neither the FIP1L1-PDGFRA fusion transcript (deletion 4q12) nor other cytogenetic abnormalities were found on a cellular sample of peripheral blood. After 5 days later his general conditions deteriorated, he became progressively confused with increasing hypoxia and passed away for respiratory failure. Post mortem revealed a mesothelioma that had diffusely surrounded and invaded the left lung and pericardium without directly affecting vascular structures. No asbestos bodies were found and no pulmonary embolism was detected.
Discussion
PBE is rare finding in mesothelioma: a large survey found one case out of 4710 patients with pleural involvement [8] whereas two more patients with pleural involvement [9, 10] and one with peritoneal involvement [11] have been described as case reports. In this setting PBE should be considered reactive as the tumour itself produces factors that promote eosinophil generation such as interleukin 3, interleukin 5 and granulocyte-monocyte colony stimulating factor [15]. The negative cytogenetic testing favours a reactive PBE in our patient.
Thrombosis development in PM is also rare: according to one series venous occlusions occurred in 6.5% (1/15) of cases [16], whereas an autopsy study on 111 patients with lung cancer identified 14 cases of PM of which 14% had evidence of clots in the venous circulation [17]; isolated reports documented occlusions of the superior vena cava [18, 19], of the left jugular and subclavian veins [20] and of the portal vein [21]. Arterial occlusions affected cerebral circulation in two cases [22, 23] and mesenteric vessels in one case (associated with nephrotic syndrome)[24].
The pathogenesis of thrombosis in PM is partly due to tumour tissue compressing veins [18, 20] that at times may progress to direct vessel infiltration [19] and partly due to a hypercoagulable state characterised by elevated levels of plasma fibrinogen [25] and increased fibrin turnover leading to disseminated intravascular coagulation [26].
Primary eosinophilic syndrome is strongly associated with thrombosis that may be recurrent despite adequate heparin and warfarin anticoagulation [27]. Eosinophils store and express tissue factor and once activated may initiate coagulation [28]. In addition eosinophils interfere with the activity of natural anticoagulants: eosinophilic cationic protein (ECP) binding to thrombomodulin prevents thrombin dependent activation of anticoagulant protein C [29] and binding to heparan sulphate (or heparin) prevents the conformational change required for the anti-thrombin neutralisation of thrombin [30]. Indeed an excess of ECP was able to override heparin binding to antithrombin [31] and may well explain the few instances where apparently therapeutic or prophylactic doses of heparin failed to prevent thrombosis [27, 32]. This was the situation of our patient who developed deep vein thrombosis being already on prophylactic low molecular weight heparin.
In conclusion we have reported an unprecedented patient with pleural mesothelioma in whom reactive PBE contributed to the development of deep vein thrombosis more than the tumour itself on the background of an inflammatory and eventually hypercoagulable state. Though difficult for mesothelioma, tumour treatment may relieve the reactive PBE [6, 14]. Clinicians should be aware of the added thrombotic risk of hypereosinophilia in cancer patients [33] and consider prophylactic or therapeutic anticoagulation according to clinical judgement and laboratory guidance, possibly with anti factor Xa monitoring in the case of low molecular weight heparin.
References
Meyer JD, Holt DL, Chen Y, Cherry NM, McDonald JC: SWORD '99: surveillance of work-related and occupational respiratory disease in the UK. Occup Med (Lond) 2001, 51: 204-208. 10.1093/occmed/51.3.204
Hamilton WT, Round AP, Sharp DJ, Peters TJ: High incidence of mesothelioma in an English city without heavy industrial use of asbestos. J Public Health 2004, 26: 77-78. 10.1093/pubmed/fdh116
Stefanini M, Claustro JC, Motos RA, Bendigo LL: Blood and bone marrow eosinophilia in malignant tumors. Cancer 1991, 64: 543-538. PublisherFullText 10.1002/1097-0142(19910801)68:3543::AID-CNCR28206803173.0.CO;2-3
Balducci L, Chapman SW, Little DD, Hardy CL: Paraneoplastic eosinophilia. Cancer 1989, 64: 2250-2253. PublisherFullText 10.1002/1097-0142(19891201)64:112250::AID-CNCR28206411113.0.CO;2-X
Coste F, Cayla J, Chevallier J, Basset F, Faye C: Un cas de liposarcome de la region scapulaire avec eosinophilie sanguine. Rev Rhum Mal Osteoartic 1960, 27: 493-496.
Catovsky D, Bernasconi C, Verdonck PJ, Postma A, Hows J, Does-van den Berg A, Rees JK, Castelli G, Morra E, Galton DA: The association of eosinophilia with lymphoblastic leukemia or lymphoma: A study of seven patients. Br J Hematol 1980, 45: 523-534. 10.1111/j.1365-2141.1980.tb07174.x
Reddy SS, Hyland RH, Alison RE, Sturgeon JFG, Hutcheon MA: Tumor associated peripheral eosinophilia: Two unusual cases. J Clin Oncol 1984., 2:
Hillerdal G: Malignant mesothelioma 1982: review of 4710 published cases. Br J Dis Chest 1983, 77(321-343):1165-1169.
Kiyoshi K, Tadaro T, Tomoyuki T, Tadao F, Chieki W, Toru K: An Autopsy Case of Malignant Pleural Mesothelioma with eosinophilia and Gastric Wall Metastasis. Japanese Journal of Lung Cancer 28(4):521-528.
Thomas AS: Tumor Associated Blood Eosinophilia and Eosinophilic Pleural Effusion: Case Report and Review of the Literature. The Internet Journal of Pulmonary Medicine 1997, 1: 1.
Davis BH: Hypereosinophilia associated with a peritoneal mesothelioma. Arch Pathol Lab Med 1979, 103: 487.
Isaacson NH, Rapoport P: Eosinophilia in malignant tumors: its significance. Ann Intern Med 1945, 25: 893-902.
Brick IB, Glazer LG: Marked eosinophilia with cancer: a poor prognostic sign. Ann Intern Med 1951, 35: 213-218.
Matsumoto S, Tamai T, Yanagisawa K, Kawamura S, Fujita S: Lung cancer with eosinophilia in the peripheral blood and the pleural fluid. Intern Med 1992, 31: 525-529. 10.2169/internalmedicine.31.525
Toshio N, Tsuneo N, Atsuo K, Koichi A, Rie K, Yukio T: Granulocyte-Macrophage Colony-Stimulating Factor and Granulocyte Colony-Stimulating Factor-Producing Malignant Pleural Mesothelioma Accompanied by Eosinophilic Pleural Fluid. Lung Cancer 2004, 44: 25-30.
Lopes C, Sotto-Mayor R, Teixeira E, Almeida A: Malignant mesothelioma: A ten years experience. Rev Port Pneumol 2005, 11(6 Suppl 1):16-18.
Vertun-Baranowska B, Fijałkowska A, Tomkowski W, Filipecki S, Szymañska D: Pulmonary embolism in malignancy of the lung: a retrospective clinical evaluation and pathomorphologic personal material. Pneumonol Alergol Pol 1996, 64: 392-402.
Martin AA, Sitton JE, Daroca PJ Jr, Moulder PV, Shepard DL: Superior vena cava syndrome associated with malignant mesothelioma. J La State Med Soc 1991, 143: 33-35.
Marcy PY, Magné N, Bentolila F, Drouillard J, Bruneton JN, Descamps B: Superior vena cava obstruction: is stenting necessary? Support Care Cancer 2001, 9: 103-107. 10.1007/s005200000173
Schattner A, Kozack N: A 47-year old man with mesothelioma and neck swelling. CMAJ 2004., 170(4):
Isildak M, Guven GS, Emri S: Mesothelioma and venous thrombosis. CMAJ 2004, 171: 11.
Molina Boix M, Ortega González G, Abel Cortés JL, Bermudo Ruiz J, Pedro de Lelis F, Paricio Núñez P: Malignant pleural mesothelioma with disseminated thrombi and myocardial metastases. Rev Clin Esp 1985, 176: 248-250.
Matsui H, Nishinaka K, Oda M, Kubori T, Udaka F: Trousseau syndrome due to pleural mesothelioma. Neurologist 2007, 13: 205-208. 10.1097/01.nrl.0000253113.53846.ec
Farmer CKT, Goldsmith DJA: Nephrotic syndrome and mesenteric infarction secondary to metastatic mesothelioma. Postgrad Med J 2001, 77: 333-334. 10.1136/pmj.77.907.333
Nakano T, Chahinian AP, Shinjo M, Tonomura A, Miyake M, Togawa N, Ninomiya K, Higashino K: Interleukin 6 and its relationship to clinical parameters in patients with malignant pleural mesothelioma. Br J Cancer 1998, 77: 907-912.
Liu L, Wang Z, Zhang X, Bu H, Qin Z: Pleural malignant mesothelioma complicated with disseminated intravascular coagulation. Hua Xi Yi Ke Da Xue Xue Bao 1993, 24: 426-428.
Spry CJF, Davies J, Tay PC, Olsen EGJ, Oakley CM, Goodwin JF: Clinical features of 15 patients with hypereosinophilic syndrome. Q J Med 1983, 52: 1-22.
Moosbauer C, Morgenstern E, Cuvelier SL, Manukyan D, Bidzhekov K, Albrecht S, Lohse P, Patel KD, Engelmann B: Eosinophils are a major intravascular location for tissue factor storage and exposure. Blood 2007, 109: 995-1002. 10.1182/blood-2006-02-004945
Slungaard A, Vercellotti GM, Tran T, Gleich GJ, Key NS: Eosinophil cationic granule proteins impair thrombomodulin function. A potential mechanism for thromboembolism in hypereosinophilic heart disease. J Clin Invest 1993, 91: 1721-1730. 10.1172/JCI116382
Fredens K, Dahl R, Venge P: In vitro studies of the interaction between heparin and eosinophil cationic protein. Allergy 1991, 46: 27-29. 10.1111/j.1398-9995.1991.tb00538.x
Santoro A, Ferrari G, Zucchelli P: Sensitivity to heparin anticoagulant response in eosinophilic patients. Kidney Int Suppl 1988, 24: S84-5.
Samsoon G, Wood ME, Knight-George AB, Britt RP: General anaesthesia and the hypereosinophilic syndrome: severe postoperative complications in two patients. Br J Anaesth 1992, 69: 653-656. 10.1093/bja/69.6.653
Lyman GH, Khorana AA, Falanga A, Clarke-Pearson D, Flowers C, Jahanzeb M, Kakkar A, Kuderer NM, Levine MN, Liebman H, Mendelson D, Raskob G, Somerfield MR, Thodiyil P, Trent D, Francis CW: American Society of Clinical Oncology. American Society of Clinical Oncology guideline: recommendations for venous thromboembolism prophylaxis and treatment in patients with cancer. J Clin Oncol 2007, 25: 5490-5505. 10.1200/JCO.2007.14.1283
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Ames, P.R.J., Aye, W.W. Pleural mesothelioma and venous thrombosis: the eosinophilia link. Thrombosis J 6, 3 (2008). https://doi.org/10.1186/1477-9560-6-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1477-9560-6-3