Abstract
Background
Male breast cancer is a rare but aggressive and devastating disease. This disease presents at a later stage and in a more advanced fashion than its female counterpart. The immunophenotype also appears to be distinct when compared to female breast cancer. Angiogenesis plays a permissive role in the development of a solid tumor and provides an avenue for nutrient exchange and waste removal. Recent scrutiny of angiogenesis in female breast cancer has shown it to be of significant prognostic value. It was hypothesized that this holds true in invasive ductal carcinoma of the male breast. In the context of male breast cancer, we investigated the relationship of survival and other clinico-pathological variables to the microvascular density of the tumor tissue.
Methods
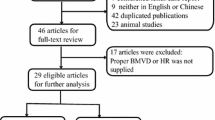
Seventy-five cases of primary male breast cancer were identified using the records of the Saskatchewan Cancer Agency over a period of 26 years. Forty-seven cases of invasive ductal carcinoma of the male breast had formalin-fixed paraffin-embedded tissue blocks that were suitable for this study. All cases were reviewed. Immunohistochemical staining was performed for the angiogenic markers (cluster designations 31 (CD31), 34 (CD34) and 105 (CD105), von Willebrand factor (VWF), and vascular endothelial growth factor (VEGF)). Microvascular density (MVD) was determined using average, centre, and highest microvessel counts (AMC, CMC, and HMC, respectively). Statistical analyses compared differences in the distribution of survival times and times to relapse between levels of MVD, tumor size, node status and age at diagnosis. In addition, MVD values were compared within each marker, between each marker, and were also compared to clinico-pathological data.
Results
Advanced age and tumor size were related to shorter survival times. There were no statistically significant differences in distributions of survival times and times to relapse between levels of MVD variables. There was no significant difference in MVD between levels of the different clinico-pathological variables. MVD was strongly and significantly correlated between AMC, CMC and HMC for CD31, CD34, and CD105 (p < 0.01) and remained moderate to weak for VWF and VEGF.
Conclusion
Microvascular density does not appear to be an independent prognostic factor in male breast cancer. However, the likelihood of death for men with breast cancer is increased in the presence of increased age at diagnosis and advanced tumor size. This is perhaps linked to inherent tumor vasculature, which is strongly related throughout a tumor section.
Similar content being viewed by others
Background
Invasive ductal carcinoma of the male breast comprises approximately 1% of all breast cancers. Invasive ductal carcinoma of the male breast is distinct from invasive ductal carcinoma of the female breast in both presentation and immunophenotype. Male breast cancer generally presents in older patients and at a more advanced stage than its female counterpart [1–3]. In contrast to female breast cancers, ductal carcinoma in situ is quite rare in men [4, 5]. Male breast cancers are also predominantly of the invasive ductal adenocarcinoma, not otherwise specified (NOS) type. Invasive ductal carcinoma of the male breast, despite being a high-grade tumor is more likely to express estrogen receptor and/or progesterone receptor and is less likely to over-express P53 or Erb-B2 when compared to invasive ductal carcinoma in the female breast [6, 7]. The combination of a unique male hormonal environment, in addition to the unique immunophenotype, points to a distinct, non-p53-dependant, pathway of tumor progression in the male. Yet, despite these differences, it appears that the overall prognosis for male and female breast invasive ductal carcinomas are similar in age and stage-matched studies [1, 8–10].
Angiogenesis is the growth and proliferation of blood vessels from existing vasculature. This process is quiescent in normal tissues and becomes active in rapidly growing tissues – including solid tumors. It has been shown that, in order to overcome tissue death by hypoxia, tumor growth beyond 1–2 mm3 is dependant upon the formation of new vasculature [11]. Angiogenesis is, thus, an established step in solid tumor progression. This has been studied in many cancers including colorectal cancer [12] non-small cell lung cancer [13, 14], hepatocelullar cancer [15], melanoma [16] prostate cancer [17], breast cancer [18–24] and bladder carcinoma [25].
Most assessments of angiogenesis in female breast carcinoma have shown it to be of significant prognostic value [18–22]. However, not all studies in this field have observed such important clinical correlations to MVD [23, 24]. There are a variety of techniques used to evaluate angiogenesis and the variability between studies is probably related to the varying techniques employed in this process.
Invasive ductal carcinoma of the male breast appears to be a unique and biologically different carcinoma [1]; it is not simply the appearance of female invasive ductal carcinoma in a male breast. Due to the rarity of the disease large cohorts are not readily available, and there is only a limited pool of published data exploring various facets of this important disease. In one study of 26 men with breast cancer, elevated MVD was associated with advanced stage of disease and poor outcome [26]. Another Japanese study confirms that angiogenesis is part of tumor progression in male breast cancer [27].
In an attempt to further characterize this rare tumor, the aim of the current study was to evaluate angiogenesis in invasive ductal carcinoma of the male breast by the assessment of microvascular density in tumor samples. Specifically, we investigated three questions: (1) do survival times and times to relapse differ between levels of MVD, demographic, and clinico-pathological variables; (2) do MVD measures differ between levels of demographic and clinico-pathological variables, and finally; (3) are different measures of MVD correlated within a section of tumor tissue? This study is an extension of our established work on immunophenotypic characterization of male breast carcinoma in Saskatchewan [6].
Patients and methods
Patients
After obtaining appropriate ethics approval from the University of Saskatchewan Advisory Committee on Human Experimentation, all cases (n = 75) of invasive ductal male breast cancer diagnosed between 1975 and 1997 were selected from the records of the Saskatchewan Cancer Agency. Detailed chart review was performed for cases where paraffin-embedded tissue samples were available (n = 59). After the removal of all cases with inadequate tissue sample, tissue staining and chart data, there remained 47 cases.
Clinical and pathological studies
Sections were cut from paraffin-embedded tissue samples. The sections were stained with hematoxylin and eosin (H & E). A detailed histopathological assessment was performed. Clinical features were recorded including age at diagnosis, date of birth, node status, tumor size, treatment method, date of relapse, and date of death.
Age at diagnosis, tumor size, node status, disease-free survival and overall survival were the clinical variables of interest in this study. Age at diagnosis was determined from the patient chart. Tumor size and node status were determined from the pathology report. Overall survival (number of years patient survived since the diagnosis of invasive breast carcinoma) and disease-free survival (number of consecutive years the patient was alive without breast cancer or other cancer relapse related to the breast carcinoma since the date of diagnosis) were calculated from the information gathered in the chart review. In cases where multiple tissue blocks were available, all H & E sections were examined in order to select a representative tissue block with a large area of invasive tumor and satisfactory tissue integrity.
Microvessel density determination
MVD determination was modeled after the method described by Kato et al., [18] and Weidner et al., [28]. Immunohistochemical staining was performed for CD31, CD34, CD105, VWF and VEGF. Staining was carried out on a representative section by the avidin-biotin-peroxidase (ABC) technique after antigen retrieval using appropriate positive and negative controls in all cases. The source and dilution for each antibody are presented in table 1.
Brown-staining areas, whether single endothelial cells or clusters of endothelial cells, regardless of the absence/presence of a lumen were counted as individual microvessels. Vessels that had a thick muscular layer were excluded from the count. Cases were evaluated in a random order. Two observers using a double-headed light microscope simultaneously performed all counts for CD31, CD34, VWF and VEGF. A single experienced observer assessed CD105. Observers were blinded to all clinical and pathological data. Average, central and highest microvessel counts (AMC, CMC, and HMC, respectively) were performed.
Ten high power (200×) fields along the border between cancer nests and the stroma were evaluated for each section (figure 1). The average number of microvessels per high power field was determined and reported as AMC.
After scanning at low power (40×), the central area of the tumor was estimated. From this area, six high power (200×) fields were evaluated for each section (figure 2). The average number of microvessels per high power field was determined and reported as CMC. For tumors with a central necrotic area, determination was completed using areas near the centre of the tumor that were viable (non-necrotic).
After scanning at low power (40×), three areas with the highest concentration of microvessels (vascular hot spots) were selected. Each area was evaluated with one high power (200×) field in such a way as to include the maximum number of microvessels (figure 3). The highest value obtained among the three fields was reported as HMC.
Highest microvessel count – VEGF. After scanning at low power (40×), three areas with the highest concentration of microvessels (vascular hot spots) were selected. Each area was evaluated with one high power (200×) field in such a way as to include the maximum number of microvessels. The highest value obtained among the three fields was reported as HMC.
Statistical analysis
Analysis was completed using the Statistical Package for the Social Sciences (SPSS) version 11.0 on an IBM PC 300PL computer. All tests were two tailed with the level of statistical significance set at p < 0.05. The demographic and clinico-pathological variables of interest included age at diagnosis (<65 and ≥ 65 years), tumor size (T1 is ≤ 2 cm, T2 is >2 cm but ≤ 5 cm, and T3 is >5 cm) and node status (positive and negative).
To compare the distribution of survival times and disease free survival times (time to relapse) we produced Kaplan-Meier curves and made statistical comparisons using the log-rank test between levels of demographic and clinico-pathological variables. In addition to this we dichotomized the MVD variables based on the median and repeated the Kaplan Meier with log-rank analysis to compare survival times and times to relapse between levels of MVD. For comparison of survival times, the outcome of interest was death while the remaining subjects (those surviving to the end of the study period) were censored. For comparison of time to relapse, the outcome of interest was relapse while the remaining subjects (those surviving to the end of the study or those who died before relapse) were censored.
Levels of MVD were also compared with levels of demographic and clinico-pathological variables using the Mann Whitney test or Kruskal Wallis test when MVD was considered as a continuous variable and chi squared or Fisher's Exact test when MVD was considered as dichotomous variable.
Finally, for each vascular marker (CD31, CD34, CD 105, VWF, and VEGF), correlation between the different measures of MVD (i.e. AMC with CMC, AMC with HMC, and CMC with HMC) was assessed using the Spearman's correlation coefficient. Correlations with a coefficient (ρ) of ≥ 0.80 were considered strong, moderate-strong correlations had coefficients that were <0.80 but ≥ 0.50, moderate-weak correlations had coefficients that were <0.50 but ≥ 0.30, weak correlations had coefficients that were <0.30.
Results
Age at diagnosis and clinicopathological characteristics
In this study of 47 cases of male breast cancer, the median age of diagnosis was 65.9 years with the youngest being 32 years and the oldest being 94 years. The frequency of male breast cancer cases by age is illustrated in figure 4. As seen in Table 2, most of the patients had a tumor size of T1 to T2 and were node status negative.
Treatment regimens
All patients underwent some form of surgical resection – most frequently a modified radical mastectomy. In 31 out of 47 cases, surgical resection was followed by some form of adjuvant therapy (radiotherapy, chemotherapy, hormonal therapy (tamoxifen), or some combination of the aforementioned). Specifically, 6 patients received only radiotherapy, 7 patients received only hormonal therapy and 2 patients received only chemotherapy. For combined therapies, 6 patients received radiotherapy with hormonal therapy, 3 patients received radiotherapy with chemotherapy, 4 patients received hormonal therapy with chemotherapy and 3 patients received all three methods of adjuvant therapy.
Patient outcome
All cases reviewed in this study came from the records of the Saskatchewan Cancer Agency between 1975 and 1997. Thirty-three of 47 patients (70%) died in the time period considered. Of the remaining 14 patients (30%), 9 (64%) had been followed for 10 years or more and 5 (36%) patients had been followed for under 10 years. Seventeen patients (36%) had documented relapse. The average age at death for patients with relapse was 72 years while the average age at death for relapse-free patients was 78 years. Although 70% of patients did die in this study, thirty-two patients (68%) survived at least 5-years after the diagnosis of breast cancer.
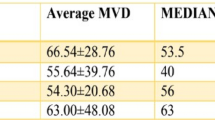
The Kaplan-Meier curves relating prognostic variables to death and relapse are illustrated in figure 5. There were significantly shorter survival times when the age of diagnosis was ≥ 65 years (p < 0.001) and when tumor size was larger (p < 0.01). However, there were no significant differences in the times to relapse by any of the clinical variables. In addition to this, there were no significant differences in survival times or times to relapse for any of the MVD markers when categorized by the median score (Table 3).
Microvascular density and clinical variables
Regardless of whether MVD was considered as a continuous variable or as a categorical variable, there were no significant differences in MVD by demographic (age group) or clinico-pathological features (tumour size or node status) although some of the differences may be clinically important. Table 4 provides median values of MVD markers at different levels of clinico-pathological variables.
Microvascular density within individual markers
Measures of MVD (AMC, CMC and HMC) were compared within each marker. These correlations are illustrated in figure 6.
CD31
Significant correlations (p < 0.01) were observed between all methods of measure (AMC correlates with CMC, CMC correlates with HMC, and HMC correlates with AMC) for CD31. The correlations between AMC and CMC, and AMC and HMC were moderate-strong (ρ = 0.76 and ρ = 0.60 respectively); the correlation between CMC and HMC was strong (ρ = 0.88).
CD34
Significant correlations (p < 0.01) were observed between all methods of measure (AMC correlates with CMC, CMC correlates with HMC, and HMC correlates with AMC) for CD34. All correlations were moderately-weak or moderate-strong (ρ = 0.45 for AMC and CMC, ρ = 0.41 for AMC and HMC, and ρ = 0.77 for CMC and HMC).
CD105
Significant correlations (p < 0.01) were observed between all methods of measure (AMC correlates with CMC, CMC correlates with HMC, and HMC correlates with AMC) for CD105. The correlations between AMC and CMC, and AMC and HMC were moderate-strong and moderate-weak (ρ = 0.62 and ρ = 0.49 respectively); the correlation between CMC and HMC was strong (ρ = 0.82).
VWF
A significant correlation (p < 0.01) was observed between CMC and HMC for VWF. A trend correlation (p < 0.10) was observed between AMC and HMC. Correlations were moderate-weak and weak (ρ = 0.47 and ρ = 0.25 respectively). There was no significant relationship between AMC and CMC for this marker.
VEGF
Significant correlations (p < 0.01) were observed between AMC and CMC, and between CMC and HMC for VEGF. Correlations were moderate-weak and moderate-strong (ρ = 0.43 and ρ = 0.68 respectively). There was no significant relationship between AMC and HMC for this marker.
Discussion
The markers
VEGF also called vascular permeability factor (VPF) is an important angiogenic activator, for both physiological and pathological angiogenesis [29, 30], and it may be associated with inflammation. VEGF plays an essential role in embryonic vasculogenesis and angiogenesis [31, 32]. It has also been implicated in postnatal development of the glomerulus [33, 34] and endochondral bone [35, 36].
VEGF mRNA has been shown to be up-regulated in the majority of human tumors investigated [37], and carcinoma of the human breast is one of these. [38, 39]. In addition, VEGF has been implicated in psoriasis [40], brain edema [41], polycystic ovary syndrome [29], age-related macular degeneration (AMD) and other intraocular neovascular syndromes [42–44] The expression of VEGF is triggered by hypoxia. That is to say, low oxygen tension provokes VEGF mRNA expression [45].
An excellent review of CD105 and its involvement in angiogenesis has been written by Duff et al., [46]. CD105 (endoglin) is commonly expressed by angiogenic endothelial cells [46–48]. CD105 is an important pro-angiogenic factor. Transforming growth factor β exerts an inhibitory influence on cell proliferation, migration and microvessel formation. The suppressive effect of CD105 on transforming growth factor β, thus, contributes to angiogenesis [49]. It is, therefore, no surprise to observe elevated CD105 expression in various tumor endothelia [50–52], including breast cancer [53]. CD105 may be shed into the blood stream. The measure of serum endoglin appears to provide important prognostic information in cancer patients [54, 55].
CD31 is an important part of the endothelial intercellular junction [56] and it plays a crucial role in leukocyte migration through vascular endothelial intracellular junctions [57–59]. This molecule is at least partially responsible for the adhesion between leucocytes/endothelial cells, leucocytes/platelets, and endothelial cells/endothelial cells [57, 60–65]. This adhesion is likely the result of CD31-CD31 [66] interactions (homophilic interactions) although adhesion between CD31 and other components of the cell membrane has been demonstrated (heterophilic interactions) [61, 67–70].
CD31 also exhibits signal transduction; its dimerization appears to upregulate integrin function [71]. This molecule appears to be involved in thrombosis, angiogenesis, wound healing, and inflammation [61]. CD31 is known to be a co-signal transducer for macrophages, inducing respiratory burst.
CD34 is a glycosylated type I transmembrane protein [72] which is expressed on hematopoietic stem cells, committed hematological progenitor cells [73–75], small vessel endothelial cells [76, 77], tumors of epithelial origin [78, 79] and a limited number of other cell populations including some haematological malignancies [72].
As specific ligands are still undefined, the precise role CD34 plays in early hematopoiesis remains uncertain. It is thought that differential splicing of sugar residues on CD34 may permit it to host a variety of ligands under different conditions [80]. Despite our meager understanding of this complex molecule there is evidence indicating that hematopoietic CD34 plays a role in modulating adhesion (this has been reviewed previously [72]).
Factor VIII related antigen, or von Willebrand factor (VWF), is a plasma protein produced by endothelial cells [81, 82]. VWF is also present in platelets, as it is produced by their megakaryocytic precursor [83].
VWF is a multifunctional protein. It is known to mediate adhesion/aggregation of platelets in clot formation (reviewed in [84]). In addition to this, VWF acts as a chaperone for circulating factor VIII. About 1 – 2% of VWF is bound by factor VIII [85]. This non-covalent bond prolongs the survival of factor VIII in the plasma. When the coagulation cascade is triggered, thrombin cleaves the complex, thereby freeing factor VIII to participate coagulation [86] (reviewed in [87]).
Age at diagnosis
Male breast cancer is a disease of older men. The likelihood of this occurring in older men that is illustrated in this study is not surprising as this is the case for most studies of e breast cancer in males [88, 89]. As mortality from common conditions (e.g. cardiovascular disease) within this group improves due to advances in treatment/intervention and a larger proportion of the population enters this age group, it seems that the relative incidence of male breast cancer is likely to rise. Such is the finding in a recent meta-analysis of male breast carcinoma [1].
Survival
In this study, 70% of the reviewed patients died. Though this number may seem high, only half of those who died had documented relapse prior to the time of death. There is, however, an interesting difference between average age at death for relapsed and relapse-free patients, 72 years versus 78 years respectively. It appears that male breast cancer is contributing to mortality, but this study did not examine the effects of co-morbid conditions. The expected life remaining for a 65 year old male in Saskatchewan between 1995 and 1997 was 16.7 years (expected age approximately 82 years) [90].
Increased tumor size increases the likelihood of death for male breast cancer patients in this study (figure 5). One possible explanation for this relationship is as follows: a tumor's size may be a function of its rate of growth and time of growth; these characteristics seem likely to increase the opportunity for relapse and metastasis. Thus, we might expect large tumors to relapse more frequently than small ones, and therefore, also contribute to death.
It appears that younger patients had a significantly better chance of not experiencing death (figures 5). This phenomenon is possibly related to improved response to treatment in younger patients; alternatively, this relationship may be demonstrating that younger patients are diagnosed with less advanced disease and vice versa. Evidence supports advanced age [88, 89] and tumor size [91] as important negative prognostic factors.
This study was not able to clearly demonstrate statistically significant differences in survival for node status. In the available literature axillary node status is an important prognostic factor [91–94].
Microvascular density, though it was the primary focus of this study, did not demonstrate statistically significant association with survival, demographic or clinico-pathological features. However, we cannot discount the importance of angiogenesis in tumor progression. The lack of correlation in this study may have been influenced by the lack of statistical power, the methods used, the age of the tissue, advanced stage of disease at presentation and method of analysis.
In most tumors studied, MVD has been identified as a prognostic factor and has had important correlations to clinical variables [12–16]. In most studies where angiogenesis has been evaluated in cancer of the female breast, MVD is an important prognostic factor [19–22]. In one study of male breast cancer using CD34 to highlight vessels, it was concluded that MVD was an important prognostic tool [26].
In an angiogenesis methodology study of 109 women with breast cancer by Kato et al., [18] it was found that CMC and HMC did not correlate to clinico-pathological variables other than peritumor vascular invasion. AMC was found to have prognostic value. The methods used to report microvessel density were modeled after this work by Kato et al, [18].
Despite a lack of strong evidence, in our study, to support angiogenesis as an independent prognostic factor, there is no evidence to disprove angiogenesis plays a critical role in tumor development. As angiogenesis remains a likely step in tumor progression, we must continue to recognize this process as a potential target for anti-tumor therapy.
Microvascular density within each marker
There were some important correlations between the different methods of measure for MVD (AMC, CMC and HMC) within the various markers. CD31, CD34 and CD105 were the strongest in this regard with correlations that were very significant (p < 0.01) and correlations that were usually moderate to strong. The correlations within VWF and VEGF were not all significant, and the relationship was moderate to weak.
It could also be that VWF and VEGF are differentially expressed in male breast cancer tissue. This seems to be the case for VEGF. In fact, it was observed that VEGF had a propensity to be over-expressed in regions where there were invading lymphocytes. This may produce a patchy pattern of expression, which could have an important effect on microvessel counts.
For the most part, this study saw strong correlations between the various microvessel count methods within the markers. Critics may suggest that evaluation of microvascular density for prognosis in tumors is flawed because, within a tumor, microvascular density is heterogeneous [24, 95]. However, the correlations observed in this study support the notion that tumor vasculature is predictable (but not ubiquitous or necessarily homogeneous) from the centre, periphery and vascular hotspot of a tumor. Notably, similar research in female invasive ductal carcinoma of the breast using VWF MVD assessment techniques also demonstrated correlation between central, peripheral and highest microvessel densities [18].
Microvessel determination, by the methods used in this study, is dependant on a predictable pattern of vasculature within a tumor. Such predictability allows for practical (in terms of time, money and ease of use) application of important clinical prognostic features of the markers. Further research to examine the relationship between these markers in cancer is wanting. Such information may prove important in improving the prognostic value of MVD determination.
Conclusion
From this evaluation of angiogenesis in male breast cancer, we can draw the following conclusions:
Microvascular density does not appear to be an independent prognostic factor in male breast cancer. Tumor vasculature (as measured by microvessel determination using antibodies to endothelial markers such as CD31, CD34, CD105) is strongly related throughout a tumor section (p < 0.01). Other endothelial markers such as VWF and VEGF appear to have a moderate to weak relationship. Advanced age at diagnosis and increased tumor size increases the likelihood of death for men with breast cancer.
Abbreviations
- AMC:
-
Average microvessel count
- CD#:
-
Cluster designation or cluster of differentiation (CD31, CD34, CD105)
- CMC:
-
Central microvessel count
- HMC:
-
Highest microvessel count
- MVD:
-
Microvessel density
- TNM:
-
Tumour nodes metastasis
- VEGF:
-
Vascular endothelial growth factor
- VWF:
-
Von Willebrand factor
References
Giordano SH, Cohen DS, Buzdar AU, Perkins G, Hortobagyi GN: Breast carcinoma in men: a population-based study. Cancer. 2004, 101: 51-57. 10.1002/cncr.20312.
Donegan WL, Redlich PN, Lang PJ, Gall MT: Carcinoma of the breast in males: a multiinstitutional survey. Cancer. 1998, 83: 498-509. 10.1002/(SICI)1097-0142(19980801)83:3<498::AID-CNCR19>3.0.CO;2-R.
Gough DB, Donohue JH, Evans MM, Pernicone PJ, Wold LE, Naessens JM, O'Brien PC: A 50-year experience of male breast cancer: is outcome changing?. Surg Oncol. 1993, 2: 325-333. 10.1016/0960-7404(93)90063-5.
Hittmair AP, Lininger RA, Tavassoli FA: Ductal carcinoma in situ (DCIS) in the male breast: a morphologic study of 84 cases of pure DCIS and 30 cases of DCIS associated with invasive carcinoma--a preliminary report. Cancer. 1998, 83: 2139-2149. 10.1002/(SICI)1097-0142(19981115)83:10<2139::AID-CNCR12>3.0.CO;2-F.
Camus MG, Joshi MG, Mackarem G, Lee AK, Rossi RL, Munson JL, Buyske J, Barbarisi LJ, Sanders LE, Hughes KS: Ductal carcinoma in situ of the male breast. Cancer. 1994, 74: 1289-1293.
Muir D, Kanthan R, Kanthan SC: Male versus female breast cancers. A population-based comparative immunohistochemical analysis. Arch Pathol Lab Med. 2003, 127: 36-41.
Weber-Chappuis K, Bieri-Burger S, Hurlimann J: Comparison of prognostic markers detected by immunohistochemistry in male and female breast carcinomas. Eur J Cancer. 1996, 32A: 1686-1692. 10.1016/0959-8049(96)00154-2.
Borgen PI, Senie RT, McKinnon WM, Rosen PP: Carcinoma of the male breast: analysis of prognosis compared with matched female patients. Ann Surg Oncol. 1997, 4: 385-388.
Cutuli B, Lacroze M, Dilhuydy JM, Velten M, De Lafontan B, Marchal C, Resbeut M, Graic Y, Campana F, Moncho-Bernier V: Male breast cancer: results of the treatments and prognostic factors in 397 cases. Eur J Cancer. 1995, 31A: 1960-1964. 10.1016/0959-8049(95)00366-5.
Joshi MG, Lee AK, Loda M, Camus MG, Pedersen C, Heatley GJ, Hughes KS: Male breast carcinoma: an evaluation of prognostic factors contributing to a poorer outcome. Cancer. 1996, 77: 490-498.
Folkman J: Clinical application of research on angiogenesis. N Engl J Med. 1995, 333: 1757-1763. 10.1056/NEJM199512283332608.
Galindo-Gallego M, Fernandez-Acenero MJ, Sanz-Ortega J, Aljama A, Lopez-Elzaurdia C: Prognostic significance of microvascular counts in rectal carcinoma. Pathol Res Pract. 2000, 196: 607-612.
Shijubo N, Kojima H, Nagata M, Ohchi T, Suzuki A, Abe S, Sato N: Tumor angiogenesis of non-small cell lung cancer. Microsc Res Tech. 2003, 60: 186-198. 10.1002/jemt.10257.
Macchiarini P, Fontanini G, Hardin MJ, Squartini F, Angeletti CA: Relation of neovascularisation to metastasis of non-small-cell lung cancer. Lancet. 1992, 340: 145-146. 10.1016/0140-6736(92)93217-B.
Qin LX, Tang ZY: The prognostic molecular markers in hepatocellular carcinoma. World J Gastroenterol. 2002, 8: 385-392.
Zettersten E, Shaikh L, Ramirez R, Kashani-Sabet M: Prognostic factors in primary cutaneous melanoma. Surg Clin North Am. 2003, 83: 61-75.
Bono AV, Celato N, Cova V, Salvadore M, Chinetti S, Novario R: Microvessel density in prostate carcinoma. Prostate Cancer Prostatic Dis. 2002, 5: 123-127. 10.1038/sj.pcan.4500572.
Kato T, Kimura T, Ishii N, Fujii A, Yamamoto K, Kameoka S, Nishikawa T, Kasajima T: The methodology of quantitation of microvessel density and prognostic value of neovascularization associated with long-term survival in Japanese patients with breast cancer. Breast Cancer Res Treat. 1999, 53: 19-31. 10.1023/A:1006193024382.
Weidner N, Semple JP, Welch WR, Folkman J: Tumor angiogenesis and metastasis--correlation in invasive breast carcinoma. N Engl J Med. 1991, 324: 1-8.
Leek RD: The prognostic role of angiogenesis in breast cancer. Anticancer Res. 2001, 21: 4325-4331.
Saaristo A, Karpanen T, Alitalo K: Mechanisms of angiogenesis and their use in the inhibition of tumor growth and metastasis. Oncogene. 2000, 19: 6122-6129. 10.1038/sj.onc.1203969.
Gasparini G: Clinical significance of determination of surrogate markers of angiogenesis in breast cancer. Crit Rev Oncol Hematol. 2001, 37: 97-114.
Goulding H, Abdul Rashid NF, Robertson JF, Bell JA, Elston CW, Blamey RW, Ellis IO: Assessment of angiogenesis in breast carcinoma: an important factor in prognosis?. Hum Pathol. 1995, 26: 1196-1200. 10.1016/0046-8177(95)90193-0.
Van Hoef ME, Knox WF, Dhesi SS, Howell A, Schor AM: Assessment of tumour vascularity as a prognostic factor in lymph node negative invasive breast cancer. Eur J Cancer. 1993, 29A: 1141-1145.
Offersen BV, Knap MM, Marcussen N, Horsman MR, Hamilton-Dutoit S, Overgaard J: Intense inflammation in bladder carcinoma is associated with angiogenesis and indicates good prognosis. Br J Cancer. 2002, 87: 1422-1430. 10.1038/sj.bjc.6600615.
Shpitz B, Bomstein Y, Sternberg A, Klein E, Liverant S, Groisman G, Bernheim J: Angiogenesis, p53, and c-erbB-2 immunoreactivity and clinicopathological features in male breast cancer. J Surg Oncol. 2000, 75: 252-257.
Kuroi K, Toi M: [Male breast cancer]. Gan To Kagaku Ryoho. 2003, 30: 599-605.
Weidner N, Folkman J, Pozza F, Bevilacqua P, Allred EN, Moore DH, Meli S, Gasparini G: Tumor angiogenesis: a new significant and independent prognostic indicator in early-stage breast carcinoma. J Natl Cancer Inst. 1992, 84: 1875-1887.
Ferrara N, Gerber HP, LeCouter J: The biology of VEGF and its receptors. Nat Med. 2003, 9: 669-676. 10.1038/nm0603-669.
Bates DO, Harper SJ: Regulation of vascular permeability by vascular endothelial growth factors. Vascul Pharmacol. 2002, 39: 225-237. 10.1016/S1537-1891(03)00011-9.
Ferrara N, Carver-Moore K, Chen H, Dowd M, Lu L, O'Shea KS, Powell-Braxton L, Hillan KJ, Moore MW: Heterozygous embryonic lethality induced by targeted inactivation of the VEGF gene. Nature. 1996, 380: 439-442. 10.1038/380439a0.
Carmeliet P, Ferreira V, Breier G, Pollefeyt S, Kieckens L, Gertsenstein M, Fahrig M, Vandenhoeck A, Harpal K, Eberhardt C, Declercq C, Pawling J, Moons L, Collen D, Risau W, Nagy A: Abnormal blood vessel development and lethality in embryos lacking a single VEGF allele. Nature. 1996, 380: 435-439. 10.1038/380435a0.
Kitamoto Y, Tokunaga H, Tomita K: Vascular endothelial growth factor is an essential molecule for mouse kidney development: glomerulogenesis and nephrogenesis. J Clin Invest. 1997, 99: 2351-2357.
Eremina V, Sood M, Haigh J, Nagy A, Lajoie G, Ferrara N, Gerber HP, Kikkawa Y, Miner JH, Quaggin SE: Glomerular-specific alterations of VEGF-A expression lead to distinct congenital and acquired renal diseases. J Clin Invest. 2003, 111: 707-716. 10.1172/JCI200317423.
Ryan AM, Eppler DB, Hagler KE, Bruner RH, Thomford PJ, Hall RL, Shopp GM, O'Neill CA: Preclinical safety evaluation of rhuMAbVEGF, an antiangiogenic humanized monoclonal antibody. Toxicol Pathol. 1999, 27: 78-86.
Gerber HP, Vu TH, Ryan AM, Kowalski J, Werb Z, Ferrara N: VEGF couples hypertrophic cartilage remodeling, ossification and angiogenesis during endochondral bone formation. Nat Med. 1999, 5: 623-628. 10.1038/9467.
Ferrara N, Davis-Smyth T: The biology of vascular endothelial growth factor. Endocr Rev. 1997, 18: 4-25. 10.1210/er.18.1.4.
Brown LF, Berse B, Jackman RW, Tognazzi K, Guidi AJ, Dvorak HF, Senger DR, Connolly JL, Schnitt SJ: Expression of vascular permeability factor (vascular endothelial growth factor) and its receptors in breast cancer. Hum Pathol. 1995, 26: 86-91. 10.1016/0046-8177(95)90119-1.
Yoshiji H, Gomez DE, Shibuya M, Thorgeirsson UP: Expression of vascular endothelial growth factor, its receptor, and other angiogenic factors in human breast cancer. Cancer Res. 1996, 56: 2013-2016.
Detmar M, Yeo KT, Nagy JA, Van de Water L, Brown LF, Berse B, Elicker BM, Ledbetter S, Dvorak HF: Keratinocyte-derived vascular permeability factor (vascular endothelial growth factor) is a potent mitogen for dermal microvascular endothelial cells. J Invest Dermatol. 1995, 105: 44-50. 10.1111/1523-1747.ep12312542.
Kovacs Z, Ikezaki K, Samoto K, Inamura T, Fukui M: VEGF and flt. Expression time kinetics in rat brain infarct. Stroke. 1996, 27: 1865-72; discussion 1872-3.
Aiello LP, Pierce EA, Foley ED, Takagi H, Chen H, Riddle L, Ferrara N, King GL, Smith LE: Suppression of retinal neovascularization in vivo by inhibition of vascular endothelial growth factor (VEGF) using soluble VEGF-receptor chimeric proteins. Proc Natl Acad Sci U S A. 1995, 92: 10457-10461.
Malecaze F, Clamens S, Simorre-Pinatel V, Mathis A, Chollet P, Favard C, Bayard F, Plouet J: Detection of vascular endothelial growth factor messenger RNA and vascular endothelial growth factor-like activity in proliferative diabetic retinopathy. Arch Ophthalmol. 1994, 112: 1476-1482.
Lopez PF, Sippy BD, Lambert HM, Thach AB, Hinton DR: Transdifferentiated retinal pigment epithelial cells are immunoreactive for vascular endothelial growth factor in surgically excised age-related macular degeneration-related choroidal neovascular membranes. Invest Ophthalmol Vis Sci. 1996, 37: 855-868.
Dor Y, Porat R, Keshet E: Vascular endothelial growth factor and vascular adjustments to perturbations in oxygen homeostasis. Am J Physiol Cell Physiol. 2001, 280: C1367-74.
Duff SE, Li C, Garland JM, Kumar S: CD105 is important for angiogenesis: evidence and potential applications. Faseb J. 2003, 17: 984-992. 10.1096/fj.02-0634rev.
Brekken RA, Li C, Kumar S: Strategies for vascular targeting in tumors. Int J Cancer. 2002, 100: 123-130. 10.1002/ijc.10462.
Sanchez-Elsner T, Botella LM, Velasco B, Langa C, Bernabeu C: Endoglin expression is regulated by transcriptional cooperation between the hypoxia and transforming growth factor-beta pathways. J Biol Chem. 2002, 277: 43799-43808. 10.1074/jbc.M207160200.
Li C, Hampson IN, Hampson L, Kumar P, Bernabeu C, Kumar S: CD105 antagonizes the inhibitory signaling of transforming growth factor beta1 on human vascular endothelial cells. Faseb J. 2000, 14: 55-64.
Burrows FJ, Derbyshire EJ, Tazzari PL, Amlot P, Gazdar AF, King SW, Letarte M, Vitetta ES, Thorpe PE: Up-regulation of endoglin on vascular endothelial cells in human solid tumors: implications for diagnosis and therapy. Clin Cancer Res. 1995, 1: 1623-1634.
Bodey B, Bodey BJ, Siegel SE, Kaiser HE: Over-expression of endoglin (CD105): a marker of breast carcinoma-induced neo-vascularization. Anticancer Res. 1998, 18: 3621-3628.
van de Kerkhof PC, Rulo HF, van Pelt JP, van Vlijmen-Willems IM, De Jong EM: Expression of endoglin in the transition between psoriatic uninvolved and involved skin. Acta Derm Venereol. 1998, 78: 19-21. 10.1080/00015559850135760.
Kumar S, Ghellal A, Li C, Byrne G, Haboubi N, Wang JM, Bundred N: Breast carcinoma: vascular density determined using CD105 antibody correlates with tumor prognosis. Cancer Res. 1999, 59: 856-861.
Li C, Guo B, Wilson PB, Stewart A, Byrne G, Bundred N, Kumar S: Plasma levels of soluble CD105 correlate with metastasis in patients with breast cancer. Int J Cancer. 2000, 89: 122-126. 10.1002/(SICI)1097-0215(20000320)89:2<122::AID-IJC4>3.0.CO;2-M.
Takahashi N, Kawanishi-Tabata R, Haba A, Tabata M, Haruta Y, Tsai H, Seon BK: Association of serum endoglin with metastasis in patients with colorectal, breast, and other solid tumors, and suppressive effect of chemotherapy on the serum endoglin. Clin Cancer Res. 2001, 7: 524-532.
van Mourik JA, Leeksma OC, Reinders JH, de Groot PG, Zandbergen-Spaargaren J: Vascular endothelial cells synthesize a plasma membrane protein indistinguishable from the platelet membrane glycoprotein IIa. J Biol Chem. 1985, 260: 11300-11306.
Muller WA, Weigl SA, Deng X, Phillips DM: PECAM-1 is required for transendothelial migration of leukocytes. J Exp Med. 1993, 178: 449-460. 10.1084/jem.178.2.449.
Vaporciyan AA, DeLisser HM, Yan HC, Mendiguren II, Thom SR, Jones ML, Ward PA, Albelda SM: Involvement of platelet-endothelial cell adhesion molecule-1 in neutrophil recruitment in vivo. Science. 1993, 262: 1580-1582.
Bogen S, Pak J, Garifallou M, Deng X, Muller WA: Monoclonal antibody to murine PECAM-1 (CD31) blocks acute inflammation in vivo. J Exp Med. 1994, 179: 1059-1064. 10.1084/jem.179.3.1059.
Albelda SM, Buck CA: Integrins and other cell adhesion molecules. Faseb J. 1990, 4: 2868-2880.
Albelda SM, Muller WA, Buck CA, Newman PJ: Molecular and cellular properties of PECAM-1 (endoCAM/CD31): a novel vascular cell-cell adhesion molecule. J Cell Biol. 1991, 114: 1059-1068. 10.1083/jcb.114.5.1059.
Bordessoule D, Jones M, Gatter KC, Mason DY: Immunohistological patterns of myeloid antigens: tissue distribution of CD13, CD14, CD16, CD31, CD36, CD65, CD66 and CD67. Br J Haematol. 1993, 83: 370-383.
Simmons DL, Walker C, Power C, Pigott R: Molecular cloning of CD31, a putative intercellular adhesion molecule closely related to carcinoembryonic antigen. J Exp Med. 1990, 171: 2147-2152. 10.1084/jem.171.6.2147.
Tawia SA, Beaton LA, Rogers PA: Immunolocalization of the cellular adhesion molecules, intercellular adhesion molecule-1 (ICAM-1) and platelet endothelial cell adhesion molecule (PECAM), in human endometrium throughout the menstrual cycle. Hum Reprod. 1993, 8: 175-181.
Metzelaar MJ, Korteweg J, Sixma JJ, Nieuwenhuis HK: Comparison of platelet membrane markers for the detection of platelet activation in vitro and during platelet storage and cardiopulmonary bypass surgery. J Lab Clin Med. 1993, 121: 579-587.
Sun QH, DeLisser HM, Zukowski MM, Paddock C, Albelda SM, Newman PJ: Individually distinct Ig homology domains in PECAM-1 regulate homophilic binding and modulate receptor affinity. J Biol Chem. 1996, 271: 11090-11098. 10.1074/jbc.271.19.11090.
Muller WA, Berman ME, Newman PJ, DeLisser HM, Albelda SM: A heterophilic adhesion mechanism for platelet/endothelial cell adhesion molecule 1 (CD31). J Exp Med. 1992, 175: 1401-1404. 10.1084/jem.175.5.1401.
Buckley CD, Doyonnas R, Newton JP, Blystone SD, Brown EJ, Watt SM, Simmons DL: Identification of alpha v beta 3 as a heterotypic ligand for CD31/PECAM-1. J Cell Sci. 1996, 109 (Pt 2): 437-45.
Piali L, Hammel P, Uherek C, Bachmann F, Gisler RH, Dunon D, Imhof BA: CD31/PECAM-1 is a ligand for alpha v beta 3 integrin involved in adhesion of leukocytes to endothelium. J Cell Biol. 1995, 130: 451-460. 10.1083/jcb.130.2.451.
DeLisser HM, Yan HC, Newman PJ, Muller WA, Buck CA, Albelda SM: Platelet/endothelial cell adhesion molecule-1 (CD31)-mediated cellular aggregation involves cell surface glycosaminoglycans. J Biol Chem. 1993, 268: 16037-16046.
Berman ME, Xie Y, Muller WA: Roles of platelet/endothelial cell adhesion molecule-1 (PECAM-1, CD31) in natural killer cell transendothelial migration and beta 2 integrin activation. J Immunol. 1996, 156: 1515-1524.
Lanza F, Healy L, Sutherland DR: Structural and functional features of the CD34 antigen: an update. J Biol Regul Homeost Agents. 2001, 15: 1-13.
Andrews RG, Singer JW, Bernstein ID: Monoclonal antibody 12-8 recognizes a 115-kd molecule present on both unipotent and multipotent hematopoietic colony-forming cells and their precursors. Blood. 1986, 67: 842-845.
Tavian M, Coulombel L, Luton D, Clemente HS, Dieterlen-Lievre F, Peault B: Aorta-associated CD34+ hematopoietic cells in the early human embryo. Blood. 1996, 87: 67-72.
Silverman JS, Tamsen A: Fibrohistiocytic differentiation in subcutaneous fatty tumors. Study of spindle cell, pleomorphic, myxoid, and atypical lipoma and dedifferentiated liposarcoma cases composed in part of CD34+ fibroblasts and FXIIIa+ histiocytes. J Cutan Pathol. 1997, 24: 484-493.
Watt SM, Karhi K, Gatter K, Furley AJ, Katz FE, Healy LE, Altass LJ, Bradley NJ, Sutherland DR, Levinsky R: Distribution and epitope analysis of the cell membrane glycoprotein (HPCA-1) associated with human hemopoietic progenitor cells. Leukemia. 1987, 1: 417-426.
Fina L, Molgaard HV, Robertson D, Bradley NJ, Monaghan P, Delia D, Sutherland DR, Baker MA, Greaves MF: Expression of the CD34 gene in vascular endothelial cells. Blood. 1990, 75: 2417-2426.
Sankey EA, More L, Dhillon AP: QBEnd/10: a new immunostain for the routine diagnosis of Kaposi's sarcoma. J Pathol. 1990, 161: 267-271.
Schlingemann RO, Rietveld FJ, de Waal RM, Bradley NJ, Skene AI, Davies AJ, Greaves MF, Denekamp J, Ruiter DJ: Leukocyte antigen CD34 is expressed by a subset of cultured endothelial cells and on endothelial abluminal microprocesses in the tumor stroma. Lab Invest. 1990, 62: 690-696.
Sutherland DR, Keating A: The CD34 antigen: structure, biology, and potential clinical applications. J Hematother. 1992, 1: 115-129.
Jaffe EA, Hoyer LW, Nachman RL: Synthesis of von Willebrand factor by cultured human endothelial cells. Proc Natl Acad Sci U S A. 1974, 71: 1906-1909.
Folkman J, Haudenschild CC, Zetter BR: Long-term culture of capillary endothelial cells. Proc Natl Acad Sci U S A. 1979, 76: 5217-5221.
Sporn LA, Chavin SI, Marder VJ, Wagner DD: Biosynthesis of von Willebrand protein by human megakaryocytes. J Clin Invest. 1985, 76: 1102-1106.
Sadler JE: Biochemistry and genetics of von Willebrand factor. Annu Rev Biochem. 1998, 67: 395-424. 10.1146/annurev.biochem.67.1.395.
Vlot AJ, Koppelman SJ, van den Berg MH, Bouma BN, Sixma JJ: The affinity and stoichiometry of binding of human factor VIII to von Willebrand factor. Blood. 1995, 85: 3150-3157.
Saenko EL, Scandella D: The acidic region of the factor VIII light chain and the C2 domain together form the high affinity binding site for von willebrand factor. J Biol Chem. 1997, 272: 18007-18014. 10.1074/jbc.272.29.18007.
de Wit TR, van Mourik JA: Biosynthesis, processing and secretion of von Willebrand factor: biological implications. Best Pract Res Clin Haematol. 2001, 14: 241-255. 10.1053/beha.2001.0132.
Goss PE, Reid C, Pintilie M, Lim R, Miller N: Male breast carcinoma: a review of 229 patients who presented to the Princess Margaret Hospital during 40 years: 1955-1996. Cancer. 1999, 85: 629-639. 10.1002/(SICI)1097-0142(19990201)85:3<629::AID-CNCR13>3.0.CO;2-V.
D'Avanzo B, La Vecchia C: Risk factors for male breast cancer. Br J Cancer. 1995, 71: 1359-1362.
Duchesne D, Tully P, Thomas B, Bourbeau R: Complete life table, Saskatchewan, 1995-1997: MALES. Life Tables Canada, Provinces and Territories 1995-1997. 2002, Ottawa, Statistics Canada Health Statistics Division, 46-
Atalay C, Kanlioz M, Altinok M: Prognostic factors affecting survival in male breast cancer. J Exp Clin Cancer Res. 2003, 22: 29-33.
Donegan WL, Redlich PN: Breast cancer in men. Surg Clin North Am. 1996, 76: 343-363.
Memon MA, Donohue JH: Male breast cancer. Br J Surg. 1997, 84: 433-435. 10.1046/j.1365-2168.1997.02721.x.
Sandler B, Carman C, Perry RR: Cancer of the male breast. Am Surg. 1994, 60: 816-820.
Bosari S, Lee AK, DeLellis RA, Wiley BD, Heatley GJ, Silverman ML: Microvessel quantitation and prognosis in invasive breast carcinoma. Hum Pathol. 1992, 23: 755-761. 10.1016/0046-8177(92)90344-3.
Acknowledgements
This study was supported in part by a grant from the Royal University Hospital Foundation Fund. The authors also wish to extend their thanks to the Saskatchewan Cancer Agency for their assistance in obtaining the records requested for this study and to Todd Reichert and Mitch Hesson for all their help in the preparation of the figures for this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
EF wrote this manuscript, aided in collection and analysis of data and is the first author.
JL provided statistical analysis of the collected data.
RK conceived the design of this study, aided in data collection and remains the corresponding and senior author.
All authors have read and approved this manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Frangou, E.M., Lawson, J. & Kanthan, R. Angiogenesis in male breast cancer. World J Surg Onc 3, 16 (2005). https://doi.org/10.1186/1477-7819-3-16
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1477-7819-3-16