Abstract
Background
Approximately 10 to 20 percent of the population is suffering from chronic pain. Since this represents a major contribution to the costs of the health care system, more efficient measures and interventions to treat these patients are sought.
Results
The development of general health and physical activity of patients with chronic pain was assessed in an interdisciplinary outpatient pain management program (IOPP). 36 patients with an average age of 48 years were included in the IOPP. Subjective assessment of well-being was performed at five time points (baseline, post intervention and 3, 6, and 12 months thereafter) by using standardized questionnaires. The study focused on the quality of life survey Medical Outcomes Study Short Form-36, which is a validated instrument with established reliability and sensitivity. In addition, the patients participated in physical assessment testing strength, power, endurance, and mobility.
Prior to therapy a substantial impairment was found on different levels. Marked improvements in the psychological parameters were obtained by the end of the program. No success was achieved with regard to the physical assessments.
Conclusion
Although many different studies have evaluated similar programs, only few of them have attained positive results such as improvements of general quality of life or of physical strength. Often no difference from the control group could be detected only some months after the intervention. In the present study no significant persistent improvement of well-being occurred. Possible reasons are either wrong instruments, wrong selection of patients or wrong interventions.
Similar content being viewed by others
Background
A trend towards a higher frequency of diseases associated with chronic pain has been observed over the past decades [1]. Ten to twenty percent of the world as well as of the Swiss population suffers from chronic pain; in 10 % treatment of pain is complicated [2]. It is the goal of the interdisciplinary outpatient pain management program (IOPP) to facilitate the patients to deal with chronic pain. Such ambulatory and multidisciplinary treatment approaches were shown to be effective in various meta-analyses [3, 4]. Magni et al. found a correlation between pain and psychological distress [5]. In patients with low back pain, representing a major fraction of chronic pain patients, the intensity of pain appeared to correlate with functional measurements and clinical outcome [6]. Quality of life (general health) can be adequately determined by at least three different methods: (i) estimation by a physician, (ii) standardized activities performed by the patient, or (iii) by standardized questionnaires [7]. Several further instruments for the measurement of general health (GH) exist [8–18]; a selection of them is presented in Table 1. Unfortunately, the applied methods vary between different studies. However, the most important aspects such as physical, psychological and social health, which is summarized as health-related quality of life (HRQL) [19], are commonly reported. Quality of life is a highly subjective item and, as indicated by the considerable number of existing methods, a reliable assessment of this parameter is very difficult, if not impossible to achieve. In the following we will present the data collected in the IOPP of the Department of Rheumatology at the University Hospital Zurich.
Results
Overall, 36 patients (22 women and 14 men) passed through IOPP from the beginning of 1999 until mid 2000 (Table 2). They suffered from chronic non-malignant pain and had multiple failed therapies in their history. Occurrence of pain for a duration exceeding six months was considered to be chronic [20].
Development of GH Short Form-36 (SF-36) during the IOPP
Comparison of pre/post pain intervention
The patients presented with marked deficiencies in the eight categories of the SF-36 before, as well as after completion of the IOPP. They were particularly impaired with regard to the parameters role-physical [RP] and bodily pain (BP). An alteration of the score values by 6 to 8 points (per dimension) was considered as clinically significant [21].
Table 3 shows that such an improvement was only achieved in the functions mental health (MH) and role-emotional (RE). The average values of the healthy US reference population were never attained in one of the 8 health categories (Figure 1). Mental health performed already much better than the physical parameters before the intervention program, but was likewise highly deficient in comparison with the average healthy US reference population [22].
Demonstration of the eight health categories of SF-36. [18] Average values at beginning (pre) and at completion (post) as well as 3 (fup1), 6 (fup2), and 12 (fup3) months, respectively, following ambulatory pain intervention program in comparison with the average healthy US reference population (US-mean, [22]).
Chronic pain causes predominantly physical impairment; subsequently and often as a consequence psychological problems follow.
Comparisons after the IOPP (post) with follow-up 1,2 and 3 (3, 6, and 12 months, respectively, following ambulatory intervention)
Physical functioning (PF) improved after six months by an average of 4 points (clinically non-significant). After the third and the last follow-up a marked and clinically significant deterioration far below the starting values was observed. RP remained constantly low over time.
Development of psychological factors and pain
6 months after the program BP clearly decreased. However, this success could not be maintained. After the following 6 months (i.e. 15 months after beginning of the study) pain increased again and on average even exceeded the original intensity. The same was observed for ME and RE; after 6 months a significant improvement was found for both parameters, which was also reduced after one year in such a way that no difference from pre-treatment remained. However, the number of patients remaining in the study until follow-up (fup) 3 was too low to be statistically calculated.
Vitality could be improved gradually. Social functioning was also improved after 6 months, but it was also not possible to maintain this positive effect. Social functioning decreased significantly and was clearly below the starting level. GH showed a wavelike progress: it already deteriorated a first time 3 months after the program, and a second time 12 months after completion of the program. It must be emphasized that GH was estimated to be worse than before IOPP 3 months after the program. In comparison with a healthy US reference population, the patients remained significantly impaired throughout the study. This is illustrated by two representative examples shown in Figure 2.
Two examples of the eight health categories of SF-36. Values of two prototype patients at beginning (pre) and end (post), as well as 3 (fup1), 6 (fup2), and 12 (fup3) months respectively following the ambulatory pain intervention program. Comparison with the average healthy US reference population (US-mean, [22]).
GH comparison between women and men
Is the impairment of general well-being more pronounced in women than in men? No significant gender differences could be found before the exercise program (Figure 3). GH of women remained stable during the IOPP as well as throughout the following year exhibiting only a minimal average increase between 6 and 12 months after the program; that of men decreased by a total of 10 points.
Development of physical fitness (assessment tests) during the IOPP
Based on the sociodemographic survey, more than 4/5 (86%) of all patients were active or moderately active before the current pain episode. At the start of the intervention all had a diminished degree of physical activity, 76% were entirely inactive. More than half of the patients were no longer able to carry out sports.
The development of muscle strength during IOPP is shown in Table 4. The force of the upper arms remained stable, those of the thigh muscles, as measured by flexion of the knee (M. quadriceps), decreased during the treatment. However, after 3 months of follow-up, flexion of the right knee showed a statistically significant improvement of muscle strength (p = 0.007, fup1) in comparison with the end of the training program (post), which decreased again during the subsequent 3 months (p = 0.013, fup2). Flexion of the left knee showed a highly significant increase of muscle strength after 3 months (p = 0.004, fup1, n = 18) in comparison with post.
The degree of subjectively-felt pain had a tendency to increase. Significant improvements were seen 9 months after the beginning of the study in the performance of the step test (p = 0.028 fup2 vs. pre) and of the arm holding test (p = 0.025 fup2 vs. post). The capability to lift a box loaded with 2.5 kg from floor to waist level (container test) improved statistically significantly during the program (p = 0.007, post vs. pre). The results of the sit and reach test, which evaluates flexibility and is thus characteristic for pain, were significantly superior against baseline at 6 (p = 0.036) and 9 months (p = 0.012) after beginning of the study, respectively. Significant temporary improvements were also observed in one leg standing (Figure 4). When comparing the heart rates by the endpoint of the sub-maximal endurance test at 9 and 6 months after study onset, a significant increase was observed (p = 0.008, fup1 vs. fup2), which suggests a diminished physical fitness. Moreover, a slight trend towards higher pulse rates at rest (before workload) was found at the fup1 compared with baseline. The subjective feeling of exhaustion in the ergometer test (Borg scale) was lower by the end of the 3 months exercise than with an identical workload at pre-treatment.
One leg standing on left (left) and right leg (right). Boxplot before (pre) and after (post) 3 month ambulatory intervention and follow-up 6 (fup1), 9 (fup2) and 15 months (fup3) following beginning of the study. n = number of patients; significant differences * p < 0.05 and ** p < 0.01 compared with pre.
Discussion
The interdisciplinary cooperation of physicians, psychologists, and physical therapists is exceptionally helpful in the treatment of patients suffering from complex health problems [23]. Many studies have examined interdisciplinary programs, some of them found a positive outcome [3, 24]. A meta-analysis performed by Flor et al. [3] found that 75% of the patients recovered from the pain disorders. In the studies of Garrat et al. (1993) and Lyons et al. (1994) the SF-36 scores were less suppressed in patients who had an interdisciplinary treatment than in those who never underwent a pain intervention program [25, 26].
In general, the comparability of different pain programs is limited due to differences in treatment, patient groups, evaluation of the results, and follow-up periods [27]. In the above-mentioned analysis of the SF-36 only a minor, non-significant improvement of the psychological healthiness and vitality was observed. In contrast, various other studies achieved comparatively slightly better results [28]. Peters et al. found a loss of treatment effect after 12 months [29].
In the IOPP deterioration already occurred after 6 months. In 1996, a study by Williams et al. [30] observed better results even though the duration of their therapy program was only 9 weeks. This raises the question whether the duration of the IOPP could be decreased. Costs are an important factor of pain intervention programs; long-term follow-up studies are therefore rare [27]. Deardorff et al. showed a significant improvement of the physical parameters in a group of ambulatory and interdisciplinary treated patients [31]. Flavell et al. studied a pain program with duration of only 6 weeks. However, after a significant initial increase the walking distance remained unchanged or even returned to baseline values during the follow-up [32]. In contrast to these studies, physical strength and fitness of our patients remained stable during the IOPP. The results of the physical components of the SF-36 appeared to correlate with those of the assessment tests. McCracken et al. showed recently that the levels of physical activity could be increased by an interdisciplinary treatment without a simultaneous decline of pain [33].
A major problem encountered with the IOPP was a relatively high rate of premature termination. It has been shown that individualized trainings, such as those employed in the IOPP, can diminish the duration of pain episodes [34]. Various studies have assessed the intensity of pain. Jensen et al. 1999 [35] has already confirmed that pain surveys, such as those used in our evaluation, are more suitable than questionnaires restricted to only a single time point.
A high prevalence of depression was seen in the present analysis, and in previous studies a correlation of self estimated pain with psychological symptoms such as anxiety and depression has been found [36]. Overall, a high number of disturbances in coping with pain (32%) and/or psychological problems (26%) were observed in the present study. Previous studies also found significant correlation between the duration of pain and the occurrence of major depression [37]. In the estimation of psychological well-being, the subscales of SF-36 turned out to be complementary to the hospital anxiety and depression scale (HADS) and to the psychological general well-being scale (PGWB) [1].
Vasseljen et al. postulated that disadvantageous working conditions might be responsible for chronic pain of shoulder and neck [38]. One third of the subjects participating in the IOPP attended only elementary schools and 50% were carrying out (or carried out in their last job) a moderately demanding physical occupation. The high number of patients who have not passed an apprenticeship indicates that disadvantages in employment (often combined with a physically wearing workload) can cause pain encompassing the vertebral column. Nonetheless, individuals with an academic degree were also affected. Chronic pain is not caused by physically demanding work alone; it also occurred in 26% of those who had a mostly sitting activity during their current (or last) occupation.
The success of rehabilitation was inferior in women than in men in the study of Jensen et al. [39]. They concluded, that distinct treatment strategies for men and women should be developed. In the IOPP, the GH of women remained stable even one year post-discharge, while that of men decreased significantly. However, the reason for this unexpected finding remains unclear.
Thirty different treatment centers in the US, Canada, Europe, and New Zealand were evaluated in 1992 by Linssen et al. [40]. The authors concluded that most of the offered treatment programs were highly complex and expensive, were adjusted to closely selected patient groups, and exhibited high dropout rates. It appears that these shortcomings could not be eliminated in the past years.
Conclusions
The disappointing success of the IOPP raises the following questions: are more specific criteria required for the treatment of diverse patients? Should the inclusion criteria be narrowed? Has the number of patients to be increased? Are the methods used sufficiently sensitive? Are the patients treated at the appropriate time point?
Patient number
The statistical power of a trial depends on a sufficiently high number of participants. Part of the question could possibly be better resolved by a multicentric proceeding [41].
Methods used
Among the high number of existing instruments it is difficult to select the most suitable. The SF-36 is a valid method for the assessment of general health [21].
Timing of treatment
Patients who underwent an interdisciplinary treatment without delay revealed less pain and a better psychological condition [28]. Early onset of therapy is thought to inhibit a possible chronification [42]. A shorter previous history of pain, a high extent of occupation before the program, preconditions related to profession and education, as well as a general elevated level of activity turned out to be positive predictors of treatment success [43].
The participants of our study stated that they have profited by the IOPP with an average goal attainment of 72.3%, which indicates that a progress towards higher quality of life and greater self-determination was achieved. However, these experiences also confirmed that the participating patients are suffering from a complex disease, which is combined to some extent with violent psychosocial impairments. Due to psychosomatic components, as well as partially major disorders of perception and thinking, an interdisciplinary proceeding with the rehabilitation program is required. A substantial need for pain management programs exists; hence it is useful to optimize them and to evaluate the long-term effectiveness. Based on the presented findings, the content and structure of the IOPP was largely modified in April 2001. First preliminary results are encouraging [44]. Further data on the outcome will be presented as soon as this ongoing study is completed.
Methods
Patient characteristics
One third of the 36 patients who completed the IOPP attended elementary school, one third had visited a vocational, trade, or business school, or an apprenticeship, and the remaining third had higher education. None of the patients carried out a very demanding physical occupation recently. Only one patient (3%) was capable to full-time work. Seven men and 14 women could earn their living with their income. One third had economical problems. Almost 30% did not obtain assistance from their family, although 70% lived together with his or her wife/husband. Three quarters lived in an urban setting. In one third the average history of suffering from chronic pain exceeded six years. 38% of the patients indicated that pain was the predominate nuisance, followed by inability to work (24%), restrictions related to free time, occupation, housekeeping, friends and quality of life (16%), psychological difficulties due to pain (11%) and loss of independence (4%). 62% were non-smoking and none said that they consume alcohol several times per day. 35% drunk no alcohol at all.
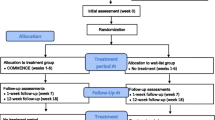
Design of the pain program
The IOPP consisted of a theoretical section, painting therapy, medical training therapy (MTT), group psychotherapy, relaxation therapy, medical motion therapy, and physiotherapeutic, psychotherapeutic and/or medicinal individual therapies adapted to individual patient problematic, and one evening with family members.
Various questionnaires were completed before (pre) and at the end of the program (post), as well as 3 (fup1), 6 (fup2) and 12 months (fup3) after completion of the program. This comprised of the SF-36 [18], health-related questionnaire (HADS-D, [11]), the multidimensional pain questionnaire (MPI-D, [45]), questions on coping with pain (CSQ, [46]), a sociodemographic and socioeconomic survey, (the model sheet [47]), the examination of goal achievement (GAS, [7]) and a pain and sleep diary. In addition the participants underwent body assessment tests to determine their development in the physical field.
Assessment of subjective well-being
The health-related (subjective) quality of life assessment was performed by the Medical Outcome Study SF-36 [48]. A German translation of the international standard version was used [49]. Questions refer to the past 4 weeks (standard version). The SF-36 consists of 36 items with 8 subscales and two summary scores for a physical (PCS=physical component summary) and a psychological component (MCS=mental component summary), respectively. Calculations of the scores were done according to Ware et al. [22]. Scales were transformed into values ranging from 0 to 100. Higher values always indicate a better health condition.
Physical fitness
Physical strength was evaluated by various assessment tests. In the step-test patients stepped up and down on a chest as often as possible. The arm holding test determined the time during which an on the back lying patient was able to hold two weights with stretched arms. In addition, the patients indicated their momentary pain intensity on a numerical scale. The Waddell test was used to discern physical from non-organic symptoms in back pain patients [50]. Coordination and equilibrium were examined by single leg standing and by a walk on balance boards. During flexibility assessment the patients had to reach forward to the toes with extended knees in a seated position (sit and reach test). Patients were also asked to lift a box loaded with 2.5 kg from floor to waist or from waist to head level, repeated five times. The weight was then progressively increased by 2.5 kg (container test). Endurance was assessed at sub-maximal workload in an ergometer test starting with a power of 25 Watt during 4 minutes. Then the patients were ask for their perceived exertion according to the Borg scale before the applied power was gradually increased by 25 Watt. Finally the maximal isometric flexion and extension strength of the left and right upper arm and thigh muscles (elbow extension and flexion, knee extension and flexion) were evaluated [51].
Statistical analysis
Statistical analysis was done using SPSS (Version 7.0, SPSS Inc., Chicago, USA). Significant differences are based on non-parametric tests. Differences of matched samples were established by using the Wilcoxon test. P-values < 0.05 were considered as statistically significant.
Abbreviations
- IOPP:
-
interdisciplinary outpatient pain management program fup1, fup2, fup3: follow-up 1, 2, and 3
References
Becker N, Bondegaard Thomsen A, Olsen AK, Sjogren P, Bech P, Eriksen J: Pain epidemiology and health related quality of life in chronic non-malignant pain patients referred to a Danish multidimensionary pain center. Pain. 1997, 73: 393-400. 10.1016/S0304-3959(97)00126-7.
Geissner E, Flor H: Klinisch-psychologische Schmerzforschung. Z Klin Psychol. 1999, 28: 233-234. 10.1026//0084-5345.28.4.233.
Flor H, Fydrich T, Turk D: Efficacy of multidisciplinary pain treatment centers: a meta-analytic review. Pain. 1992, 49: 221-230. 10.1016/0304-3959(92)90145-2.
Malone MD, Strube MJ, Scogin FR: Meta-analysis of non-medical treatments for chronic pain. Pain. 1988, 34: 231-244. 10.1016/0304-3959(88)90118-2.
Magni G, Moreschi C, Rigatti-Luchini S, Merskey H: Prospective study on the relationship between depressive symptome and chronic muskuloskeletal pain. Pain. 1994, 56: 289-297. 10.1016/0304-3959(94)90167-8.
Holmstrom E, Moritz U: Low back pain –– correspondence between questionnaire, interview and clinical examination. Scand J Rehabil Med. 1991, 23: 119-125.
Sangha O, Stucki G: Patienten-zentrierte Evaluation der Krankheitsauswirkungen bei muskuloskelettalen Erkrankungen: Uebersicht über die wichtigsten Outcome-Instrumente. Z Rheumatol. 1997, 56: 322-333. 10.1007/s003930050046.
Balaban DJ, Sagi PC, Goldfarb NI, Nettler S: Weigths for scoring the quality of well-being instrument among rheumatoid arthritics. A comparison to general population weights. Med Care. 1986, 24: 973-980.
Kessler S, Jäckel WH, Cziske R, Potthoff P, Jacobi E: Sickness Impact Measurement Scales: Validierung einer deutschen Version. Z Rheumatol. 1990, 49: 48-
Beck AT, Steer RA, Garbin MG: Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin Psychol Rev. 1988, 8: 77-100. 10.1016/0272-7358(88)90050-5.
Zigmond AS, Snaith RP: The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983, 67: 361-370.
Dupuy HJ: The psychological general well-being (PGWB) index. In: Assessment of quality of life in clinical trials of cardiovascular therapies. Edited by: Wenger NK, Mattson ME, Furberg JF, Elinson JA. 1984, New York, LeJacq, 170-183.
Dworkin SF, von Korff M, Witney CW, LeResche L, Dicker BG, Barlow W: Measurement of characteristic pain intensity in field research. Pain. 1990, Suppl 5: 290-10.1016/0304-3959(90)92696-N.
McDowell IM, Martini CJ, Waugh W: A method for self-assessment of disability before and after hip replacement operations. Br Med J. 1978, 2: 857-859.
Nicholas MK: An evaluation of cognitive, behavioural and relaxation treatments for chronic low back pain. PhD thesis, University of Sydney, Australia. 1988
McCracken LM, Gross RT: The Pain Anxiety Symptoms Scale (PASS) and the assessment of emotional responses to pain. In: Innovation in clinical practice: a sourcebook. Edited by: VandeCreek L, Knapp S, Jackson TL. 1995, Sarasota, Professional Resources Press, 14: 309-321.
Ware JE, Kosinski M, Keller SD: A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996, 34: 220-233. 10.1097/00005650-199603000-00003.
Ware JE, Sherbourne CD: The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992, 30: 473-483.
Schipper H: Guidelines and caveats for quality of life measurement in clinical practice and research. Oncology Huntingt. 1990, 4: 51-57.
Rosomoff HL, Fishbain DA, Goldberg M, Santana R, Rosomoff RS: Physical findings in patients with chronic intractable benign pain of the neck and/or back. Pain. 1989, 37: 279-287. 10.1016/0304-3959(89)90192-9.
Bronfort G, Bouter LM: Responsivness of general health status in chronic low back pain: a comparison of the COOP Charts and the SF-36. Pain. 1999, 83: 201-209. 10.1016/S0304-3959(99)00103-7.
Ware JE, Snow KK, Kosinski M, Gandek B: SF-36 Health survey manual and interpretation guide. Boston, MA: New England Medical Centre, The Health Institute. Orion Software Development, Santa Clara, USA. 1993
Fordyce WE: Psychological factors in the failed back. Int Disabil Stud. 1988, 10: 29-31.
Morley S, Eccleston C, Williams A: Systematic review and meta-analysis of randomized controlled trials of cognitive behaviour therapy and behaviour therapy for chronic pain in adults, excluding headaches. Pain. 1999, 80: 1-13. 10.1016/S0304-3959(98)00255-3.
Garratt AM, Ruta DA, Abdalla MI, Buckingham JK, Russell IT: The SF-36 health survey questionnaire: an outcome measure suitable for routine use within the NHS?. BMJ. 1993, 306: 1440-1444.
Lyons RA, Lo SV, Littlepage BN: Comparative health status of patients with 11 common illnesses in Wales. J Epidemiol Community Health. 1994, 48: 388-390.
Harkapaa K, Mellin G, Jarvikoski A, Hurri H: A controlled study on the outcome of inpatient and outpatient treatment of low back pain. Part III. Long-term follow-up of pain, disability, and compliance. Scand J Rehabil Med. 1990, 22: 181-188.
Becker N, Sjogren P, Bech P, Olsen AK, Eriksen J: Treatment outcome of chronic non-malignant pain patients managed in a Danish multidisciplinary pain centre compared to general practice: a randomised controlled trial. Pain. 2000, 84: 203-211. 10.1016/S0304-3959(99)00209-2.
Peters J, Large RG, Elkind G: Follow-up results from a randomised controlled trial evaluating in- and outpatient pain management programmes. Pain. 1992, 50: 41-50. 10.1016/0304-3959(92)90110-W.
Williams AC, Richardson PH, Nicholas MK, Pither CE, Harding VR, Ridout KL, Ralphs JA, Richardson IH, Justins DM, Chamberlain JH: Inpatient vs. outpatient pain management: results of a randomised controlled trial. Pain. 1996, 66: 13-22. 10.1016/0304-3959(96)02996-X.
Deardorff WW, Rubin HS, Scott DW: Comprehensive multidisciplinary treatment of chronic pain: a follow-up study of treated and non-treated groups. Pain. 1991, 45: 35-43. 10.1016/0304-3959(91)90162-Q.
Flavell HA, Carrafa GP, Thomas CH, Disler PB: Managing chronic back pain: impact of an interdisciplinary team approach. Med J Aust. 1996, 165: 253-255.
McCracken LM, Spertus IL, Janeck AS, Sinclair D, Wetzel FT: Behavioral dimensions of adjustment in persons with chronic pain: pain-related anxiety and acceptance. Pain. 1999, 80: 283-289. 10.1016/S0304-3959(98)00219-X.
Dettori JR, Bullock SH, Sutlive TG, Franklin RJ, Patience T: The effects of spinal flexion and extension exercises and their associated postures in patients with acute low back pain. Spine. 1995, 20: 2303-2312.
Jensen MP, Turner JA, Romano JM, Fisher LD: Comparative reliability and validity of chronic pain intensity measures. Pain. 1999, 83: 157-162. 10.1016/S0304-3959(99)00101-3.
Linton SJ, Götestam KG: Relations between pain, anxiety, mood and muscle tension in chronic pain patients. A correlation study. Psychother Psychosom. 1985, 43: 90-95.
Herr KA, Mobily PR, Smith C: Depression and the experience of chronic back pain: a study of related variables and age differences. Clin J Pain. 1993, 9: 104-114.
Vasseljen O, Westgaard RH: Can stress-related shoulder and neck pain develop independently of muscle activity?. Pain. 1996, 64: 221-230. 10.1016/0304-3959(95)00103-4.
Jensen I, Nygren A, Gamberale F, Goldie I, Westerhol P: Coping with long-term muskuloskeletal pain and its consequences: Is gender a factor?. Pain. 1994, 57: 167-172. 10.1016/0304-3959(94)90220-8.
Linssen AC, Spinhoven P: Multimodal treatment programmes for chronic pain: a quantitative analysis of existing research data. J Psychosom Res. 1992, 36: 275-286. 10.1016/0022-3999(92)90092-G.
Bergstrom G, Jensen IB, Bodin L, Linton SJ, Nygren AL, Carlsson SG: Reliability and factor structure of the Multidimensional Pain Inventory – Swedish Language Version: (MPI-S). Pain. 1998, 75: 101-110. 10.1016/S0304-3959(97)00210-8.
Wilkes MS: Chronic back pain: does bed rest help?. West J Med. 2000, 172: 121-10.1136/ewjm.172.2.121.
Loupasis GA, Stamos K, Katonis PG, Sapkas G, Korres DS, Hartofilakidis G: Seven- to 20-year outcome of lumbar discectomy. Spine. 1999, 24: 2313-2317. 10.1097/00007632-199911150-00005.
Litschi M, Reiss A, Buhler D, Dober S, Jeger P, Luscher C, Neukom S, Willi U, Michel BA, Uebelhart D, Sprott H: Interdisciplinary outpatient pain program (IOPP). Swiss Med Wkly. 2001, 31 (Suppl 126): S24-
Flor H, Rudy TE, Birbaumer N, Streit B, Schugens MM: Zur Anwendbarkeit des West Haven-Yale Multidimensional Pain Inventory im deutschen Sprachraum. Schmerz. 1990, 4: 82-87.
Rosenstiel AK, Keefe FJ: The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain. 1983, 17: 33-44. 10.1016/0304-3959(83)90125-2.
Tobler A, Fransen J, Huber E, Steiner W: Anwendung des Rehab-Cycles in der klinischen Praxis. Fallbeispiel: suprapatellärer Knieschmerz. Physiotherapie. 2001, 7: 4-11.
Bullinger M, Kirchberger I: SF-36: Fragebogen zum Gesundheitszustand (Handanweisung). Hogrefe Verlag für Psychologie. 1998, 7:
Ware JE, Gandeck B, and the IQOLA Project Group: The SF-36 health survey: development and use in mental health research and the IQOLA Project. Int J Mental Health. 1994, 23: 49-73.
Waddell G: Occupational low-back pain, illness behavior and disability. Spine. 1991, 16: 683-685.
Huber E, Stoll T, Ehrat B, Hofer HO, Seifert B, Stucki G: Zuverlässigkeit und Normperzentilen einer neuen isometrischen Muskelkraftmessmethode. Physiotherapie. 1997, 2-8.
Acknowledgements
We thank L. Ryser for excellent patient care, D. Bühler for assistance with physiotherapy, Dr. W. Steiner for IT support and L. Pobjoy for manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contributions
HS conceived and accomplished the study and participated in the analysis and writing of the manuscript. DU participated in study design and coordination. BAM participated in the design of the study. BJ carried out the statistical analysis and participated in writing of the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Joos, B., Uebelhart, D., Michel, B.A. et al. Influence of an outpatient multidisciplinary pain management program on the health-related quality of life and the physical fitness of chronic pain patients. J Negat Results BioMed 3, 1 (2004). https://doi.org/10.1186/1477-5751-3-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1477-5751-3-1