Abstract
Background
α-Galactosylceramide (α-GalCer) can be presented by CD1d molecules of antigen-presenting cells, and is known to induce a potent NKT cell-dependent cytotoxic response against tumor cells. However, the main effector cells in α-GalCer-induced antitumor immunity are still controversial.
Methods
In order to elucidate the cell phenotype that plays the most important role in α-GalCer-induced antitumor immunity, we purified and analyzed tumor-infiltrating leukocytes (TILs) from liver metastatic nodules of a colon cancer cell line (Colon26), comparing α-GalCer- and control vehicle-treated mice. Flow cytometry was performed to analyze cell phenotype in TILs and IFN-γ ELISA was performed to detect antigen-specific immune response.
Results
Flow cytometry analysis showed a significantly higher infiltration of NK cells (DX5+, T cell receptor αβ (TCR)-) into tumors in α-GalCer-treated mice compared to vehicle-treated mice. The DX5+TCR+ cell population was not significantly different between these two groups, indicating that these cells were not the main effector cells. Interestingly, the CD8+ T cell population was increased in TILs of α-GalCer-treated mice, and the activation level of these cells based on CD69 expression was higher than that in vehicle-treated mice. Moreover, the number of tumor-infiltrating dendritic cells (DCs) was increased in α-GalCer-treated mice. IFN-γ ELISA showed stronger antigen-specific response in TILs from α-GalCer-treated mice compared to those from vehicle-treated mice, although the difference between these two groups was not significant.
Conclusions
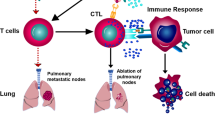
In α-GalCer-induced antitumor immunity, NK cells seem to be some of the main effector cells and both CD8+ T cells and DCs, which are related to acquired immunity, might also play important roles in this antitumor immune response. These results suggest that α-GalCer has a multifunctional role in modulation of the immune response.
Similar content being viewed by others
Background
Colorectal cancer is one of the most common neoplasms worldwide. The mortality of this malignancy is closely related to the existence of metastatic liver disease [1, 2]. Many treatments, including chemotherapy and transcatheter arterial embolization, have been used to treat patients with metastatic liver lesions of colorectal cancer, however, the clinical outcome has not been satisfactory [2, 3]. Therefore, a new treatment modality is necessary to achieve a breakthrough in this area.
Recently, a specific glycolipid antigen, α-galactosylceramide (α-GalCer), has been reported to induce significant antitumor immunity in the mouse hepatic metastases model [4–6]. α-GalCer can be presented by CD1d molecules of antigen-presenting cells, and is known to induce a potent natural killer T (NKT) cell-dependent cytotoxic response against tumor cells [7–10]. Several reports have indicated the direct cytotoxicity of NKT cells in murine in vivo or in vitro models [6, 7, 11, 12], which suggested that NKT cells were the main effector cells in α-GalCer-induced antitumor immunity. On the other hand, other studies suggested that NK cells are the main cytotoxic effectors in the liver of α-GalCer-treated mice [5, 13–15]. Some reports [4, 5] demonstrated that α-GalCer-induced regression of hepatic metastases was related to marked augmentation of the cytotoxicity of hepatic lymphocytes against tumor cell lines in vitro, and the main effector cells among the hepatic lymphocytes of the induced cytotoxicity were NK cells, not NKT cells. In addition, they suggested that CTLs specific to tumor cells were also generated in vivo in response to α-GalCer, since mice cured of hepatic metastases upon treatment with α-GalCer acquired tumor-specific immunity. Our previous study [16] also demonstrated that, among human hepatic lymphocytes, Va24 NKT cells proliferated significantly in response to α-GalCer, whereas the direct effector cells of the elicited antitumor cytotoxicity in vitro were CD3-CD56+ NK cells. The proliferating Vα24 NKT cells did not exhibit any cytotoxicity against the K562 and Colo201 cell lines. Eberl and MacDonald demonstrated that activated NKT cells selectively induced NK cell proliferation and cytotoxicity via an IFN-γ and IL-12-dependent pathway [17]. Thus, NKT cells, activated by a specific CD1d-restricted antigen, may induce innate immunity indirectly via NK cells.
In this study, to elucidate the cell phenotype that plays the major role in this α-GalCer-induced antitumor immunity, we purified tumor-infiltrating leukocytes (TILs) from liver metastatic nodules of mice 3 weeks after the intrasplenic inoculation of colon cancer cells. The cell population consisting of TILs was analyzed by flow cytometry and compared between α-GalCer- and control Vehicle-treated mice. CD8+ T cells and DCs as well as NK cells infiltrated metastatic tumors more extensively in α-GalCer-treated mice. Our results suggest that α-GalCer has a multifunctional role in modulation of the immune response.
Methods
Mice
Female Balb/c mice were obtained from Japan SLC (Shizuoka, Japan) and kept in a specific pathogen-free animal facility in our university. They were used in experiments at 6 to 7 weeks of age. Groups of 9 mice were used in each experiment. Experiments were repeated three times.
Antibodies
FITC-labeled anti-mouse CD3 (145-2C11), CD4 (GK1.5), CD11c (HL3), CD69 (H1.2F3), anti-mouse αβ T cell receptor (H57-597), and anti-I-Ad (AMS-32.1), and PE-labeled anti-panNK cell (DX5), anti-CD8 (53-6.7), anti-CD80 (16-10A1), and anti-B220 (RA3-6B2) monoclonal antibodies were purchased from Becton-Pharmingen (San Diego, CA).
Liver metastasis model of colorectal cancer in mice
Mice were anesthetized and the left flank was cut to open the peritoneal cavity. After the spleen was pulled out, it was inoculated with 2 × 105 Colon26 cells, followed by splenectomy. The mice were allowed to recover for 6 days, randomized and divided into two groups on day 7: alpha-galactosylceramide (α-GalCer, kindly provided by Kirin Brewery Co, LTD) treatment group and control treatment (vehicle-treated) group. On days 7, 14, 17, and 20, mice were injected intraperitoneally with 100 μg/kg (mouse body weight) of α-GalCer or an equal amount of vehicle (0.5% polysorbate 20 in 0.9% NaCl solution). On day 21, mice were sacrificed and their livers were collected and weighed. At this time, metastasis to other organs was also examined.
Preparation of hepatic leukocytes and tumor-infiltrating leukocytes
Tumor nodules were carefully cut out from the livers macroscopically and treated so as not to include adjacent normal liver parenchyma using a razor. Tumor nodules were then inoculated with 1% of collagenase type IV solution using 27G needles and then minced using scissors. Nodules were then incubated at 37°C for 30 min, and a single-cell suspension was obtained by pushing these incubated tissue sections using the piston of a 10 ml syringe. Cell suspensions were passed through a 100-gauge stainless steel mesh to eliminate dead aggregated cells. Erythrocytes were then lysed by treating them with NH4Cl buffer (0.15 M NH4Cl, 0.1 mM EDTA, 10 mM KHCO3). Hepatic leukocytes (HLs) were collected using basically the same methods. To separate leukocytes from tumor cells or hepatocytes, cells were washed three times with PBS containing 100 units/ml heparin, suspended in PBS, and overlaid on Lympholyte M (1.0875; Cedarlane, Ontario, Canada). Centrifugation was performed at 1,500 g for 30 min at room temperature. The interface fraction was collected, and washed at least three times with PBS. According to the microscopic findings, almost all of contaminating hepatocytes and tumor cells were spun down to the high-density fraction. Finally, anti-CD45 MicroBeads (Miltenyi Biotec GmbH, Bergish Gladbach, Germany) were added to the cells collected from the interface fraction and leukocytes were positively selected using MiniMACS (Miltenyi Biotec) according to manufacturer's instructions. Collected leukocytes were analyzed by flow cytometry.
Flow Cytometry
Approximately 1 million cells were suspended in 100 μl of PBS/0.1%BSA/0.1% sodium azide and then incubated with anti-FcR (Pharmingen) for 15 min at 4°C to prevent nonspecific binding by mAb. The cells were then spun down, resuspended in 100 μl of PBS/0.1%BSA/0.1% sodium azide, and 2 μl of labeled Ab was added. After 30 min of incubation at 4°C, the suspension was washed two times with PBS/0.1%BSA/0.1% sodium azide. Analysis was performed using a FACSCalibur flow cytometer (Becton Dickinson, San Jose, CA). CellQuest software (Becton Dickinson) was used for data analysis.
IFN-γ ELISA
TILs were suspended in 10% FCS-RPMI 1640 medium at a density of 2 × 105 cells or 2 × 104 cells per 100 μl per well in 96-well U-bottomed plates. Irradiated Colon26 tumor cells or NIH3T3 cells were suspended at a density of 2 × 105 cells/ml and 100 μl of suspension was added to each well. Supernatants were harvested after 24 h of incubation at 37°C, and tested for the IFN-γ concentration using an ELISA kit (Genzyme, Cambridge, MA). Assays were performed according to the manufacturer's instructions.
Statistical Analysis
Survival time was compared with the Kaplan-Meier method, and significance was determined by the log-rank test. Student's t-test was used to determine statistical significance. Differences at P < 0.05 were considered statistically significant.
Results
Establishment of liver metastatic models of colon cancer cells
Balb/C mice were inoculated with tumor cells to determine the optimal conditions for mimicking liver metastasis of colorectal cancer in humans. Liver metastasis of colorectal cancer usually consisted of discrete nodular lesions, rather than diffusely infiltrating lesions. The injection of more than one million cells into the spleen sometimes gave very diffuse metastatic lesions in the liver without discrete nodules. However, when the spleen was inoculated with 2 × 105 cells of cancer cells, liver metastases were always discrete lesions that ranged in diameter from 3 mm to 8 mm when the mice were sacrificed on day 14. When 4 × 104 or fewer tumor cells were injected, the establishment of macroscopic metastasis on day 14 was inconsistent. Therefore, we decided to inoculate 2 × 105 Colon26 cells to each mouse on day 0.
On day 7, mice were first treated with α-GalCer or vehicle. The same treatment was repeated on day 14 and then once every three days until death. Figure 1 shows the survival curves of the α-GalCer-treated and control groups. These two groups showed a statistically significant difference in survival (p < 0.0001). The first death occurred on day 22 in the control group and on day 33 in the α-GalCer group. All of the mice in the control group died within 31 days after tumor inoculation. On the other hand, more than half of the mice in the α-GalCer group was still alive on day 37. However, perhaps due to the late start of α-GalCer treatment after tumor inoculation, none of the mice survived after 55 days even in the α-GalCer-treated group. Thus, we decided to sacrifice mice in both groups on day 21 to enucleate tumor nodules.
Survival in the Colon26 hepatic metastasis model. 2 × 105 Colon26 cells were injected into the spleen of each mouse on day 0. Colon26-bearing mice were randomly divided into an α-GalCer group and a control Vehicle group (9 mice per group). On day 7, day 14, and every 3 days thereafter, α-GalCer (100 μg/kg body weight) or control Vehicle (same volume as α-GalCer) was inoculated into the peritoneal cavity, and survival was monitored daily until all of the mice had died. ○, Vehicle-treated mice; □, α-GalCer-treated mice.
Table 1 shows the liver weight and the number of tumor nodules per mouse in both groups on day 21. Vehicle-treated mice had significantly heavier livers than control mice (p < 0.05) due to extensive metastasis, whereas there was no significant difference between these mice and the α-GalCer-treated group. On the other hand, there were significantly fewer metastatic nodules in the α-GalCer group than in the vehicle-treated group (p < 0.05). Peritoneal tumor nodules were also found in three mice in the vehicle-treated group, but not in the α-GalCer group. These mice had slightly bloody ascites. No distant metastasis was found in either group.
Comparison of cell populations comprising tumor-infiltrating leukocytes
To obtain an adequate number of TILs for flow cytometry analysis, tumor nodules obtained from three mice in the same group were pooled and mixed into one sample. Since both groups had nine mice, in each experiment flow cytometry data were acquired in triplicate. Although this difference was not statistically significant, there were more TILs in the α-GalCer group (1.19 × 108 cells/g tumor tissue) than in the control group (1.05 × 108 cells/g tumor tissue).
Figure 2 shows the flow cytometry analysis of TILs and HLs from α-GalCer-treated or vehicle-treated mice. The percentages of DX5+ TCR- NK cells and DX5+ TCR+ NKT cells among TILs were less than those in HLs in normal liver parenchyma. The percentage of NK cells in TILs was lower than that in HLs purified from control mice that were not injected with tumor (α-GalCer-treated: 5.8 ± 0.7% vs. 8.0 ± 0.9%, vehicle-treated: 2.8 ± 0.3% vs. 9.4 ± 1.1%). However, NK cell infiltration into the tumors was significantly enhanced by α-GalCer-treatment of mice (5.8 ± 0.7% vs. 2.8 ± 0.3%). On the other hand, no significant increase in the DX5+ NKT cell population was found in the tumors of α-GalCer-treated mice compared to Vehicle-treated mice. Interestingly, the proportion of CD8+ T cells in TIL was clearly enhanced in α-GalCer-treated mice (11.7 ± 1.3%) compared to vehicle-treated mice (3.4 ± 0.3%). Accordingly, the CD8/CD4 ratio was higher in TIL from α-GalCer-treated mice (ratio 0.40) than in that from vehicle-treated mice (ratio 0.16). Moreover, CD69 expression was mildly enhanced on CD8+ T cells from α-GalCer-treated mice (33.3 ± 2.7% positive in CD8+ population) compared to those from vehicle-treated mice (12.4 ± 1.6% positive in CD8+ population).
Flow cytometry analysis of tumor-infiltrating cells (I). Leukocytes were isolated from liver parenchyma or metastatic liver tumors as described in the Materials and Methods. After incubation with anti-FcR antibody, cells were stained with pairs of FITC- and PE-labeled antibodies to analyze lymphocyte populations. The following combinations were used; FL1/FL2: αβ TCR/panNK (DX5), CD4/CD8, and CD69/CD8. Average percentages of each quadrant, calculated from three samples, are indicated. Underlined numbers in the CD4/CD8 dot plots show the CD8/CD4 ratio. The histograms show CD69 expression on CD8+ T cells and the percentages of CD69+ cells among CD8+ T cells are indicated. Representative data of three experiments are shown. TIL: tumor-infiltrating leukocyte, HL: hepatic leukocyte.
Interestingly, the DC population was significantly larger in TILs of α-GalCer-treated mice than in those of vehicle-treated mice (3.1 ± 0.7% vs. 1.4 ± 0.3%) (Figure 3). The DC population in TILs was greater than that in corresponding hepatic lymphocytes (α-GalCer-treated: 2.8 ± 0.7% vs. 0.4 ± 0.2%, vehicle-treated: 1.4 ± 0.3% vs. 1.2 ± 0.2%), suggesting the active infiltration of DCs into tumors, especially in α-GalCer-treated mice. A comparison of CD11c/CD80 and I-A/B220 staining data indicated that some of the tumor-infiltrating DCs in α-GalCer-treated mice were CD80-negative, which suggested the enhanced infiltration of immature DCs.
Flow cytometry analysis of tumor-infiltrating cells (II). Leukocytes isolated from liver parenchyma or metastatic liver tumors were stained with pairs of FITC- and PE-labeled antibodies to analyze the DC population. After incubation with anti-FcR antibody, cells were stained with the following antibody combinations. FL1/FL2: CD11c/CD80, and I-A/B220. The numbers in each dot plot show the average percentages of the quadrant calculated from three samples. Representative data of three experiments are shown. TIL: tumor-infiltrating leukocyte, HL: hepatic leukocyte.
IFN-γ secretion by TILs
TILs purified from α-GalCer-treated and vehicle-treated mice were cultured with 1 × 104 target cells for 24 h and supernatants were collected for ELISA. Figure 4 shows the IFN-γ secretion in each of 3 subgroups from α-GalCer- and vehicle-treated mice. Although the amounts secreted were low and no significant differences were observed between the two groups (average at 10:1 of E:T ratio; α-GalCer: 57.8 ± 10.0 pg/ml, Vehicle: 45.1 ± 4.9 pg/ml), some of the pooled TIL samples from α-GalCer-treated group showed slightly higher IFN-γ secretion when Colon26 tumor cells were used as target cells. No IFN-γ secretion was observed when control cells were used as a target (average at 10:1 of E:T ratio; α-GalCer: 20.0 ± 3.2 pg/ml, Vehicle: 19.5 ± 3.7 pg/ml).
IFN-γ secretion by tumor-infiltrating cells. TILs purified from α-GalCer-treated and Vehicle-treated mice were cultured with 1 × 104 target cells for 24 h and supernatants were collected for IFN-γ ELISA. Each sample of α-GalCer-treated and Vehicle-treated group is shown. Filled symbols: TILs from α-GalCer-treated mice, Open symbols: TILs from Vehicle-treated mice. Representative data of two experiments are shown.
Discussion
α-GalCer can elicit a very strong antitumor immune response in many tumor models of mice. Recent studies have demonstrated that IFN-γ secreted by α-GalCer-activated NKT cells can activate NK cells, resulting in enhanced antitumor immunity [13, 15, 18]. Several murine models have shown that NKT cell-deficient mice or NK cell-depleted mice have decreased or diminished antitumor immunity [19, 20]. On the other hand, some studies have suggested that tumor-specific T cells are involved in the shrinkage or rejection of tumors [5, 21, 22]. Therefore, the collaboration of several cell types seems to be important for the anti-metastatic effect of α-galactosylceramide.
To investigate how innate and adoptive immunity work in the α-GalCer-induced antitumor immune response, especially at the site of liver metastasis of colorectal cancer, we used a well-established murine colon cancer cell line, Colon26, in Balb/C mice. We first tried to establish a C57BL/6 mice model with the syngeneic MC38 colon cancer cell line [23] using the NK1.1 molecule as a NKT cell marker. However, it was hard to determine the optimal conditions to achieve constant numbers of discrete nodules, since MC38 cells sometimes showed diffuse invasive metastasis to the liver. Thus, we chose the Colon26 liver metastasis model in Balb/C mice for this study.
Although Balb/C mouse strain does not express NK1.1 antigen [24, 25], recent reports have demonstrated that a panNK cell marker, DX5 antigen, can be a marker of NKT cells in NK1.1 allelic negative mice [26, 27]. According to our results, the DX5+ TCR+ NKT cell population in TILs did not increase by α-GalCer treatment (Fig. 2). However, it is becoming clear that the NKT cell population consists of several subpopulations [28], and therefore, our flow cytometry data may not exclude the involvement of DX5- NKT cells in this antitumor immunity. Our data demonstrate that NK cells are some of the main effector cells in our system, since there was a significant increase in the DX5+TCR- NK cell population in α-GalCer-treated mice (Fig. 2). Correspondingly, Kobayashi et al. [4] and Nakagawa et al. [5] demonstrated, using a hepatic metastasis model, that the administration of α-GalCer to mice enhanced the cytotoxicity of HLs against tumor cell lines in vitro, and showed that the main effector cells among HLs were NK cells, not NKT cells. Our previous study [16] also demonstrated that, among human HLs, Vα24 NKT cells proliferated significantly in response to α-GalCer, whereas the direct effector cells of the induced antitumor cytotoxicity in vitro were CD3-CD56+ NK cells.
On the other hand, the finding that the proportion of tumor-infiltrating DCs increased is highly significant (Fig. 3), since this may indicate the subsequent establishment of acquired immunity. Clinically, an increased number of tumor-infiltrating DCs has been reported to correlate with a better prognosis in cancer patients [29, 30]. Interestingly, we observed a stronger infiltration of CD80-negative DCs as well as CD80-positive DCs into tumors in α-GalCer-treated mice than in vehicle-treated mice. An increased number of immature DCs in tumors might reflect the rapid infiltration of DCs from surrounding liver parenchyma, and these DCs might mature during antigen processing. Since immature DCs have advantages for infiltrating tumor nodules and taking up tumor antigens for T cell priming, this finding may be related to a better prognosis. Importantly, the proportion of CD8+ T cell infiltration increased from 3.6% to 10%, and the activation level of these CD8+ T cells was upregulated in α-GalCer-treated mice, based on the expression of an early activation marker, CD69, on these cells (Fig. 2). These findings suggest that cytotoxic T lymphocytes might play a significant role as effector cells in this model. The establishment of an antigen-specific T cell response has been suggested in recent reports [4, 5, 21, 22], since α-GalCer-injected mice that had survived an initial tumor-cell challenge rejected tumor growth after a second injection. In the present study, we could not directly confirm the establishment of tumor-specific immunity in vivo by a second inoculation of tumor cells into surviving mice, since all of the mice, including those in the α-GalCer-treated group, died, probably due to the late start of α-GalCer treatment in our model.
An immunohistological analysis of tumor-infiltrating cells has been reported using a liver metastasis model of B16 melanoma in C57BL/6 mice [22], indicated increased T cell infiltration as well as NK cell invasion into tumor nodules. However, this analysis was not quantitative and the functional properties of these TILs remained obscure. We observed a slight increase in IFN-γ production by TILs from α-GalCer-treated mice compared to TILs from control mice (Fig. 4), but this difference was not significant. In the present study, TILs contained crude cell populations and they were used for the assay soon after isolation procedures without an incubation period for the recovery of cell function. Therefore, IFN-γ ELISA might not have been sensitive enough to see a tumor-specific reaction in this assay condition. Further study is needed to determine more detailed functional properties of TILs.
Conclusions
In this study, α-GalCer was shown to activate antitumor immunity, and to enhance NK cell infiltration into tumor nodules. This reagent may also elicit more profound immunity, including acquired immunity, by inducing the infiltration of DC and CD8+T cells into tumor nodules. These findings suggest that this glycolipid antigen may be a promising candidate for the treatment of cancer patients.
Abbreviations
- DC:
-
dendritic cell
- α-GalCer:
-
α-galactosylceramide
- mAb:
-
monoclonal antibody
- CTL:
-
cytotoxic T lymphocyte
- TIL:
-
tumor-infiltrating leukocyte
- HL:
-
hepatic leukocyte
- APC:
-
antigen-presenting cell
- PBMC:
-
peripheral blood mononuclear cell
- PBS:
-
phosphate-buffered saline.
References
Ravikumar TS, Gallos G: Resection of liver metastases: state of the art. Oncology (Huntingt). 2002, 16: 1240-1256.
Saltz LB, Kelsen DP: Adjuvant treatment of colorectal cancer. Annu Rev Med. 1997, 48: 191-202. 10.1146/annurev.med.48.1.191.
Bonetti A: Hepatic artery infusion for liver metastases from colorectal cancer. Lancet. 2003, 361: 358-359. 10.1016/S0140-6736(03)12439-7.
Kobayashi E, Motoki K, Uchida T, Fukushima H, Koezuka Y: KRN7000, a novel immunomodulator, and its antitumor activities. Oncol Res. 1995, 7: 529-534.
Nakagawa R, Motoki K, Ueno H, Iijima R, Nakamura H, Kobayashi E, Shimosaka A, Koezuka Y: Treatment of hepatic metastasis of the colon26 adenocarcinoma with an α-galactosylceramide, KRN7000. Cancer Res. 1998, 58: 1202-1207.
Kawano T, Cui J, Koezuka Y, Toura I, Kaneko Y, Sato H, Kondo E, Harada M, Koseki H, Nakayama T, Tanaka Y, Taniguchi M: Natural Killer-like non-specific tumor cell lysis mediated by specific ligand-activated Vα14NKT cells. Proc Natl Acad Sci USA. 1998, 95: 5690-5693. 10.1073/pnas.95.10.5690.
Burdin N, Brossay L, Koezuka Y, Smiley ST, Grusby MJ, Gui M, Taniguchi M, Hayakawa K, Kronenberg M: Selective ability of mouse CD1 to present glycolipids: α-galactosylceramide specifically stimulates Vα14+NK T lymphocytes. J Immunol. 1998, 161: 3271-3281.
Spada FM, Koezuka Y, Porcelli SA: CD1d-restricted recognition of synthetic glycolipid antigens by human natural killer T cells. J Exp Med. 1998, 188: 1529-1534. 10.1084/jem.188.8.1529.
Kawano T, Cui J, Koezuka Y, Toura I, Kaneko Y, Motoki K, Ueno H, Nakagawa R, Sato H, Kondo E, Koseki H, Taniguchi M: CD1d-restricted and TCR-mediated activation of Vα14 NKT cells by glycosylceramides. Science. 1997, 278: 1626-1629. 10.1126/science.278.5343.1626.
Brossay L, Chioda M, Burdin N, Koezuka Y, Casorati G, Dellabona P, Kronenberg M: CD1d-mediated recognition of an α-galactosylceramide by natural killer T cells is highly conserved through mammalian evolution. J Exp Med. 1998, 188: 1521-1528. 10.1084/jem.188.8.1521.
Hashimoto W, Takeda K, Anzai R, Ogasawara K, Sakihara H, Sugiura K, Seki S, Kumagai K: Cytotoxic NK1.1 Ag+ αβT cells with intermediate TCR induced in the liver of mice by IL-12. J Immunol. 1995, 154: 4333-4340.
Takeda K, Seki S, Ogasawara K, Anzai R, Hashimoto W, Sugiura K, Takahashi M, Sato M, Kumagai K: Liver NK1.1+CD4+ αβT cells activated by IL-12 as a major effector in inhibition of experimental tumor metastasis. J Immunol. 1996, 156: 3366-3373.
Carnaud C, Lee D, Donnars O, Park S-H, Beavis A, Koezuka Y, Bendelac A: Cross-talk between cells of the innate immune system: NKT cells rapidly activates NK cells. J Immunol. 1999, 163: 4647-4650.
Trobonjaca Z, Kroger A, Stober D, Leithauser F, Moller P, Hauser H, Schirmbeck R, Reimann J: Activating immunity in the liver. II. IFN-beta attenuates NK cell-dependent liver injury triggered by liver NKT cell activation. J Immunol. 2002, 168: 3763-3770.
Hayakawa Y, Takeda K, Yagita H, Kakuta S, Iwakura Y, Van Kaer L, Saiki I, Okumura K: Critical contribution of IFN-gamma and NK cells, but not perforin-mediated cytotoxicity, to anti-metastatic effect of alpha-galactosylceramide. Eur J Immunol. 2001, 31: 1720-1727. 10.1002/1521-4141(200106)31:6<1720::AID-IMMU1720>3.3.CO;2-L.
Ishihara S, Nieda M, Kitayama J, Osada T, Yabe T, Kikuchi A, Koezuka Y, Porcelli SA, Tadokoro K, Nagawa H, Juji T: Alpha-glycosylceramides enhance the antitumor cytotoxicity of hepatic lymphocytes obtained from cancer patients by activating CD3-CD56+ NK cells in vitro. J Immunol. 2000, 165: 1659-1664.
Eberl G, MacDonald HR: Selective induction of NK cell proliferation and cytotoxicity by activated NKT cells. Eur J Immunol. 2000, 30: 985-992. 10.1002/(SICI)1521-4141(200004)30:4<985::AID-IMMU985>3.0.CO;2-E.
Smyth MJ, Crowe NY, Pellicci DG, Kyparissoudis K, Kelly JM, Takeda K, Yagita H, Godfrey DI: Sequential production of IFN-γ by NKT cells and NK cells is essential for the anti-metastatic effect of α-galactosylceramide. Blood. 2002, 99: 1259-66. 10.1182/blood.V99.4.1259.
Takeda K, Hayakawa Y, Atsuta M, Hong S, Van Kaer L, Kobayashi K, Ito M, Yagita H, Okumura K: Relative contribution of NK and NKT cells to the anti-metastatic activities of IL-12. Int Immunol. 2000, 12: 909-914. 10.1093/intimm/12.6.909.
Smyth MJ, Thia KY, Street SE, Cretney E, Trapani JA, Taniguchi M, Kawano T, Pelikan SB, Crowe NY, Godfrey DI: Differential tumor surveillance by natural killer (NK) and NKT cells. J Exp Med. 2000, 191: 661-668. 10.1084/jem.191.4.661.
Nishimura T, Kitamura H, Iwakabe K, Yahata T, Ohta A, Sato M, Takeda K, Okumura K, Van Kaer L, Kawano T, Taniguchi M, Nakui M, Sekimoto M, Koda T: The interface between innate and acquired immunity: glycolipid antigen presentation by CD1d-expressing dendritic cells to NKT cells induces the differentiation of antigen-specific cytotoxic T lymphocytes. Int Immunol. 2000, 12: 987-94. 10.1093/intimm/12.7.987.
Nakagawa R, Serizawa I, Motoki K, Sato M, Ueno H, Iijima R, Nakamura H, Shimosaka A, Koezuka Y: Antitumor activity of α-Galactosylceramide, KRN7000, in mice with the melanoma B16 hepatic metastasis and immunohistological study of tumor infiltrating cells. Oncol Res. 2000, 12: 51-58.
Gong J, Chen D, Kashiwaba M, Kufe D: Induction of antitumor activity by immunization with fusions of dendritic and carcinoma cells. Nat Med. 1997, 3: 558-561.
Bendelac A, Rivera MN, Park S-H, Roark JH: Mouse CD1-specific NK1 T cells: development, specificity, and function. Annu Rev Immunol. 1997, 15: 535-562. 10.1146/annurev.immunol.15.1.535.
Hammond KJ, Pellicci DG, Poulton LD, Naidenko OV, Scalzo AA, Baxter AG, Godfrey DI: CD1d-restricted NKT cells: an interstrain comparison. J Immunol. 2001, 167: 1164-1173.
Moodycliffe AM, Maiti S, Ullrich SE: Splenic NK1.1-negative, TCRαβ intermediate CD4+ T cells exist in naive NK1.1 allelic positive and negative mice, with the capacity to rapidly secrete large amounts of IL-4 and IFN-γ upon primary TCR stimulation. J Immunol. 1999, 162: 5156-5163.
Ortaldo JR, Winkler-Pickett R, Mason AT, Mason LH: The Ly-49 families: regulation of cytotoxicity and cytokine production in murine CD3+ cells. J Immunol. 1998, 160: 1158-1165.
Kronenberg M, Gapin L: The unconventional lifestyle of NKT cells. Nat Rev Immunol. 2002, 2: 557-568.
Coventry BJ, Morton J: CD1a-positive infiltrating-dendritic cell density and 5-year survival from human breast cancer. Br J Cancer. 2003, 89: 533-538. 10.1038/sj.bjc.6601114.
Zeid NA, Muller HK: S100 positive dendritic cells in human lung tumors associated with cell differentiation and enhanced survival. Pathology. 1993, 25: 338-343.
Acknowledgements
This work was supported by a Grant-in-Aid for Cancer Research (No.11671152) from the Ministry of Education, Science, Culture and Sports of Japan.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contributions
TO conceived of the study and carried out murine in vivo experiments and flow cytometry assays. HK performed statistical analysis and participated in the design of the study. YS participated in the design of the study and in flow cytometry analysis.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Osada, T., Nagawa, H. & Shibata, Y. Tumor-infiltrating effector cells of α-galactosylceramide-induced antitumor immunity in metastatic liver tumor. J Immune Based Ther Vaccines 2, 7 (2004). https://doi.org/10.1186/1476-8518-2-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1476-8518-2-7