Abstract
Background
There are many reports about the anti-arrhythmic effects of ω-3 polyunsaturated fatty acids, however, the mechanisms are still not completely delineated. The purpose of this study was to investigate the characteristics of action potentials and transient outward potassium currents (Ito) of Sprague-Dawley rat ventricular myocytes and the effects of docosahexaenoic acid (DHA) on action potentials and Ito.
Methods
The calcium-tolerant rat ventricular myocytes were isolated by enzyme digestion. Action potentials and Ito of epicardial, mid-cardial and endocardial ventricular myocytes were recorded by whole-cell patch clamp technique.
Results
1. Action potential durations (APDs) were prolonged from epicardial to endocardial ventricular myocytes (P < 0.05). 2. Ito current densities were decreased from epicardial to endocardial ventricular myocytes, which were 59.50 ± 15.99 pA/pF, 29.15 ± 5.53 pA/pF, and 12.29 ± 3.62 pA/pF, respectively at +70 mV test potential (P < 0.05). 3. APDs were gradually prolonged with the increase of DHA concentrations from 1 μmol/L to 100 μmol/L, however, APDs changes were not significant as DHA concentrations were in the range of 0 μmol/L to 1 μmol/L. 4. Ito currents were gradually reduced with the increase of DHA concentrations from 1 μmol/L to 100 μmol/L, and its half-inhibited concentration was 5.3 μmol/L. The results showed that there were regional differences in the distribution of action potentials and Ito in rat epicardial, mid-cardial and endocardial ventricular myocytes. APDs were prolonged and Ito current densities were gradually reduced with the increase of DHA concentrations.
Conclusion
The anti-arrhythmia mechanisms of DHA are complex, however, the effects of DHA on action potentials and Ito may be one of the important causes.
Similar content being viewed by others
Background
Fatty acids, especially polyunsaturated fatty acids (PUFAs), play an important role in life and death of cardiac cells. Reasons are as follow: 1. they are essential fuels for mechanical, electrical, and synthetic activities of the heart; 2. their levels are abnormally high in an ischemia followed by a reperfusion; and 3. dietary fish oil is apparently beneficial for heart function [1, 2]. Therefore, the beneficial effects of PUFAs on cardiovascular diseases, such as fish oil, have been reported, and the effects of PUFAs on anti-arrhythmias and prevention of sudden death have been highlights [3–6]. It has been reported that PUFAs have the roles of anti-arrhythmias and prevention of malignant ventricular arrhythmias, however, the mechanisms of which are still not completely delineated [7, 8].
ω-3 PUFAs mainly include docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA). More attentions have been paid to their beneficial effects on cardiovascular diseases in recent years, especially in their anti-arrhythmias and prevention of sudden cardiac death [9–13]. However, most of these studies are clinical trials, and the mechanisms of which are still not completely known. To investigate the mechanisms of ω-3 PUFAs on anti-arrhythmias and prevention of sudden cardiac death [1, 8], we observed the effects of DHA on action potentials and transient outward potassium currents (Ito) of Sprague-Dawley rat ventricular myocytes by whole-cell patch clamp technique in this study. The results may provide some experimental evidences for rational applications of ω-3 PUFAs to prevent and treat arrhythmias in clinical practice.
Methods
Major experimental instruments
The instruments used were: MultiClamp 700B patch clamp amplifier (Axon Instruments, USA), D/A and A/D converter (DigiData 1322, Axon Instruments, USA), Pclamp 9.0 pulse software (Axon Instruments, USA), MP-285 motorized micromanipulator (Sutter Instruments, USA), IX71 inverted microscope (Olympus, Japan), SA-OLY/2 and DH-35 culture dish heater (Warner Instruments, USA), P-97 micropipette puller (Sutter Instruments, USA).
Reagents, solutions and drugs
The reagents, solutions and drugs used were: DHA (Sigma, USA), molecular weight 328.5, 100 mmol/L stock solution was prepared by being dissolved in absolute ethanol and protected from light in refrigerator at -20°C. The experimental concentration of DHA was obtained by dilution of stock solution before each experiment. Action potential internal solution (in mmol/L) was KCl 120, CaCl2 1, MgCl2 5, Na2 ATP 5, EGTA 11, HEPES 10, glucose 11, pH 7.3 adjusted with KOH. Action potential external solution was Tyrode's solution [14]. Ito external solution (in mmol/L) was NaCl 140, KCl 4, CaCl2 1.5, MgCl2 1, CdCl2 0.5, HEPES 5, glucose 10, pH 7.4 adjusted with NaOH. Ito internal solution (in mmol/L) was KCl 140, MgCl2 1, K2 ATP 5, EGTA 5, HEPES 10, pH 7.4 adjusted with KOH. KB solution (in mmol/L) was L-Glutamic acid 50, KCl 40, KH2PO4 20, Taurine 20, MgCl2 3, KOH 70, EGTA 0.5, HEPES 10, glucose 10, pH 7.4 adjusted with KOH.
Cell isolation
The investigation was approved by our institute ethics committee and conformed to the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH publication No. 85-23, revised 1996). Healthy Sprague-Dawley rats of either sex, aged 8-12 weeks and weighing approximately 200 g, were provided by the Experimental Animal Center of Soochow University (Suzhou, China). Animals were anesthetized with pentobarbital sodium intraperitoneally (i.p.), Hearts were removed and retrograde perfusion through the aorta was performed as described [15]. After retrograde perfusion was finished, epicardial, mid-cardial, and endocardial ventricular myocardium were obtained respectively by cutting with eye scissor and plyer. Isolated cells were kept at room temperature in KB solution and used within 6 hr; only relaxed, striated, and rod-shaped cells were used.
Recordings of action potentials and Ito with and without DHA
Currents in whole-cell voltage clamp configuration were recorded following the method of Hamill et al [16]. Myocytes were transferred to a 1 ml chamber (DH-35 culture dish heater, Warner Instruments, USA) containing external solution placed on the stage of an inverted microscope. The chamber was continuously perfused at a rate of 1-2 ml/min with external solution. Electrodes were prepared from borosilicate glass (Clark Instruments, UK) using P-97 micropipette puller with resistances typically between 2 and 4 MΩ when filled with internal solution. Whole-cell voltage-clamp experiments were performed with MultiClamp 700B amplifier. Whole-cell capacitance and series resistance were compensated by 60-80%. Experiments were performed at 36-37°C. Voltage clamp pulses were generated via an IBM-compatible computer connected to Digidata 1322. Data acquisition and analyses were performed using pCLAMP software. To obtain action potentials, 5 ms depolarizing pulse with 900pA, 1 Hz in current-clamp configuration was applied. DHA at 0.01 μmol/L, 0.1 μmol/L, 1 μmol/L, 10 μmol/L, and 100 μmol/L was perfused for 10 min respectively to observe the influence on action potential durations (APDs). To obtain Ito, 600 ms depolarizing pulses in the range -40 mV to +70 mV were applied to the ventricular myocytes every 5 s in +10 mV increment from -40 mV holding potential (HP). Recordings of action potentials and Ito were performed at physiological temperature range (36-37°C). DHA at various concentrations was applied to investigate the effects on Ito.
Statistical analysis
Continuous variables were expressed as mean ± standard error ( ± se). SPSS11.5 (SPSS Inc, Chicago, Illinois, USA) was used for statistical analysis. Comparisons among groups were performed by repeated measurement analysis of variance (ANOVA) and least-significant difference contrast. Control and drug data for individual groups were compared by Paired t-test. P ≤ 0.05 was considered significant. OriginPro 7.5 software (OriginLab, USA) was utilized to calculate the half-inhibited concentration (IC50).
± se). SPSS11.5 (SPSS Inc, Chicago, Illinois, USA) was used for statistical analysis. Comparisons among groups were performed by repeated measurement analysis of variance (ANOVA) and least-significant difference contrast. Control and drug data for individual groups were compared by Paired t-test. P ≤ 0.05 was considered significant. OriginPro 7.5 software (OriginLab, USA) was utilized to calculate the half-inhibited concentration (IC50).
Results
Characteristics of action potentials and Ito of rat ventricular myocytes
Action potentials of epicardial, mid-cardial and endocardial ventricular myocytes were recorded respectively with action potential stimulus protocol. The action potential morphologies were different in epicardial, mid-cardial and endocardial ventricular myocytes (Figure 1). APD25, APD50, and APD90 were gradually prolonged from epicardial to endocardial ventricular myocytes. Table 1 showed APDs' variations in myocytes of different layers; however, maximal velocity of action potential depolarization (Vmax), amplitude (APA), and overshoot (OS), didn't have remarkable changes in epicardial, mid-cardial and endocardial ventricular myocytes (Table 2).
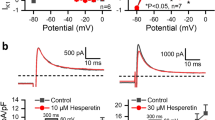
Ito current tracings at various test potentials were elicited by 600 ms depolarization in the range of -40 mV to +70 mV pulses applied to the ventricular myocytes every 5 s in +10 mV increments from -40 mV HP. The representative current tracings were shown in figure 2. The current densities of epicardial, mid-cardial and endocardial ventricular myocytes at +70 mV were 59.50 ± 15.99 pA/pF, 29.15 ± 5.53 pA/pF, and 12.29 ± 3.62 pA/pF, respectively.
The representative current tracings of transient outward potassium currents at various test potentials: Currents were elicited by 600 ms depolarizing in the range of -40 mV to +70 mV pulses in +10 mV increments from -40 mV holding potential. The currents were enhanced with the increase of test potentials, activated rapidly and inactivated slowly.
The current-voltage curves of Ito were plotted with current densities at each test potential (Figure 3). The threshold potential of Ito channel opening was -30.3 ± 2.8 mV, i.e., Ito channel began to activate at more than -30 mV. Ito currents were gradually enhanced with the increase of test potentials. The activation of Ito channel was very rapid, and only needed to about 10 ms, nonetheless, its inactivation was relatively slow. The time constants of epicardial, mid-cardial, and endocardial ventricular myocytes were almost the same at each test potential. They were 31.8 ± 1.7 ms, 32.9 ± 2.4 ms, and 33.2 ± 2.9 ms, respectively, at +70 mV test potential (P > 0.05).
The current-voltage curves of transient outward potassium currents in epicardial, mid-cardial and endocardial ventricular myocytes: Currents in epicardial, mid-cardial and endocardial ventricular myocytes were all enhanced with the increase of test potentials from -40 mV to +70 mV, whereas currents in epicardial were higher than those in mid-cardial and endocardial at the same test potential, and currents in mid-cardial were larger than those in endocardial.
Effects of DHA on action potentials
DHA at 0.01 μmol/L, 0.1 μmol/L, 1 μmol/L, 10 μmol/L, and 100 μmol/L was applied on epicardial ventricular myocytes, respectively. The results showed that: ① APDs were gradually prolonged with the increase of DHA, whereas APDs' changes were not significant at low concentration of DHA (<1 μmol/L). The prolongation of APD25, APD50, and APD90 was less than 15% compared with the control (0 min) when 0.1 μmol/L DHA was applied (Figure 4). ② APDs were prolonged in a concentration-dependent manner when DHA concentrations were more than 1 μmol/L. APD25, APD50, and APD90 were 7.7 ± 2.0 ms, 21.2 ± 3.5 ms, and 100.1 ± 9.8 ms respectively when 10 μmol/L DHA was used at 5 min (Figure 5C). APD25, APD50, and APD90 were 15.2 ± 4.0 ms, 45.7 ± 6.8 ms, and 215.6 ± 15.7 ms respectively when 100 μmol/L DHA was utilized at 5 min (Figure 5D), which was significantly prolonged compared with those without addition of DHA (P < 0.05).
Action potential changes of rat ventricular myocytes at 0.1 μmol/L DHA: A, B, and C were morphologies of action potential when 0.1 μmol/L DHA was applied at 0 min, 1 min, and 5 min, respectively. The action potential duration was increased; however, compared with the control (0 min), the prolongation of action potential duration was less than 15%.
Action potential changes of rat ventricular myocytes at different DHA concentrations: A, B, and C were the applications of 10 μmol/L DHA at 0 min, 1 min, and 5 min. D was DHA at concentration of 100 μmol/L for 5 min. Action potential durations were significantly prolonged in concentration-dependent manner when DHA concentrations were more than 10 μmol/L.
Effects of DHA on Ito
DHA at 0.01 μmol/L, 0.1 μmol/L, 1 μmol/L, 10 μmol/L, and 100 μmol/L was applied, respectively. Ito currents were blocked by DHA in a concentration-dependent manner. Currents were gradually decreased with the increase of DHA concentrations. The current density of Ito at +70 mV was 30.1 ± 7.2 pA/pF with DHA at 100 μmol/L. The representative current tracings blocked by DHA at 100 μmol/L were shown in figures 6. IC50 of DHA on Ito was fitted with Hill function and calculated by OriginPro 7.5 software, which was 5.3 μmol/L.
Alterations of transient outward potassium currents after DHA at 100 μmol/L was applied: A, B, C, D, and E were representative transient outward potassium current tracings with DHA at 0 min, 1 min, 5 min, 10 min, and 15 min, respectively. Transient outward potassium currents were remarkably blocked by DHA.
Discussion
The typical action potential consists of 5 phases or stages, i.e., 0, 1, 2, 3, and 4. The present study has showed that the rat ventricular myocytes don't have the typical action potential morphology. APDs are the shortest in epicardial ventricular myocytes, and repolarization rapidly appears after depolarization, showing no platform phase [17]. The phenomenon of "spike and dome" [18] sometimes can be seen, however, this phenomenon does not appear in endocardial ventricular myocytes. Action potential repolarization in endocardial ventricular myocytes is slow, showing relative standard action potential morphology. The action potential morphologies of mid-cardial ventricular myocytes are between epicardial and endocardial ventricular myocytes [19, 20], but action potential repolarization is still rapid, and has the tendency of platform phase compared with the epicardial ventricular myocytes. The reasons why these alterations appear are that there are regional differences of Ito in epicardial, mid-cardial and endocardial ventricular myocytes. The Ito channels are the most abundant in rat epicardial ventricular myocytes and then in mid-cardial and endocardial ventricular myocytes by turns. The Ito current densities in epicardial, mid-cardial and endocardial ventricular myocytes were different in this study, which further illustrates that Ito channels of rat ventricular myocytes have regional differences. Ito channels in epicardial myocytes are extremely abundant, and therefore, Ito currents are the largest, which makes action potential repolarization rapid, calcium inflow time and APDs short. In contrast, Ito channels in endocardial myocytes are few or lack, and therefore, APDs prolong. APA, Vmax, and OS are formed mainly by 0 phase depolarization. Because regional differences of Ito channels do not affect depolarization of ventricular myocytes, and thus, APA, Vmax, and OS don't have significant differences in epicardial, mid-cardial and endocardial myocytes [21].
The Ca2+-insensitive but 4-aminopyridine-sensitive Ito currents play a major role in modulating cardiac electrical activity [22]. It underlies phase 1 repolarization, and thus, by setting the voltage of the early plateau phase, it influences activation and inactivation of other plateau currents that control repolarization. It has also been reported in several studies that Ito channels are potentially important targets for both neuromodulatory control [23] and antiarrhythmic drug actions [24]. These currents have been suggested to contribute significantly to the regional electrophysiological heterogeneity within the ventricular wall, a fact considered to be responsible for T-wave polarity. The heterogeneous distribution of Ito thus appears to be essential in causing the transmural electrical gradients necessary for proper repolarization of cardiac action potentials. It is expected that changes in Ito distribution and availability can be expressed in the ECG by typical J-wave and T-wave alterations and may lead to cardiac arrhythmias during evolving heart diseases.
The present study results have showed that there are regional differences of action potentials and Ito amplitude and morphology of rat epicardial, mid-cardial and endocardial myocytes. Regional differences of action potentials and Ito should be considered when rats are chosen as the experimental animal. We should try to obtain same regional ventricular myocytes to avoid experiment errors when we perform cellular electrophysiological study. Consequently, in this study, we only chose epicardial myocytes to investigate the effects of DHA on action potentials and Ito.
ω-3 PUFAs mainly include DHA and EPA. In order to investigate the mechanisms of ω-3 PUFAs on anti-arrhythmias and prevention of sudden death, we performed this experiment to study the effects of DHA on action potential and Ito of rat ventricular myocytes. The reasons that we chose the rats as experimental animal is not only because the rats have many advantages, e.g. cheap, strong vitality, and easily bred, but more important is that there are many similar electrophysiological characteristics of rat and the human being's cardiomyocytes [25, 26].
After DHA at various concentrations was applied, APDs were gradually prolonged and Ito currents were decreased by degrees with the increase of DHA concentrations. DHA could inhibit Ito currents, prolong APDs, and extend effective refractory period of myocardial myocytes [27]. The effects of DHA on action potentials and Ito may be one of its anti-arrhythmia mechanisms.
Figure 6 clearly showed that DHA could inhibit Ito currents. However, from the morphologic changes of action potentials in figure 5, we found that the morphologic changes of action potentials mainly appeared in phase 2 and phase 3 with the increase of DHA concentrations. In contrast, action potential phase 1 formed mainly by Ito current efflux didn't have significant changes. This means DHA may have the effects on other ion currents in addition to Ito current.
The present study has some limitations, e.g., we only investigated the effects of DHA on action potentials and Ito of rat ventricular myocytes. On the other hand, ω-3 PUFAs not only include DHA but also EPA, the electrophysiological effects of EPA on rat ventricular myocytes, and DHA on other ion currents such as INa, ICa-L, IK, and IK1 are still needed to further study. Only we completely explore the anti-arrhythmia mechanisms of ω-3 PUFAs, we can apply them correctly in clinical practice to prevent and treat cardiovascular diseases [28–32].
Conclusion
In summary, the present findings obtained by the patch-clamp technique have clearly shown that APDs are prolonged, and Ito currents are gradually reduced with the increase of DHA concentrations. Effects of DHA on action potentials and Ito may be one of the important causes of anti-arrhythmias.
References
Lavie CJ, Milani RV, Mehra MR, Ventura HO: Omega-3 polyunsaturated fatty acids and cardiovascular diseases. J Am Coll Cardiol. 2009, 54: 585-94. 10.1016/j.jacc.2009.02.084
Crumb JR, Munfakh N, Heck HA, Harrison LH: Fatty acid block of the transient outward current in adult human atrium. J Pharmacol Exp Ther. 1999, 289: 386-91.
Wilhelm M, Tobias R, Asskali F, Kraehner R, Kuly S, Klinghammer L, Boehles H, Daniel WG: Red blood cell omega-3 fatty acids and the risk of ventricular arrhythmias in patients with heart failure. Am Heart J. 2008, 155: 971-7. 10.1016/j.ahj.2007.11.045
Arshad A, Mandava A, Kamath G, Musat D: Sudden cardiac death and the role of medical therapy. Prog Cardiovasc Dis. 2008, 50: 420-38. 10.1016/j.pcad.2007.12.003
Anand RG, Alkadri M, Lavie CJ, Milani RV: The role of fish oil in arrhythmia prevention. J Cardiopulm Rehabil Prev. 2008, 28: 92-8.
Metcalf RG, Sanders P, James MJ, Cleland LG, Young GD: Effect of dietary n-3 polyunsaturated fatty acids on the inducibility of ventricular tachycardia in patients with ischemic cardiomyopathy. Am J Cardiol. 2008, 101: 758-61. 10.1016/j.amjcard.2007.11.007
Von Schacky C: Omega-3 fatty acids: antiarrhythmic, proarrhythmic or both?. Curr Opin Clin Nutr Metab Care. 2008, 11: 94-9. 10.1097/MCO.0b013e3282f44bdf
He K: Fish, long-chain omega-3 polyunsaturated fatty acids and prevention of cardiovascular disease--eat fish or take fish oil supplement?. Prog Cardiovasc Dis. 2009, 52: 95-114. 10.1016/j.pcad.2009.06.003
Smith CE, Freeman LM, Rush JE, Cunningham SM, Biourge V: Omega-3 fatty acids in Boxer dogs with arrhythmogenic right ventricular cardiomyopathy. J Vet Intern Med. 2007, 21: 265-73.
Leaf A: Omega-3 fatty acids and prevention of arrhythmias. Curr Opin Lipidol. 2007, 18: 31-4. 10.1097/MOL.0b013e328012d61b
Leaf A: Prevention of sudden cardiac death by n-3 polyunsaturated fatty acids. Fundam Clin Pharmacol. 2006, 20: 525-38. 10.1111/j.1472-8206.2006.00438.x
Von Schacky C, Harris WS: Cardiovascular benefits of omega-3 fatty acids. Cardiovasc Res. 2007, 73: 310-5. 10.1016/j.cardiores.2006.08.019
Kottke TE, La Wu, Brekke LN, Brekke MJ, White RD: Preventing sudden death with n-3 (omega-3) fatty acids and defibrillators. Am J Prev Med. 2006, 31: 316-23. 10.1016/j.amepre.2006.06.006
Yazawa K, Kaibara M, Ohara M, Kameyama M: An improved method for isolating cardiac myocytes useful for patch-clamp studies. Jap J Physiol. 1990, 40: 157-63. 10.2170/jjphysiol.40.157.
Tytgat J: How to isolate cardiac myocytes. Cardiovasc Res. 1994, 28: 280-3. 10.1093/cvr/28.2.280
Hamill OP, Marty A, Nether E, Sakmann B, Sigworth FJ: Improved patch-clamp techniques for high-resolution current recording from cells and cell-free membrane patches. Pflugers Arch. 1981, 391: 85-100. 10.1007/BF00656997
Shigematsu S, Kiyosue T, Sato T, Arita M: Rate-dependent prolongation of action potential duration in isolated rat ventricular myocytes. Basic Res Cardiol. 1997, 92: 123-8. 10.1007/BF00788629
Hulme JT, Orchard CH: Effect of acidosis on transient outward potassium current in isolated rat ventricular myocytes. Am J Physiol Heart Circ Physiol. 2000, 278: 50-9.
Stilli D, Berni R, Bocchi L, Zaniboni M, Cacciani F, Sgoifo A, Musso E: Vulnerability to ventricular arrhythmias and heterogeneity of action potential duration in normal rats. Exp Physiol. 2004, 89: 387-96. 10.1113/expphysiol.2003.027110
Fauconnier J, Bedut S, Le Guennec JY, Babuty D, Richard S: Ca2+ current-mediated regulation of action potential by pacing rate in rat ventricular myocytes. Cardiovasc Res. 2003, 57: 670-80. 10.1016/S0008-6363(02)00731-9
Orta-Salazar G, Bouchard RA, Morales-Salgado F, Salinas-Stefanon EM: Inhibition of cardiac Na+ current by primaquine. Br J Pharmacol. 2002, 135: 751-63. 10.1038/sj.bjp.0704460
Antzelevitch C, Sicouri S, Litovsky SH, Lukas A, Krishnan SC, Di Diego JM, Gintant GA, Liu DW: Heterogeneity within the ventricular wall: electrophysiology and pharmacology of epicardial, endocardial, and M cells. Circ Res. 1991, 69: 1427-49.
Fedida D, Braun AP, Giles WR: α1-Adrenoceptors in myocardium: functional aspects and transmembrane signaling mechanisms. Physiol Rev. 1993, 73: 469-87.
Duan D, Fermini B, Nattel S: Potassium channel blocking properties of propafenone in rabbit atrial myocytes. J Pharmacol Exp Ther. 1993, 264: 1113-23.
He JY, Kargacin ME, Kargacin GJ, Ward CA: Tamoxifen inhibits Na+ and K+ currents in rat ventricular myocytes. Am J Physiol Heart Circ Physiol. 2003, 285: 661-8.
Bryant SM, Shipsey SJ, Hart G: Normal regional distribution of membrane current density in rat left ventricle is altered in catecholamine-induced hypertrophy. Cardiovasc Res. 1999, 42: 391-401. 10.1016/S0008-6363(99)00033-4
Adamantidis MM: Mechanisms of action of class III antiarrhythmia agents. Arch Des Maladies du Coeur et des Vaisseaux. 1995, 88: 33-40.
Xiao YF, Sigg DC, Ujhelyi MR, Wilhelm JJ, Richardson ES, Iaizzo PA: Pericardial delivery of omega-3 fatty acid: A novel approach to reducing myocardial infarct sizes and arrhythmias. Am J Physiol Heart Circ Physiol. 2008, 294: H1144-52. 10.1152/ajpheart.91502.2007.
Den Ruijter HM, Berecki G, Verkerk AO, Bakker D, Baartscheer A, Schumacher CA, Belterman CN, de Jonge N, Fiolet JW, Brouwer IA, Coronel R: Acute administration of fish oil inhibits triggered activity in isolated myocytes from rabbits and patients with heart failure. Circulation. 2008, 117: 536-44. 10.1161/CIRCULATIONAHA.107.733329
Reiner E, Tedeschi-Reiner E, Stajminger G: The role of omega-3 fatty acids from fish in prevention of cardiovascular diseases. Lijec Vjesn. 2007, 129: 350-5.
Jacobson TA: Beyond lipids: the role of omega-3 fatty acids from fish oil in the prevention of coronary heart disease. Curr Atheroscler Rep. 2007, 9: 145-53. 10.1007/s11883-007-0011-x
Farzaneh-Far R, Lin J, Epel ES, Harris WS, Blackburn EH, Whooley MA: Association of marine omega-3 fatty acid levels with telomeric aging in patients with coronary heart disease. JAMA. 2010, 303: 250-7. 10.1001/jama.2009.2008
Acknowledgements
This work was supported, in part, by a grant (CS20010015) from Wuxi Science and Technology Bureau of Jiangsu Province, China. The authors thank Miss Hong-xia Li and Miss Lian-hua Han for their assistance in the preparations of this paper.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
XRL, XJY, and WPP designed research and revised the manuscript; RXW, LPS, SXG, and ZYY performed research; RXW wrote the manuscript; RXW and TG analyzed data. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Wang, Rx., Li, Xr., Guo, T. et al. Docosahexaenoic acid has influence on action potentials and transient outward potassium currents of ventricular myocytes. Lipids Health Dis 9, 39 (2010). https://doi.org/10.1186/1476-511X-9-39
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1476-511X-9-39