Abstract
Background
Community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA) is a serious pathogen in several regions in the United States. It is unclear which populations are at high risk for the emergence of these strains.
Methods
All unique patient isolates of S. aureus were collected from hospitals in Brooklyn, NY over a three-month period. Isolates of MRSA that were susceptible to clindamycin underwent SCCmec typing. Isolates with the SCCmec type IV (characteristic of CA-MRSA strains) underwent ribotyping. Demographic information involving the neighborhoods of Brooklyn was also gathered and correlated with the prevalence of CA-MRSA strains.
Results
Of 1316 isolates collected during the surveillance, 217 were MRSA susceptible to clindamycin. A total of 125 isolates possessed SCCmec type IV; 72 belonged to the USA300 strain and five belonged to the USA400 strain. Hospitals in the eastern part of the city had the highest prevalence of USA300 strain. Individuals in the eastern region, when compared to the western region, were more likely to be Black, Hispanic, female, and < 18 years of age, and to have households of ≥ 3 persons. In addition, the median household income was lower, and the proportion of individuals on public assistance was higher, for the population in the eastern region.
Conclusion
The USA300 strain of CA-MRSA is emerging in New York City. In this population-based study, urban regions of lower socioeconomic status and with evidence of overcrowding appear to be at higher risk for the emergence of this pathogen.
Similar content being viewed by others
Background
Community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA) has emerged as a frequent and serious pathogen in several regions in the United States. The CA-MRSA strains have distinctive phenotypic and genotypic features when compared to typical hospital-acquired strains. Most CA-MRSA remain susceptible to other non-β-lactam antibiotics [1–4]. CA-MRSA strains typically possess type IV SCCmec gene and the Panton-Valentine leukocidin (PVL)[1, 4, 5]. Two distinctive pulsed field gel electrophoresis types of CA-MRSA have predominated in the United States [1]. The USA400 type was isolated from children in the Midwestern United States, and has been associated with nosocomial infections in neonates and post-partum women [6–8]. The USA300 type has been associated with outbreaks in prisons and sports teams, and has become the predominant type in certain regions in the United States [2, 9, 10].
Prior to the emergence of the USA 300/400 strains, most patients with community-onset MRSA infections had identifiable risk factors, including recent hospitalization or nursing home residence, invasive/percutaneous procedure, and/or chronic dialysis therapy [11–13]. However, initial reports have noted patients with USA300/400 strains have not possessed these risk factors; risk factors for infection with these strains remain poorly defined.
Most reports of CA-MRSA have examined outbreak situations; relatively few studies have performed population-based analyses [14]. In this report, we examine the prevalence of CA-MRSA in Brooklyn, NY and examine characteristics of urban neighborhoods identified with a higher prevalence.
Materials and methods
Surveillance study
From December 2005 through February 2006, all single patient isolates of S. aureus were gathered from 15 of the 16 hospitals in Brooklyn, NY; the Department of Veterans Affairs Medical Center, which serves select patients from throughout the city, was not included in the study. Bacterial isolates were identified by the participating microbiology laboratories according to standard techniques. Susceptibility testing was performed in the central research laboratory by the agar or broth (for tigecycline and daptomycin) dilution methods, according to CLSI standards [15].
Characterization of bacterial isolates
Since susceptibility to clindamycin and possession of SCCmec IV are typical features of the USA 300/400 strains, all MRSA isolates gathered in the surveillance study that were susceptible to clindamycin underwent initial mec typing according to the methods of Oliveira et al [16]. Isolates that were nontypeable or found to possess a SCCmec IV underwent further mec characterization according to the multiplex assay of Zhang et al [17]. Selected isolates also underwent ribotyping, pulsed field gel electrophoresis, and PCR screening for the genes encoding PVL, as previously described [1, 8].
Population-based analysis
Data concerning the city of Brooklyn, and the 72 neighborhoods that comprise the city, were obtained using the Infoshare Community Data System (Community Studies of New York, Inc). Demographic, income, and health data were recorded for each of the neighborhoods. The information in this database largely reflects the year 2000 census records. The 72 Brooklyn neighborhoods were assigned, based on location, to one of the 15 hospitals as the primary medical center delivering care to the neighborhood.
A retrospective chart review was conducted on selected patients; information collected included demographic data (including home address), record of recent hospitalization, clinical status on presentation, and clinical outcome (survival).
Statistical analysis included chi square analysis for categorical data and student's t-test for continuous variables.
This study has been approved by the Institutional Review Board at SUNY- Downstate Medical Center.
Results
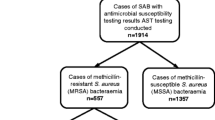
A total of 1316 isolates of S. aureus were collected during the three-month surveillance study; 581 (44%) were found to be MRSA (Table 1). Of the MRSA isolates, 217 (37%) were susceptible to clindamycin. SCCmec type IV was found in 125 (58%) of these isolates (123 with type IVa and two with type IVb). One isolate possessed SCCmec type I, 47 possessed type II, and 44 were unable to be typed. Seventy-five (60%) of the isolates with SCCmec type IV carried the genes for PVL. Ribotyping was performed on 120 of the 125 (96%) isolates with SCCmec type IV, and 72 (58%) belonged to the USA300 strain. PVL genes were identified in 81% of the USA300 isolates. Only 5 (4%) isolates belonged to the USA400 strain. The remaining 48 isolates belonged to 12 different ribogroups.
Fingerprinting by pulsed field gel electrophoresis correlated well with the ribotyping results. Representative isolates belonging to the same ribogroup as USA300 also had the same pulsed field type (Fig. 1). To assess if bacteria with a nontypeable SCCmec were unrecognized strains related to either USA300 or USA400 types, seven nontypeable isolates underwent pulsed field gel electrophoresis. None of these isolates were closely related to the two CA-MRSA strains (Fig. 1).
Pulsed field gel electrophoresis results for selected MRSA isolates. Lanes 1–7: clinical isolates belonging to the same ribotype as USA300. Lane 8: Clinical isolate belonging to the same ribotype as USA400. Lane 9: representative USA400 strain. Lane 10: lamda ladder. Lane 11: representative USA300 isolate. Lanes 12–16: isolates with nontypeable SCCmec.
The 72 isolates belonging to the USA300 type were examined in further detail. Forty-six isolates originated from wound/soft tissue cultures, seven were from respiratory specimens, seven were from blood cultures and 12 cultures were from miscellaneous or unidentified sources. Fifty-one of the 72 (71%) isolates originated from patients from six hospitals; however, these hospitals supplied 49% of all S. aureus isolates (P < 0.001). The USA300 strains accounted for 7.9% (range, 6.7–9.2%) of the S. aureus isolates collected from these six hospitals. In contrast, the USA300 strains accounted for 3.1% (range 0–5.0%) of the S. aureus isolated from the remaining nine hospitals.
The six hospitals with the greater prevalence of USA300 strains all serve neighborhoods located in the eastern section of the city, while the nine remaining hospitals serve neighborhoods in the western half of the city (Fig. 2). During the surveillance period, there were 4.6 cases/100,000 in the high prevalence region, compared to 1.6 cases/100,000 in the lower region. The populations comprising these two regions displayed markedly different characteristics (Table 2). The population in the high prevalence region was more likely to be Black and Hispanic, female, and less than 18 years of age. Residents in the high prevalence region were more likely to be economically disadvantaged, to have ≥ 3 persons per household, and had a nearly sevenfold increased incidence of newly diagnosed HIV infection.
To determine if our selection criteria (clindamycin-susceptible MRSA) was too restrictive for identifying the USA300 strains, pulsed field gel electrophoresis was performed on the first four clindamycin-resistant isolates from six hospitals. To examine for potential bias, 20 isolates originated from hospitals in the western (low prevalence) part of the city. None of clindamycin-resistant MRSA were related to either USA300 or USA400 strains (Fig. 3).
Pulsed field gel electrophoresis of clindamycin-resistant clinical isolates. Lane 1: lamda ladder. Lane 2: representative USA300 isolate. Lanes 3–10: isolates collected from two hospitals in the western part of the city. Lane 11: representative USA400 isolate. Lanes 12–15: isolates from a hospital in the eastern part of the city. Lanes 16–27: isolates collected from three hospitals in the western part of the city.
To determine if patients with cultures positive for the USA300 strain were representative of the population of the high prevalence neighborhoods, records of 20 patients from two medical centers within the higher prevalence region were reviewed. Of the 20 patients, three were ≤ 18 years of age and 11 were female. Seventeen of the 20 patients resided within the neighborhoods with the higher prevalence. Two patients were known to be HIV positive. Prior hospitalization (within the previous year) was documented in five patients and one patient was on hemodialysis. Six patients had Medicaid or Medicare as their health insurance, and only two patients possessed private health insurance. Race and ethnicity were recorded in only ten of the patients; nine were Black and one was white/Hispanic.
Discussion
Several studies, often performed without the benefit of genetic fingerprinting of the bacterial isolates, found several identifiable risk factors (e.g., hospitalization within one year, nursing home residence, hemodialysis, or placement of a long-term intravascular device) that were associated with community-onset MRSA infection or colonization [11–13]. However, this scenario has changed dramatically with the emergence of two MRSA strains, USA300 and USA400. While several well-described outbreaks involving USA300 (e.g., in prisons and sports teams) and USA400 (e.g., in postpartum women and maternity units) have been reported [7–10], risk factors for acquisition of these strains in the general population are largely unknown. In Atlanta, patients with skin and soft tissue infections with the USA300/400 strains were more likely to be black and female when compared to patients with infections due to MSSA [2]. The USA300 type predominated in this study, and the medical center served a largely black and indigent population [2]. In Minnesota, patients with cultures with CA-MRSA were more likely to be younger, nonwhite, and of lower socioeconomic status when compared to patients with hospital-acquired strains of MRSA [4]. In a multicenter study involving patients from Atlanta, Baltimore, and Minnesota, patients with CA-MRSA were likely to have several underlying conditions (e.g., tobacco use, prior skin infections, diabetes mellitus, asthma, and HIV infection) and were of lower socioeconomic status; isolates in this report were not fingerprinted [14]. In a nationwide survey examining rates of nasal colonization, S. aureus was more common in men, those with asthma, and in subjects < 65 years of age; blacks and Mexicans had lower colonization rates when compared to whites. Risk factors for MRSA colonization included age > 65 years, female sex, underlying diabetes mellitus, and residence in a long-term care facility; Hispanics were less likely than whites to be colonized with MRSA [3]. However, approximately half of the MRSA isolates in the last study possessed SCCmec II, suggesting that many were hospital-associated strains.
As the boundary between cases with nosocomial and community-associated MRSA becomes hazy, it is increasingly apparent that future epidemiological studies will require thorough characterization of the bacterial isolates. In this report, only 35% of our isolates with the antibiotic phenotype suggestive of CA-MRSA (MRSA susceptible to clindamycin) belonged to the USA300/400 types. In addition, only 62% of isolates with SCCmec type IV belonged to the USA300/400 types; whether the other isolates represent CA-MRSA strains unique to our region requires further investigation.
In this report, we performed a population-based analysis of CA-MRSA in Brooklyn, NY using all S. aureus isolates identified in hospital microbiology laboratories. By itself, Brooklyn would rank as the fourth largest city in the United States, and has an extremely heterogeneous population. In this urban setting, we found a higher prevalence of USA300 strains in neighborhoods with several distinguishing characteristics. Neighborhoods with a higher prevalence of USA300 had a greater proportion of blacks, Hispanics, females, and children, and had measures indicative of a disadvantaged socioeconomic status. As more households had ≥ 3 persons in the high prevalence neighborhoods, crowded living conditions are likely an important contributing factor for the spread of the USA300 strain. Although racial and ethnic risk factors have been noted in other studies of CA-MRSA [2–4], it remains to be determined if these features are causal in nature or just reflect lower socioeconomic status (and crowded living conditions).
Our results are in stark contrast to a prior study examining epidemiology of Streptococcus pneumoniae in Brooklyn [18]. In that report, the western region of the city (identified with the lower prevalence of USA300) had a higher rate of penicillin-resistant S. pneumoniae, and was attributed to greater access to healthcare (and antimicrobial agents). Indeed, increased antibiotic consumption has been postulated as a protective factor against CA-MRSA in certain populations [3]. It is evident that in a large urban setting, these two resistant community pathogens do not share similar epidemiological characteristics.
Conclusion
The USA300 strain of CA-MRSA is emerging in Brooklyn, NY. In this population-based study, urban regions with characteristics of lower socioeconomic status and with evidence of overcrowding appear to have a higher prevalence of this pathogen.
References
McDougal LK, Steward CD, Killgore GE, Chaitram JM, McAllister SK, Tenover FC: Pulsed-field gel electrophoresis typing of oxacillin-resistant Staphylococcus aureus isolates from the United States: Establishing a national database. J Clin Microbiol. 2003, 41: 5113-5120. 10.1128/JCM.41.11.5113-5120.2003
King MD, Humphrey BJ, Wang YF, Kourbatova EV, Ray SM, Blumberg HM: Emergence of community-acquired methicillin-resistant Staphylococcus aureus USA 300 clone as the predominant cause of skin and soft-tissue infections. Ann Intern Med. 2006, 144: 309-317.
Graham PL, Lin SX, Larson EL: A U.S. population-based survey of Staphylococcus aureus colonization. Ann Intern Med. 2006, 144: 318-325.
Naimi TS, LeDell KH, Como-Sabetti K, Borchardt SM, Boxrud DJ, Etienne J, Johnson SK, Vandenesch F, Fridkin S, O'Boyle C, Danila RN, Lynfield R: Comparison of community- and health care-associated methicillin-resistant Staphylococcus aureus infection. J Am Med Assoc. 2003, 290: 2976-2984. 10.1001/jama.290.22.2976.
Vandenesch F, Naimi T, Enright MC, Lina G, Nimmo GR, Heffernan H, Liassine N, Bes M, Greenland T, Reverdy M-E, Etienne J: Community-acquired methicillin-resistant Staphylococcus aureus carrying Panton-Valentine leukocidin genes: Worldwide emergence. Emerg Infect Dis. 2003, 9: 978-984.
Centers for Disease Control and Prevention : Four pediatric deaths from community-acquired methicillin-resistant Staphylococcus aureus -Minnesota and North Dakota, 1997–1999. J Am Med Assoc. 1999, 282: 1123-1125. 10.1001/jama.282.12.1123.
Saiman L, O'Keefe M, Graham PL, Wu F, Said-Salim B, Kreiswirth B, LaSala A, Schlievert PM, Della-Latta P: Hospital transmission of community-acquired methicillin-resistant Staphylococcus aureus among postpartum women. Clin Infect Dis. 2003, 37: 1313-1319. 10.1086/379022
Bratu S, Eramo A, Kopec R, Coughlin E, Ghitan M, Yost R, Chapnick EK, Landman D, Quale J: Community-associated methicillin-resistant Staphylococcus aureus in hospital nursery and maternity units. Emerg Infect Dis. 2005, 11: 808-813.
Centers for Disease Control and Prevention : Methicillin-resistant Staphylococcus aureus skin or soft tissue infections in a state prison-Mississippi, 2000. Morb Mortal Wkly Rep. 2001, 50: 919-922.
Centers for Disease Control and Prevention : Public health dispatch: outbreaks of community-associated methicillin-resistant Staphylococcus aureus skin infections-Los Angeles County, California, 2002–2003. Morb Mortal Wkly Rep. 2003, 52: 88-
Jernigan JA, Pullen AL, Partin C, Jarvis WR: Prevalence of risk factors for colonization with methicillin-resistant Staphylococcus aureus in an outpatient clinic population. Infect Control Hosp Epidemiol. 2003, 24: 445-450. 10.1086/502223
Layton MC, Hierholzer WJ, Patterson JE: The evolving epidemiology of methicillin-resistant Staphylococcus aureus at a university hospital. Infect Control Hosp Epidemiol. 1995, 16: 12-17.
Charlebois ED, Bangsberg DR, Moss NJ, Moore MR, Moss AR, Chambers HF, Perdreau-Remington F: Population-based community prevalence of methicillin-resistant Staphylococcus aureus in the urban poor of San Francisco. Clin Infect Dis. 2002, 34: 425-433. 10.1086/338069
Fridkin SK, Hageman JC, Morrison M, Thomson Sanza L, Como-Sabetti K, Jernigan JA, Harriman K, Harrison LH, Lynfield R, Farley MM, : Methicillin-resistant Staphylococcus aureus disease in three communities. N Eng J Med. 2005, 352: 1436-1444. 10.1056/NEJMoa043252.
Clinical Laboratories Standards Institute : Performance standards for antimicrobial susceptibility testing; sixteenth informational supplement. CSLI document M100-S16. 2006, Clinical Laboratories Standards Institute, Wayne, PA
Oliveira DC, de Lencastre H: Multiplex PCR strategy for rapid identification of structural types and variants of the mec element in methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother. 2002, 46: 2155-2161. 10.1128/AAC.46.7.2155-2161.2002
Zhang K, McClure JA, Elsayed S, Louie T, Conly JM: Novel multiplex PCR assay for characterization and concomitant subtyping of staphylococcal cassette chromosome mec types I to V in methicillin-resistant Staphylococcus aureus. J Clin Microbiol. 2005, 43: 5026-5033. 10.1128/JCM.43.10.5026-5033.2005
Quale J, Landman D, Ravishankar J, Flores C, Bratu S: Susceptibility and epidemiology of Streptococcus pneumoniae in Brooklyn, NY: Fluoroquinolone resistance at our doorstep. Emerging Infect Dis. 2002, 8: 594-597.
Acknowledgements
Funding for this study was provided as research grants from Cubist Pharmaceuticals, Pfizer, Inc., and Wyeth-Ayerst Pharmaceuticals.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
SB, DL, and JQ conceived the study, participated its design and coordination, and helped draft the manuscript. JG, MT, and MP participated in the design and coordination of the study. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Bratu, S., Landman, D., Gupta, J. et al. A population-based study examining the emergence of community-associated methicillin-resistant Staphylococcus aureus USA300 in New York City. Ann Clin Microbiol Antimicrob 5, 29 (2006). https://doi.org/10.1186/1476-0711-5-29
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1476-0711-5-29