Abstract
Background
Class 1 integrons contain genetic elements for site-specific recombination, capture and mobilization of resistance genes. Studies investigating the prevalence, distribution and types of integron located resistance genes are important for surveillance of antimicrobial resistance and to understand resistance development at the molecular level.
Methods
We determined the prevalence and genetic content of class 1 integrons in Enterobacteriaceae (strain collection 1, n = 192) and E. coli (strain collection 2, n = 53) from bloodstream infections in patients from six Norwegian hospitals by molecular techniques. Class 1 integrons were also characterized in 54 randomly selected multiresistant E. coli isolates from gastrointestinal human infections (strain collection 3).
Results
Class 1 integrons were present in 10.9% of the Enterobacteriaceae blood culture isolates of collection 1, all but one (S. Typhi) being E. coli. Data indicated variations in class 1 integron prevalence between hospitals. Class 1 integrons were present in 37% and 34% of the resistant blood culture isolates (collection 1 and 2, respectively) and in 42% of the resistant gastrointestinal E. coli. We detected a total of 10 distinct integron cassette PCR amplicons that varied in size between 0.15 kb and 2.2 kb and contained between zero and three resistance genes. Cassettes encoding resistance to trimethoprim and aminoglycosides were most common. We identified and characterized a novel plasmid-located integron with a cassette-bound novel gene (linF) located downstream of an aadA2 gene cassette. The linF gene encoded a putative 273 aa lincosamide nucleotidyltransferase resistance protein and conferred resistance to lincomycin and clindamycin. The deduced LinF amino acid sequence displayed approximately 35% identity to the Enterococcus faecium and Enterococcus faecalis nucleotidyl transferases encoded by linB and linB'
Conclusions
The present study demonstrated an overall low and stable prevalence of class 1 integron gene cassettes in clinical Enterobacteriaceae and E. coli isolates in Norway. Characterization of the novel lincosamide resistance gene extends the growing list of class 1 integron gene cassettes that confer resistance to an increasing number of antibiotics.
Similar content being viewed by others
Background
Integrons are genetic units containing elements for site-specific recombination, capture and mobilization of gene cassettes [1]. To date, five distinct integron classes have been found [2] with more than 60 different antibiotic resistance genes identified within gene cassettes either alone or in combination [3, 4]. Conserved segments are flanking the cassette region usually encoding resistance to various antimicrobials. In class 1 integrons, dominating in clinical Enterobacteriaceae isolates [5–7], the 5' conserved region contains essential elements for insertion and mobilization of gene cassettes: the intI1 gene encoding the integrase which catalyzes site-specific recombination of adjacent gene cassettes; attI, the specific gene cassette insertion site, and Pc, a promoter common for transcription of cassette resistance genes [8, 9]. The 3' conserved segment usually contains the truncated qacE (qacEΔ1) gene encoding low level resistance to disinfectants based on quaternary ammonium compounds, the sul1 gene encoding sulfonamide resistance and an open reading frame (ORF5) of unknown function [4, 10].
Integrons are widely distributed among both nosocomial and community gram-negative isolates [6, 11–13]. However, few studies exist on the prevalence and distribution of integrons from distinct clinical settings (e.g. blood culture isolates and gastrointestinal E. coli). Septicaemia is one of the most serious invasive bacterial infections and the choice of an appropriate antibiotic is of critical importance for the outcome of the infection. Antibiotic resistance among bacteria causing septicemia is still at a low level in Norway [14, 15]. To understand, maintain or even improve this favorable situation, surveillance of antimicrobial resistance is important. Little information exists on resistance at the molecular level among clinical isolates of Enterobacteriaceae. We have investigated the types and occurrence of integron-located antibiotic resistance genes in blood culture Enterobacteriaceae isolates from Norwegian hospitals. The isolates (mainly E. coli) originated from patients at six hospitals covering most parts of Norway. The study also included multiresistant gastrointestinal isolates for comparison of integrons in other E. coli pathovars. Although a narrow spectrum of different gene cassette combinations was observed, we identified and characterized a new plasmid-born class 1 integron located in a blood culture E. coli isolate. The integron contained two cassettes including a novel gene, linF that encoded a putative lincosamide nucleotidyl transferase that conferred resistance to the lincosamides clindamycin and lincomycin.
Methods
Strain collections and selection of bacterial isolates
Strain collection 1
This investigation included 192 clinically relevant Enterobacteriaceae blood culture isolates from separate patients at four university hospitals in Norway collected during the period March 1998–February 1999. All isolates were previously screened for phenotypic antibiotic resistance [14]. The collection included all Enterobacteriaceae isolates among the first ten clinically relevant blood culture isolates each calendar month from four of the five university hospitals in Norway: Tromsø University hospital, Tromsø (n = 39), Trondheim University hospital, Trondheim (n = 46), Haukeland University Hospital, Bergen (n = 52) and Ullevål University Hospital, Oslo (n = 55). The 192 Enterobacteriaceae isolates included E. coli (n = 131), Klebsiella spp. (n = 29), Proteus mirabilis (n = 15), Enterobacter spp. (n = 7), Salmonella spp. (n = 3), Serratia marcescens (n = 3), Proteus vulgaris (n = 2), Citrobacter diversus (n = 1), Yersinia enterocolitica (n = 1).
Strain collection 2
We included 53 multiresistant (resistant to two or more antibiotics) E. coli blood culture isolates sampled at Molde County Hospital (n = 34) and at the Norwegian Radium Hospital, Oslo (n = 19) during 1991–92 and 1995–96 [13]. All the above isolates were selected based on phenotypic resistance to antimicrobials as determined by Leegaard et al. [15].
Strain collection 3
We also included 54 multiresistant E. coli isolates obtained from clinically relevant gastrointestinal human infections randomly selected from the strain collection at the Norwegian Reference laboratory for Enteropathogenic microbes at the Norwegian Institute of Public Health. Isolates collected in 2000 and 2001 included enteroinvasive E. coli (n = 12), enteropathogenic E. coli (n = 3) and E. coli isolates of unknown pathovar (n = 39). These isolates were routinely screened for resistance to ampicillin, ciprofloxacin, tetracycline, chloramphenicol, nalidixic acid and trimethoprim-sulfamethoxazole by a tablet diffusion method according to the manufacturer's guidelines (Rosco diagnostics, Taastrup, Denmark).
Detection and sizing of class 1 integron conserved regions by PCR
Previously described primers 5'CS and 3'CS [16] with homology to the 5' and 3' conserved regions were applied to detect and determine the size of the gene cassettes. Boiled suspensions of bacterial cells were used as template in PCR reactions (94°C for 5 min followed by 25 cycles of 94°C for 30 s, 55°C for 30 s, 72°C for 30 s and a final 7 min extension step at 72°C for 7 min).
PCR-restriction fragment length polymorphism
Obtained integron cassette PCR products were subjected to restriction enzyme analyses with Mse I (5U; New Englands Biolab, Beverly, MA) and electrophoresis of restriction products in 2% metaphor agarose (Cambrex Bio Science, Copenhagen, Denmark) for 2.5 h. Cassettes with identical restriction profiles were regarded to contain the same gene cassettes. One or two cassette amplicons representatives for each restriction profile were selected for DNA sequence characterization.
DNA sequence analyses
Purified (QIAquick PCR purification kit (QIAGEN, Hilden, Germany) gene cassette PCR products were subjected to direct sequencing using the BigDye Terminator kit (ABI biosystems, Foster City, CA) and 3.2 pmol of the 5'CS and 3'CS primers [16] in separate reactions. A primer walking strategy completed double strand sequencing. All sequencing reactions were purified with the DyeEx Spin Kit (QIAGEN) to remove unincorporated dye terminators prior to electrophoresis on an ABI-310 Genetic Analyzer (ABI biosystems). Sequence data were exported from the ABI-310 into Lasergene software (DNASTAR, Madison, WI) for sequence alignments, comparisons and on-line searches for related sequences via the National Center for Biotechnology Information (NCBI) BLAST server. The cassette promoter region of the E. coli X1D61 integron was determined by sequencing of both strands with 3.2 pmol of primers IntA2-upper (5'GCCGCCAATGCCTGACGAT-3') and aadA2_IntI1 (5'-TATCGCTGTATGGCTTCA-3') of an appropriate PCR product.
Cloning and transformation of a novel open reading frame
The integron-located novel open reading frame (ORF) of E. coli X1D61 was cloned in pET101/D-TOPO vector and transformed into E. coli BL21 Star (DE3) using the pET Directional Expression kit (Invitrogen, Carlsbad, CA). As a control, the aadA2 gene (streptomycin/spectinomycin resistance) located in the same integron, was cloned and transformed separately in the same expression system. The vector constructs containing the novel ORF and aadA2 gene were designated pET101X38 and pET101A17, respectively. Prior to cloning, PCR primers for both genes were designed (Table 1) and PCR amplicons obtained using 55°C annealing temperature and Platinum Pfx DNA polymerase according to the manufacturer's instructions (Invitrogen). The orientation and sequences of transformant DNA-inserts were analyzed by PCR and double strand sequencing using combinations of primers annealing within the insert and the T7 reverse and T7 forward primers annealing in the vector.
Plasmid isolation and southern blotting
Plasmids were isolated as described by Kapperud et al. [17], separated by 0.7% agarose gel electrophoresis and photographed under UV light after ethidium bromide staining. Plasmid DNA was transferred to hybond-N+ membranes (Amersham Biosciences, Buckinghamshire, England) by vacuum blotting and hybridized at 55°C with an intI1 specific PCR probe using the AlkPhos Direct labelling kit and chemiluminescent detection with CDP-Star (Amersham-Pharmacia Biotech).
Susceptibility tests
E. coli BL21 Star (DE3) transformants containing the constructs pET101X38 and pET101A17 were tested for resistance to lincosamides (lincomycin, clindamycin) and aminoglycosides (streptomycin, gentamycin and kanamycin) in an assay for determining the minimal inhibitory concentration (MIC). Tubes with 5 ml LB-broth, ampicillin (Amp) 50 μg/ml and isopropylthio-β-galactosid (IPTG) 0.5 mM were inoculated by 50 μl of over night grown (LB-broth, Amp 50 μg/ml, 37°C with shaking) cultures of transformants and incubated at 37°C for two hours for induction of gene expression. Induced cultures (100 μl) were transferred to tubes containing 2 ml LB-broth, Amp (50), IPTG (1 mM) and two-fold dilutions of the appropriate antibiotic before incubation at 37°C in a roller drum for 18 hours. The MICs were determined as the lowest concentration completely inhibiting visual growth.
Nucleotide sequence accession number
The nucleotide sequence of the partial integron of isolate X1D61 described in this study has been assigned the accession number AJ561197.
Results
Class 1 integrons in clinical Enterobacteriaceae isolates
Source/hospital of isolation, characteristics and distribution of integron gene cassettes in blood culture isolates (strain collection 1 and 2) and gastrointestinal isolates (strain collection 3) are summarized in Table 2.
Among the 192 blood culture Enterobacteriaceae isolates (131 E. coli) from blood stream infections at four university hospitals in Norway (strain collection 1), 21 isolates (E. coli (n = 20), Salmonella Typhi (n = 1)) contained class 1 integron resistance gene cassettes. Integron-positive E. coli were isolated from bloodstream infections in all four hospitals. All 20 class 1 integron-positive E. coli isolates were resistant to one (a single strain) or more antibiotics based on previously determined antibiotic susceptibility data [12]. In total, fifty-four of the 131 E. coli strain collection 1 isolates were resistant to antibiotics. Thus, class 1 integrons were present in 37.0% (20/54) of the resistant E. coli isolates. Among E. coli isolates of collection 2 (53 isolates) and 3 (54 isolates) (all strains resistant to at least two antibiotics), 34.0% (18/53) and 42.6% (23/54), respectively, harbored integron class 1 specific gene cassettes.
Preliminary characterization by PCR restriction fragment length polymorphism (PCR-RFLP) separated all cassette amplicons into a total of 10 distinct profiles. Sequence analyses of PCR products representing each of the PCR-RFLP profiles identified a single gene cassette in each of the amplicons with sizes of 700 bp, 800 bp and 1000 bp. Two gene cassettes present in tandem were detected in the 1600 bp 1800, 1900 bp and 2000 bp amplicons, while three gene cassettes were present in the 2200 bp amplicon. The 150 bp amplicon observed in a single isolate was found to be a class 1 integron variable region without a gene cassette present.
Characterization of antibiotic resistance gene cassettes of class 1 integrons
The most common type of gene cassettes included trimethoprim resistance genes (six genes (number of isolates in parenthesis): dfrA5 (n = 21), dfrA1 (n = 10), dfrA17 (n = 10), dfrA7 (n = 4), dfrA12 (n = 2), dfrB2 (n = 1) followed by aminoglycoside resistance genes (three genes: aadA1 (n = 24), aadA2 (n = 3) and aadA5 (n = 10); Table 2). All integrons with present gene cassettes encoded either trimethoprim resistance, aminoglycoside resistance or both. Among blood culture isolates (strain collection 1 and 2), four cassette or cassette combinations (dfrA5 (23.1%), aadA1 (23.1%), dfrA1 + aadA1 (17.9%), dfrA17 + aadA5 (20.5%) represented 84.6% (33/39) of the integron cassette structures. For gastrointestinal isolates, more than 50% (12/23) of the gene cassettes obtained contained the dfrA5 gene. Only four blood culture isolates contained integrons with cassettes encoding resistance to additional antibiotics: beta-lactam resistance (oxa1, two isolates), chloramphenicol resistance (catB2, one isolate) and a novel open reading frame (ORF) was identified in one isolate.
Characterization of a novel class 1 integron gene cassette with flanking sequences
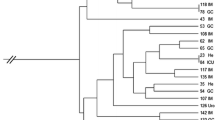
Sequence analyses of a 1.9 kb cassette region of a blood culture isolate identified a cassette region flanked by 5'-conserved segment (CS) and 3'CS. Two cassettes each with a single ORF were identified in the cassette region. The first cassette contained the aadA2 gene flanked by conserved gene cassette features including a candidate integrase recombination core site (attI1) 5' of aadA2 and a 59-be 3'to the gene. The aadA2 gene cassette was followed by a second putative cassette containing the 822 bp novel ORF. Analyses of a 45 bp region between the 3'end of the ORF and the 3'conserved segment (containing qacEΔ1 and sul1) showed presence of imperfect inverted repeat elements and a consensus core site at the junction with the 3'-conserved segment consistent with a 59-be (Fig. 1). A candidate 59-be inverse core site (GCACAAC, nt 2130–2136) was present in the gene coding region just upstream the stop codon but could not be identified at the left-hand end of the element as expected. Despite the short length, but with partial homology to previously analyzed 59-be, the present element were regarded as a novel variant of 59-be [18]. The novel integron was plasmid located as shown by hybridization (Fig. 2).
Southern blot hybridization of E. coli X1D61 plasmid DNA showing plasmid bound location of a novel class 1 integron. Lane 1: Positive control and plasmid size standard (mix of plasmids from E. coli V517 (Macrina et al. [30] and an E. coli strain hosting the class1 integron containing plasmid R1). Lane 2: Negative control (plasmids from E. coli V517. Lane 3: Plasmids from E. coli X1D61 containing the novel linF resistance gene cassette.
The novel ORF encoded a putative 273 amino acid protein (termed LinF) and shared 34.9–35.2% identity to LinB in Enterococcus faecium [19]; Accession No. AAD26631) and LinB-like sequences (Accession No. AAL05554 and CAC05684) that confer lincosamide resistance in E. faecalis and an uncultured bacterium (Fig. 3). Homology was also evident to a nucleotidyltransferase domain involved in nucleotidyl transferases responsible for some types of bacterial resistance to aminoglycosides. The promoter region located in the 5'-CS included a hybrid Pc (formerly Pant or P1) promoter with a strong and weak -35 hexamer (TGGACA, nt 140–145) and -10 hexamer (TAAACT, nt 163–168), respectively. The potential secondary P2 promoter sequence was consistent with a non-functional promoter (TTGTTA-n14-TACAGT; nt 258–283).
LinF expresses resistance to lincosamides
Based on BLAST homology search results, the novel ORF was suspected to be putative lincosamide and/or aminoglycoside resistance gene. The BL21 Star(DE3)/pET101X38(linF) transformants expressed increased resistance to both lincomycin (MIC = 512) and clindamycin (MIC = 128) compared to control strains, but were susceptible to the other antibiotics tested (Table 3). The aadA2 containing transformant BL21 Star(DE3)/pET101A17(aadA2) expressed as expected resistance to streptomycin (MIC = 256) compared to susceptible isolates (MIC = 4; Table 3).
Discussion
The prevalence and molecular characteristics of class 1 integrons in blood culture Enterobacteriaceae isolates and gastrointestinal E. coli from patients at Norwegian hospitals were studied. The blood culture collections included Enterobacteriaceae (collection 1) and E. coli (collection 2) collected in different time periods from hospitals covering all parts of Norway. This study should therefore give a representative picture of class 1 integron prevalence in Norwegian blood culture Enterobacteriaceae (mainly E. coli) isolates. Class 1 integrons were present in 10.9% of blood culture Enterobacteriaceae isolates collected from four university hospitals in Norway during a one year period (1998–1999; collection 1). All but one (S. Typhi) of the integron positive isolates were E. coli. Schmitz et al. [6] reported 13% of 278 blood culture Enterobacteriaceae isolates including E. coli (16.7%), Klebsiella spp. and Enterobacter spp. collected during a four-month period in 1998 at a single hospital (University Hospital Düsseldorf, Germany), to contain class 1 integrons. Our data indicated variation in integron prevalence among the hospitals under study. Only a single isolate (2.1%) from the University Hospital of Trondheim, contained a class 1 integron. This represents a significantly lower prevalence (P = 0.025) than in the other three hospitals associated with strain collection 1 (Bergen (15.4%), Oslo (12.7%), Tromsø (12.8%)). This indicates hospital to hospital variations and/or regional differences in the incidence of integrons. No significant differences in the prevalence or types of integron cassettes could be observed between isolates from the specialist national cancer hospital (Norwegian Radium Hospital) assumed to confer an environment with a high antibiotic selection pressure, and the regional hospital (Molde County Hospital; strain collection 2). The limited number of isolates we investigated may only have allowed the detection of major changes. The overall low and stable prevalence of class 1 integron gene cassettes is concurrent with the low and stable occurrence of phenotypic antibiotic resistance reported in Norwegian Enterobacteriaceae blood culture isolates compared to other regions of the world [15].
Among E. coli isolated from patients with gastrointestinal infections, 42.6 (23/54) contained a class 1 integron. Notably, a selection bias was applied in that only strains resistant to two or more of six antibiotics used in routine screening were analyzed for integron content. Previous reports have shown higher class 1 integron prevalence in other clinical E. coli isolates: 62% (intensive care and surgical unit isolates from hospitals in nine European countries, [20]) 52% (various clinical specimen isolates, [21]; 45% (urinary isolates, [22]). Variations in selection pressures in different clinical environments may lead to different integron prevalence in various E. coli pathovars.
A few distinct gene cassettes (aacA4, aadA1, dfrA1/aadA1) have been reported to predominate in blood culture Enterobacteriacea e isolated from different European hospitals [23]. In the present study, genes encoding resistance to trimethoprims and the early aminoglycosides also dominated the gene cassettes. Among blood culture isolates (strain collection 1 and 2), four cassettes or cassette combinations (dfrA5 (23.1%), aadA1 (23.1%), dfrA1 + aadA1 (17.9%), dfrA17 + aadA5 (20.5%)) represented 84.6% (33/39) of the integrons. Gene cassettes encoding resistance to other antibiotics were present in a few isolates but always in combination with aminoglycoside and/or trimethoprim resistance cassettes. The oxa1/aadA1 cassette configuration, found in two blood culture isolates, is characteristic for the transposon Tn2603 [24]. Integrons with this cassette structure have recently been located in Salmonella Typhimurium of diverse geographical origin [7, 25, 26]. A single isolate (blood culture isolate) hosted a class 1 integron with three gene cassettes (dfrB2, aadA1 and the catB2). This integron may have evolved by the insertion of a dfrB2 cassette in the integron of transposon Tn2424 containing the aadA1 and catB2 genes [27].
Interestingly, sequencing analyses of a 1900 bp variable integron region of an E. coli blood culture isolate identified a novel open reading frame (ORF) downstream of an aadA2 gene cassette. A translated BLAST search (blastx) revealed amino acid identity (34.9%) to the highly similar lincosamide resistance proteins LinB and LinB-like proteins reported in E. faecium and E. faecalis, respectively and 35.2% identity to a LinB-like protein of an uncultured bacterium (Accession no. CAC05684). LinF did not display any significant homology with the sequences of staphylococcal lincosamide nucleotidyltransferases encoded by linA' and linA [28, 29]. Partial amino acid identity to a nucleotidyltransferase domain of aminoglycoside resistance enzymes was also evident by the RPS-BLAST program. MIC-analyses of E. coli transformants showed the novel ORF to be a gene encoding lincosamide resistance. The identity to the previously characterized LinB resistance protein indicates the resistance mechanism to be enzyme inactivation by nucleotidylation of a hydroxyl group. Downstream of linF, a short region (45 bp) was regarded as a novel variant of 59-be present between the linF stop codon and the 3' conserved segment. Previously reported 59-be varies considerably in sequence length (57–141 bp) and composition and only short segments including imperfect repeated elements at the outer ends are conserved [18]. The present 45 bp region has a consensus core site (GTTAGAT) at the junction with the 3'-conserved segment while a candidate inverse core site (GCACAAC) was present in the gene coding region adjacent to the linF stop codon and not in the left hand region as expected. Possible consequences of the observed structure and sequence (e.g. on gene cassette recombination activity) are at present unknown. The characterization of linF represents the first report of an integron-located gene cassette that encodes resistance to lincosamides.
Conclusions
A few stable integron structures seem to predominate in Norway as in most other countries. However, this study also illustrates the ability of integrons to capture and collect novel genes encoding resistance to classes of antibiotics whose resistance has not previously been associated with integrons. This extends the growing list of class 1 integron gene cassettes that confer resistance to an increasing number of antibiotics within many classes. A restrictive antibiotic subscription policy is needed to avoid an increased selection pressure where integrons play a potential significant role for the uptake and dissemination of resistance genes. This could have further negative implications for future therapeutic use of antibiotics.
References
Hall RM, Stokes HW: Integrons: novel DNA elements which capture genes by site-specific recombination. Genetica. 1993, 90: 115-132.
Collis CM, Kim MJ, Partridge SR, Stokes HW, Hall RM: Characterization of the class 3 integron and the site-specific recombination system it determines. JBacteriol. 2002, 184: 3017-3026. 10.1128/JB.184.11.3017-3026.2002.
Nield BS, Holmes AJ, Gillings MR, Recchia GD, Mabbutt BC, Nevalainen KM, Stokes HW: Recovery of new integron classes from environmental DNA. FEMS MicrobiolLett. 2001, 195: 59-65. 10.1016/S0378-1097(00)00546-2.
Recchia GD, Hall RM: Gene cassettes: a new class of mobile element. Microbiology. 1995, 141 ( Pt 12): 3015-3027.
Mazel D, Dychinco B, Webb VA, Davies J: Antibiotic resistance in the ECOR collection: integrons and identification of a novel aad gene. Antimicrob Agents Chemother. 2000, 44: 1568-1574. 10.1128/AAC.44.6.1568-1574.2000
Schmitz FJ, Martinez-Freijo P, Theis S, Fluit AC, Verhoef J, Heinz HP, Jones ME: Class I integrons: prevalence and impact on antibiotic susceptibility in 278 consecutive unrelated Gram-negative blood isolates. ClinMicrobiolInfect. 1999, 5: 496-498.
Tosini F, Visca P, Luzzi I, Dionisi AM, Pezzella C, Petrucca A, Carattoli A: Class 1 integron-borne multiple-antibiotic resistance carried by IncFI and IncL/M plasmids in Salmonella enterica serotype typhimurium. AntimicrobAgents Chemother. 1998, 42: 3053-3058.
Collis CM, Hall RM: Expression of antibiotic resistance genes in the integrated cassettes of integrons. AntimicrobAgents Chemother. 1995, 39: 155-162.
Partridge SR, Recchia GD, Scaramuzzi C, Collis CM, Stokes HW, Hall RM: Definition of the attI1 site of class 1 integrons. Microbiology. 2000, 146 ( Pt 11): 2855-2864.
Paulsen IT, Littlejohn TG, Radstrom P, Sundstrom L, Skold O, Swedberg G, Skurray RA: The 3' conserved segment of integrons contains a gene associated with multidrug resistance to antiseptics and disinfectants. AntimicrobAgents Chemother. 1993, 37: 761-768.
Leverstein-van Hall MA, HE M.Blok, AR T.Donders, Paauw A, Fluit AC, Verhoef J: Multidrug resistance among Enterobacteriaceae is strongly associated with the presence of integrons and is independent of species or isolate origin. JInfectDis. 2003, 187: 251-259. 10.1086/345880.
Leverstein-van Hall MA, Paauw A, Box AT, Blok HE, Verhoef J, Fluit AC: Presence of integron-associated resistance in the community is widespread and contributes to multidrug resistance in the hospital. JClinMicrobiol. 2002, 40: 3038-3040. 10.1128/JCM.40.8.3038-3040.2002.
Zhao S, White DG, Ge B, Ayers S, Friedman S, English L, Wagner D, Gaines S, Meng J: Identification and characterization of integron-mediated antibiotic resistance among Shiga toxin-producing Escherichia coli isolates. ApplEnvironMicrobiol. 2001, 67: 1558-1564. 10.1128/AEM.67.4.1558-1564.2001.
Leegaard TM, Bevanger L, Jureen R, Lier T, Melby KK, Caugant DA, Oddvar Froholm L., Hoiby EA: Antibiotic sensitivity still prevails in Norwegian blood culture isolates. IntJAntimicrobAgents. 2001, 18: 99-106. 10.1016/S0924-8579(01)00364-8.
Leegaard TM, Vik E, Caugant DA, Froholm LO, Hoiby EA: Low occurrence of antibiotic resistance in Escherichia coli and staphylococci isolated from blood cultures in two Norwegian hospitals in 1991-92 and 1995-96. APMIS. 1999, 107: 1060-1068.
Levesque C, Piche L, Larose C, Roy PH: PCR mapping of integrons reveals several novel combinations of resistance genes. AntimicrobAgents Chemother. 1995, 39: 185-191.
Kapperud G, Lassen J, Dommarsnes K, Kristiansen BE, Caugant DA, Ask E, Jahkola M: Comparison of epidemiological marker methods for identification of Salmonella typhimurium isolates from an outbreak caused by contaminated chocolate. JClinMicrobiol. 1989, 27: 2019-2024.
Stokes HW, O'Gorman DB, Recchia GD, Parsekhian M, Hall RM: Structure and function of 59-base element recombination sites associated with mobile gene cassettes. MolMicrobiol. 1997, 26: 731-745. 10.1046/j.1365-2958.1997.6091980.x.
Bozdogan B, Berrezouga L, Kuo MS, Yurek DA, Farley KA, Stockman BJ, Leclercq R: A new resistance gene, linB, conferring resistance to lincosamides by nucleotidylation in Enterococcus faecium HM1025. AntimicrobAgents Chemother. 1999, 43: 925-929.
Martinez-Freijo P, Fluit AC, Schmitz FJ, Grek VS, Verhoef J, Jones ME: Class I integrons in Gram-negative isolates from different European hospitals and association with decreased susceptibility to multiple antibiotic compounds. JAntimicrobChemother. 1998, 42: 689-696. 10.1093/jac/42.6.689.
Chang CY, Chang LL, Chang YH, Lee TM, Chang SF: Characterisation of drug resistance gene cassettes associated with class 1 integrons in clinical isolates of Escherichia coli from Taiwan, ROC. JMedMicrobiol. 2000, 49: 1097-1102.
White PA, McIver CJ, Rawlinson WD: Integrons and gene cassettes in the enterobacteriaceae. AntimicrobAgents Chemother. 2001, 45: 2658-2661. 10.1128/AAC.45.9.2658-2661.2001.
Martinez-Freijo P, Fluit AC, Schmitz FJ, Verhoef J, Jones ME: Many class I integrons comprise distinct stable structures occurring in different species of Enterobacteriaceae isolated from widespread geographic regions in Europe. AntimicrobAgents Chemother. 1999, 43: 686-689.
Ouellette M, Roy PH: Homology of ORFs from Tn2603 and from R46 to site-specific recombinases. Nucleic Acids Res. 1987, 15: 10055-
Guerra B, Soto S, Cal S, Mendoza MC: Antimicrobial resistance and spread of class 1 integrons among Salmonella serotypes. AntimicrobAgents Chemother. 2000, 44: 2166-2169. 10.1128/AAC.44.8.2166-2169.2000.
Lindstedt BA, Heir E, Nygard I, Kapperud G: Characterization of class I integrons in clinical strains of Salmonella enterica subsp. enterica serovars Typhimurium and Enteritidis from Norwegian hospitals. JMedMicrobiol. 2003, 52: 141-149. 10.1099/jmm.0.04958-0.
Parent R, Roy PH: The chloramphenicol acetyltransferase gene of Tn2424: a new breed of cat. JBacteriol. 1992, 174: 2891-2897.
Brisson-Noel A, Courvalin P: Nucleotide sequence of gene linA encoding resistance to lincosamides in Staphylococcus haemolyticus. Gene. 1986, 43: 247-253. 10.1016/0378-1119(86)90213-1
Brisson-Noel A, Delrieu P, Samain D, Courvalin P: Inactivation of lincosaminide antibiotics in Staphylococcus. Identification of lincosaminide O-nucleotidyltransferases and comparison of the corresponding resistance genes. JBiolChem. 1988, 263: 15880-15887.
Macrina FL, Kopecko DJ, Jones KR, Ayers DJ, McCowen SM: A multiple plasmid-containing Escherichia coli strain: convenient source of size reference plasmid molecules. Plasmid. 1978, 1: 417-420.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contributions
EH had the primary responsibility for study design, data collection and writing the manuscript. B-AL participated in the study design and had intellectual contributions. TML provided strains and resistance data on strain collections 1 and 2 and had intellectual contributions. EG verified the results and had intellectual contributions. GK had intellectual contributions.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Heir, E., Lindstedt, BA., Leegaard, T.M. et al. Prevalence and characterization of integrons in blood culture Enterobacteriaceae and gastrointestinal Escherichia coli in Norway and reporting of a novel class 1 integron-located lincosamide resistance gene. Ann Clin Microbiol Antimicrob 3, 12 (2004). https://doi.org/10.1186/1476-0711-3-12
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1476-0711-3-12