Abstract
Background
Resistance of Helicobacter pylori to clarithromycin has been associated with A2142G and A2143G point mutations in the 23S rRNA gene. Thus, the purpose of the present study was to determine the prevalence of each mutation in 52 clarithromycin-resistant H. pylori strains and to characterize the influence each type of mutation on the MIC.
Methods
The MIC for clarithromycin was determined by the agar dilution method, and the point mutations of H. pylori were detected by PCR followed by restriction fragment length polymorphism.
Results
Clarithromycin MICs ranged from 2 to >256 microgram ml-1 among the 52 strains included in this study. Both the A2142G and the A2143G mutations were present in 94.2% of clarithromycin-resistant H. pylori strains examined. A relationship was observed between the presence of the A2142G mutation and the highest MIC values (p = 0.01).
Conclusion
In an H. pylori- infected population, the A2142G mutation may incur to a greater probability of treatment failure if clarithromycin is used.
Similar content being viewed by others
Background
Helicobacter pylori is a gram-negative bacterium that colonizes the human stomach and is associated with a variety of digestive diseases, such as chronic gastritis and peptic ulcer disease [1, 2]. Infection with H. pylori can be effectively treated by the combination of a proton pump inhibitor with multiple antibiotics. The first-line regimen consists mainly of a triple therapy, and clarithromycin is one of the most widely used components. Although the bacteria can be eradicated in up to 90% of patients, side effects, poor compliance and resistance to the antibiotics used are common causes of treatment failure [3, 4].
The increasing use of clarithromycin has resulted in the development of resistance. The prevalence of resistant strains varies among countries and ranges from 1% in Norway [5] to 29% in Japan [6]. The mechanism of resistance to clarithromycin in H. pylori seems to be due to a decrease in binding of macrolides to the ribosome, associated with point mutations within the peptidyltransferase-encoding region of 23S rRNA gene [7, 8]. Three major point mutations in two positions have been described in which an adenine residue is replaced by a guanine or a cytosine residue at adjacent positions: A2142C, A2142G, and A2143G [7–10]. Thus, the purpose of the present study was to determine the prevalence of each mutation in 52 clarithromycin-resistant H. pylori strains and also characterize the influence of the type of mutation upon MIC.
Material and Methods
Bacterial growth conditions and MIC determination
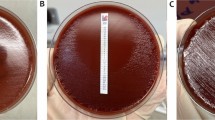
H. pylori strains used in this study were isolated in the Clinical Pharmacology and Gastroenterology Unit of Sao Francisco University Medical School, Braganca Paulista, SP, Brazil. Fifty-two previously isolated clarithromycin-resistant (claR) strains were inoculated on Brain Heart Infusion agar plates (Difco, Detriot, MI, USA) supplemented with 2.5 g L-1 yeast extract (Difco) and 10% lysed sheep blood (BBV, Campinas, Brazil), and 6 mg L-1 vancomycin (Sigma Aldrich Chemie, St. Louis, MO, USA), 20 mg L-1 nalidixic acid (Sigma Aldrich Chemie), 2 mg L-1 amphotericin B (Sigma Aldrich Chemie), 40 mg L-1 2,3,5, triphenyl-tetrazolium chloride (Sigma Aldrich Chemie), referred to as BHI-YE plates, followed by incubation for 3–5 days at 37°C under microaerophilic conditions. The MIC for clarithromycin was determined by the agar dilution method, using twofold increments (0.125 to 256 μg ml-1) on Mueller-Hinton agar (Merck, Darmstadt, Germany) supplemented with 10% sheep blood, and incubated at 37°C under microaerophilic conditions [11]. The isolates were considered resistant when the MIC of clarithromycin was > 1 μg ml-1 [12–14].
Detection of mutation associated with clarithromycin resistance
The point mutations of H. pylori were detected by PCR followed by restriction fragment length polymorphism (RFLP). DNA from 52 claR H. pylori isolates was extracted by a standard phenol-chloroform method [15]. Part of the 23S rRNA gene was amplified with primers 18 (5'-AGTCGGGACCTAAGGCGAG-3') and 21 (5'-TTCCCGCTTAGATGCTTTCAG-3'), and the amplicon of approximately 1.4 Kb was digested with Mbo II (New England Biolabs, Beverly, MA, USA) or Bsa I (New England Biolabs) to detect the A2142G and the A2143G mutations, respectively [8]. The restriction fragments were analyzed on a 3% agarose gel.
Sequence analysis
When none of the aforementioned mutations were detected, direct sequencing was used. An internal fragment, that comprises the majority of mutations related to clarithromycin resistance, was amplified using the following primers; 5'-GTAACTATAACGGTCCTAAG-3' (Cla1995Fw) and 5'-GAAACATCAAGGGTGGTATC-3' (Cla2274Rev). PCR was performed in a final volume of 50 μl, with approximately 25 pg of template genomic DNA and 25 pmol of each primer. PCR amplification was carried out through 35 cycles consisting of a denaturation step of 95° C for 30 sec, a primer-annealing step of 50°C for 30 sec and an extension step at 72°C for 30 sec, with a single final extension step of 72°C for 10 min. A 280 bp fragment was purified with Wizard® SV Gel and PCR Clean-up System (Promega, Madison, WI) and the direct sequencing was performed by the Hemocentro/UNICAMP genome center (Campinas, Brazil). Sequence data were analyzed with Chromas (Technelysium Pty. Ltd., Helensvale, Australia).
Nucleotide sequence accession numbers
The nucleotide sequences of the BZ440, BZ447 and BZ450 regions of the clarithromycin resistant strains were deposited in GenBank under accession numbers AY303829 to AY303831, respectively.
Natural transformation
Natural transformation was used to verify if the 23S rRNA gene is involved in resistance in cases where none of the mutations related to clarithromycin resistance were detected. Briefly, the clarithromycin sensitive (claS) reference strain, 26695, was transformed with ~1 μg of genomic DNA or ~250 ng of PCR products (1.4 Kb and 280 bp) from the claR strains, as previously described [16]. The resistant transformants were selected on BHI-YE plates supplemented with clarithromycin at 0.5 and 2 μg ml-1 (Abbot Laboratories, North Chicago, Ill). As controls, bacteria were transformed with either DNA from claR strain BZ586 (MIC >256 μg ml-1), DNA from claS strain 26695 [17] or TE [1 mM Tris-HCl (pH 8.0), 0.1 mM EDTA].
Statistical analysis
Statistical analyses were performed using either the χ2 test with Yates continuity correction or Fisher's exact test. A p value of < 0.05 was considered statistically significant.
Results and Discussion
Clarithromycin is a key component of most current triple-therapy regimens for treatment of H. pylori infection, however resistance is a major determinant in the failure of eradication regimens [3]. Clarithromycin resistance varies around the world with rates ranging from 1 to 29% [5, 6], in Brazil the resistance rate observed was 16% [18]. Increasing resistance rates have been observed and seem to be due to the increase in the use of this antibiotic, not only for H. pylori eradication but also for treatment of respiratory tract infections [3].
The molecular mechanism of H. pylori resistance to clarithromycin is associated with A-to-G substitution within the peptidyltransferase-encoding region of the 23S rRNA gene [7, 8]. The clarithromycin MICs ranged from 2 to >256 μg ml-1 for the 52 strains included in this study. Either the A2142 mutation or the A2143G mutation were present in 94.2% of clarithromycin-resistant H. pylori strains examined. The majority of isolates (82.7%) contained the A2142G mutation, whereas the A2143G was present in 11.5% (Table 1). Additionally, when an MIC of ≥ 64 μg ml-1 was used to define a high level of clarithromycin resistance, differences in prevalence of each mutation were observed (Table 1). There was a relationship between the presence of the A2142G mutation and the highest MIC values (p = 0.01).
Some authors have shown that the A2143G mutation was the most frequently detected mutation [19, 20], however, our data and those of others demonstrate that the A2142G mutation is more prevalent in Brazil [8, 21]. Although the presence of the A2143G mutation was rare in the present study and the A2142G mutation demonstrated the highest frequency observed, the clinical relevance of this distinction has a limited value, since the presence of either of these mutations is able to confer clarithromycin resistance [22]. A high level of resistance to clarithromycin has been associated with the presence of the A2142G mutation in H. pylori [13, 23]. According to our results, a greater effect upon MIC was observed among strains possessing the A2142G mutation. Thus, this mutation may incur a greater probability of treatment failure in populations infected by H. pylori [13].
In three isolates, the PCR-RFLP method was unable to detect these substitutions. The sequence analysis of these isolates, from the internal fragment that comprises the majority of point mutations related to clarithromycin resistance, revealed only a T-to-C transition at position 2245 (Based on GenBank accession no. U27270). To determine whether the T2245C mutation observed was responsible for clarithromycin resistance, the 26695 claS H. pylori strain was transformed with genomic DNA and specific PCR products. For this purpose, the 23S rRNA was amplified using primers, 18 and 21 [8], while internal primers, Cla1995 and Cla2274, created a 280 bp fragment that only contained the T2245C substitution. The transformants were selected on BHI-YE plates supplemented with clarithromycin. Although the T2245C substitution was present in these three resistant strains, clarithromycin-resistant transformants containing the T2245C substitution were only observed after transformation with genomic DNA, but not after transformation with 23S rRNA PCR fragments. While transformants were found after transformation with DNA and PCR products from the BZ586 claR strain, none of the transformants were selected after transformation with DNA from the claS strain 26695 or TE. The MIC values of clarithromycin of 10 randomly selected resistant transformants was determined by agar dilution and were identical to those of donor strains.
Although, in the sequence data only a T2245C substitution was found, natural transformation was unable to detect an association between the presence of mutations in the 23S rRNA gene and clarithromycin resistance. Additionally, analysis of several sequences based on GenBank indicated that the T2245C substitution was detected in both resistant and susceptible H. pylori strains (AB088050-to-AB088065). Thus, the molecular mechanism of clarithromycin resistance remains undetermined in these three cases.
Conclusions
In conclusion, our results support the hypothesis that the A2142G and A2143G mutations in the 23s rRNA gene of H. pylori are linked to clarithromycin resistance, this finding may have a significant impact on patient management, providing rapid information for the clinician, allowing, for example, appropriate antibiotic prescription and prediction of treatment outcome.
Abbreviations
- PCR-RFLP:
-
Polymerase chain reaction – restriction fragment length polymorphism
- claR:
-
clarithromycin resistant H. pylori strains
- claS:
-
clarithromycin sensitive H. pylori strains.
References
Blaser MJ: Ecology of Helicobacter pylori in the human stomach. J Clin Invest. 1997, 100: 759-762.
Dunn BE, Cohen H, Blaser MJ:Helicobacter pylori. Clinical Microbiology Reviews. 1997, 10: 720-741.
Megraud F: Epidemiology and mechanism of antibiotic resistance in Helicobacter pylori. Gastroenterology. 1998, 115: 1278-1282.
de Boer WA, van Etten RJ, Schneeberger PM, Tytgat GN: A single drug for Helicobacter pylori infection: first results with a new bismuth triple monocapsule. Am J Gastroenterol. 2000, 95: 641-645. 10.1016/S0002-9270(00)00763-2
Megraud F, Lehn N, Lind T, Bayerdorffer E, O'Morain C: Antimicrobial susceptibility testing of Helicobacter pylori in a large multicenter trial: the MACH 2 study. Antimicrobial Agents and Chemotherapy. 1999, 43: 2747-2752.
Kato S, Fujimura S, Udagawa H, Shimizu T, Maisawa S, Ozawa K, Linuma K.: Antibiotic resistance of Helicobacter pylori strains in Japanese children. J Clin Microbiol. 2002, 40: 649-653. 10.1128/JCM.40.2.649-653.2002
Occhialini A, Urdaci M, Doucet-Populaire F, Bebear CM, Lamouliatte H, Megraud F: Macrolide resistance in Helicobacter pylori : rapid detection of point mutations and assays of macrolide binding to ribosomes. Antimicrob Agents Chemother. 1997, 41: 2724-2728.
Versalovic J, Shortridge D, Kibler K, Griffy MV, Beyer J, Flamm RK, Tanaka SK, Graham DY, Go MF: Mutations in 23S rRNA are associated with clarithromycin resistance in Helicobacter pylori. Antimicrob Agents Chemother. 1996, 40: 477-480.
Hulten K, Gibreel A, Skold O, Engstrand L: Macrolide resistance in Helicobacter pylori : mechanism and stability in strains from clarithromycin-treated patients. Antimicrob Agents Chemother. 1997, 41: 2550-2553.
van Doorn LJ, Glupczynski Y, Kusters JG, Megraud F, Midolo P, Maggi-Solca N, Queiroz DM, Nouhan N, Stet E, Quint WG: Accurate prediction of macrolide resistance in Helicobacter pylori by a PCR line probe assay for detection of mutations in the 23S rRNA gene: multicenter validation study. Antimicrob Agents Chemother. 2001, 45: 1500-1504. 10.1128/AAC.45.5.1500-1504.2001
Glupczynski Y, Labbe M, Hansen W, Crokaert F, Yourassowsky E: Evaluation of the E-test for quantitative antimicrobial susceptibility testing of Helicobacter pylori. Journal of Clinical Microbiology. 1991, 29: 2072-2075.
Mendonça S, Ecclissato C, Sartori MS, Godoy APO, Guerzoni RA, Degger M, Pedrazzoli JJ: Prevalence of Helicobacter pylori resistance to metronidazole, clarithromycin, amoxicillin, tetracycline, and furazolidone in Brazil. Helicobacter. 2000, 5: 79-83. 10.1046/j.1523-5378.2000.00011.x
Versalovic J, Osato MS, Spakovsky K, Dore MP, Reddy R, Stone GG, Shortridge D, Flamm RK, Tanaka SK, Graham DY: Point mutations in the 23S rRNA gene of Helicobacter pylori associated with different levels of clarithromycin resistance. J Antimicrob Chemother. 1997, 40: 283-286. 10.1093/jac/40.2.283
Alarcón T, Domingo D, Prieto N, Lopez-Brea M: Clarithromycin resistance stability in Helicobacter pylori : influence of the MIC and type of mutation in the 23S rRNA. J Antimicrob Chemother. 2000, 46: 613-616. 10.1093/jac/46.4.613
Ge Z, Taylor DE: H. pylori DNA transformation by natural transformation and electroporation. In Methods in molecular medicine: Helicobacter pylori protocols. Edited by: Clayton CL, Mobley HLT. 1997, Totowa: N.J: Humana Press Inc,
Wang Y, Roos KP, Taylor DE: Transformation of Helicobacter pylori by chromosomal metronidazole resistance and by a plasmid with a selectable chloramphenicol resistance marker. Journal of General Microbiology. 1993, 139: 2485-2493.
Tomb JF, White O, Kerlavage AR, Clayton RA, Sutton GG: The complete genome sequence of the gastric pathogen Helicobacter pylori. Nature. 1997, 388: 539-547. 10.1038/41483
Godoy APO, Ribeiro ML, Benvengo YH, Vitiello L, Miranda Md MB, Mendonca S, Pedrazzoli J: Analysis of antimicrobial susceptibility and virulence factors in Helicobacter pylori clinical isolates. BMC Gastroenterol. 2003, 3: 20- 10.1186/1471-230X-3-20
Domingo D, Alarcon T, Sanz JC, Sanchez I, Lopez-Brea M: High frequency of mutations at position 2144 of the 23S rRNA gene in clarithromycin-resistant Helicobacter pylori strains isolated in Spain. J Antimicrob Chemother. 1998, 41: 573-574. 10.1093/jac/41.5.573
Pina M, Occhialini A, Monteiro L, Doermann HP, Megraud F: Detection of point mutations associated with resistance of Helicobacter pylori to clarithromycin by hybridization in liquid phase. J Clin Microbiol. 1998, 36: 3285-3290.
Stone GG, Shortridge D, Flamm RK, Versalovic J, Beyer J, Idler K, Zulawinski L, Tanaka SK: Identification of a 23S rRNA gene mutation in clarithromycin-resistant Helicobacter pylori. Helicobacter. 1997, 1: 227-228.
Oleastro M, Menard A, Santos A, Lamouliatte H, Monteiro L, Barthelemy P, Megraud F: Real-time PCR assay for rapid and accurate detection of point mutations conferring resistance to clarithromycin in Helicobacter pylori. Clin Microbiol. 2003, 41: 397-402. 10.1128/JCM.41.1.397-402.2003.
Debets-Ossenkopp YJ, Brinkman AB, Kuipers EJ, Vandenbroucke-Grauls CM, Kusters JG: Explaining the bias in the 23S rRNA gene mutations associated with clarithromycin resistance in clinical isolates of Helicobacter pylori. Antimicrob Agents Chemother. 1998, 42: 2749-2751.
Acknowledgments
This work was supported by the Fundacao de Amparo a Pesquisa do Estado de Sao Paulo (01/12369-1). YHBB is supported by a fellowship from Fundacao de Amparo a Pesquisa do Estado de Sao Paulo (02/08566-9)
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contribition
MLR and MCBM carried out the molecular genetic studies; APOG, YHBB, LV and SM participated in the antimicrobial susceptibility analysis; MLR drafted the manuscript; MLR and LV performed the statistical analysis; MLR, SM and JPJ participated in the design of the study and coordination; All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Ribeiro, M.L., Vitiello, L., Miranda, M.C. et al. Mutations in the 23S rRNA gene are associated with clarithromycin resistance in Helicobacter pylori isolates in Brazil. Ann Clin Microbiol Antimicrob 2, 11 (2003). https://doi.org/10.1186/1476-0711-2-11
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1476-0711-2-11