Abstract
Background
Given the threat of resistance of human malaria parasites, including to artemisinin derivatives, new agents are needed. Chloroquine (CQ) has been the most widely used anti-malarial, and new analogs (CQAns) presenting alkynes and side chain variations with high antiplasmodial activity were evaluated.
Methods
Six diaminealkyne and diaminedialkyne CQAns were evaluated against CQ-resistant (CQ-R) (W2) and CQ-sensitive (CQ-S) (3D7) Plasmodium falciparum parasites in culture. Drug cytotoxicity to a human hepatoma cell line (HepG2) evaluated, allowed to calculate the drug selectivity index (SI), a ratio of drug toxicity to activity in vitro. The CQAns were re-evaluated against CQ-resistant and -sensitive P. berghei parasites in mice using the suppressive test. Docking studies with the CQAns and the human (Hss LDH) or plasmodial lactate dehydrogenase (Pf LDH) enzymes, and, a β-haematin formation assay were performed using a lipid as a catalyst to promote crystallization in vitro.
Results
All tested CQAns were highly active against CQ-R P. falciparum parasites, exhibiting half-maximal inhibitory concentration (IC50) values below 1 μΜ. CQAn33 and CQAn37 had the highest SIs. Docking studies revealed the best conformation of CQAn33 inside the binding pocket of Pf LDH; specificity between the residues involved in H-bonds of the Pf LDH with CQAn37. CQAn33 and CQAn37 were also shown to be weak inhibitors of Pf LDH. CQAn33 and CQAn37 inhibited β-haematin formation with either a similar or a 2-fold higher IC50 value, respectively, compared with CQ. CQAn37 was active in mice with P. berghei, reducing parasitaemia by 100%. CQAn33, -39 and -45 also inhibited CQ-resistant P. berghei parasites in mice, whereas high doses of CQ were inactive.
Conclusions
The presence of an alkyne group and the size of the side chain affected anti-P. falciparum activity in vitro. Docking studies suggested a mechanism of action other than Pf LDH inhibition. The β-haematin assay suggested the presence of an additional mechanism of action of CQAn33 and CQAn37. Tests with CQAn34, CQAn37, CQAn39 and CQAn45 confirmed previous results against P. berghei malaria in mice, and CQAn33, 39 and 45 were active against CQ-resistant parasites, but CQAn28 and CQAn34 were not. The result likely reflects structure-activity relationships related to the resistant phenotype.
Similar content being viewed by others
Background
Malaria remains a major public health problem, resulting in 207 million cases and 627,000 deaths worldwide in 2012 [1]. There is no available vaccine, and the control of the disease relies on the use of bed nets, other individual protection against mosquito bites, and the successful drug treatment of infected patients [2]. Presently, chemotherapy has been hampered by the low sensitivity of the parasite to most available anti-malarial drugs [3], including artemisinin derivatives [4–6]. Resistance to chloroquine, in the case of P. falciparum, is linked to mutations in the P. falciparum chloroquine resistance transporter (pfcrt) gene, which alters the transport and accumulation of the drug in the digestive vacuole (DV) of the parasite [7, 8]. Plasmodium vivax resistance to CQ has been described [9, 10] and seems related to the intense malaria morbidity in the Amazon region [11]. However, neither CQ-R nor mutation markers were detected among P. vivax in recent studies of 47 isolates from the West Amazon, all from patients with non-severe malaria [12].
Chemical modifications of CQ have been used as a powerful strategy to find new anti-P. falciparum agents effective against drug-resistant parasites [13, 14]. Structural modifications of the alkyldiamine side chains have provided rather active compounds with decreased cross-resistance to CQ [15] and with different structure-activity relationships [16–18]. In the present work, six CQ analogs (CQAns) that reduced parasitaemia in P. berghei-infected mice [19], comprising diaminealkynes and diaminedialkynes, were evaluated in vitro against CQ-R (W2 clone) and CQ-S (3D7 strain) forms of P. falciparum parasites in cultures. These CQAns were then reevaluated in mice with CQ-sensitive or CQ-resistant P. berghei parasites. The compounds with the best selectivity index, based on drug cytotoxicity and activity in vitro, were evaluated for the inhibition of β-hematin formation. To clarify the possible mechanism of action of the CQAns evaluated herein, docking studies were also performed based on interactions between the CQAns and the plasmodial lactate dehydrogenase (Pf LDH) enzyme, a known target of 4-aminoquinolines [20, 21].
Methods
Synthesis of the molecules
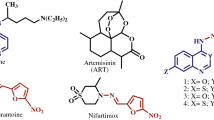
Drug synthesis was performed as previously reported by Da Silva et al. [22]. In brief, 4-alkyldiamino-7-chloroquinolines were treated with 2 eq. of propargyl bromide and K2CO3 in EtOH at 0°C for 72 h to produce the compounds CQAn28, CQAn33, and CQAn34 at a 50% to 60% yield. The addition of 4 eq. of propargyl bromide under the same conditions led to the production of the compounds CQAn37, CQAn39, and CQAn45 at a 50% to 60% yield (Figure 1). All the compounds were characterized via one-dimensional nuclear magnetic resonance (1D-NMR), infrared (IR) spectroscopy, and melting point (MP) assays, and the results were in accordance with data in the literature [22].
Cytotoxicity tests in vitro
A human hepatoma cell line (HepG2), originally received from the University of Lisbon as a kind gift, was cultured as described [23]. The cells were maintained in RPMI 1640 medium (Sigma-Aldrich, ref 6504) supplemented with 40 mg/L gentamicin and 10% heat-inactivated foetal calf serum (FCS), and they were maintained in a 5% CO2 atmosphere at 37°C. When confluent, the cell monolayer was trypsinized, washed with culture medium supplemented with 10% FCS, counted, diluted (5 × 103 cells/well), placed in flat-bottom 96-well plates (Corning, Santa Clara, CA, USA), and incubated for 18 h at 37°C to allow cell adhesion. The compounds were added to the plates at concentrations up to 1,700 μM, followed by incubation for an additional 24 h, after which 20 μL (5 μg/mL) of 3-(4,5-dimethylthiazol-2-yl)-2,5 diphenyltetrazolium bromide (MTT) solution was added per well to evaluate drug cytotoxicity. After 3 h, the supernatant was discarded, 100 μL of dimethyl sulphoxide (DMSO) was added per well, and the optical density was measured (SpectraMax340PC384, Molecular Devices) at 570 nm (test) and 630 nm (background). Cell viability was expressed as the percentage of the absorbance compared to the absorbance of the untreated cells and subtracted from the appropriate background measurement. The lethal drug dose for 50% of the cells (MLD50) was determined as described [24] and was used to calculate the SI of the active compounds, a ratio of the in vitro cell toxicity and activity against P. falciparum (MLD50/IC50).
Continuous cultures of P. falciparum
CQ-R P. falciparum parasites (W2 clone) [25] and CQ-S (3D7 strain), originally received from New York University Medical School, were maintained in continuous culture at 37°C in human erythrocytes (A+) using complete medium (RPMI 1640 supplemented with 10% blood group A+ human serum) changed daily [26]. Before tests with the molecules were performed, ring stage parasites were synchronized using sorbitol [27] and the parasitaemia and haematocrit were adjusted; 180 μL/well was added to 96-well microtiter plates (Corning, Santa Clara, CA, USA) containing the diluted compounds tested in triplicate. Drug activity was evaluated in relation to control cultures with no drugs [28] and was measured using the anti-histidine-rich protein II (HRPII) test as described [29]. CQ was used in each test as a control, and two to four experiments were performed for each parasite strain.
In vitro tests of drug activity
The anti-HRPII test was performed using P. falciparum cultures adjusted for 0.05% parasitaemia and 1.5% haematocrit. The cultures were added to plates containing the diluted drugs, followed by incubation for 24 h under standard culture conditions [26]. The contents of six wells with no drugs were harvested in each test plate, pooled in microtubes, and frozen for later use to measure the background parasite growth as described [29]. After a 48 h incubation, the plates were frozen and thawed twice, and 100 μL of lysed cells from each well was added to a plate that had been precoated overnight at 4°C with a primary anti-HRPII monoclonal antibody (MPFM-55A ICLLAB®, USA) for an immunoassay. Phosphate-buffered saline (PBS) containing 0.05% Tween and 4% bovine serum albumin was used for plate blocking (3 h at room temperature) to avoid nonspecific antibody binding. After 1 h at room temperature, the plate was washed, and 100 μL/well of a secondary antibody solution (MPFG-55P ICLLAB®, USA) was added, followed by incubation with 3,3′,5,5′-tetramethylbenzidine (TMB) chromogen (KPL, Gaithersburg, MD, USA) in the dark. The reaction was stopped using 1 M sulfuric acid, and the absorbance was read (450 nm) in a spectrophotometer (SpectraMax340PC384, Molecular Devices). The anti-P. falciparum drug activity was evaluated by comparing the parasite growth in the drug-free control cultures, considered 100% growth, with that in the drug test cultures. Using curve-fitting software (Microcal Origin Software 5.0, Inc.), a sigmoidal dose–response curve was generated, enabling the determination of drug IC50 values. CQAns presenting IC50 ≤ 1 μM were considered active; between 1–5 μM as partially active; and above 5 μM as inactive.
Protocol for animal use in the anti-malarial tests
The protocol for animal use was approved by the Ethics Committee for Animal Use (CEUA LW-23/13) of the Oswaldo Cruz Foundation (Fiocruz). Only Swiss adult female mice (20 ± 2 g weight) were used; they were raised at the animal facilities at FIOCRUZ-Minas.
Anti-malarial tests against P. berghei in mice
The suppressive test was performed as described [30] using the P. berghei NK65 blood parasites, with some modifications [31]. Briefly, the blood parasites were maintained through weekly blood passages in mice. For the experiments, groups of 20–30 mice were inoculated with 1 × 105 infected erythrocytes. Approximately three hours later, they were randomly distributed into groups of five to six mice per cage, which were treated daily by gavage for four consecutive days. All the compounds were freshly diluted in 3% DMSO (Sigma-Aldrich) in RPMI medium and were administered orally at doses of 25 mg/kg or 50 mg/kg. The control mice received the drug vehicle. On days 5 and 7 after parasite inoculation, blood was taken from the tail of each mouse and used to prepare thin smears, which were methanol-fixed, Giemsa-stained and examined microscopically to determine parasitaemia. The inhibition of parasite growth was evaluated in relation to parasitaemia in the untreated mice, which were considered to have 100% parasite growth.
A P. berghei NK65 CQ-resistant strain maintained at -70°C, selected by increasing doses of CQ, maintained in mice under constant drug pressure (CQ 150 mg/kg) [32] and stored at -70°C was also defrosted and used to inoculate mice. When parasitaemic, the drug-resistant parasites were subjected to serial blood passages maintained under CQ treatment with increasingly higher doses, up to 150 mg/kg, then used for the experiments. The mice were inoculated with 107 parasitized RBCs using blood parasites from a donor with parasites resistant to 150 mg/kg of CQ. Groups of five mice each were separated 24 h after the parasite inoculation, then treated orally with the test CQAn at doses of 25 or 50 mg/kg for three consecutive days. Two control groups were used in each experiment; one received CQ at 150 mg/kg and the other was infected but treated with vehicle only (no drugs). The inhibition of parasitaemia was evaluated as described for the mice inoculated with the CQ-sensitive parasites. A compound was considered active when it inhibited parasitaemia more than 40% in relation to the infected but vehicle-treated (no drugs) group.
Inhibition of β-haematin formation assay
The assay was performed using a lipid as a catalyst to promote crystallization [33]. Briefly, drug stock solutions were prepared in DMSO and were used at a final concentration of up to 30 mM. A haem stock (10 mM) was made in DMSO and was diluted to 50 μM with 100 mM sodium acetate (pH 4.8). A 10 mM 1-monooleoyl-rac-glycerol (MOG) stock was made in ethanol and was sonicated before being added to a 50 μM haem stock to make 25 μM MOG–50 μM haem in 100 mM sodium acetate (pH 4.8). The 25 μM MOG–50 μM haem solution was sonicated and added to the assay plate at 100 μL/well. The plates were incubated at 37°C for 2 h to allow crystallization, followed by the addition of 100 μl of 200 mM sodium bicarbonate (pH 9.1) to solubilize any remaining monomeric haem. After incubation for 30 min at room temperature, the amount of solubilized monomeric haem was determined by measuring the absorbance at 405 nm. Finally, 20 μl of 1 M sodium hydroxide was added to the plates to dissolve any crystals that had been formed, and the absorbance was read at 405 nm to determine the total amount of haem present in each well. The inhibition of haem crystallization was determined as a function of the amount of monomeric haem that was not crystallized divided by the total amount of haem present in the assay mixture. The results are expressed as IC50 values based on the percentage inhibition of β-haematin formation by the CQAn.
Docking studies
The structures of the inhibitors studied were constructed and optimized with the program Spartan 08 [34] using the Merck Molecular Force Field (MMFF) method [35]. In addition, the partial charges were calculated by single-point energy calculations using the RM1 method [36]. The crystallographic structures of Pf LDH and Hss LDH were downloaded from the Protein Data Bank [37] under the codes 1LDG (resolution 1.74 Å and R factor = 0.197) and 1IOZ (resolution 2.10 Å and R factor = 0.179), respectively.
The program Molegro Virtual Docker® (MVD) [38] was used for the docking studies, and the methodology used was validated by re-docking. To observe possible interactions of the ligands with the solvent present in the crystal, 35 water molecules from a cavity approximately 10 Å in size were considered for the calculations with Pf LDH, whereas 54 molecules were considered for the calculations with Hss LDH. The docking region was restricted to a radius of 15 Å from the centre of the cavity inside each enzyme. The best ligand conformations inside the enzymes were chosen based on 100 runs for each ligand, and considering the superposition to the structure of NADH molecules present in the crystallographic structures combined with the best values for interaction energy, and for the H-bonds with water molecules and the residues of the active sites.
The volumes of the cavities of the NADH-binding sites inside Pf LDH and Hss LDH were determined using MVD® [38].
Results
Anti-P. falciparum activity and selectivity indexes of CQAns
All the CQAns were active in vitro against CQ-R P. falciparum parasites, exhibiting half-maximal inhibitory concentration (IC50) values below 1 μM; the most active molecule was CQAn33 (IC50 = 0.02 ± 0.001 μM). Tested against the CQ-S parasites in parallel, CQAn34 and CQAn37 were active; CQAn33, CQAn39 and CQAn45 were partially active; and CQAn28 was inactive (Table 1).
Most of the CQAns were less toxic than CQ (MLD50 = 410.4±26.6 μM), with MLD50 values ranging from 943 to 1699 μM. The ratios of cytotoxicity to activity (selectivity index, SI) of compounds CQAn37, CQAn33, CQAn39, and CQAn34 were 24275, 7645, 5011, and 4101, respectively, considering the CQ-R parasites. For CQAn28 and CQAn45, the SI values were 2125 and 119, respectively; and for CQ, the SI was 1080. Using CQ-S P. falciparum parasites, none of the CQAns showed an SI higher than CQ (SI = 5679). The highest SI values were exhibited by CQAn34 (SI = 3144) and CQAn37 (SI = 2981); all the other CQAns had SI values below 1500 (Table 2).
Anti-P. berghei malaria activity of the CQAns
All the compounds (CQAn28, CQAn33, CQAn34, CQAn37, CQAn39, and CQAn45) that were tested in mice with P. berghei caused between 73% and 100% inhibition of parasitaemia after treatment with a 25 mg/kg oral dose, compared with the untreated control group on day 5. On day 7, the parasitaemia inhibition reached 93% (Table 3). CQ, used as a control, inhibited parasitaemia by 100% and 97% on days 5 and 7, respectively. The 50 mg/kg dose of CQAn33, CQAn37 and CQ caused 100% inhibition of P. berghei parasitaemia on days 5 and 7 after infection. Two of the five mice receiving CQAn37 and all the mice receiving CQ survived the infection at least 30 days after the end of treatment; CQ cured the mice.
The CQAns were evaluated against a CQ-resistant P. berghei strain (maintained by constant drug pressure at a dose of 150 mg/kg daily until the last passage before the test). The dose of 50 mg/kg was active for all the CQAns on day 5. CQAn45 caused the highest parasitaemia reduction (63%), followed by CQAn39, CQAn33 and CQAn37, which reduced parasitaemia by 62%, 53% and 47%, respectively. CQAn28 and CQAn34 were inactive at 25 mg/kg. As expected, CQ at the highest tolerated dose of 150 mg/kg was inactive against the CQ-resistant P. berghei parasites in mice (Table 3).
Inhibition of β-haematin formation by CQAn
The inhibition of β-haematin formation was evaluated for CQAn33 and CQAn37, the most active CQAns against P. falciparum in vitro. The results showed that CQAn33 inhibited β-haematin formation with an IC50 value similar to that of CQ, whereas CQAn37 inhibited β-haematin formation at a concentration 2-fold higher than that of CQ (Table 4).
Docking studies and the mechanism of activity of the CQAns
The root-mean-square deviation (RMSD) values obtained through re-docking of the NADH structure inside each crystal were lower than 2.00 Å in the case of Pf LDH and Hss LDH (Tables 5 and 6). The cavities of the NADH-binding sites inside Pf LDH and the human lactate dehydrogenase enzyme (Hss LDH) were determined to have volumes of 117,248 and 7,936 Å3, respectively. Both cavities were generated around the NADH structure present inside the crystallographic structures. The results suggest that the new CQAns studied have affinities for the NADH-binding sites of Pf LDH and Hss LDH. These compounds were able to dock and to establish highly stable H-bonds with amino acids and water molecules in the sites, as reflected by the highly negative total intermolecular energy (IE) values (Tables 5 and 6). The IE values were less negative inside Hss LDH than inside Pf LDH.
Inside Pf LDH, all the compounds (except CQAn45) H-bonded to Asp53 and/or Thr97 plus water molecules and displayed good (negative) H-bond energy values. The intermolecular energies were ranked as follows: CQ > CQAn39 > CQAn37 > CQAn33 > CQAn28 > CQAn45 > CQAn34, with lower values than NADH. The highest H-bond energy was observed for CQAn33 and the lowest for CQAn45.
Most of the active-site residues of Pf LDH involved in H-bonds differed from those of Hss LDH. Thus, the residues of Pf LDH involved in H-bonds with CQAn33 and CQAn37 were Thr97, Val138 and H20; and Asp53 and H20, respectively. The residues of Hss LDH for the same molecules were Lys147, Ala146 and Asn116; and Gly15, Asn116, Ala146 and Lys147, respectively.
To better understand the experimentally observed selectivity, the electrostatic potentials of the NADH-binding sites inside Pf LDH and Hss LDH were determined. The results showed differences in the binding pockets: inside the Pf LDH pocket, the electrostatic potential was totally positive, whereas inside Hss LDH, it was mostly negative, as illustrated by CQAn33 docked inside both enzymes (Figures 2 and 3).
Discussion
Although CQ-R is widespread, CQAns may help to overcome the drug resistance, especially considering that it is believed to be stage specific [39] and/or related to the compound structure [15]. Indeed, various CQAns have shown potent antiplasmodial activity against CQ-R P. falciparum blood parasites [40–42]. Among the six CQAns tested against P. falciparum in the present work, all exhibited high activity against CQ-R parasites. CQAn28, 33, 37 and 39 were more potent against the CQ-R W2 clone than against the 3D7 CQ-S parasites.
Variation in side chains seems to be a promising strategy concerning the anti-malarial activity of CQAns, and small changes in the spacer length can dramatically affect the activity exhibited against CQ-S and CQ-R parasites [43]. Moreover, the presence of a terminal alkyne seems important: CQAn33, which has a terminal alkyne, showed an IC50 more than 10-fold higher than that of CQ, which has no terminal alkyne.
The activity of 4-aminoquinolines involves their binding to haematin in the monomeric and dimeric forms, inhibiting haemozoin formation and resulting in parasite death [44]. The activity of CQ against P. falciparum also involves interactions with the parasite enzyme Pf LDH [20], as shown by in silico studies with docking and molecular dynamics in the present work. The complex formed between the dimeric haematin and the quinolinic drugs inhibited Pf LDH, as shown with other quinoline derivatives [21].
In previous studies, RMSD values below 2.00 Å were obtained for the plasmodial and human enzymes in re-docking studies, which validates this methodology [45–47]. The intermolecular energy values for the CQAns were higher than for CQ and NADH, showing that the molecules studied here are weak inhibitors of Pf LDH and suggesting that they have a different mechanism of action.
CQAn33 and CQAn37, the molecules with the highest SI in vitro, were also evaluated for their ability to inhibit β-haematin formation. The results showed that CQAn33 inhibited β-haematin formation with an IC50 similar to that of CQ, whereas CQAn37 exhibited an IC50 more than 2-fold higher than CQ, which is in accordance with this molecule being less active than CQAn33 against P. falciparum. The results obtained for anti-P. falciparum activity through the HRPII test showed a rather higher activity of these CQAns in relation to CQ, suggesting another mechanism of action than that related to haemozoin formation, such as apoptosis, autophagy or the inhibition of P-glycoprotein-mediated transport. Metacaspase-like proteins, which are related to caspases [48], have previously been shown to be inducers of apoptosis in P. falciparum parasites exposed to CQ, with more intense DNA fragmentation in CQ-R parasites than in CQ-S [49]. Autophagy-related proteins have been identified in P. falciparum[50, 51]. Indeed, after CQ pressure, P. falciparum parasites exhibited cytoplasmic vacuolization [52], a sign of autophagic cell death [53] rather than of apoptosis. A recent study showed that CQ significantly inhibited P-glycoprotein-mediated transport [54], which is involved in drug evasion in P. falciparum[55].
The highest and lowest H-bond energies were observed for CQAn33 and CQAn45, respectively, a result that corroborates the in vitro data showing that CQAn33 was the most active molecule and CQAn45 the least active against P. falciparum. Another difference is the residues of the plasmodial and human enzymes involved in the H-bonds, specific for CQAn33 and CQAn37; this result is consistent with them having the highest SIs.
The differences in the binding pockets of the studied compounds’ tails inside Pf LDH and Hss LDH could be explained by a large concentration of negative charges due to the presence of the alkyne groups. This finding suggests a better stabilization inside the more positive pocket of Pf LDH, which is caused by the size of the cavity and increases drug specificity. Indeed, the smaller cavity of Pf LDH allows for better accommodation of the ligands than inside Hss LDH.
The most active CQAn in vitro also inhibited P. berghei parasitaemia in mice, as shown in the present work and in our previous studies with the same compounds [19]. An increase in mouse survival resulting from treatment with CQAn37 may well be a consequence of the alkyl side chain altering the structure-activity relationship in the terminal nitrogen [15], which may favor drug lipophilicity. All the CQAns inhibited CQ-R P. berghei parasitaemia in mice, translating the in vitro data, with the exception of CQAn28 and 34, which is likely a result of metabolism [13] or of the structure-activity relationships inherent to the resistance phenotype, e.g., those related to pfcrt[7, 56], also in vivo[57].
The data reported herein highlight the use of CQAns in malaria-endemic areas where drug resistance has been reverted, i.e., sensitivity to CQ has reappeared [58]. CQ is the most widely used anti-malarial drug worldwide [2] due to its low cost, high efficacy and lack of toxicity. In addition, the cost of a treatment course is rather low at US$0.21 per patient [59]. The CQAns evaluated in this study are generated in two steps using readily available, inexpensive starting materials and can be produced in good yields [22] at a cost expected to be as low as that of CQ. Thus, the CQAns studied in the present work may be produced at large scale to proceed in drug development for anti-malarials, since they are promising alternatives for malaria control.
Conclusions
Among the six CQAns tested in vitro, three were more active than CQ, inhibiting 50% of P. falciparum growth at low doses: CQAn33 (IC50 0.02 ± 0.001 μM), CQAn34 (IC50 0.23 ± 0.15 μM), and CQAn37 (IC50 0.07 ± 0.03 μM). All were more active against the CQ-R (W2) parasites than against the CQ-S (3D7) parasites, which suggests the absence of cross-CQ-R. In addition, the therapeutic indexes (or SI) of all CQAns, with the exception of CQAn45, were higher than that of CQ. Docking studies with CQAn33 and CQAn37 corroborated the outstanding anti-P. falciparum activity observed herein and showed that CQAn33 had the highest H-bond energy with the plasmodial enzyme, indicating specificity for Pf LDH. Additionally, they showed that the CQAns are weak inhibitors of Pf LDH, suggesting a different mechanism of action. The inhibition of β-haematin formation by CQAn33 and CQAn37 also suggested mechanisms of action other than those related to haemozoin formation. The in vivo results with CQAn34, CQAn37, CQAn39, and CQAn45 confirm previous data showing their high anti-malarial activity. Furthermore, the CQAns also inhibited the parasitaemia caused by CQ-R P. berghei but CQ did not, translating in vitro to in vivo data. However, CQAn28 and CQAn34 did not inhibit CQ-R P. berghei parasitaemia, what may be a result of metabolism issues or structure-activity relationships related to the resistant phenotype. Altogether, the present results highlight the CQAns studied here as promising anti-malarial agents due to their SI and in vivo activity against malaria in mice.
References
WHO: World Malaria Report 2013. 2014, Geneva: World Health Organization,http://www.who.int/malaria/publications/world_malaria_report_2013/report/en/,
WHO: Guidelines for Treatment of Human Malaria. 2010, Geneva: World Health Organization, 2
WHO: Global Report on Antimalarial Drug Efficacy and Drug Resistance 2000–2010. 2010, Geneva: World Health Organization
Dondorp AM, Nosten F, Yi P, Das D, Phyo AP, Tarning J, Lwin KM, Ariey F, Hanpithakpong W, Lee SJ, Ringwald P, Silamut K, Imwong M, Chotivanich K, Lim P, Herdman T, An SS, Yeung S, Singhasivanon P, Day NP, Lindegardh N, Socheat D, White NJ: Artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med. 2009, 361: 455-457. 10.1056/NEJMoa0808859.
Phyo AP, Nkhoma S, Stepniewska K, Ashley EA, Nair S, McGready R, ler Moo C, Al-Saai S, Dondorp AM, Lwin KM, Singhasivanon P, Day NP, White NJ, Anderson TJ, Nosten F: Emergence of artemisinin-resistant malaria on the western border of Thailand: a longitudinal study. Lancet. 2012, 379: 1960-1966. 10.1016/S0140-6736(12)60484-X.
Miotto O, Almagro-Garcia J, Manske M, Macinnis B, Campino S, Rockett KA, Amaratunga C, Lim P, Suon S, Sreng S, Anderson JM, Duong S, Nguon C, Chuor CM, Saunders D, Se Y, Lon C, Fukuda MM, Amenga-Etego L, Hodgson AV, Asoala V, Imwong M, Takala-Harrison S, Nosten F, Su XZ, Ringwald P, Ariey F, Dolecek C, Hien TT, Boni MF: Multiple populations of artemisinin-resistant Plasmodium falciparum in Cambodia. Nat Genet. 2013, 45: 648-655. 10.1038/ng.2624.
Fidock DA, Nomura T, Talley AK, Cooper RA, Dzekunov SM, Ferdig MT, Ursos LM, Sidhu AB, Naudé B, Deitsch KW, Su XZ, Wootton JC, Roepe PD, Wellems TE: Mutations in the P. falciparum digestive vacuole transmembrane protein PfCRT and evidence for their role in chloroquine resistance. Mol Cell. 2000, 6: 861-871. 10.1016/S1097-2765(05)00077-8.
Roepe PD: PfCRT-mediated drug transport in malarial parasites. Biochemistry. 2011, 50: 163-171. 10.1021/bi101638n.
Price RN, Douglas NM, Anstey NM: New developments in Plasmodium vivax malaria: severe disease and the rise of chloroquine resistance. Curr Opin Infect Dis. 2009, 22: 430-435. 10.1097/QCO.0b013e32832f14c1.
Graf PC, Durand S, Alvarez Antonio C, Montalvan C, Galves Montoya M, Green MD, Santolalla ML, Salas C, Lucas C, Bacon DJ, Fryauff DJ: Failure of supervised chloroquine and primaquine regimen for the treatment of Plasmodium vivax in the Peruvian Amazon. Malar Res Treat. 2012, 2012: 936067-
Gama BE, Lacerda MVG, Daniel-Ribeiro CT, Ferreira-da-Cruz MDF: Chemoresistance of Plasmodium falciparum and Plasmodium vivax parasites in Brazil: consequences on disease morbidity and control. Mem Inst Oswaldo Cruz. 2011, 106: 159-166.
Aguiar AC, Pereira DB, Amaral NS, De Marco L, Krettli AU: Plasmodium vivax and Plasmodium falciparum ex vivo susceptibility to anti-malarials and gene characterization in Rondônia, West Amazon, Brazil. Malar J. 2014, 13: 73-10.1186/1475-2875-13-73.
Hocart SJ, Liu H, Deng H, De D, Krogstad FM: 4-aminoquinolines active against chloroquine-resistant Plasmodium falciparum: basis of antiparasite activity and quantitative structure-activity relationship analyses. Antimicrob Agents Chemother. 2011, 55: 2233-2244. 10.1128/AAC.00675-10.
Casagrande M, Barteselli A, Basilico N, Parapini S, Taramelli D, Sparatore A: Synthesis and antiplasmodial activity of new heteroaryl derivatives of 7-chloro-4-aminoquinoline. Bioorg Med Chem. 2012, 20: 5965-5979. 10.1016/j.bmc.2012.07.040.
Stocks PA, Raynes KJ, Bray PG, Park BK, O’Neill PM, Ward SA: Novel short chain chloroquine analogues retain activity against chloroquine resistant K1 Plasmodium falciparum. J Med Chem. 2002, 45: 4975-4983. 10.1021/jm0108707.
Solomon VR, Puri SK, Srivastava K, Katti SB: Design and synthesis of new antimalarial agents from 4-aminoquinoline. Bioorg Med Chem. 2005, 33: 2165-
Cunico W, Cechinel CA, Bonacorso HG, Martins MAP, Zanatta N, de Souza MVN, Freitas IO, Soares RPP, Krettli AU: Antimalarial activity of 4-(5-trifluoromethyl-1H-pyrazol-1-yl)-chloroquine analogues. Bioorg Med Chem Lett. 2006, 16: 649-653. 10.1016/j.bmcl.2005.10.033.
Madrid PB, Wilson NT, DeRisi JL, Guy RK: Parallel synthesis and antimalarial screening of a 4-aminoquinoline library. J Comb Chem. 2004, 6: 437-442. 10.1021/cc0340473.
de Souza NB, Carmo AM, Lagatta DC, Alves MJ, Fontes AP, Coimbra ES, da Silva AD, Abramo C: 4-aminoquinoline analogues and its platinum (II) complexes as antimalarial agents. Biomed Pharmacother. 2011, 65: 313-316. 10.1016/j.biopha.2011.03.003.
Read JA, Wilkinson KW, Tranter R, Sessions RB, Brady RL: Chloroquine binds in the cofactor binding site of Plasmodium falciparum lactate dehydrogenase. J Biol Chem. 1999, 274: 10213-10218. 10.1074/jbc.274.15.10213.
Cortopassi WA, Oliveira AA, Guimarães AP, Rennó MN, Krettli AU, França TC: Docking studies on the binding of quinoline derivatives and hematin to Plasmodium falciparum lactate dehydrogenase. J Biomol Struct Dyn. 2011, 29: 207-218. 10.1080/07391102.2011.10507383.
Carmo AM, Silva FM, Machado PA, Fontes AP, Pavan FR, Leite CQ, Leite SR, Coimbra ES, Da Silva AD: Synthesis of 4-aminoquinoline analogues and their platinum(II) complexes as new antileishmanial and antitubercular agents. Biomed Pharmacother. 2011, 65: 204-209. 10.1016/j.biopha.2011.01.003.
Denizot F, Lang R: Rapid colorimetric assay for cell growth and survival: modifications to the tetrazolium dye procedure giving improved sensitivity and reliability. J Immunol Methods. 1986, 89: 271-277. 10.1016/0022-1759(86)90368-6.
do Céu de Madureira M, Paula Martins A, Gomes M, Paiva J, Proença da Cunha A, do Rosário V: Antimalarial activity of medicinal plants used in traditional medicine in S Tomé and Príncipe islands. J Ethnopharmacol. 2002, 81: 23-29. 10.1016/S0378-8741(02)00005-3.
Oduola AM, Milhous WK, Weatherly NF, Bowdre JH, Desjardins RE: Plasmodium falciparum: induction of resistance to mefloquine in cloned strains by continuous drug exposure in vitro. Exp Parasitol. 1988, 67: 354-360. 10.1016/0014-4894(88)90082-3.
Trager W, Jensen JB: Human malaria parasites in continuous culture. Science. 1976, 193: 673-675. 10.1126/science.781840.
Lambros C, Vanderberg JP: Synchronization of Plasmodium falciparum erythrocytic stages in culture. J Parasitol. 1979, 65: 418-420. 10.2307/3280287.
Rieckmann KH, Campbell GH, Sax LJ, Mrema JE: Drug sensitivity of Plasmodium falciparum. An in vitro microtechnique. Lancet. 1978, i: 22-23.
Noedl H, Wongsrichanalai C, Miller RS, Myint KS, Looareesuwan S, Sukthana Y, Wongchotigul V, Kollaritsch H, Wiedermann G, Wernsdorfer WH: Plasmodium falciparum: effect of anti-malarial drugs on the production and secretion characteristics of histidine-rich protein II. Exp Parasitol. 2002, 102: 157-163. 10.1016/S0014-4894(03)00051-1.
Peters W, Portus JH, Robinson BL: The four-day suppressive in vivo antimalarial test. Ann Trop Med Parasitol. 1975, 69: 155-171.
Andrade-Neto VF, Goulart MFO, Silva-Filho JF, Matusalém JS, Pinto MCFR, Pinto AV, Zalis MG, Carvalho LH, Krettli AU: Antimalarial activity of phenazines from lapachol, β-lapachone and its derivatives against Plasmodium falciparum in vitro and Plasmodium berghei in vivo. Bioorg Med Chem Lett. 2004, 14: 1145-1149. 10.1016/j.bmcl.2003.12.069.
Krettli AU, Pereira JP, Brener Z: Comparative study of experimental infections in mice inoculated with normal and chloroquine-resistant strains of Plasmodium berghei. Rev Inst Med Trop Sao Paulo. 1969, 11: 94-100.
Pisciotta JM, Coppens I, Tripathi AK, Scholl PF, Shuman J, Bajad S, Shulaev V, Sullivan DJ: The role of neutral lipid nanospheres in Plasmodium falciparum haem crystallization. Biochem J. 2007, 402: 197-204. 10.1042/BJ20060986.
Hehre WJ: A Guide to Molecular Mechanics and Quantum Chemical Calculations. 2003, Irvine: Wavefunction, Inc
Halgren TA: Merck molecular force field. I. Basis, form, scope, parameterization, and performance of MMFF94. J Comput Chem. 1996, 17: 490-519. 10.1002/(SICI)1096-987X(199604)17:5/6<490::AID-JCC1>3.0.CO;2-P.
Rocha GB, Freire RO, Simas AM, Stewart JJ: RM1: a reparameterization of AM1 for H, C, N, O, P, S, F, Cl, Br, and I. J Comput Chem. 2006, 27: 1101-1111. 10.1002/jcc.20425.
Berman HM, Westbrook J, Feng Z, Gilliland G, Bhat TN, Weissig H, Shindyalov IN, Bourne PE: The protein data bank. Nucl Acids Res. 2000, 28: 235-242. 10.1093/nar/28.1.235.
Thomsen R, Christensen MH: MolDock: a new technique for high-accuracy molecular docking. J Med Chem. 2006, 49: 3315-3321. 10.1021/jm051197e.
Gligorijevic B, Purdy K, Elliott DA, Cooper RA, Roepe PD: Stage independent chloroquine resistance and chloroquine toxicity revealed via spinning disk confocal microscopy. Mol Biochem Parasitol. 2008, 159: 7-23. 10.1016/j.molbiopara.2007.12.014.
Solomon VR, Haq W, Srivastava K, Puri SK, Katti SB: Synthesis and antimalarial activity of side chain modified 4-aminoquinoline derivatives. J Med Chem. 2007, 50: 394-398. 10.1021/jm061002i.
Solaja BA, Opsenica D, Smith KS, Milhous WK, Terzić N, Opsenica I, Burnett JC, Nuss J, Gussio R, Bavari S: Novel 4-aminoquinolines active against chloroquine-resistant and sensitive P. falciparum strains that also inhibit botulinum serotype A. J Med Chem. 2008, 51: 4388-4391. 10.1021/jm800737y.
Wenzel NI, Chavain N, Wang Y, Friebolin W, Maes L, Pradines B, Lanzer M, Yardley V, Brun R, Herold-Mende C, Biot C, Tóth K, Davioud-Charvet E: Antimalarial versus cytotoxic properties of dual drugs derived from 4-aminoquinolines and Mannich bases: interaction with DNA. J Med Chem. 2010, 53: 3214-3226. 10.1021/jm9018383.
Iwaniuk DP, Whetmore ED, Rosa N, Ekoue-Kovi K, Alumasa J, de Dios AC, Roepe PD, Wolf C: Synthesis and antimalarial activity of new chloroquine analogues carrying a multifunctional linear side chain. Bioorg Med Chem. 2009, 17: 6560-6566. 10.1016/j.bmc.2009.08.003.
Egan TJ, Ncokazi KK: Quinoline antimalarials decrease the rate of β-hematin formation. J Inorg Biochem. 2005, 99: 1532-1539. 10.1016/j.jinorgbio.2005.04.013.
Kontoyianni M, McClellan LM, Sokol GS: Evaluation of docking performance: comparative data on docking algorithms. J Med Chem. 2004, 47: 558-565. 10.1021/jm0302997.
Leach AR, Shoichet BK, Peishof CE: Prediction of protein-ligand interactions. Docking and scoring: Successes and gaps. J Med Chem. 2006, 49: 5851-5855. 10.1021/jm060999m.
Warren GL, Andrews CW, Capelli AM, Clarke B, LaLonde J, Lambert MH, Lindvall M, Nevins N, Semus SF, Senger S, Tedesco G, Wall ID, Woolven JM, Peishoff CE, Head MS: A critical assessment of docking programs and scoring functions. J Med Chem. 2006, 49: 5912-5931. 10.1021/jm050362n.
Uren AG, O’Rourke K, Aravind LA, Pisabarro MT, Seshagiri S, Koonin EV, Dixit VM: Identification of paracaspases and metacaspases: two ancient families of caspase-like proteins, one of which plays a key role in MALT lymphoma. Mol Cell. 2000, 6: 961-967.
Meslin B, Barnadas C, Boni V, Latour C, De Monbrison F, Kaiser K, Picot S: Features of apoptosis in Plasmodium falciparum erythrocytic stage through a putative role of PfMCA1 metacaspase-like protein. J Infect Dis. 2007, 195: 1852-1859. 10.1086/518253.
Kitamura K, Kishi-Itakura C, Tsuboi T, Sato S, Kita K, Ohta N, Mizushima N: Autophagy-related Atg8 localizes to the apicoplast of the human malaria parasite Plasmodium falciparum. PLoS One. 2012, 7: e42977-10.1371/journal.pone.0042977.
Walker DM, Mahfooz N, Kemme KA, Patel VC, Spangler M, Drew ME: Plasmodium falciparum erythrocytic stage parasites require the putative autophagy protein PfAtg7 for normal growth. PLoS One. 2013, 8: e67047-10.1371/journal.pone.0067047.
Totino PR, Daniel-Ribeiro CT, Corte-Real S, de Fátima F-d-C M: Plasmodium falciparum: erythrocytic stages die by autophagic-like cell death under drug pressure. Exp Parasitol. 2008, 118: 478-486. 10.1016/j.exppara.2007.10.017.
Bursch W: The autophagosomal-lysosomal compartment in programmed cell death. Cell Death Differ. 2001, 8: 569-581. 10.1038/sj.cdd.4400852.
Rijpma SR, van den Heuvel JJ, van der Velden M, Sauerwein RW, Russel FG, Koenderink JB: Atovaquone and quinine anti-malarials inhibit ATP binding cassette transporter activity. Malar J. 2014, 13: 359-10.1186/1475-2875-13-359.
Nogueira F, Lopes D, Alves AC, do Rosário VE: Plasmodium falciparum multidrug resistance protein (MRP) gene expression under chloroquine and mefloquine challenge. J Cell An Biol. 2008, 2: 010-020.
Zishiri VK, Joshi MC, Hunter R, Chibale K, Smith PJ, Summers RL, Martin RE, Egan TJ: Quinoline antimalarials containing a dibemethin group are active against chloroquinone-resistant Plasmodium falciparum and inhibit chloroquine transport via the P. falciparum chloroquine-resistance transporter (PfCRT). J Med Chem. 2011, 54: 6956-6968. 10.1021/jm2009698.
Ghobakhloo N, Nateghpour M, Rezaee S, Hajjaran H, Mohebali M, Abedkhojasteh H: Variation of the chloroquine resistance transporter (Crt) gene in chloroquine-resistant and chloroquine-sensitive Plasmodium berghei. Iran J Parasitol. 2008, 3: 39-44.
Frosch AE, Laufer MK, Mathanga DP, Takala-Harrison S, Skarbinski J, Claassen CW, Dzinjalamala FK, Plowe CV: Return of widespread chloroquine-sensitive Plasmodium falciparum to Malawi. J Infect Dis. 2014, 210: 1110-1114. 10.1093/infdis/jiu216.
WHO: AFR E: Cost Effectiveness Results for Malaria. 2010, Available at http://www.who.int/choice/results/mal_afre/en/
Acknowledgements
We thank the financial support from the Brazilian funding agencies MCT/CNPq/CT-Saúde/MS/SCTIE/DECIT (Edital PRONEX-55675/2009-2 and Edital Doenças Negligenciadas-404455/2012-3); to FAPEMIG (PRONEX-Project 16712); FIOCRUZ for providing facilities and mice, and to CNPq for the fellowships to the authors (AUK; NBS).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
NBS performed the biological tests, ADS was the chemist responsible for planning and synthesizing the CQAn, TCCF performed the docking studies, AUK was the project leader that conceived the study and was responsible for the pharmacological tests. All of the authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
de Souza, N.B., Carmo, A.M., da Silva, A.D. et al. Antiplasmodial activity of chloroquine analogs against chloroquine-resistant parasites, docking studies and mechanisms of drug action. Malar J 13, 469 (2014). https://doi.org/10.1186/1475-2875-13-469
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1475-2875-13-469