Abstract
Background
Labisia Pumila var. alata (LPva) has shown potential as an alternative to estrogen replacement therapy (ERT) in prevention of estrogen-deficient osteoporosis. In earlier studies using postmenopausal model, LPva was able to reverse the ovariectomy-induced changes in biochemical markers, bone calcium, bone histomorphometric parameters and biomechanical strength. The mechanism behind these protective effects is unclear but LPva may have regulated factors that regulate bone remodeling. The aim of this study is to determine the bone-protective mechanism of LPva by measuring the expressions of several factors involved in bone formative and resorptive activities namely Osteoprotegerin (OPG), Receptor Activator of Nuclear Factor kappa-B Ligand (RANKL), Macrophage-Colony Stimulating Factor (MCSF) and Bone Morphogenetic Protein-2 (BMP-2).
Methods
Thirty-two female Wistar rats were randomly divided into four groups: Sham-operated (Sham), ovariectomized control (OVXC), ovariectomized with Labisia pumila var. alata (LPva) and ovariectomized with ERT (Premarin®) (ERT). The LPva and ERT were administered via daily oral gavages at doses of 17.5 mg/kg and 64.5 μg/kg, respectively. Following two months of treatment, the rats were euthanized and the gene expressions of BMP-2, OPG, RANKL and MCSF in the femoral bones were measured using a branch - DNA technique.
Results
The RANKL gene expression was increased while the OPG and BMP-2 gene expressions were reduced in the OVXC group compared to the SHAM group. There were no significant changes in the MCSF gene expressions among the groups. Treatment with either LPva or ERT was able to prevent these ovariectomy-induced changes in the gene expressions in ovariectomized rats with similar efficacy.
Conclusion
LPva may protect bone against estrogen deficiency-induced changes by regulating the RANKL, OPG and BMP-2 gene expressions.
Similar content being viewed by others
Background
Osteoporosis is defined as a systemic skeletal disease that is characterized by low bone mass and micro-architectural deterioration of bone tissue, with a consequent increase in bone fragility and susceptibility to fracture[1]. According to the World Health Organization[2], osteoporosis occurs when the bone mineral density falls more than 2.5 standard deviations (SD) below the standard reference for maximum bone mineral density of young adult females. The bone mass in females begins to decline slowly after the age of 35 to 40, followed by a phase of dramatic bone loss after menopause. This is due to estrogen deficiency which occurs naturally with aging or by surgical ovariectomy.
By 50 years of age, the bone mass in women is only two-thirds of that in men[3]. The relatively lower bone mass in women is due to a combination of lower peak bone mass and faster rate of bone loss. This leads to higher incidence of osteoporosis in elderly women compared to men[4]. Osteoporosis should be managed appropriately as statistics have shown that 1 in 3 women aged more than 50 years old suffered an osteoporotic fracture during their lifetime[5].
Estrogen Replacement Therapy (ERT) is one of the main form of treatment and prevention of postmenopausal osteoporosis. Estrogen given alone or in combination with progesterone is able to prevent postmenopausal osteoporosis effectively[6]. Estrogen binds to its receptors on the osteoclast surface, causing the release of chemical mediators which led to reduction of osteoclastic activity and inhibition of bone resorption[7].
The “Women’s Health Initiative Study” found that women who took ERT have slightly higher rates of ovarian cancer, breast cancer, heart attack, thromboembolism, stroke, and Alzheimer’s disease[8–10]. These negative reports on the serious adverse-effects of ERT have led to many postmenopausal women searching for available alternatives for their postmenopausal symptoms. These have also paved way for missions to discover alternative anti-osteoporotic agents that are comparable in effectiveness to estrogen but with minimal adverse effects. Several potential alternative agents were discovered including soy[11], blueberry[12], Achyranthes bidentata[13] and tocotrienol[14]. Recently, Labisia pumila var. alata (LPva), a herb used for women’s health, was found to produce beneficial effects similar to estrogen on bone biomarkers in postmenopausal osteoporosis animal model[15]. These bone protective effects were further confirmed by bone histomorphometric analysis[14–16] and bone biomechanical strength[15–17].
Labisia Pumila (LP), a plant from the family of Myrinaceae is a popular herb in Malaysia, Indonesia and Indo-China. There are three variants of Labisia pumila, which are var. alata (LPva), var. pumila and var. lanceolata[18]. In Malaysia, it is known locally as “Kacip Fatimah” and the extract can simply be prepared by boiling the leaves, roots or the whole plant in water and the extract is taken orally[18, 19]. Nowadays, various Labisia pumila preparations are available commercially in the forms of capsules or added to drinks. It is used exclusively by women to shrink the uterus, facilitate labor, and improve menstrual irregularities and as post-partum medicine[19, 20]. Its limited use by women for their health supplements has led to the belief that it is a phytoestrogen, a compound with similar chemical structure to estrogen[21]. Several studies have demonstrated the estrogenic properties of LPva. It was found to inhibit estradiol binding to antibodies raised against estradiol[22] and exert a specific estrogenic effect on human endometrial adenocarcinoma cells (Ishikawa-Var I line)[23]. It mimicked estrogen action by preventing the shrinkage of the uterus due to estrogen deficiency in ovariectomized rats[22] and initiate lipolysis in adipose tissue[24]. LPva was also found to down-regulate 11β-hydroxysteroid dehydrogenase-1 expressions in liver and adipose tissues and also decrease serum corticosterone levels in ovariectomized rats[25]. In terms of bone protection against estrogen deficiency, LP was reported to exert estrogen-like effects on bone remodeling[15–17].
Bone remodeling involves a fine balance between bone formation and resorption. Any disturbance to the balance between these two processes would lead to bone pathology. There are several factors or cytokines known to play important roles in bone remodeling. Bone resorption is regulated by Receptor Activator of Nuclear Factor kappa-B ligand (RANKL) and Osteoprotegerin (OPG), which are produced by osteoblasts[26]. RANKL binds to RANK receptors which are located on osteoclast precursors to promote differentiation into mature osteoclasts and activate their bone resorptive activity[27]. It was reported that administration of serum RANKL to mice promoted osteoclast growth and activation, leading to osteoporosis[28]. OPG acts as anti-resorptive decoy receptor by binding to RANKL and preventing it from binding to RANK receptors. As a result, OPG inhibits osteoclast differentiation and its bone resorptive activity. In a recent development, a fully human monoclonal antibody against RANKL was developed to inhibit osteoclast activity. This new agent named denosumab is still under clinical trial as a new anti-osteoporotic agent[29].
Osteoclastogenesis also requires Macrophage-Colony Stimulating Factor (MCSF), which is also expressed by osteoblasts. It binds to the MCSF receptors situated in the osteoclasts and stimulates osteoclastogenesis, but the mechanism involved is still unclear[30]. There are several factors which are known to affect osteoblast activity and differentiation. Among the important one is bone morphogenetic protein-2 (BMP-2), which promotes osteoblast differentiation and plays an important role in bone repair and regeneration[31]. In summary, the differentiation and activation of osteoclast are influenced by the RANKL/OPG system and MCSF, while BMP-2 plays a key role in osteoblast differentiation. Estrogen was able to maintain bone density by regulating the gene expressions of these factors[32] and LPva may have similar actions. To the best of our knowledge, there is no study on the mechanism of LPva extract in preventing bone loss due to estrogen deficiency. Therefore, the aim of the study is to determine the molecular mechanism of LPva in protecting bone against estrogen-deficient osteoporosis by measuring the bone-related gene expressions.
Methods
Animal and treatment
Thirty-two female Wistar rats, aged three months old and weighing 200 to 250 grams, were used as the animal model in this study. The rats were allowed to acclimatize for a week before the start of the study. They were housed two per cage, at normal room temperature with adequate ventilation and normal 12-hour light-dark cycle. All rats were allowed free access to water and food (commercial laboratory rat’s food containing 0.97% calcium, 0.85% phosphorus and 1.05 IU/g of Vitamin D3)(Gold Coin, Selangor, Malaysia). They were randomly divided into four main groups. The sham-operated group (Sham) and the ovariectomized control group (OVXC) were given oral gavages of deionized water (vehicle) throughout the study. The treatment group was either given LPva at the dose of 17.5 mg/kg (LPva group) or Premarin® at the dose of 64.5 μg/kg (ERT group) via daily oral gavages for the duration of 8 weeks. The ERT group acted as the positive control group. The rats were euthanized upon completion of the study and both femora dissected out and cleaned of any tissues. The approval for this study was obtained from the University Animal Ethic Committee of Universiti Kebangsaan Malaysia (PP/FAR/2009/NAZRUN/14 JULY/267-JULY 2009-MAY-2010).
Labisia pumila var. alata (LP) extract
The root extract of LPva (Batch No: KF071107) was purchased from Phytes Biotek Sdn Bhd. (Malaysia), a Good Manufacturing Practice (GMP) licensed manufacturer of herbal products, in the form of a freeze-dried standardized extract. All LPva extractions were performed at the factory in Shah Alam, Selangor, Malaysia, using a patented high-pressure water extraction process (US 7,132,117 B2). They were filtered at 1 to 4 mm and freeze-dried without maltodextrin or lactose. The brownish powdered LPva extract used in this study was similar to the extract used in previous studies by Fathilah et al.[16, 17] and Nazrun et al.[15]. This extract was also the same form used for human consumption as health supplements. Phytochemical testing of the LPva extract by the Forest Research Institute Malaysia (FRIM) found the extract to contain flavonoids, saponins and triterpenes. The LPva extract was dissolved in deionised water and given to the LPva group via oral gavages at the dose of 17.5 mg/kg rat weight at 9 am daily for 8 weeks[15–17]. The Premarin® (Wyeth-Ayerst, Canada) tablet containing 0.625 mg of conjugated estrogen was crushed, dissolved in deionised water and given to the ERT group via oral gavages at the dose of 64.5 μg/kg rat weight at 9 am daily for 8 weeks[15–17]. These doses were chosen based from our previous studies, which have demonstrated protective effects against estrogen-deficient osteoporosis[15–17].
Gene expression measurements
Gene expressions were measured using branched DNA (bDNA) technique as described by Fathilah et. al[33]. The bDNA assay is a sandwich nucleic acid hybridization method that uses bDNA molecules to amplify signals from captured target RNA. Briefly, the femoral bones were ground into a fine powder with a pestle and mortar with the addition of liquid nitrogen. Proteinase K was added to release the ribonucleic acid (RNA), which was then prepared according to directions suggested by Panomics (Fremont, CA) for analysis of mRNA expression using the Panomics QuantiGene Plex 2.0 systems. The bDNA method combines RNA signal amplification and microspheres with unique fluorescent signatures to enable quantitation of multiple mRNA targets simultaneously in the same sample, without having the amplification inaccuracies of RT-PCR (reverse transcriptase–polymerase chain reaction). The method allows for discrimination of highly homologous messages[34, 35]. Specific oligonucleotide capture and extender probe sets (3 per target) annealed exclusively to each mRNA of interest and the housekeeping mRNAs. They were designed according to the unique sequences within each message sequence. The housekeeping genes used in this study were glyceraldehyde-3-phosphate dehydrogenase (GAPDH), glucuronidase-beta (Gusb) and hypoxanthine phosphoribosyltransferase-1 (HPRT1). Specific mRNA transcripts were captured to specific fluorescent beads by hybridization to capture probe-extender probe interactions. The signal from each hybridized unit was amplified by attachment of biotinylated label probes at multiple binding sites on the complexes, which were in turn bound to streptavidin-conjugated R-phycoerythrin (SAPE) to produce fluorescence. The fluorescent signals associated with individual capture beads were read using a Luminex100 IS system (Luminex Corp., Austin, TX, US) with the bead signature designating RNA target and the SAPE signal designating abundance. For each well, the total fluorescence from each individual bead type (corresponding to individual mRNA species) minus the background fluorescence for that bead type was normalized to the geometric mean of the fluorescence of the 3 housekeeping genes. The normalized signals for individual mRNAs from triplicate wells were averaged to yield a single value for each mRNA species being measured.
Statistical analysis
The results were expressed as mean ± standard error of the mean (SEM). The data analysis was performed using the Statistical Package for Social Sciences software (SPSS 19; SPSS, Chicago, IL, USA). The data were first tested for normality using the Kolmogorov–Smirnov test. For normally distributed data, the statistical tests used were the analysis of variance (ANOVA), followed by Tukey’s Honestly Significant Difference (HSD) test. For data that were not normally distributed, Kruskal–Wallis and Mann–Whitney tests were used.
Results
RANKL gene expressions
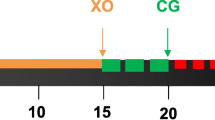
The RANKL gene expression of the femoral bones was significantly higher in the OVXC group compared to other groups. Treatment with ERT was able to prevent the ovariectomy-induced elevation of RANKL gene expression, until it was at the same level as the Sham group. LPva supplementation was also able to prevent the ovariectomy-induced elevation of RANKL gene expression. There were no significant differences in the RANKL gene expression levels between the Sham, ERT and LPva groups (Figure 1).
RANKL Gene Expression. Samples were normalized to GAPD MFI (MedianFluorescence Intensity). Error bars represent the standard deviations of the average responses. Values were expressed as mean ± SEM; p < 0.05 is considered significant. a indicates significant difference compared to the Sham group. Sham (water vehicle), OVXC (water vehicle), LPva (Labisia pumila var. Alata 17.5 mg/kg/day), ERT (Premarin 64.5 μg/kg/day).
OPG gene expressions
The OPG gene expression of the femoral bones was significantly lower in the OVXC group compared to the other groups. Treatment with ERT was able to prevent the ovariectomy-induced reduction of OPG gene expression, until it was at the same level as the Sham group. LPva supplementation was also able to prevent the ovariectomy-induced reduction of OPG gene expression. There were no significant differences in the OPG gene expression levels between the Sham, ERT and LPva groups (Figure 2).
Osteoprotegerin Gene Expression. Samples were normalized to GAPD MFI (MedianFluorescence Intensity). Error bars represent the standard deviations of the average responses. Values were as mean ± SEM; p < 0.05 is considered significant. a indicates significant difference compared to the Sham group. Sham (water vehicle), OVXC (water vehicle), LPva (Labisia pumila var. Alata 17.5 mg/kg/day), ERT (Premarin 64.5 μg/kg/day).
MCSF gene expression
There were no significant changes in MCSF gene expressions of the femoral bones for all the groups (Figure 3).
BMP-2 gene expression. Samples were normalized to GAPD MFI (MedianFluorescence Intensity). Error bars represent the standard deviations of the average responses. Values were as mean ± SEM; p < 0.05 is considered significant. a indicates significant difference compared to the Sham group. Sham (water vehicle), OVXC (water vehicle), LPva (Labisia pumila var. Alata 17.5 mg/kg/day), ERT (Premarin 64.5 μg/kg/day).
BMP-2 gene expression
The BMP-2 gene expression of the femoral bones was significantly lower in the OVXC group compared to the other groups. Treatment with ERT was able to prevent the ovariectomy-induced reduction of BMP-2 gene expression, until it was at the same level as the Sham group. LPva supplementation was also able to prevent the ovariectomy-induced reduction in BMP-2 gene expression. There were no significant differences in the BMP-2 gene expression levels between the Sham, ERT and LPva groups (Figure 4).
MCSF Gene Expression. Samples were normalized to GAPD MFI (MedianFluorescence Intensity). Error bars represent the standard deviations of the average responses. Values were expressed as mean ± SEM. P < 0.05 is considered significant. a indicates significant difference compared to the Sham group. Sham (water vehicle), OVXC (water vehicle), LPva (Labisia pumila var. Alata 17.5 mg/kg/day), ERT (Premarin 64.5 μg/kg/day).
Discussion
Hormone replacement therapy (HRT/ERT) has been used for the treatment and prevention of postmenopausal osteoporosis, but it has been associated with serious side-effects (Ferguson, 2004)[36]. Multiple studies have reported that women who took HRT have slightly higher rates of thromboembolism, heart attack, breast cancer, ovarian cancer, stroke, and Alzheimer’s disease[8–10]. LPva has potential as an alternative to ERT for the treatment of postmenopausal osteoporosis. In terms of safety, several toxicity studies have confirmed that LPva is safe[37, 38]. While, in terms of its action, LPva has demonstrated phytoestrogenic properties[20, 21]. In an earlier study, LPva was found to reverse the bone biochemical marker changes due to ovariectomy[15]. Following that, a further study reported that LPva protected bone from osteoporotic changes due to estrogen deficiency. This was based on its ability to preserve the bone histomophometric parameters of ovariectomised rats[16]. These osteo-protective effects of LPva would be beneficial if they are accompanied by improvement in the bone strength, thus reducing the risk of fracture. This was confirmed by a biomechanical study which showed that supplementation of LPva in ovariectomised rats resulted in stronger femoral bone[17].
Several mechanisms of the bone protective effects of LPva were proposed. Other than acting as phytoestrogen, LPva may exert anti-inflammatory and anti-oxidant effects[17]. There were reports that inflammation may induce osteoporosis[39, 40]. LPva may inhibit inflammation that may be responsible for osteoporosis by inhibiting tumor necrosis factor (TNF)-α production and down-regulating cyclooxygenase-2 expression[41].
Reactive oxygen species were shown to cause bone loss by stimulating osteoclast differentiation[42] and promoting osteoblast apoptosis[43]. LPva exhibited anti-oxidative properties as it contains flavanoids, ascorbic acid, beta-carotene, anthocyanin and phenolic compounds[44]. Beta-carotene was found to have the best correlation with anti-oxidative capacities of LP, followed by flavonoids, ascorbic acid, anthocyanin and phenolic content[45]. Flavonoids were confirmed by phytochemical screening to be present in our LPva extract. It is a potent free radical scavenger in oxidative stress-related diseases such as osteoporosis and rheumatism[46]. Other potent anti-oxidants such as vitamin E have also been shown to protect bone against osteoporosis[14]. Therefore, the anti-oxidative and anti-inflammatory properties of LPva extract may have contributed to the effectiveness of this medicinal plant in treating osteoporosis.
In the final pathway for pathogenesis of osteoporosis, there will be an imbalance between bone formation by osteoblast and bone formation by osteoclasts with the latter getting the upper hand. RANKL/OPG system, MCSF and BMP-2 played an important role in the regulation of the osteoclastic and osteoblastic activities. Therefore, their gene expressions were measured in this study to better understand the mechanism of LPva. To the best of our knowledge, this is the first report on the molecular mechanism of LPv in preventing bone loss due to estrogen-deficient osteoporosis.
The function of OPG is to block the binding of RANKL to RANK receptors on committed pre-osteclastic cells[47]. Therefore, OPG is a potent anti-osteoclastogenic factor. Estrogen is known to stimulate production of OPG, while, estrogen deficiency leads to down-regulation of OPG[48]. As expected, in the present study, the OPG gene expression of the ovariectomised control group was found to be down-regulated. Both the LPva supplementation and ERT were able to revert back the OPG gene expression to sham levels. This study has shown that osteo-protective mechanism of LPva may be similar to ERT i.e. via stimulation of OPG production.
Estrogen deficiency led to up-regulation of pro-inflammatory cytokines such as TNF-α and interleukins[49, 50]. TNF is an important cofactor of bone resorption as it supports osteoclasts activation mediated by RANKL and c-Fms/MCSF. RANKL is a membrane-bound molecule of TNF ligand family which promotes osteoclasts formation[51]. In the present study, LPva may share similar mechanisms with ERT to protect bone as both were able to down-regulate the RANKL gene expression of ovariectomised rats.
This suggested a novel regulation of OPG and RANKL by LPva, which may help us to understand the mechanism of protection against estrogen-deficient bone loss. Interestingly, phytoestrogens such as genistein were also able to enhance osteoblastic OPG production through ER-dependent mechanisms and concurrently suppress RANKL gene expression which is associated with an inhibition of osteoclastogenesis[52–55]. Therefore, the phytoestrogenic element in LPva could be the reason for these novel findings.
We did not find any significant change in the MCSF gene expression after ovariectomy. An in vitro study of human endometrial stromal cells found that MCSF production was dose-dependently enhanced by the addition of sex hormone[56]. However, in this study, both ERT and LPva did not produce any significant changes in the MCSF gene expression. This meant that M-CSF was not affected in this model of osteoporosis.
BMP-2 plays an important role in bone repair and regeneration[31]. The BMP-2 gene expressions in the femora of ovariectomised rats were significantly increased by both LPva and ERT until they were similar to the sham level. Similar to our findings, Zhou et. al[57] also found that estrogen was able to activate BMP-2 gene transcription. Estrogen has been shown to stimulate the differentiation and activity of osteoblasts[58, 59] and increase bone formation and bone mass in animal models[60, 61]. Based on our results, the increased BMP-2 in LPva group was probably contributed by the phytoestrogenic effects of LPva.
Conclusions
As a conclusion, LPva is comparable to ERT in regulating OPG, RANKL and BMP-2 gene expressions of ovariectomised rats. Therefore, LPva has potential as an alternative to ERT for the treatment and prevention of estrogen-deficient osteoporosis. LPva may also be taken as supplements by postmenopausal women who are uncomfortable with the risk of serious side-effects with ERT.
References
Consensus Development Conference: Diagnosis, prophylaxis and treatment of osteoporosis. Am J Med. 1993, 94: 646-650.
World Health Organization: Summary Meeting Report. WHO Scientific Group on the Assessment of Osteoporosis at Primary Health Care Level. 2007, Brussels, Belgium: WHO Press, Geneva, 5–7 May 2004
Thomsen K, Godfredsen A, Christiansen C: Is Postmenopausal bone loss an age related phenomenon?. Calcif Tissue Int. 1986, 39: 123-127. 10.1007/BF02555106.
Ismail NMN: Postmenopausal osteoporosis: epidemiology, pathophysiology and treatment. Malaysian J Pathol. 1997, 19 (1): 21-25.
International Osteoporosis Foundation: Facts and statistics about osteoporosis and its impact. International osteoporosis foundation. J Bone Miner Res. 2009, 4: 113-118. 10.1002/jbmr.5650040116.http://www.iofbonehealth.org/facts-and-statistics.html,
Al-Azzawi F: Prevention of postmenopausal osteoporosis and associated fractures: clinical evaluation of the choice between estrogen and biphosphonates. Gynaecol Endrocrinol. 2008, 24: 601-609. 10.1080/09513590802296245.
Arcangelo VP, Peterson AM: Pharmacotherapeutics for advanced practice: a practical approach. 2005, USA: Lippincott Williams & Wilkins, 2
Rossouw J, Anderson G, Prentice R: Risks and benefits of estrogen plus progestin in postmenopausal women: principal results from the women’s health initiative randomized controlled trial. JAMA. 2002, 288: 321-333. 10.1001/jama.288.3.321.
Chlebowski RT, Hendrix SL, Langer RD, Stefanick ML, Gass M, Lane D, Rodabough RJ, Gilligan MA, Cyr MG, Thomson CA, Khandekar J, Petrovitch H, McTiernan A: Influence of estrogen plus progestin on breast cancer and mammography in healthy postmenopausal women: the women’s health Initiative randomized trial. JAMA. 2003, 289: 3243-3253. 10.1001/jama.289.24.3243.
Shumaker SA: Estrogen plus progestin and the incidence of dementia and mild cognitive impairment in postmenopausal women, the women’s health initiative memory studies: a randomized controlled trial. JAMA. 2003, 289: 2651-2662. 10.1001/jama.289.20.2651.
Devareddy L, Khalil DA, Smith BJ, Lucas EA, Soung DY, Marlow DD, Arjmandi BH: Soy moderately improves microstructural properties without affecting bone mass in an ovariectomized rat model of osteoporosis. Bone. 2006, 8: 686-693.
Devareddy L, Hooshmand S, Collins JK, Lucas EA, Chai SC, Arjmandi BH: Blueberry prevents bone loss in ovariectomized rat model of postmenopausal osteoporosis. J Nutr Biochem. 2008, 19: 694-699. 10.1016/j.jnutbio.2007.09.004.
He CC, Hui RR, Tezuka Y, Kadota S, Li JX: Osteoprotective effect of extract from achyranthes bidentata in ovariectomized rats. J Ethnopharmacol. 2010, 127: 229-234. 10.1016/j.jep.2009.11.016.
Shuid AN, Zulfadli M, Norliza M, Norazlina M, Ima Nirwana S: Vitamin E exhibit bone anabolic properties. Jour Bone Min Metab. 2010, 28: 149-156. 10.1007/s00774-009-0122-2.
Nazrun AS, Ping LL, Norliza M, Norazlina M, Nirwana SI: The effects of Labisia pumila var.alata on bone markers and bone calcium in a rat model of post-menopausal osteoporosis. J Ethnopharmacol. 2010, 133: 538-542.
Fathilah SN, Ahmad NS, Norazlina M, Norliza M, Nirwana SI: Labisia pumila protects the bone of estrogen-deficient rat model: a histomorphometric study. J Ethnopharmacol. 2012, 142: 294-299. 10.1016/j.jep.2012.04.029.
Fathilah SN, Shahrum M, Norazlina M, Ahmad NS: Labisia pumila prevents complications of osteoporosis by increasing bone strength in a rat model of postmenopausal osteoporosis. eCAM. 2012,doi:10.1155/2012/948080., 2012,
Stone BC: Notes on the genus Labisia Lindl. (Myrsinaceae). Malay Nat J. 1998, 42: 43-51.
Burkill IH: Dictionary of the Economic Products of the Malay Peninsula. 1935, London: Publisher Crown Agents for the Colonies
Runi SP: Studies on medicinal plant in Sarawak. Towards Bridging Science and Herbal Industry. Edited by: Chang YS. 2001, Kuala Lumpur: Forest Research Institute of Malaysia (FRIM), 112-119.
Zakaria M, Mohammed MA: Traditional Malay Medicinal Plants. 1994, Kuala Lumpur: Fajar Bakti
Jamia AJ, Houghton JP, Milligan RS, Jantan I: The oestrogenic and cyto- toxic effects of the extracts of Labisia pumila var. alata and Labisia pumila var. pumila in vitro. Jurnal Sains Kesihatan. 2003, 1: 53-60.
Husniza H: Estrogenic and Androgenic Activities of Kacip Fatimah (Labisia pumila). 2002, Kuala Lumpur: Abstracts of Research Projects, Institute of Medical Research, Ministry of Health Malaysia, 8-
Fazliana M, Wan Nazaimoon WM, Gua HF, Östensona CG: Labisia pumila extract regulates body weight and adipokines in ovariectomized rats. Maturitas. 2009, 62: 91-97. 10.1016/j.maturitas.2008.10.004.
Jamia AJ, Houghton JP, Milligan RS: Testing of Labisia pumila for oestro- genic properties using a recombinant yeast screen. J Pharm Pharmacol. 1998, 50: 79-10.1111/j.2042-7158.1998.tb02279.x.
Ayida AW, Wan Nazaimoon WM, Farihah HS, Azian AL: Effect of ovariectomy, Labisia Pumila var. alata treatment and estrogen replacement therapy on the morphology of adipose tissue in ovariectomized Sprague Dawley rats. J Med Biol Sc. 2007, 1: 1-7.
Teiteilbaum SL: Bone resorption by osteoclast. Science. 2000, 289: 1504-1508. 10.1126/science.289.5484.1504.
Lacey DL, Timms E, Tan HL, Kelley MJ, Dunstan CR, Elliott R, Colombero A, Elliott G: Osteoprotogerin ligand is a cytokine that regulated osteocast differentiation and activation. Cell. 1998, 93: 165-176. 10.1016/S0092-8674(00)81569-X.
Lewiecki EM: RANK ligand inhibition with denosumab for the management of osteoporosis. Expert Opin Biol Ther. 2006, 6: 1041-1050. 10.1517/14712598.6.10.1041.
Lloyd SAJ, Yuan YY, Kostenuik PJ, Ominsky MS, Lau AG: Soluble RANKL induces high bone turnover and decreases bone volume, density, and strength in mice. Calcif Tiss Int. 2008, 82 (5): 361-372. 10.1007/s00223-008-9133-6.
Riley EH, Lane JM, Urist MR, Lyons KM, Lieberman JR: Bone morphogenetic protein-2 biology and applications. Clin Orthop Rel Res. 1996, 324: 39-46.
Bord S, Ireland DC, Beavan SR, Compston JE: The effects of estrogen on osteoprotegerin, RANKL, and estrogen receptor expression in human osteoblasts. Bone. 2003, 32 (2): 136-141. 10.1016/S8756-3282(02)00953-5.
Siti Noor Fathilah AA: Branched DNA: a novel technique in molecular diagnostics. RUMeS. 2013, 1 (1): 27-29.
Boyle WJ, Simonest WS, Lacey DL: Osteoclast differentiation and activation. J Nat. 2003, 423: 337-342. 10.1038/nature01658.
Andras SC, Power JB, Cockin EC, Davey MR: Strategies for signal amplification in nucleic acid detection. Mol Biotechnol. 2001, 19 (1): 29-44.
Ferguson N: Osteoporosis in Focus. 2004, Oxford: Pharmaceutical Press
Wan Ezumi MF, Siti Amrah S, Suhaimi AWM, Mohsin SSJ: Evaluation of the female reproductive toxicity of aqueous extracts of Labisia pumila var. alata in rats. Indian J Pharmacol. 2007, 39: 30-32. 10.4103/0253-7613.30760.
Singh GD, Ganjoo M, Youssouf MS, Koul A, Sharma R, Singh S, Sangwan PL, Koul S, Ahamad DB, Johri RK: Sub-acute toxicity evaluation of an aqueous extract of Labisia pumila, a Malaysian herb. Food Chem Toxicol. 2009, 47: 2661-2665. 10.1016/j.fct.2009.07.031.
Arron JR, Choi Y: Bone versus immune system. Nature. 2000, 408: 535-536. 10.1038/35046196.
Lorenzo J: Interactions between immune and bone cells: new insights with many are remaining questions. JCI. 2000, 106: 749-752. 10.1172/JCI11089.
Choi HK, Kim DH, Kim JW, Ngadiran S, Sarmidi MR, Park CS: Labisia pumila extract protects skin cells from photoaging caused by UVB irradiation. J Biosc Bioeng. 2010, 109: 291-296. 10.1016/j.jbiosc.2009.08.478.
Fabien W, Laurent L, Veronique C, Jerome G, Yohann W: Oxidative stress bone remodelling and disease. Trends Mol Med. 2009, 15 (10): 468-475. 10.1016/j.molmed.2009.08.004.
Almeida M, Han L, Martin-Millan M, Plotkin LI, Stewart SA, Roberson PK, Kousteni S, O’Brien CA, Bellido T, Parfitt AM, Manolagas SC: Skeletal involution by age-associated oxidative stress and its acceleration by loss of sex steroids. J Biol Chem. 2007, 282: 27285-27297. 10.1074/jbc.M702810200.
Huang J, Zhang H, Shimizu N, Takeda T: Triterpenoid saponins from Arsidia mamillata. Phytochemistry. 2000, 54: 817-822. 10.1016/S0031-9422(00)00173-4.
Norhaiza M, Maziah M, Hakiman M: Antioxidative properties of leaf extracts of a popular Malaysian herb, Labisia pumila. J Med Plants Res. 2009, 3: 217-223.
Sies H, Stahl W: Vitamin E and C, beta carotene and other carotenoids as antioxidants. Am J Clin Nutr. 1995, 62: 1315S-1321S.
Hofbauer LC, Khosla S, Dunstan CR, Lacey DL, Spelsberg TC, Riggs BL: Estrogen stimulates gene expression and protein production of osteoprotegerin in human osteoblastic cells. Endocrinol. 1999, 140: 4367-4370. 10.1210/en.140.9.4367.
Cenci S, Weitzmann MN, Roggia C, Namba N, Novack D, Woodring J, Pacifici R: Estrogen deficiency induces bone loss by enhancing T-cell production of TNF-α. JCI. 2000, 106: 1229-1237. 10.1172/JCI11066.
Jilka RL: Cytokines, bone remodeling, and estrogen deficiency. Bone. 1998, 23: 75-81. 10.1016/S8756-3282(98)00077-5.
Papanicolaou DA, Wilder RL, Manolagas SC, Chrousos GP: The pathophysiologic roles of interleukin-6 in human disease. Ann Intern Med. 1998, 128: 127-137. 10.7326/0003-4819-128-2-199801150-00009.
Fuller K, Wong B, Choi Y, Chambers TJ: TRANCE is necessary and sufficient for osteoblast-mediated activation of bone resorption. J Exp Med. 1998, 188: 997-1001. 10.1084/jem.188.5.997.
Flagella M, Bui S, Zheng Z, Nguyen CT, Zhang A, Pastor L, Ma Y, Yang W, Crawford KL, McMaster GK, Witney F, Luo Y: A multiplex branched DNA assay for parallel quantitative gene expression profiling. Anal Biochem. 2006, 352 (1): 50-60. 10.1016/j.ab.2006.02.013.
Chen XW, Garner SC, Anderson JJ: Isoflavones regulate interleukin-6 and osteoprotegerin synthesis osteoblast cell differentiation via an estrogen-receptor dependent pathway. Biochem Biophys Res Commun. 2002, 295: 417-422. 10.1016/S0006-291X(02)00667-8.
Viereck V, Gründker C, Blaschke S, Siggelkow H, Emons G, Hofbauer LC: Phytoestrogen genistein stimulates the production of osteoprotegerin by the human trabecular osteoblasts. J Cell Biochem. 2002, 84: 725-735. 10.1002/jcb.10087.
Yamagishi T, Otsuka E, Hagiwara H: Reciprocal control of expression of mRNAs for osteoclast differentiation factor and OPG in osteogenic stromal cells by genistein: evidence for the involvement of topoisomerase II in osteoclastogenesis. Endocrinol. 2001, 142: 3632-3637. 10.1210/en.142.8.3632.
Kanzaki H, Hatayama H, Narukawa S, Kariya M, Fujita J, Mori T: Hormonal regulation in the production of macrophage colony-stimulating factor and transforming growth factor-beta by human endometrial stromal cells in culture. Horm Res. 1995, 44 (S2): 30-35.
Zhou S, Turgeman G, Harris SE, Leitman DC, Komm BS, Bodine PV, Gazit D: Estrogens activate bone morphogenetic protein-2 gene transcription in mouse mesenchymal stem cells. Mol Endocrinol. 2003, 17 (1): 56-66. 10.1210/me.2002-0210.doi:10.1210/me.2002-0210.,
Komm BS, Terpening CM, Benz DJ, Graeme KA, Gallegos A, Korc M, Greene GL, O’Malley BW, Haussler MR: Estrogen binding, receptor mRNA, and biologic response in osteoblast-like osteosarcoma cells. Science. 1988, 241: 81-84. 10.1126/science.3164526.
Ernst M, Heath JK, Rodan GA: Estradiol effects on proliferation, messenger ribonucleic acid for collagen and insulin-like growth factor-I, and parathyroid hormone-stimulated adenylate cyclase activity in osteoblastic cells from calvariae and long bones. Endocrinol. 1989, 125: 825-833. 10.1210/endo-125-2-825.
Takano-Yamamoto T, Rodan GA: Direct effects of 17b-estradiol on trabecular bone in ovariectomized rats. PNAS. 1990, 87: 2172-2176. 10.1073/pnas.87.6.2172.
Chow JWM, Lean JM, Chambers TJ: 17b-Estradiol stimulates cancellous bone formation in female rats. Endocrinol. 1992, 130: 3025-3032. 10.1210/en.130.5.3025.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1472-6882/13/217/prepub
Acknowledgements
We are grateful to the staff of the Pharmacology Department, UKM Medical Centre for their technical support and Dr Thuan D. Bui for his contribution in helping with the data analysis of this study. We also thank the Faculty of Medicine Universiti Kebangsaan Malaysia and the Ministry of Higher Education for providing the grant FRGS, UKM-FF-03-FRGS0047-2009 for this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare to have no conflict of interest whatsoever. The authors alone are responsible for the content and writing of this paper.
Authors’ contributions
ANS, INS and INM designed the study. SNF carried out the study and collected the samples. NM and NM participated in the statistical analysis. SNF and ANS drafted the manuscript. INS, INM, NM and NM read and edited the manuscript. All authors approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Fathilah, S.N., Mohamed, N., Muhammad, N. et al. Labisia pumila regulates bone-related genes expressions in postmenopausal osteoporosis model. BMC Complement Altern Med 13, 217 (2013). https://doi.org/10.1186/1472-6882-13-217
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1472-6882-13-217