Abstract
Background
Women can choose from a range of contraceptive methods that differ in important ways. Inadequate decision support may lead them to select a method that poorly fits their circumstances, leading to dissatisfaction, misuse, or nonuse. Decision support interventions, such as decision aids, may help women choose a method of contraception that best fits their personal circumstances. To guide future decision aid development, we aim to summarize the attributes of contraceptive methods included in available decision aids as well as surveys and interviews of women actively choosing a contraceptive method.
Methods
We conducted a systematic review to identify attributes of contraceptive methods that may be important to women when engaging in this decision making process. We performed a database search of MEDLINE/PubMed, Ovid EMBASE, OVID CENTRAL, Ovid PsycInfo, EBSCO CINAHL, Popline, and Scopus from 1985 until 2013 to identify decision aids, structured interviews and questionnaires reporting attributes of contraceptive options that are of importance to women. A free-text internet search was also performed to identify additional decision support tools. All articles and tools were reviewed in duplicate for inclusion, and a summary list of attributes was compiled.
Results
We included 20 surveys, 1 semistructured interview report and 19 decision aids, reporting 32 unique attributes. While some attributes were consistently included in surveys/interviews and decision aids, several were included more often in decision aids as opposed to surveys/interviews (e.g., STI prevention, noncontraceptive benefits, how the method is used, requirement of a healthcare provider), and vice versa (e.g., a woman’s vicarious experience with contraceptive methods). Key attributes mentioned in both surveys/interviews and decision aids include efficacy (29 total mentioned) and side effects/health risks (28 total mentioned). While a limited number of decision support tools were formally evaluated, many were not rigorously studied.
Conclusions
Many attributes were identified as potentially important to women choosing a method of contraception, but these were inconsistently included in the reviewed resources. Formal evaluation of decision support tools for contraceptive choice and involvement of users in the development process may lead to more user-centered design and implementation.
Similar content being viewed by others
Background
Contraceptive use is widespread in the United States, with 99% of sexually active women in the United States having used a form of contraception at some time [1]. Currently, 62% of all women of childbearing age use some form of contraception. Use is inconsistent, however, and 11% of women who are at risk of unintended pregnancy are not using any form of contraception [1]. Moreover, nearly half (49%) of all pregnancies in the United States are unintended [2]. The finding that 95% of these unintended pregnancies are due to inconsistent and non-use of contraceptives despite their wide availability indicates that the problem is not the efficacy of contraception—the problem is whether people will use contraception and use it consistently [3].
When choosing a method of contraception, women are faced with a wide range of options and various attributes associated with these options to consider. When faced with complex decisions in the absence of adequate decision support, some women inevitably choose a method that does not optimally fit their personal circumstances. This poor “fit” is reflected in the fact that 40% of married women and 61% of unmarried women in the United States change contraceptive methods within a two-year period [4]. Some of this method switching may also be attributed to women’s evolving needs and highlights that women frequently re-visit this decision.
Shared decision making (SDM) is a process whereby a person makes decisions with a healthcare professional, considering the available evidence regarding options being considered, in the context of the person’s needs, values and preferences [5]. Increasingly, women are requesting the SDM approach in contraceptive choice [6]. Decision aids (DAs) can facilitate SDM by presenting complex and multifaceted attributes of these options in ways that are both evidence-based and easy for users to understand [7]. Because of the complexity of options and attributes about each to be considered, DAs may usefully facilitate the choice of contraception methods [8].
In order to understand if existing tools fit the needs of users, and to inform the development of future DAs for women considering contraception, we systematically assessed whether the attributes of contraceptive options that women are considering align with those reported in available contraception decision support tools.
Methods
A librarian experienced with performing systematic reviews related to SDM (P.E.) performed a literature search through MEDLINE/PubMed, Ovid EMBASE, OVID CENTRAL, Ovid PsycInfo, EBSCO CINAHL, Popline, and Scopus, from 1985 until January 2013. The strategy comprised subject headings and textwords describing all forms of family planning and reproductive control for women. This conceptual grouping was matched with methods to communicate with the person and facilitate informed choice, such as DAs, person education techniques, and pamphlets. Sample search strategies are included in Additional file 1. Authors were not contacted to identify additional studies.
Eligible studies were experimental or observational studies of any design published in English with or without comparator groups and targeting any population. Given the nature of our question, qualitative studies were included. Reports should describe the application of a DA or other method (e.g., survey, semi-structured interview) intended to facilitate sharing of information during a clinical encounter or in the setting of an actual decision about contraception (whether during or outside of the clinical encounter) and should report attributes relevant to a woman’s choice of contraception. Decision aids were not required to meet specific criteria in order to be included. Surveys of women not actively considering contraceptives were not eligible for inclusion. Studies were included regardless of reported outcomes.
In an effort to be as inclusive as possible, we also conducted free-text internet searches to identify online DAs for contraception that may not have been published in the database-indexed literature or formally studied. Inclusion of these resources was based on consensus of two reviewers.
Analysis
All attributes included in included resources were extracted and added to a master list. The master list was then examined for related attributes that could be classified together under a single category, and a reclassification round was used to confirm the stability of these categories. The main reviewer (K.D.W) and a second reviewer (A.L.) met at each stage to achieve consensus on attribute identification and classification; also, a 10% sample was extracted in duplicate by an independent reviewer to ensure the reproducibility of the process. Extraction was not confirmed with study/tool authors.
Results
Search results
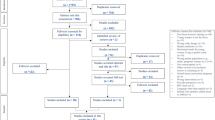
Figure 1 reveals the flow of our search and selection process resulting in 28 articles for inclusion (10 surveys, 1 semi-structured interview, 7 DAs, 10 DA + survey), of which two (one DA only and one DA + survey) did not report the attributes sufficiently for extraction of meaningful data to be performed. Common reasons for articles not being included were not reporting on a method of patient engagement and not being used in the context of an actual decision regarding contraception. Five articles reported on the World Health Organization (WHO) Decision-making Tool for Family Planning Clients and Providers (DMT) and were considered together. Eight other DAs were found online only. Table 1 describes included resources (19 unique decision aids, 20 surveys, and 1 semistructured interview) from which we could extract meaningful data. These surveys, interview, and decision aids have been used in the United States, Europe and the developing world.
Of the studies reporting decision aids, only five were randomized trials. One study utilized a pseudo-randomized design, six were quazi-experimental (usually comparing pre- and post-implementation of intervention), and five evaluated the decision aid with a questionnaire after use (with or without pre-intervention questionnaire). Details on the reported processes for developing included decision aids are reported in Additional file 2.
Overarching categories
After creating and reviewing the master list of attributes from the included resources, 32 unique attributes were identified. Each of these could be classified in one of four overarching categories, which were chosen by the authors after review of the master list: Mechanistic, Method Effect, Social/Normative, Practical (Table 2). An earnest effort was made to avoid redundant attributes and classify each attribute under only one overarching category, realizing that attributes and overarching categories are not mutually exclusive. Mechanistic captured aspects of how the method is used, including some implied considerations, such as whether the method required use of a needle or hormones and whether the method could be used post-coital (i.e., used after unprotected intercourse to prevent pregnancy). Method effect included the method’s efficacy for pregnancy prevention and noncontraceptive effects, including side effects, health risks, health benefits, and menstrual changes. Social/Normative encompassed how internal influences—such as a person’s prior experience or expectations—and external influences—such as vicarious experience (i.e., a woman’s understanding of contraceptive use as obtained through others [e.g., family and friends] who have used the methods and shared their experience) and partner support—impact contraceptive choice. Practical included attributes such as a person’s ability to obtain the method and the attribute’s compatibility with their means and sexual experiences.
Attributes included in individual resources
Figure 2 shows the number of resources that mentioned each attribute. Because decision aids and surveys from the same paper do not necessarily include the same attributes, they do not necessarily lead to a mirrored appearance when added to the figure. In general, efficacy and side effects/health risks were prominent attributes in both surveys/interviews and DAs. Several attributes included in decision aids were not mentioned in surveys/interviews (i.e., needle phobia, post-coital, pre-sex preparation, postpartum compatibility, alarm signs, religious considerations).
Comparison of surveys/interviews and DAs
While the limited number of resources precludes a quantitative statistical comparison of how often surveys/interviews versus DAs included each issue, some tentative observations can be made. Some issues were highlighted more often in decision aids compared to surveys/interviews: STI prevention (11 vs. 4), noncontraceptive benefits (11 vs. 4), how used (9 vs. 2), cost (6 vs. 2), and requirement of healthcare provider (4 vs. 1). A woman’s vicarious experience with contraceptive methods was considered more often in surveys/interviews than decision aids (8 vs. 1).
Discussion
We summarize a number of surveys and decision aids that uncover which issues women may consider when choosing a method of contraception. Our results revealed that there are many important attributes women may consider when choosing among contraceptive methods and that these attributes are themselves heterogeneous in the way they are experienced (and named). While some tools (e.g., the WHO DMT) have been rigorously studied, many (in particular, the online tools) remain unstudied. Given that many women may be turning to online resources to help them make decisions about contraception, evaluation of these tools is imperative to ensure that tools address the needs of their users.
It is also imperative that decision making tools are evidence-based and that intended users are included in the development process to ensure that relevant attributes are considered. Tools can only be effective if they address the needs of their users, and in the case of contraceptive choice, this means addressing the attributes about methods that matter most to women. However, this goal sometimes proves elusive, as contraceptive choice is influenced by a multitude of socio-cultural, geographical, and personal factors such that a one-size-fits-all approach may not work. For instance, cost may not be a concern in areas where contraception is provided at no cost to the user, and menstrual changes could be seen as a positive or negative aspect of a contraceptive method, depending on the user. Moreover, the issues that matter most to a woman at a given point in her life may be different later on in life. The diversity of factors that influence contraceptive choice is likely reflected in the heterogeneity of issues included in the resources we reviewed—while some of the medical issues (e.g., efficacy, STI prevention, side effects) were almost unanimously included, some more practical considerations such as the burden of use associated with the method and socio-cultural attitudes about the methods were less-often considered.
Indeed, it was striking to see the differences observed in how frequently and inconsistently many issues were included in surveys/interviews compared to DAs. Medical considerations, such as STI prevention, noncontraceptive benefits, and requirement of a healthcare provider were highlighted more often in decision aids compared to surveys/interviews. In contrast, the vicarious experiences of women were considered in surveys/interviews far more often than decision aids. While we have no gold standard to identify the “true” perspective of women, if we assume that the surveys/interviews reflect the true perspective of women, the discrepancies observed between attributes included in surveys/interviews and DAs suggest that the true perspectives of users are not being reflected in the available tools. This is to say that tools may be including medical issues that women do not consider very important in lieu of including practical issues that matter to them more. Alternatively, given that many of the attributes included in surveys/interviews were investigator-driven, it is possible that both the surveys/interviews and DAs both may be reflective of investigator biases as opposed to what truly matters to women. A third hypothesis is that contraceptive choice is such an individualized process that surveys and decision aids will always show variability in the issues they include based on who the users are. While it is clear that all of the issues we listed are important to some extent, some will be more important than others, and the relative importance of each will vary from user to user. Future decision aids need to keep this in mind and may need to be tailored to individual populations. Qualitative research within a target population may be useful prior to implementing a decision aid to ensure that the aid is of the utmost relevance to its users.
As the issues emphasized in DAs appear to reflect what providers feel are important to women when choosing a method of contraception, it remains unclear how providers influence patients’ choice of contraceptives and whether provider influence is concordant with patient preference. An international study of women in the United States and Europe observed that physicians have the greatest influence on what type of contraception women choose, with over half of all women seeking advice from health care professionals and less seeking this advice from family, friends, or the internet [46]. Another large study of over 18,000 women demonstrated that nearly half (47%) chose a different method than the one they originally planned to choose after receiving counseling from a health care provider [47]. This highlights the key role that providers play in influencing women’s choice of contraception.
Although patients want their physicians to be involved in contraception decisions, they want this involvement in the context of choosing a method that fits their personal values and preferences [6]. Do recommendations made by health professionals reflect their own personal biases or their patients’ true preferences and values? To examine the role provider preference plays on recommendations they make to patients, an international study of healthcare providers (over two-thirds of which were obstetrician-gynecologists) examined providers’ own choice of contraception, reasons for choice, and if these choices are concordant with recommendations they make to patients. The majority of healthcare providers used an intrauterine device, and most common reasons for use among these providers included the method matching their family situation (28%) and contraceptive efficacy (22.8%). These providers were more likely than others to recommend the method for patients who have completed planned childbearing (p < 0.001), and they were also more likely to not recommend oral contraceptives for patients who have not completed their childbearing plans (p = 0.011). This suggests that providers who use an intrauterine device are more likely to recommend to patients the method they use in favor of those they do not, and the reasons providers choose a contraceptive method may differ from reasons their patients do [48].
How do we, then, ensure that tools reflect the needs of their users (i.e., women)? Certainly, individualizing decision aids presents challenges. If a decision aid were to present all 32 unique attributes we list across the approximately 20 contraceptive methods available, it would certainly be unwieldy and introduce a heavy cognitive burden. Computer-based tools are a natural solution to this problem, as they provide a means to develop modular and easily-adaptable decision aids. For example, a decision aid could only present the options available to a woman based on stated preferences (e.g., permanent sterilization methods can be excluded if she states a preference for future childbearing) and could present only the attributes about these methods that a woman deems important. Indeed, some online tools we reviewed have taken this approach.
Development of modular tools for low-resource settings, however, produces certain challenges, as cost and the need for electricity limit use of computer-based decision aids. In the past, our group has developed decision aids using an “issue cards” approach, where users are given several cards, each which highlights a certain attribute about treatment options (e.g., cost, side effects, how it is used) compares across all of the options available to the user [49]. In low-resource settings, this design may be more feasible as the number of contraceptive options may be limited on the basis of availability. In this case, cards would only need to include the few options available, and a card could be generated for each attribute, with only the most relevant attribute cards being presented to the woman based on stated or elicited preferences.
Given recent advances in technology, computer-based solutions may not be far out of reach for low-resource settings. In 2007, Amazon.com introduced the Kindle E-reader. Initially designed as a book reader and sold for $399 USD, it featured a “e-ink” display which presents text and graphics on a screen with minimal glare and ultra-low power usage [50]. Today, a Kindle retails for $69 USD and can last weeks on a single charge [51]. The low power usage makes the device attractive for use in low-resource settings, and the low-glare screen is beneficial if used outdoors in the sun. Versions of the Kindle offer global cellular connectivity, permitting for wireless delivery of content to remote locations [52]. Based on its low cost, the Kindle may be a feasible computer-based decision aid delivery device for low-resource settings. To our knowledge, the Kindle has not been used as a decision aid delivery device before.
Certainly, factors other than the content of a decision aid will influence whether it is effective. While many of these aspects have not been formally studied, recent work from our group [Under review in Implementation Science] has shown that when providers do not use decision aids as intended, that providers involve patients less and knowledge transfer suffers. Therefore, effective training interventions which ensure proper use of decision aids may make these tools more effective.
This study has several important limitations. For one, the degree to which each attribute was deemed important to women was not included in all studies nor was the quality of the evidence and risk of bias able to be assessed, given that unpublished online tools were included and these tools were not necessarily subject to quality control measures. Moreover, the major source of bias identified was that investigators often selected the items included on surveys and decision aids. This limited our ability to prioritize attributes according to relative importance and quality of evidence but did not impair our ability to generate a master list and classify attributes from which women might choose the most pertinent and important to them. Future meta-analysis could attempt to summarize how important women deem each attribute in relation to others to understand general trends, realizing that these preferences vary from woman to woman. The search strategy and extraction process also had several limitations, including that the search strategy did not provide a means for including paper-based decision aids that were not published in academic journals, the online search for “gray literature” was not systematic (and could have been affected by selection bias), and additionally, only 10% of data was extracted by 2 people independently. Strengths included the systematic search and duplicate study selection process.
Overall, contraceptive choice is a complex decision, marked with multiple considerations that must be carefully deliberated across an assortment of options. Moreover, the attributes that matter most differ from woman to woman based on individual context and may change for a given woman over time. Given the complexity of this decision, DAs might help women choose birth control methods that fit their values, needs and preferences. Ideally, if women find methods that fit their needs, values and preferences, this will lower rates of inconsistent use and nonuse and limit unintended pregnancies. While many DAs exist, they remain poorly studied, and aspects of effective DAs for contraceptive choice (including the attributes of methods that should be included) remain unclear. Here, we provide a framework for future DA development that takes into account attributes that may be considered when choosing a method of contraception and gives consideration for low-resource settings.
Conclusions
Many attributes were identified as potentially important to women choosing a method of contraception, but these were inconsistently included in the reviewed resources, perhaps reflecting the individualized nature of contraceptive choice. Decision aids should be tailored to include the attributes that are most important to users.
Additional resources
Readers interested in the community-level version of the WHO DMT may find it at http://www.who.int/reproductivehealth/publications/family_planning/9789241503754/en/index.html. WHO also publishes a decision making tool for people living with HIV that can be found online: http://www.who.int/reproductivehealth/publications/family_planning/9241595132/en/index.html.
References
Mosher W, Jones J: Use of contraception in the United States: 1982–2008. Vital Health Stat. 2010, Series 23, No 29
Finer LB, Zolna MR: Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011, 84: 478-485. 10.1016/j.contraception.2011.07.013. doi:410.1016/j.contraception.2011.1007.1013. Epub 2011 Aug 1024
Fact sheet: contraceptive use in the United States. [http://www.guttmacher.org/pubs/fb_contr_use.html]
Grady WR, Billy JO, Klepinger DH: Contraceptive method switching in the United States. Perspect Sex Reprod Health. 2002, 34: 135-145. 10.2307/3097712.
Makoul G, Clayman ML: An integrative model of shared decision making in medical encounters. Patient Educ Couns. 2006, 60: 301-312. 10.1016/j.pec.2005.06.010.
Dehlendorf C, Levy K, Kelley A, Grumbach K, Steinauer J: Women’s preferences for contraceptive counseling and decision making. Contraception. 2013, 88: 250-256. 10.1016/j.contraception.2012.10.012. doi: 210.1016/j.contraception.2012.1010.1012. Epub 2012 Nov 1021
Barry MJ: Health decision aids to facilitate shared decision making in office practice. Ann Intern Med. 2002, 136: 127-135. 10.7326/0003-4819-136-2-200201150-00010.
French RS, Wellings K, Cowan FM: How can we help people to choose a method of contraception? The case for contraceptive decision aids. J Fam Plann Reprod Health Care. 2009, 35: 219-220. 10.1783/147118909789587169.
Adinma JIB, Agbai AO, Nwosu BO: Contraceptive choices among Nigerian women attending an antenatal clinic. Adv Contracept. 1998, 14: 131-145. 10.1023/A:1006590717562.
Ameh N, Sule ST: Contraceptive choices among women in Zaria, Nigeria. Niger J Clin Pract. 2007, 10: 205-207.
Amin R: Choice of contraceptive method among females attending family planning center in Hayat Abad Medical Complex, Peshawar. J Pak Med Assoc. 2012, 62: 1023-1028.
Balanced counseling strategy plus: a toolkit for family planning service providers working in high HIV/STI prevalence settings (BCS+). [http://www.popcouncil.org/pdfs/2012RH_BCSPlusCounselingCards.pdf]
Method explorer. [http://bedsider.org/methods]
Side by side. [http://bedsider.org/methods/matrix]
Build your own. [http://bedsider.org/methods/side_by_side]
Chewning B, Mosena P, Wilson D, Erdman H, Potthoff S, Murphy A, Kuhnen KK: Evaluation of a computerized contraceptive decision aid for adolescent patients. Patient Educ Couns. 1999, 38: 227-239. 10.1016/S0738-3991(99)00014-2.
Chin-Quee DS, Janowitz B, Otterness C: Counseling tools alone do not improve method continuation: further evidence from the decision-making tool for family planning clients and providers in Nicaragua. Contraception. 2007, 76: 377-382. 10.1016/j.contraception.2007.07.003.
Johnson SL, Kim YM, Church K: Towards client-centered counseling: development and testing of the WHO decision-making tool. Patient Educ Couns. 2010, 81: 355-361. 10.1016/j.pec.2010.10.011.
Kim YM, Davila C, Tellez C, Kols A: Evaluation of the World Health Organization’s family planning decision-making tool: improving health communication in Nicaragua. Patient Educ Couns. 2007, 66: 235-242. 10.1016/j.pec.2006.12.007.
Kim YM, Kols A, Martin A, Silva D, Rinehart W, Prammawat S, Johnson S, Church K: Promoting informed choice: evaluating a decision-making tool for family planning clients and providers in Mexico. Int Fam Plan Perspect. 2005, 31: 162-171. 10.1363/3116205.
Langston AM, Rosario L, Westhoff CL: Structured contraceptive counseling–a randomized controlled trial. Patient Educ Couns. 2010, 81: 362-367. 10.1016/j.pec.2010.08.006.
Decision-making tool for family planning clients and providers. [http://whqlibdoc.who.int/publications/2005/9241593229_eng.pdf]
Choosing wisely (Birth control selection tool). [http://www.sexualityandu.ca/games-and-apps/choosing-wisely-birth-control-selection-tool]
Costa ARR, Palma F, Sa JL, Vicente L, Bombas T, Nogueira AM, Rocha P: Impact of a women’s counselling programme on combined hormonal contraception in Portugal - The IMAGINE Study. Eur J Contracept Reprod Health Care. 2011, 16: 409-417. 10.3109/13625187.2011.608441.
Egarter C, Grimm C, Nouri K, Ahrendt HJ, Bitzer J, Cermak C: Contraceptive counselling and factors affecting women’s contraceptive choices: results of the CHOICE study in Austria. Reprod BioMed Online. 2012, 24: 692-697. 10.1016/j.rbmo.2011.12.003.
Fait T: Combined hormone contraceptive choice experience in Czech Republic. Cent Eur J Med. 2011, 6: 582-587. 10.2478/s11536-011-0062-9.
Garbers S, Meserve A, Kottke M, Hatcher R, Ventura A, Chiasson MA: Randomized controlled trial of a computer-based module to improve contraceptive method choice. Contraception. 2012, 86: 383-390. 10.1016/j.contraception.2012.01.013.
Gold MA, Coupey SM: Young women’s attitudes toward injectable and implantable contraceptives. J Pediatr Adolesc Gynecol. 1998, 11: 17-24. 10.1016/S1083-3188(98)70102-0.
Goldstuck ND: Factors influencing the initial decision to use an intrauterine device. Br J Clin Pract. 1989, 43: 173-176.
Johnson LK, Edelman A, Jensen J: Patient satisfaction and the impact of written material about postpartum contraceptive decisions. Am J Obstet Gynecol. 2003, 188: 1202-1204. 10.1067/mob.2003.308.
Leon FR, Brambila C, de la Cruz M, Colindres JG, Morales C, Vasquez B: Providers’ compliance with the balanced counseling strategy in Guatemala. Stud Fam Plan. 2005, 36: 117-126. 10.1111/j.1728-4465.2005.00049.x.
Lete I, Doval JL, Perez-Campos E, Sanchez-Borrego R, Correa M, de la Viuda E, Gomez MA, Gonzalez JV, Lertxundi R, Martinez MT, et al: Factors affecting women’s selection of a combined hormonal contraceptive method: the TEAM-06 Spanish cross-sectional study. Contraception. 2007, 76: 77-83. 10.1016/j.contraception.2007.04.014.
Madden T, Mullersman JL, Omvig KJ, Secura GM, Peipert JF: Structured contraceptive counseling provided by the contraceptive CHOICE Project. Contraception. 2012, 88 (2): 243-249.
Merckx M, Donders GG, Grandjean P, Van De Sande T, Weyers S: Does structured counselling influence combined hormonal contraceptive choice?. Eur J Contracept Reprod Health Care. 2011, 16: 418-429. 10.3109/13625187.2011.625882.
Method match. [http://www.arhp.org/methodmatch/]
My contraception tool. [http://www.brook.org.uk/contraception/my-contraception-tool]
My method. [http://www.plannedparenthood.org/all-access/my-method-26542.htm]
Proctor A, Jenkins TR, Loeb T, Elliot M, Ryan A: Patient satisfaction with 3 methods of postpartum contraceptive counseling: a randomized, prospective trial. J Reprod Med. 2006, 51: 377-382.
Rubin SE, Winrob I: Urban female family medicine patients’ perceptions about intrauterine contraception. J Women's Health. 2010, 19: 735-740. 10.1089/jwh.2009.1549.
Steiner MJ, Dalebout S, Condon S, Dominik R, Trussell J: Understanding risk: a randomized controlled trial of communicating contraceptive effectiveness. Obstet Gynecol. 2003, 102: 709-717. 10.1016/S0029-7844(03)00662-8.
Steiner MJ, Trussell J, Mehta N, Condon S, Subramaniam S, Bourne D: Communicating contraceptive effectiveness: a randomized controlled trial to inform a World Health Organization family planning handbook. Am J Obstet Gynecol. 2006, 195: 85-91. 10.1016/j.ajog.2005.12.053.
Venkat P, Masch R, Ng E, Cremer M, Richman S, Arslan A: Knowledge and beliefs about contraception in urban Latina women. J Community Health. 2008, 33: 357-362. 10.1007/s10900-008-9100-1.
Vogt C, Schaefer M: Disparities in knowledge and interest about benefits and risks of combined oral contraceptives. Eur J Contracept Reprod Health Care. 2011, 16: 183-193. 10.3109/13625187.2011.561938.
Wall EM: Development of a decision aid for women choosing a method of birth control. J Fam Pract. 1985, 21: 351-355.
Weldegerima B, Denekew A: Women’s knowledge, preferences, and practices of modern contraceptive methods in Woreta, Ethiopia. Res Social Adm Pharm. 2008, 4: 302-307. 10.1016/j.sapharm.2007.10.001.
Johnson S, Pion C, Jennings V: Current methods and attitudes of women towards contraception in Europe and America. Reprod Health. 2013, 10: 7-10.1186/1742-4755-10-7. doi:10.1186/1742-4755-10-7
Bitzer J, Gemzell-Danielsson K, Roumen F, Marintcheva-Petrova M, van Bakel B, Oddens BJ: The CHOICE study: effect of counselling on the selection of combined hormonal contraceptive methods in 11 countries. Eur J Contracept Reprod Health Care. 2012, 17: 65-78. 10.3109/13625187.2011.637586. doi:10.3109/13625187.13622011.13637586
Gemzell-Danielsson K, Cho S, Inki P, Mansour D, Reid R, Bahamondes L: Use of contraceptive methods and contraceptive recommendations among health care providers actively involved in contraceptive counseling–results of an international survey in 10 countries. Contraception. 2012, 86: 631-638. 10.1016/j.contraception.2012.06.002. doi: 610.1016/j.contraception.2012.1006.1002. Epub 2012 Jul 1016
Mullan RJ, Montori VM, Shah ND, Christianson TJ, Bryant SC, Guyatt GH, Perestelo-Perez LI, Stroebel RJ, Yawn BP, Yapuncich V, et al: The diabetes mellitus medication choice decision aid: a randomized trial. Arch Intern Med. 2009, 169: 1560-1568. doi: 1510.1001/archinternmed.2009.1293
Press release: introducing Amazon kindle. [http://phx.corporate-ir.net/phoenix.zhtml?c=176060&p=irol-newsArticle&ID=1079388]
Kindle with global wireless. [http://client0.cellmaps.com/tabs.html#cellmaps_intl_tab]
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1472-6874/14/28/prepub
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests. This study had no specific funding source.
Authors’ contributions
KW envisioned the study, performed the majority of data extraction, and drafted the first draft of the manuscript. RA aided in data extraction, assisted in analysis of the results, and made substantial contributions to the early drafts of the manuscript. DC and JB aided in analysis of the results and provided critical revisions to later versions of the manuscript. VM and AL contributed to the design of the study, analysis of the results, and provided critical revisions to the manuscript. PE aided in the design of the study, including development of the literature search, and provided critical revisions to the manuscript. All authors have approved this final version of the manuscript for publication.
Electronic supplementary material
12905_2013_392_MOESM2_ESM.doc
Additional file 2: Details extracted from published studies regarding the process for designing decision aids, when reported.(DOC 48 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Wyatt, K.D., Anderson, R.T., Creedon, D. et al. Women’s values in contraceptive choice: a systematic review of relevant attributes included in decision aids. BMC Women's Health 14, 28 (2014). https://doi.org/10.1186/1472-6874-14-28
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1472-6874-14-28