Abstract
Background
It has become increasingly clear that β-cell failure plays a critical role in the pathogenesis of type 2 diabetes. Free-radical mediated β-cell damage has been intensively studied in type 1 diabetes, but not in human type 2 diabetes. Therefore, we studied the protein expression of the DNA repair enzyme Ogg1 in pancreases from type 2 diabetics. Ogg1 was studied because it is the major enzyme involved in repairing 7,8-dihydro-8-oxoguanosine DNA adducts, a lesion previously observed in a rat model of type 2 diabetes. Moreover, in a gene expression screen, Ogg1 was over-expressed in islets from a human type 2 diabetic.
Methods
Immunofluorescent staining of Ogg1 was performed on pancreatic specimens from healthy controls and patients with diabetes for 2–23 years. The intensity and islet area stained for Ogg1 was evaluated by semi-quantitative scoring.
Results
Both the intensity and the area of islet Ogg1 staining were significantly increased in islets from the type 2 diabetic subjects compared to the healthy controls. A correlation between increased Ogg1 fluorescent staining intensity and duration of diabetes was also found. Most of the staining observed was cytoplasmic, suggesting that mitochondrial Ogg1 accounts primarily for the increased Ogg1 expression.
Conclusion
We conclude that oxidative stress related DNA damage may be a novel important factor in the pathogenesis of human type 2 diabetes. An increase of Ogg1 in islet cell mitochondria is consistent with a model in which hyperglycemia and consequent increased β-cell oxidative metabolism lead to DNA damage and the induction of Ogg1 expression.
Similar content being viewed by others
Background
It has become increasingly clear that β-cell failure plays a critical role in the pathogenesis of type 2 diabetes (for a review see [1]). Normally, increased peripheral insulin resistance and consequent insulin demand are met by increased β-cell activity and/or β-cell mass. Failure of β-cells to meet the demand for increased insulin secretion leads to overt diabetes [2–4]. The mechanisms behind the β-cell failure are less well understood, but a number of factors have been implicated, including hyperlipedemia [5], supraphysiological concentrations of circulating glucose [6, 7], formation of intra- and extra-cellular islet amyloid deposits [8], or a combination of these factors. Amyloid deposition has been shown to trigger β-cell apoptosis and necrosis [9]. Lipotoxicity causes β-cell dysfunction by inhibiting insulin secretion [10] and by direct cytotoxicity [11]. β-cell glucotoxicity has been described both in rodents and humans leading to apoptosis, decreased cell division and effects on transcriptional factor expression [6, 7, 12–16]. However, the relative contributions of these different mechanisms to β-cell failure remains unknown.
Free radicals and DNA-damage in diabetes
Free-radicals (e.g., superoxide, hydroxyl radicals, nitric oxide and peroxynitrite) have long been thought to be a key element in the cellular dysfunction and death that are central to the pathogenesis of many aspects of diabetes. In type 1 diabetes, it has been shown that inflammatory cytokines play a central role in the destruction of insulin producing β-cells [17–19], resulting in the production of oxygen-derived free radicals that induce DNA-damage and apoptosis in both rodent and human β-cells [20–25]. In both type 1 and type 1, as well as, type 2 diabetes, the role of free radicals in diabetic complications is well studied. The most prominent feature of diabetes, hyperglycemia, is believed to augment free radical production [26], probably due to the increased mitochondrial oxidative metabolism that is secondary to a high intracellular glucose concentration. Glucose also leads to advanced glycation end products, which initiate free radical cascades and are toxic to cells, including β-cells [27, 28].
Free radicals cause damage to cells by various mechanisms, resulting in damage to proteins, lipids, and nucleic acids, i.e., virtually all cellular structures. In particular, free radicals may lead to nuclear and mitochondrial DNA damage and mutations, causing diminished proliferative capacity, premature cellular senescence, and impaired mitochondrial function [29, 30]. For the β-cell, one of the most metabolically active cells in the body, mitochondrial function is essential, and diabetes is a prominent feature of many primary disorders of mitochondrial function [30].
While free radicals play a central role in the pathogenesis of many aspects of diabetes and it is known that free radicals can cause DNA damage, direct evidence is sparse for DNA damage in the pathogenesis of β-cell failure in type 2 diabetes. The exceptions are a study in which it was reported that the oxygen radical derived DNA adduct 7,8-dihydro-8-oxoguanosine (8-OH-dG) is present in the islets of diabetic Goto-Kakizaki rats, a model of type 2 diabetes [31]. Also, after submission of the present study, it was reported that an increased number of 8-OH-dG positive islet cells is observed in pancreata from human type 2 diabetic subjects. In that study, an increased number of cells with DNA damage correlated with a decreased β-cell mass [32].
Hypothesis
We hypothesized that oxidative DNA damage plays a role in the β-cell dysfunction and loss that occurs in human type 2 diabetes. To test this hypothesis, we screened the gene expression patterns of islets from a normal control and a type 2 diabetic subject with Affymetrix gene chip arrays, with special reference to genes involved in DNA repair (Tyrberg & Levine, unpublished data). One gene that was over-expressed in islets from the type 2 diabetic subject, was the DNA glycosylase 8-OxoG DNA glycosylase (Ogg1). This enzyme is the major repair enzyme involved in the defense against accumulation of the 8-OH-dG adducts discussed above. In light of the previous publication on the role of 8-OH-dG adducts in a rat model of type 2 diabetes [31], and the finding that the Ogg1 gene was over-expressed in human type 2 diabetes, we evaluated the expression of Ogg1 protein in pancreas specimens from type 2 diabetic and healthy subjects, as a marker for β-cell oxidative DNA damage in type 2 diabetes.
Methods
Tissue collection
Specimens from human pancreata were collected in La Jolla, CA; Sofia, Bulgaria; Seoul, South Korea and São Paolo, Brazil, post mortem or post surgery. Normal control subjects were never diagnosed with any form of diabetes while patients with type 2 diabetes had been diagnosed 2, 7, 15, 20 or 23 years before the specimens were collected. Diagnoses were based on hospital records. The patient with a 23 year history of diabetes also had a history of alcoholism. None of the subjects had a history of receiving cancer therapy, a possible confounding factor in the analysis of DNA damage. More detailed patient records are found in Table 1.
Immunofluorescent staining and fluorescence microscopy
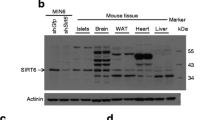
Sections from human pancreata were double stained for Ogg1 and somatostatin, as a marker for the islets, with rabbit anti-human Ogg1 (Novus Biologicals, Littleton, CO) and goat anti-human somatostatin antibodies (Santa Cruz Biotechnology, Santa Cruz, CA), after antigen retrieval by boiling for 10 min in acidic antigen retrieval solution (Biogenex, San Ramon, CA). Antibody binding was detected with an Alexa488 donkey anti-rabbit antibody (Molecular Probes, Eugene, OR) and an Alexa590 donkey anti-goat antibody (Molecular Probes). All sections were finally counter-stained with nuclear DAPI staining (Molecular Probes), and mounted with anti-fading mounting media (DAKO fluorescent mounting media, DAKO, Glostrup, Denmark). To evaluate the specificity of the Ogg1 antibody, slides were stained with fluorescent secondary antibody alone, which resulted in no background staining (data not shown). Also, as a positive control, pancreas from a mouse injected with the oxidative radical inducing agent alloxan [33], were stained one day after the injection, with a marked increase of Ogg1 nuclear and cytoplasmic staining as a result (data not shown).
Tissue sections were examined in a fluorescent microscope with 200–400× magnification. The pancreatic islets were evaluated blindly with semi-quantitative morphological scoring of fluorescent intensity: 0, no or very weak Ogg1 staining; 1, moderate Ogg1 staining; and 2, strong Ogg1 staining. They were also scored for Ogg1 positive islet area as follows: 0; no or very small area of the islet stained for Ogg1; 25, approximately 25% of the islet area was Ogg1 positive; 50, approximately 50%; 75, approximately 75%; and 100, approximately 100%. The total number of islets evaluated in the five pancreata from type 2 diabetic patients were 232 (46.4± 8.5 per pancreas) and in the seven pancreata from normal controls: 306 (43.7 ± 8.6 per pancreas). Sections were evaluated live in the fluorescence microscope with a combined filter for green and red fluorescence, which means that camera exposure time and other camera settings, did not influence the intensity of the Ogg1 staining. Also, the Alexa dyes are very stable fluorophores, even under UV light exposure, so that fading is unlikely to be a significant issue in influencing the results [34].
Ethics
Human tissue collection were approved by the respective local human IRBs (UCSD, La Jolla, CA; Veterans Hospital, La Jolla, CA; Military Medical Academy, Sofia, Bulgaria; University Hospital of São Paolo, São Paolo, Brazil; The Catholic University of Korea, Seoul, South Korea). No information that would identify the subjects was provided.
Statistical analysis
Data are presented as means ± SEM. The average semi-quantitative unparametric morphological scores for each individual was compared with Mann-Whitney's unparametric test.
Results
Pancreatic paraffin sections from five type 2 diabetic subjects and seven healthy controls were compared by immunohistochemistry for Ogg1. Co-staining for somatostatin as a marker of islets of Langerhans was performed (Fig. 1). Somatostatin rather than insulin was chosen as an islet marker because insulin expression can be significantly decreased in islets from patients with longstanding type 2 diabetes.
Ogg1 immunofluorescent staining in human pancreata. Ogg1 staining (green) and somatostatin (red), as a marker for islets of Langerhans, in normal human pancreata (A, C, E); and pancreata from type 2 diabetic subjects (B, D, F). Micrograph A is representative of an islet with no or very little Ogg1 staining; B of an islet with moderate staining intensity of 25% of the area; C, strong staining of 50% of the area; D, strong staining of 100% of the area; E, strong staining of 75% of the area; and F, strong staining of 100% of the area. Notably, the surrounding exocrine tissue is positive for Ogg1 at varying degrees (B and D vs. the rest). The micrographs were captured with identical camera settings. Original optical magnification 400×.
Two parameters were chosen to measure islet Ogg1 expression. The percentage of the islet that stained positively for Ogg1 was used as a measure of the number of Ogg1-expressing cells. The intensity of the Ogg1 staining was used as a measure of the level of Ogg1 expression in positive cells. By semi-quantitative scoring, both the intensity and the area of Ogg1 staining were significantly increased (P < 0.05 and P < 0.02, respectively) in islets from the type 2 diabetic subjects compared to the healthy controls (Fig. 2,3,4,5). Interestingly, the Ogg1 fluorescent staining intensity, but not the percent positive islet area, increases with increasing duration of diabetes (Fig. 6). Pancreatic exocrine tissue expressed Ogg1 at various degrees (Fig. 1), but no correlation was found with type 2 diabetes (data not shown).
Islet area stained for Ogg1. Islets were semi-quantitatively scored according to Methods into five different groups depending on the percentage of the area stained positive for Ogg1. Islets from type 2 diabetic subjects (2, 7, 15, 20, 23 years of diabetes duration, red) have significantly larger areas stained for Ogg1 (P < 0.05) than islets from healthy controls (a-g, green).
Islet area stained for Ogg1. Islets were semi-quantitatively scored according to Methods into five different groups depending on the percentage of the area stained positive for Ogg1. The frequency distribution of the scoring in normal and diabetic subjects shows that it is shifted to the left in islets from type 2 diabetic subjects.
Ogg1 fluorescent staining intensity. Islets were semi-quantitatively scored according to Methods into three different groups depending on the islet Ogg1 fluorescent intensity. Islets from type 2 diabetic subjects (2, 7, 15, 20, 23 years of diabetes duration, red) have significantly higher islet Ogg1 fluorescent intensity (P < 0.02) than islets from healthy controls (a-g, green).
Ogg1 fluorescent staining intensity. Islets were semi-quantitatively scored according to Materials and Methods into three different groups depending on the islet Ogg1 fluorescent intensity. The frequency distribution of the scoring in normal and diabetic subjects shows that it is shifted to the left in islets from type 2 diabetic subjects. Fluorescent intensity is expressed as arbitrary units.
Discussion
This study demonstrates that the enzyme Ogg1, which is involved in the repair of oxidative DNA damage, is up-regulated in the islets of patients with type 2 diabetes. This is consistent with the hypothesis that oxidative DNA damage is an important factor in the β-cell failure that plays a role in the pathogenesis of human type 2 diabetes.
We interpret the upregulation of Ogg1 as a response to an increased level of 8-OH-dG DNA, the lesion that it repairs. Increases in Ogg1 activity and expression have been found by a number of investigators [35–37]. Although antibodies to 8-OH-dG exist [38], Ogg1 was used as a surrogate for the amount of oxidative DNA damage. The reason for this is that we found high levels of background staining with the anti-8-OH-dG antibodies, which is not unusual when using streptavidin/biotin detection systems in immunohistochemistry [39]. Unfortunately, secondary antibodies directly linked to a fluorophore or a detection enzyme were not sensitive enough to detect the 8-OH-dG adduct in our hands.
The mechanism by which Ogg1 protein is increased in type 2 diabetic islets is unknown. The promoter of the Ogg1 gene does not have a TATA box [40], but Ogg1 is differentially expressed in the rat CNS, and its expression is increased after mouse forebrain ischemia-reperfusion [35, 36], suggesting that regulation occurs, either at the transcriptional or post-transcriptional level. Unfortunately, there have been no studies of the effects of long-term chronic increases in oxidative DNA damage on Ogg1 expression. The association between the duration of diabetes and Ogg1 levels (Fig. 6) suggests that such long-term exposure may be important for Ogg1 up-regulation.
Most of the staining observed was detected in the cytoplasm of the islet cells. As Ogg1 either is sublocalized into the nucleus or the mitochondria, this indicates that βOgg1, the mitochondrial form of Ogg1, accounts for the observed increase. βOgg1 is an alternatively spliced form of Ogg1 that contains a mitochondrial targeting signal in the C-terminal portion of the protein [41]. Specific upregulation of mitochondrial but not nuclear Ogg1 occurs during aging in rodents [42]. A specific increase of Ogg1 in islet cell mitochondria is consistent with the idea that increased β-cell mitochondrial oxidative metabolism due to hyperglycemia is a major factor behind the DNA damage. In a study published after this report was submitted, an increased number of 8-OH-dG positive islet cells in human type 2 diabetic subjects was observed [32]. The staining was found to be mainly nuclear in contrast to the cytoplasmic Ogg1 staining found in the present report. Unfortunately, we were unable to obtain specific staining with antibodies to 8-OH-dG. However, the nuclear localization of 8-OH-dG [32] and the increased Ogg1 reported here are consistent with a model in which mitochondrial Ogg1 is up-regulated but nuclear Ogg1 is not, leading to an increase in nuclear but not mitochondrial 8-OH-dG adducts [32]. Further studies will be required to resolve this issue, but β-cells in type 2 diabetes may well suffer from both nuclear and mitochondrial DNA damage, leading to decreased β-cell function and eventual loss of β-cell mass.
In this study, both the area and the intensity of Ogg1 staining were assessed. Since it was not practical to collect specimens in a controlled manner, it could be argued that differences in fixation technique could affect the fluorescence intensity of the immunostaining. However, as we also detected a significant increase in the islet area stained for Ogg1, we are confident that islet cell Ogg1 is actually upregulated in type 2 diabetes. The direct correlation between the fluorescence intensity and the duration of diabetes that held true for samples collected from disparate locations also argues in favor of the hypothesis. It is interesting that the Ogg1 positive area did not show the same increase with increasing duration of diabetes as the Ogg1 staining intensity. We have observed that the number of β-cells varies considerably in the islets from type 2 diabetic subjects and that large areas of the islets are sometimes replaced by amorphous material (data not shown), probably reflecting fibrosis or amyloidosis. Such a variation in cell number per islet would bias a correlation of Ogg1 positive cells with duration of diabetes. Moreover, it is possible that β-cells from patients with longstanding diabetes have a higher threshold for an apoptotic response to DNA-damage than β-cells in normal subjects, as it has been shown that this threshold increases with age [43]. Consequently, β-cells with high levels of DNA damage from younger individuals with a shorter duration of diabetes might be eliminated by apoptosis, while similarly damaged β-cells from older individuals, who are likely to have had diabetes for a longer time may be resistant to apoptosis and so remain. Such an apoptotic defect could account for the increasing intensity of Ogg1 staining, following accumulated levels of 8-OH-dG adducts with longer duration of diabetes. Further epidemiological studies in which age was specifically studied would be required to address this issue more definitively.
We noted that the variability in the amount of Ogg1 staining is higher in the control group than in the samples from the diabetic patients. It is well known that there is a high incidence of undiagnosed diabetes in the general population. Since detailed patient records were not available, it is possible that undiagnosed diabetes in the control group could account for the increased variability.
Ogg1 knockout mice possess increased levels of 8-OH-dG in their genome, particularly in the mitochondrial genome, but do not seem to exhibit an increased frequency of malignancies [44–46]. It was postulated that the consequences of 8-OH-dG adducts and Ogg1 deficiency affects mainly cells with high oxygen metabolism and slow proliferation, such as liver cells [45]. While β-cells were not examined in that study, they certainly exhibit both high oxidative metabolism and a low rate of proliferation, consistent with them being a target for the effects of 8-OH-dG adducts. It would be of great interest to study the Ogg1 mutant mice to determine whether an increase level of 8-OH-dG adducts predisposes to diabetes. This would be important in establishing oxidative DNA damage as a causal mechanism in diabetes as opposed to merely being an epiphenomenon in which the important targets for diabetes pathogenesis lie elsewhere in the β-cell. Further epidemiological studies of Ogg1 expression as well as studies of the expression of other genes and proteins that are involved in DNA damage responses should also be performed to further test the hypothesis that DNA damage is involved in the pathogenesis of type 2 diabetes.
Conclusions
We conclude that the expression of the DNA repair enzyme Ogg1 is up-regulated in islets from type 2 diabetic specimens. Moreover, Ogg1 expression intensity is directly correlated with the duration of diabetes. These finding are consistent with the hypothesis that oxidative DNA damage is playing a role in the pathogenesis of β-cell damage in type 2 diabetes.
References
Tyrberg B, Levine F: Current and future treatment strategies for type 2 diabetes: the β-cell as a therapeutic target. Curr Opin Investig Drugs. 2001, 2: 1568-1574.
Finegood DT, Scaglia L, Bonner-Weir S: Dynamics of beta-cell mass in the growing rat pancreas. Estimation with a simple mathematical model. Diabetes. 1995, 44: 249-256.
Sorenson RL, Brelje TC: Adaptation of islets of Langerhans to pregnancy: beta-cell growth, enhanced insulin secretion and the role of lactogenic hormones. Horm Metab Res. 1997, 29: 301-307.
Kahn BB: Type 2 diabetes: when insulin secretion fails to compensate for insulin resistance. Cell. 1998, 92: 593-6. 10.1016/S0092-8674(00)81125-3.
Farnier M, Picard S: Diabetes: Statins, Fibrates, or Both?. Curr Atheroscler Rep. 2001, 3: 19-28.
Eizirik DL, Korbutt GS, Hellerström C: Prolonged exposure of human pancreatic islets to high glucose concentrations in vitro impairs the β-cell function. J Clin Invest. 1992, 90: 1263-1268.
Maedler K, Spinas GA, Lehmann R, Sergeev P, Weber M, Fontana A, Kaiser N, Donath MY: Glucose induces beta-cell apoptosis via upregulation of the Fas receptor in human islets. Diabetes. 2001, 50: 1683-90.
Höppener JW, Ahrén B, Lips CJ: Islet amyloid and type 2 diabetes mellitus. N Engl J Med. 2000, 343: 411-9. 10.1056/NEJM200008103430607.
Janson J, Ashley RH, Harrison D, McIntyre S, Butler PC: The mechanism of islet amyloid polypeptide toxicity is membrane disruption by intermediate-sized toxic amyloid particles. Diabetes. 1999, 48: 491-8.
Zhou YP, Grill VE: Long-term exposure of rat pancreatic islets to fatty acids inhibits glucose-induced insulin secretion and biosynthesis through a glucose fatty acid cycle. J Clin Invest. 1994, 93: 870-6.
Cnop M, Hannaert JC, Hoorens A, Eizirik DL, Pipeleers DG: Inverse relationship between cytotoxicity of free fatty acids in pancreatic islet cells and cellular triglyceride accumulation. Diabetes. 2001, 50: 1771-7.
Donath MY, Gross DJ, Cerasi E, Kaiser N: Hyperglycemia-induced beta-cell apoptosis in pancreatic islets of Psammomys obesus during development of diabetes. Diabetes. 1999, 48: 738-44.
Tyrberg B, Eizirik DL, Hellerström C, Pipeleers DG, Andersson A: Human pancreatic β-cell DNA-synthesis in islet grafts decreases with increasing organ donor age but increases in response to glucose stimulation in vitro. Endocrinology. 1996, 137: 5694-5699. 10.1210/en.137.12.5694.
Ling Z, Pipeleers DG: Prolonged exposure of human beta cells to elevated glucose levels results in sustained cellular activation leading to a loss of glucose regulation. J Clin Invest. 1996, 98: 2805-2812.
Marshak S, Leibowitz G, Bertuzzi F, Socci C, Kaiser N, Gross DJ, Cerasi E, Melloul D: Impaired beta-cell functions induced by chronic exposure of cultured human pancreatic islets to high glucose. Diabetes. 1999, 48: 1230-1236.
Harmon JS, Gleason CE, Tanaka Y, Oseid EA, Hunter-Berger KK, Robertson RP: In vivo prevention of hyperglycemia also prevents glucotoxic effects on PDX-1 and insulin gene expression. Diabetes. 1999, 48: 1995-2000.
Mandrup-Poulsen T, Bendtzen K, Nielsen JH, Bendixen G, Nerup J: Cytokines cause functional and structural damage to isolated islets of Langerhans. Allergy. 1985, 40: 424-9.
Rabinovitch A, Sumoski W, Rajotte RV, Warnock GL: Cytotoxic effects of cytokines on human pancreatic islet cells in monolayer culture. J Clin Endocrinol Metab. 1990, 71: 152-6.
Arnush M, Heitmeier MR, Scarim AL, Marino MH, Manning PT, Corbett JA: IL-1 produced and released endogenously within human islets inhibits beta cell function. J Clin Invest. 1998, 102: 516-26.
Rabinovitch A, Suarez WL, Thomas PD, Strynadka K, Simpson I: Cytotoxic effects of cytokines on rat islets: evidence for involvement of free radicals and lipid peroxidation. Diabetologia. 1992, 35: 409-413.
Brenner HH, Burkart V, Rothe H, Kolb H: Oxygen radical production is increased in macrophages from diabetes prone BB rats. Autoimmunity. 1993, 15: 93-98.
Rabinovitch A, Suarez-Pinzon W, Strynadka K, Lakey J, Rajotte R: Human pancreatic islet β-cell destruction by cytokines involves oxygen free radicals and aldehyde production. J Clin Endocrinol Metab. 1996, 81: 3197-3202. 10.1210/jc.81.9.3197.
Delaney CA, Tyrberg B, Bouwens L, Vaghef H, Hellman B, Eizirik DL: Sensitivity of human pancreatic islets to peroxynitrite-induced cell dysfunction and death. FEBS Lett. 1996, 394: 300-306. 10.1016/0014-5793(96)00977-5.
Hadjivassiliou V, Green MH, James RF, Swift SM, Clayton HA, Green IC: Insulin secretion, DNA damage, and apoptosis in human and rat islets of Langerhans following exposure to nitric oxide, peroxynitrite, and cytokines. Nitric Oxide. 1998, 2: 429-41. 10.1006/niox.1998.0203.
Lakey JR, Suarez-Pinzon WL, Strynadka K, Korbutt GS, Rajotte RV, Mabley JG, Szabo C, Rabinovitch A: Peroxynitrite is a mediator of cytokine-induced destruction of human pancreatic islet beta cells. Lab Invest. 2001, 81: 1683-92.
Zou MH, Shi C, Cohen RA: High Glucose via Peroxynitrite Causes Tyrosine Nitration and Inactivation of Prostacyclin Synthase That Is Associated With Thromboxane/Prostaglandin H(2) Receptor-Mediated Apoptosis and Adhesion Molecule Expression in Cultured Human Aortic Endothelial Cells. Diabetes. 2002, 51: 198-203.
Singh R, Barden A, Mori T, Beilin L: Advanced glycation end-products: a review. Diabetologia. 2001, 44: 129-46. 10.1007/s001250051591.
Tajiri Y, Möller C, Grill V: Long-term effects of aminoguanidine on insulin release and biosynthesis: evidence that the formation of advanced glycosylation end products inhibits B cell function. Endocrinology. 1997, 138: 273-80. 10.1210/en.138.1.273.
Vijg J: Somatic mutations and aging: a re-evaluation. Mutat Res. 2000, 447: 117-35. 10.1016/S0027-5107(99)00202-X.
Kagawa Y, Cha SH, Hasegawa K, Hamamoto T, Endo H: Regulation of energy metabolism in human cells in aging and diabetes: FoF(1), mtDNA, UCP, and ROS. Biochem Biophys Res Commun. 1999, 266: 662-76. 10.1006/bbrc.1999.1884.
Koyama M, Wada R, Sakuraba H, Mizukami H, Yagihashi S: Accelerated loss of islet beta cells in sucrose-fed Goto-Kakizaki rats, a genetic model of non-insulin-dependent diabetes mellitus. Am J Pathol. 1998, 153: 537-45.
Sakuraba H, Mizukami H, Yagihashi N, Wada R, Hanyu C, Yagihashi S: Reduced beta-cell mass and expression of oxidative stress-related DNA damage in the islet of Japanese Type II diabetic patients. Diabetologia. 2002, 45: 85-96. 10.1007/s125-002-8248-z.
Tyrberg B, Andersson A, Borg LAH: Species differences in susceptibility of transplanted and cultured pancreatic islets to the β-cell toxin alloxan. Gen Comp Endocrinol. 2001, 122: 238-251. 10.1006/gcen.2001.7638.
Anonymous: Figure 1.35. Photobleaching profiles of cells stained with Alexa Fluor 488 or fluorescein conjugates. Access: January, 14, 2002. Molecular Probes, Inc. 2001, [http://www.probes.com/handbook/figures/0842.html]
Verjat T, Dhenaut A, Radicella JP, Araneda S: Detection of 8-oxoG DNA glycosylase activity and OGG1 transcripts in the rat CNS. Mutat Res. 2000, 460: 127-38. 10.1016/S0921-8777(00)00022-7.
Lin LH, Cao S, Yu L, Cui J, Hamilton WJ, Liu PK: Up-regulation of base excision repair activity for 8-hydroxy-2'-deoxyguanosine in the mouse brain after forebrain ischemia-reperfusion. J Neurochem. 2000, 74: 1098-105.
Saitoh T, Shinmura K, Yamaguchi S, Tani M, Seki S, Murakami H, Nojima Y, Yokota J: Enhancement of OGG1 protein AP lyase activity by increase of APEX protein. Mutat Res. 2001, 486: 31-40. 10.1016/S0921-8777(01)00078-7.
Takahashi S, Hirose M, Tamano S, Ozaki M, Orita S, Ito T, Takeuchi M, Ochi H, Fukada S, Kasai H, Shirai T: Immunohistochemical detection of 8-hydroxy-2'-deoxyguanosine in paraffin-embedded sections of rat liver after carbon tetrachloride treatment. Toxicol Pathol. 1998, 26: 247-52.
Agudelo S, Portus M: Leishmania antigen nonspecific binding to avidin in biotin-avidin immunoassays. Clin Diagn Lab Immunol. 2000, 7: 717-8. 10.1128/CDLI.7.4.717-718.2000.
Ishida T, Hippo Y, Nakahori Y, Matsushita I, Kodama T, Nishimura S, Aburatani H: Structure and chromosome location of human OGG1. Cytogenet Cell Genet. 1999, 85: 232-6. 10.1159/000015299.
Nishioka K, Ohtsubo T, Oda H, Fujiwara T, Kang D, Sugimachi K, Nakabeppu Y: Expression and differential intracellular localization of two major forms of human 8-oxoguanine DNA glycosylase encoded by alternatively spliced OGG1 mRNAs. Mol Biol Cell. 1999, 10: 1637-52.
de Souza-Pinto NC, Hogue BA, Bohr VA: DNA repair and aging in mouse liver: 8-oxodG glycosylase activity increase in mitochondrial but not in nuclear extracts. Free Radic Biol Med. 2001, 30: 916-23. 10.1016/S0891-5849(01)00483-X.
Suh Y, Lee KA, Kim WH, Han BG, Vijg J, Park SC: Aging alters the apoptotic response to genotoxic stress. Nat Med. 2002, 8: 3-4. 10.1038/nm0102-3.
Klungland A, Rosewell I, Hollenbach S, Larsen E, Daly G, Epe B, Seeberg E, Lindahl T, Barnes DE: Accumulation of premutagenic DNA lesions in mice defective in removal of oxidative base damage. Proc Natl Acad Sci U S A. 1999, 96: 13300-5. 10.1073/pnas.96.23.13300.
de Souza-Pinto NC, Eide L, Hogue BA, Thybo T, Stevnsner T, Seeberg E, Klungland A, Bohr VA: Repair of 8-oxodeoxyguanosine lesions in mitochondrial dna depends on the oxoguanine dna glycosylase (OGG1) gene and 8-oxoguanine accumulates in the mitochondrial dna of OGG1-defective mice. Cancer Res. 2001, 61: 5378-81.
Osterod M, Hollenbach S, Hengstler JG, Barnes DE, Lindahl T, Epe B: Age-related and tissue-specific accumulation of oxidative DNA base damage in 7,8-dihydro-8-oxoguanine-DNA glycosylase (Ogg1) deficient mice. Carcinogenesis. 2001, 22: 1459-63. 10.1093/carcin/22.9.1459.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1472-6823/2/2/prepub
Acknowledgements
We thank Dr. Linda Wasserman, UCSD Tissue Core Facility, for providing us with normal pancreatic tissue. This work was supported by grants from NIDDK to Fred Levine and by The Swedish Academy of Pharmaceutical Sciences and The Swedish Medical Society to Björn Tyrberg. Fred Levine is an Adjunct Professor at the Burnham Institute.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing Interests
None declared.
Authors' Contribution
B.T. participated in the design of the study, carried out the immunofluorescence stainings, interpreted the data and wrote the manuscript. K.A.A, S.A.D., J.W-R and K-H.Y. supplied the pancreatic specimens and took part in the editing of the manuscript. F.L. conceived of the study and participated in the interpretation of the data and the writing of the manuscript.
All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Tyrberg, B., Anachkov, K.A., Dib, S.A. et al. Islet expression of the DNA repair enzyme 8-oxoguanosine DNA glycosylase (Ogg1) in human type 2 diabetes. BMC Endocr Disord 2, 2 (2002). https://doi.org/10.1186/1472-6823-2-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1472-6823-2-2