Abstract
Background
Hemolytic Uremic Syndrome (HUS) may follow infection with Shiga-toxin-producing organisms, principally E. coli O157: H7 (STEC), causing high morbidity and mortality. Our aim was to identify interventions to prevent diarrhea-associated HUS.
Methods
Systematic search of the literature for relevant systematic reviews (SRs), randomised controlled trials (RCTs) and public health guidelines.
Results
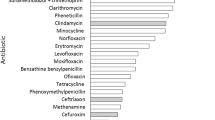
Of 1097 animal and 762 human studies, 18 animal studies (2 SRs, 2 reviews, plus 14 RCTs) and 6 human studies (3 SRs, plus 3 RCTs) met inclusion criteria. E. coli O157: H7 Type III secreted protein vaccination decreased fecal E. coli O157 shedding in cattle (P = 0.002). E. coli O157: H7 siderophore receptor and porin proteins (SRP) vaccines reduced fecal shedding in cows (OR 0.42 (95% CI 0.25 to 0.73) and increased anti-E. coli 0157: H7 SRP antibodies in their calves (P < 0.001). Bacterin vaccines had no effect. Probiotic or sodium chlorate additives in feeds reduced fecal E. coli O157 load as did improved farm hygiene (P < 0.05). Solarization of soil reduced E. coli O157: H7 contamination in the soil (P < 0.05). In an RCT examining the role of antibiotic treatment of E. coli O157: H7 diarrhea, HUS rates were similar in children treated with Trimethoprim-sulfamethoxazole and controls (RR 0.57; 95% CI 0.11 to 2.81). In another RCT, HUS rates were similar in children receiving Synsorb-Pk and placebo (RR 0.93; 95% CI 0.39 to 2.22). In one SR, hand washing reduced diarrhea by 39% in institutions (IRR 0.61; 95% CI 0.40 to 0.92) and 32% in community settings (IRR 0.68; 95% CI 0.52 to 0.90) compared to controls. Guidelines contained recommendations to prevent STEC transmission from animals and environments to humans, including appropriate food preparation, personal hygiene, community education, and control of environmental contamination, food and water quality.
Conclusions
Animal carriage of STEC is decreased by vaccination and improved farm practices. Treatment of STEC diarrhea with antibiotics and toxin-binders did not prevent HUS. Public health interventions are the key to preventing STEC-associated diarrhea and HUS.
Similar content being viewed by others
Background
Diarrhea-associated Hemolytic Uremic Syndrome (HUS) usually affects young children and occurs sporadically or in outbreaks, as in Germany in 2011 [1]. HUS may complicate diarrhea due to Shiga-toxin-producing organisms including Shigella dysenteriae and Shiga-toxin-producing E. coli (STEC). Worldwide, STEC O157: H7 is the most common cause of HUS [1], although many serotypes have been implicated. In adults, STEC infections occasionally cause HUS, but more commonly cause thrombotic thrombocytopenic purpura (TTP) [2]. In HUS, renal thrombotic microangiopathy results in clinical presentation with acute renal impairment, thrombocytopenia and microangiopathic hemolytic anemia.
Although most patients with diarrhea-associated HUS recover from the acute episode, there is potential for long-term renal impairment and extra-renal complications including seizures, diabetes, severe colitis and hypertension, are common. In one study, 39% of participants with HUS had one or more abnormality at 10-year follow-up, including proteinuria, low creatinine clearance or hypertension [3]. In another study, 63% of children recovered fully while others had proteinuria, reduced creatinine clearance and/or hypertension and 3.4% developed end-stage renal failure. [4].
Outbreaks of STEC diarrhea are often traced to animals, particularly cattle. Approximately 30% of feedlot cattle shed E. coli O157: H7 [5]. Other animals [6, 7]; contaminated water, both for drinking [8] and in swimming pools [9] and lakes [10]; food such as meats [11], mettwurst [12], salad sprouts [13] and lettuce [14]; drinks including unpasteurized apple juice [15] and milk; and direct contact with animals in petting farms [16] may also be sources of STEC.
In Australia and the USA the annual incidence of diarrhea-associated HUS in children under 5 years is ~1 per 100 000, with 3%-6% mortality [17, 18]. HUS in the elderly causes death in up to 90% [19, 20]. STEC 0157 infections cost the USA over U$400 million annually [21]. Approximately 8% of STEC infections progress to HUS [18]. Hence, prevention of HUS would significantly impact health outcomes and health expenditure.
Our aim was to systematically search and review the literature for SRs and RCTs of interventions to prevent diarrhea-associated HUS and to identify relevant evidence-based guidelines and public health policies.
Methods
We performed electronic searches of CENTRAL (Issue 3, March 2012), Medline (1946 to March week 1, 2012) and EMBASE (1988 to 2012, week 11). For animal studies we searched Medline (1990-week 3, 2012). We used a search strategy, with no restriction on language, to identify relevant trials and systematic reviews (See Search Strategy, Additional file 1). We also reviewed reference lists of papers identified in the search. Electronic searches of the internet and medical literature were performed for evidence-based guidelines and public health policies addressing prevention or treatment of STEC infections to prevent HUS.
Eligible studies included RCTs for the prevention of STEC infections or diarrhea-associated HUS; SRs; evidence-based guidelines; and public health policies or recommendations on prevention of STEC infection and/or HUS. We included any intervention for preventing E. coli infection and/or HUS. Two reviewers independently reviewed abstracts obtained from the literature search to identify relevant publications (Figure 1) [22]. The quality of RCTs was assessed by two reviewers, based on specific criteria for minimizing bias, including sequence generation, allocation concealment, blinding, complete outcome data and selective outcome reporting [23, 24].
Results
We identified 1097 animal studies in the literature search, of which 18 (2 SRs [25, 26], two reviews [5, 27] and 14 additional RCTs [28–42]) met our inclusion criteria. One SR evaluated animal vaccination [30], another SR examined the effect of a wide range of farming practices on fecal E. coli O157 load [26] and two reviews evaluated dietary manipulation [5, 27]. Of 762 human studies, six (3 SRs [43–45] and 3 additional RCTs [46–48]) met inclusion criteria. One SR investigated hand washing [45] and two SRs investigated specific treatments (antibiotics for STEC infection [43, 44].
Prevention of animal carriage
Two SR [25, 26], 2 reviews [5, 27] and 14 additional RCT [28–42] on prevention of animal carriage of E. coli O157 infections were included in the review. Potential ways to minimize animal carriage of STEC included: animal vaccination, additives and manipulation of animal feeds, and farm practices (Table 1).
Vaccination of animals
Two SR [25, 26] and two additional relevant RCT [28, 29], not included in the SR, investigated animal vaccination. One RCT investigated E. coli O157 Type III secreted protein (TTSP) vaccines [28] and the second RCT investigated E. coli O157: H7 siderophore receptor and porin protein (SRP) vaccines [29]. A systematic review on the role of vaccines in reducing fecal shedding of E. coli O157 in weaned domestic ruminants was inconclusive. Two studies reported a significant reduction of E. coli O157 shedding after E. coli O157 TTSP vaccination (P < 0.05) [26] but study protocols were heterogeneous. In a more recent systematic review with meta-analysis, E. coli O157: H7 TTSP vaccines significantly reduced fecal load of E. coli O157 in cattle (OR 0.38 95% CI 0.29 to 0.51) [25]. E. coli O157: H7 SRP vaccines reduced fecal load (OR 0.42 (95% CI 0.20 to 0.61), but bacterin vaccines were ineffective [25]. Thus, RCTs in domestic ruminants (cattle and pigs) showed that some vaccines increase protective antibody levels and decrease colonization, carriage, duration of fecal shedding and transmission of STEC. In a recent RCT, calves vaccinated with an E. coli O157 TTSP vaccine shed significantly less E. coli O157 than the control group on days 3–10 after vaccination (P = 0.002). Also, the number of calves shedding E. coli O157 during days 3–6 was significantly lower among the vaccinated, compared to control group (P ≤ 0.05) [28]. There was a low risk of bias in this study: interventions were randomly assigned and there was allocation concealment and blinding of staff to treatment. Another study reported that calves born to cows vaccinated with E. coli O157: H7 SRP vaccine had higher titers of anti- E. coli O157: H7 SRP antibodies at branding time (P < 0.001) [29]. However E. coli O157: H7 SRP vaccination had effect on fecal E. coli O157 shedding (P > 0.05), indicating that timing of vaccination may be relevant [29]. Treatments were randomly assigned, there was allocation concealment, and both study and laboratory personnel were blinded, indicating low risk of bias in this study.
Animal feeds and supplements
We identified one SR [26], two reviews [5, 49] and nine RCT [30–32, 35–37, 40, 50, 51] not included in the reviews evaluating manipulation of animal diets. Interventions included addition of probiotics (SR [26], plus 3 additional RCT [35, 37, 50]), grain versus forage feeds (2 reviews [5, 26], plus 4 RCT [30–32, 51]), and feed supplementation with vitamin D (1 RCT [36]), chlorate (SR) [27] and other additives (1 RCT [40]). The SR examined the effect of a wide range of farming practices on fecal E. coli O157 load [26]. Addition of probiotics and sodium chlorate to feed or water was effective in reducing fecal E. coli O157 load, but antimicrobials neither decreased nor increased the load [26]. There was insufficient evidence on the effectiveness of bacteriophages and other feed additives such as oral polyclonal anti-E. coli O157: H7 antibodies to support their use. The review was limited by lack of high quality studies, inconsistent results, and conduct of studies in an artificial environment. One RCT not included in the SR showed improved hygiene (dry bedding and cohorting of animals by herd) decreased fecal shedding of E. coli O157 (P < 0.05) [41]. A recent RCT concluded that soil solarization in feeding pens significantly decreased E. coli O157: H7 contamination of soil (P < 0.05) [42].
Probiotics
One SR of preharvest strategies [26], and 3 additional RCTs [35–37] reported on probiotics. The SR included 6 RCTs, in which controls received no treatment or placebo [26] and concluded that there was evidence of efficacy for the probiotic combination L. acidophilus NP51 (NPC 747) and P. freudenreichii[26] in reducing fecal STEC. A 10-year review reported that STEC could be significantly reduced by probiotics [5].
After microbial feeds, E. coli O157 was 74% less likely to be isolated from hides of cattle (P < 0.05) and 69% less likely to be found in faeces (P < 0.01) [35]. Steers fed L. acidophilus NP51 were 35% less likely to shed E. coli 0157: H7 than controls (OR 0.58, P = 0.008), confirming results from earlier trials [36]. Another RCT showed that cattle given L. acidophilus NP51 shed fewer E. coli 0157 in the feeding period compared with controls (P < 0.01), there being a dose response with a linear decrease in E. coli O157 shedding with increasing probiotic dose (P < 0.01) [37]. One SR (with 1 RCT and 3 challenge trials) concluded that addition of sodium chlorate to feed significantly decreased fecal shedding of E. coli O157: H7 [26].
Distillers’ grains
Two reviews [5, 49] and four additional RCTs [30–32, 34] reported on the effect of dietary distillers’ grains (DG) on fecal shedding. Up to 30% of cattle, particularly feedlot cattle, shed E. coli O157: H7 [5]. To increase feed efficiency, cattle are fed high grain rations [49], such as distillers’ grains (DG), which consist mainly of bran, protein and germ [52]. Grain-fed cattle have increased fecal shedding of E. coli O157: H7 because of alterations in gut fermentation, suggesting that dietary manipulations and feed supplements may affect ruminal or hindgut fermentation of DG and alter fecal shedding of E. coli O157: H7 [5, 33, 40]. An abrupt change in diet from grain (corn) to (forage) hay decreased fecal E. coli O157: H7 load in cattle by up to 1000-fold within 5 days, suggesting this intervention could be used pre-slaughter to reduce E. coli contamination [49]. In a large scale RCT however, no association was found between E. coli 0157: H7 load and feeding dried distiller’s grains, in contrast to previous trials [30]. A RCT in feedlot cattle confirmed that feeding wet DG had no effect on fecal E. coli O157: H7 load [32]. In another RCT wet DG with solubles (WDGS) increased fecal E. coli O157: H7 shedding in cattle (P < 0.001) [31] and lowering the dietary WDGS concentration for 56 days prior to slaughter reduced shedding (P < 0.05) [34].
Vitamin D
Vitamin D supplementation in cattle naturally infected with E. coli 0157: H7 does not affect shedding of E. coli 0157: H7 [39].
Bacteriophages
A SR concluded there was insufficient evidence of effectiveness of bacteriophages on fecal shedding [26]. A recent RCT investigated bacteriophages adapted to E. coli O157: H7 and encapsulated to prevent inactivation by gastric acid. These bacteriophages did not reduce shedding of E. coli O157: H7 in feedlot cattle [38], although they reduced duration of shedding by 14 days compared to controls (P < 0.1) [38].
Antibiotics, antimicrobials and growth promoters
One SR [26] and 2 RCTs [40, 53] investigated these food additives. No study included in the SR found a significant association between ionophore use and fecal shedding of E. coli O157 [26]. One RCT investigated the effect of two commercial feed additives, monensin (an ionophore against gram-positive bacteria) and ractopamine (a growth promoter) on fecal E. coli O157: H7 [40]. Cattle fed monensin at 44 mg/kg of feed had less fecal E. coli O157: H7 than cattle fed 33 mg/kg (4.3 vs. 6.8%, P = 0.05) [40]. Ractopamine had no effect on fecal shedding of E. coli O157: H7 (4.4 vs. 4.0%, P = 0.89) [40]. In one RCT B. subtilis was ineffective in reducing E. coli O157: H7 in feed lot cattle [53].
Farm practices
Two relevant RCTs evaluating farm practices were identified [41, 42]. One investigated whether improved hygiene and farm practices prevented carriage of E. coli O157: H7 [41]. Thirty farms (all having young cattle), were divided into four groups. Interventions were introduced to change farm practices in three groups of farms, which were compared with the fourth (control) group. Interventions included providing a clean environment and/or closed groups of young stock, improving water and feed hygiene, or no change in practice (controls). Providing dry bedding and keeping animals in the same herd groupings significantly decreased E. coli O157: H7 levels during the 4.5 month trial (P < 0.05) [41]. Treatments were randomly assigned with the allocation concealed; however blinding was not possible due to the differences in the treatments, so risk of bias is unclear. In a recent RCT, solarization of soil in feedlot pens was investigated, because soil is a potential point at which to reduce E. coli O157: H7 contamination [42]. After 1 week of solarization, there was a 2.0-log decrease in E. coli in soil and by week 6 of solarization, there was a >3.0-log reduction (P = 0.05) compared to controls [42].
Treatment of human STEC infections
Minimization of person to person contact and isolation of infected persons
During STEC outbreaks in the community or hospitals, people infected should be isolated to contain the outbreak [54]. Infections that may be complicated by HUS may be spread through person-to-person contact [55] in institutions (including psychiatric hospitals [56], nurseries [57], and child care centers [58]) and from mother to baby [59]. Guidelines to minimize person-to-person transmission have been issued by the Health Protection Agency (HPA) in the UK for public health physicians and environmental health officers. They recommend microbiological screening of close contacts of infected persons, provision of adequate hygiene and toilet facilities and supervised hand washing, particularly with children [60, 61]. UK guidelines advise that the best way for patients or their carers to avoid STEC infection is to adhere to essential hygiene, including frequent hand washing with soap and water, touching the face only with clean hands and keeping hard surfaces clean and disinfected [62].
An appropriate public health response to the management of acute bloody diarrhea in children is an important first step in preventing HUS. Children with proven STEC infection should not return to school, nursery or childcare until 48 hr after diarrhea ceases. Longer exclusion periods may be necessary for children aged less than five or with difficulty following hygienic practices.
During an outbreak of STEC diarrhea, UK guidelines recommend [63]:
-
Immediate risk assessment of the school’s eating/food preparation areas and toilets
-
Exclusion of high risk children until microbiological clearance
-
Exclusion of symptomatic children and staff until microbiological clearance
-
Consideration of microbiological screening and exclusion of asymptomatic contacts when there is a risk of ongoing environmental or person-to-person transmission
-
Improvement in hand hygiene within the institution e.g. increasing supervision of hand washing by children, particularly those under 5 years
-
Provision of information to parents on measures to control spread, including improved hygiene at home
-
Implementing environmental controls such as increased cleaning and decontamination of high risk surfaces, toys, toilets and eating facilities
-
Improving food preparation procedures where necessary
-
Consideration of temporary school closure if there is a risk of ongoing transmission from the environmental or person-to-person
-
Searching for additional cases in the community and consider collecting and analyzing epidemiological data and/or environmental samples from the school
-
Ensuring appropriate levels of hygiene are maintained according to guidelines and that there are effective procedures to remedy non-compliance
-
Considering measures for long term infection control, such as altering the layout of wash basins and toilets, or providing more such facilities in prominent positions [63]
Inpatient management
Inpatients with STEC infections should be isolated to prevent spread of infection to other patients, staff and visitors. Fluids should be monitored and the patient observed for complications, including signs of HUS [1]. Anti-diarrheal and anti-motility agents should be avoided [1, 64]. STEC infection should be notified to the relevant public health authority and patient contacts assessed.
Antibiotics
The risk of developing HUS after antibiotic treatment for E. coli O157: H7 diarrhea in children was addressed in two SRs [43, 44]. Both were inconclusive: antibiotics neither prevented nor increased the risk of HUS. Panos reviewed 19 studies with no meta-analysis, concluding that more RCTs were required to determine the effect of antibiotics on the duration and severity of enteritis and the potential for developing HUS [44]. Safdar included nine heterogeneous studies (only one RCT) [43]. Six of these studies showed no increased risk of HUS associated with antibiotic use in STEC infection; one showed a protective effect and two showed an increased risk. However, meta-analysis showed neither protection nor increased risk of HUS with antibiotic use (pooled odds ratio 1.15 (95% CI 0.79-1.68). We identified two completed RCTs, which examine the role of specific treatments for STEC in preventing HUS [46, 47] (Table 2).
TM (trimethoprim-sulfamethoxazole, TMP-SMX) antibiotic
In the RCT [46] included in Safdar’s SR [43], TMP-SMX for 5 days was compared with no antibiotic in children with diarrhea in who tested positive for E. coli O157: H7 (N = 47). There is a potential risk of bias in this trial: although it was randomized using computer generation, allocation concealment was not specified, neither participants nor investigators were blinded and use of intention-to-treat analysis was not stated. There was 100% follow-up and no adverse effects were reported. The HUS rate in children treated with antibiotics did not differ statistically from controls (RR 0.57; 95% CI 0.09 to 3.46, P = 0.67). Treatment commenced only after E. coli O157: H7 was isolated from stools, so there was potentially a delay between diarrhea onset and antibiotic treatment. At randomization only 20% of participants were excreting E. coli O157: H7 in the stool, hence if the infection was already established, the pathogenic mechanisms leading to HUS may already have been triggered prior to antibiotic treatment.
Synsorb-Pk
In the second completed RCT, Synsorb-Pk (SP) treatment for 7 days was compared with corn meal (control) in children with E. coli O157: H7 infection, symptoms consistent with STEC infection, or a close contact with HUS or STEC infection [47]. Synsorb is an agent that binds to ST to prevent its absorption from the gut. There is a risk of bias in this RCT because the methods of randomization and allocation concealment were not specified and intention-to-treat analysis was not stated. Both participants and investigators were blinded. No adverse effects were reported. The risk of developing HUS in the SP and control groups was similar RR 0.93 (95% CI 0.39 to 2.22). Thus, there is no evidence that Synsorb-Pk is effective in preventing HUS secondary to STEC infection. In this trial only 20% of participants were enrolled within 4 days of onset of diarrhea. Thus, Shiga toxin may already have been absorbed from the gut in the majority, rendering ineffective a treatment designed to bind and prevents absorption of toxin.
Monoclonal antibodies
An RCT currently in progress is assessing the role of monoclonal antibodies against Shiga-toxins 1 and 2 in preventing HUS in children with STEC infection [48].
Environmental contamination
Open farms, petting zoos and farms
To minimize environmental contamination in wildlife open or pet farms, provision of adequate hand washing facilities and eating areas that are separate from the animals is essential [45, 63]. Following outbreaks of E. coli infection involving children who visited petting farms, the Centers for Disease Control (CDC) and Prevention in the USA published guidelines that included recommendations to prevent veterinarians, farm visitors, animal keepers and visitors from acquiring infection in petting zoos and other public farms [66]. The most effective intervention is hand washing [63, 66]. Animals should be kept healthy, visitors should be informed about measures to prevent catching diseases from animals, food should be prohibited in areas where animals are kept, and areas for food consumption should be separated from animals by a transition area [66]. The Health Protection Agency (HPA) UK specifically designed guidelines for the general public when visiting farms, following an outbreak of E. coli O157 infection [67]. They also advise that the risk of acquiring serious E. coli O157 infection from animals and their surroundings will be greatly reduced if people maintain basic hygiene and warn that pregnant women should be particularly careful. The main recommendations are that people should avoid touching their face or put fingers in mouths after patting animals or visiting farms. Children in particular should not put their faces close to, or kiss, animals. There should be no eating or drinking while walking round the farm or touching animals. No food that drops on the ground should be eaten. Soap and water should be used to clean hands because this is more effective at removing E. coli O157 in dirt than gels or wipes. Children should be well-supervised to ensure they wash their hands thoroughly. Hands should be washed after touching animals or surfaces such as fences and before eating or drinking. Eating should only occur in separately located, designated areas such as restaurants or picnic areas. After contact with animals, boots, shoes, clothes and prams should be carefully cleaned, with thorough hand washing to follow [67].
Illustrative case 1. Petting zoo
Outbreak: 159 cases of E. coli O157: H7 infection in children who attended a fair in Canada in 1999[68].
Detection: After interviewing people testing positive for E. coli 0157: H7 or with diarrhea, authorities identified animals from the travelling petting zoo as a potential source of infection, since goats and sheep from this zoo, but no local cows, tested positive for E. coli 0157: H7. The same rare phage type was identified by subtyping in both human and animal samples.
Public health response: Guidelines developed as a result of this outbreak recommended separation of animals and food outlets and better facilities for hand washing after contact with animals[63], consistent with other studies[45].
Swimming water
HUS has been linked to contamination of private [69] and public [70] paddling pools with E. coli O157 and may result from failure to drain pools after use or inadequate chlorination [70]. WHO guidelines for safe swimming pools and other recreational waters ‘Water sanitation and health’ provide recommendations to ensure water hygiene for public swimming pools and lakes, including monitoring and surveillance of water quality, cleanliness of the facility, and measures to reduce infection risk, including education, design and construction of facilities and high quality maintenance and operation [71]. The guidelines target national and local authorities, owners, operators and designers, public health professionals, researchers and the general public [71]. Other guidelines regarding water quality of pools and lakes include recommendations for disinfecting pools [72], managing health and safety [73] and operating facilities [74]. Wildlife such as ducks are a potential source of E. coli contamination in lakes [75]. Guidelines such as those from the National Health and Medical Research Council of Australian include procedures to help prevent contamination of swimming water [76]. Beach water and sand are potential sources of E. coli infection [77, 78]. Health risk from sand is due mainly to contaminated sand on the hands being transferred to the mouth, so thorough hand washing may prevent infection [45].
Drinking water
Globally, one of the most critical determinants of human health is drinking water quality [71]. Diarrhea is the most common waterborne disease and over 4 billion diarrhea cases and over 2 million deaths occur globally each year [71]. Water may be contaminated in catchment areas by human or animal feces or within the supply system through unsanitary equipment or bad hygiene. Contaminated well water has been implicated in outbreaks of E. coli O157: H7 infection. In 1999, nearly 1000 people were infected and at least two died after consuming water at a county fair in New York State. The ground water well at the fair had been contaminated by manure run-off from a cattle exhibit barn after a heavy rainfall and the unchlorinated water was used by vendors for drinks and ice [8].
Illustrative case 2. Contaminated drinking water
Outbreak: In 2000 in Walkerton Ontario, Canada, 2,300 people became infected with E. coli O157: H7 in contaminated drinking water, of whom 65 were hospitalized and seven died[79].
Detection: A judicial provincial government inquiry found numerous contributing failures, including assumptions that bore water was safe, insufficient surveillance of bore catchment areas, inadequate chlorination of water and inadequately trained operating staff in the treatment plant[79].
Public health response: Following the outbreak, new Drinking Water Regulations were introduced for providers, including stringent guidelines for testing for bacterial contamination[79]. Canadian guidelines now recommend regular testing of all drinking water systems for E. coli. The number, frequency, and location of samples depends on the type and size of the system and local authority requirements[80]. The maximum acceptable concentration of E. coli in public, semi-public, and private drinking water systems is set at non-detectable (0 mg/L)[80].
Guidelines for improving water quality were amongst the earliest produced by the World Health Organization (WHO) and are regularly revised [71]. Many countries including Australia produce their own guidelines for monitoring drinking water quality [81]. Many guidelines originated in response to outbreaks of E. coli infection.
Domestic food preparation: prevention of contamination
Public education regarding safe preparation of domestic food is important. The WHO produces guidelines on preparing food for the general public [65, 82].
The five keys to safer food are:
-
1.
Keep clean (hands, food preparation equipment and kitchen areas);
-
2.
Separate raw and cooked food (e.g. keep raw meat from salad foods; use separate equipment such as knives and chopping boards for raw food; store raw food in separate containers to avoid cross contamination);
-
3.
Cook and reheat food thoroughly, especially meat, poultry, eggs and seafood, to ensure food reaches boiling temperature ( ≥70°C) to kill E. coli.;
-
4.
Store food at safe temperatures (refrigerate promptly, don’t leave cooked food at room temperature for > 2 hours, don’t store food for too long, don’t thaw frozen food at room temperature, and keep cooked food hot at > 60°C) and;
-
5.
Use safe water and raw materials (fresh food, washed fruit and vegetables especially if eaten raw, in-date food, food processed for safety e.g. pasteurized milk [65].
Public health prevention measures
Over 700,000 guidelines were identified in the internet search using text words ‘guidelines’ , ‘E. coli O157′ and ‘prevention’. We selected representative, evidence-based guidelines, such as those from the Centers for Disease Control, USA which summarize strategies for preventing infection with E. coli O157: H7 and other STEC. Prevention measures include appropriate food preparation and storage, promotion of personal hygiene, public health education campaigns, legislation, programs to prevent environmental contamination by STEC, and testing food and water quality.
Hand washing
There is strong evidence that hand washing is effective in preventing diarrhea, hence indirectly reducing the risk of HUS infection. A Cochrane review included 14 RCTs [45]: eight institution-based trials in high income countries, five community-based trials in lower income countries, and one in high risk (AIDS) patients. Meta-analysis showed hand washing lowered diarrhea rates by approximately one third: in institutions (2 RCTS, 39% reduction, IRR 0.61 (95% CI 0.40 - 0.92); and in community settings (4 RCTS, 32% reduction, IRR 0.68 (95% CI 0.52 - 0.90) [45]. Hand washing guidelines are available from WHO [82] and elsewhere [83–85]. The WHO recommends frequent, thorough washing with soap and water, lathering for at least 20 seconds [82]. Hand sanitizers should be used where soap and water are unavailable [82]. The Mayo Clinic notes that antibacterial soap is no more effective for killing pathogens than ordinary soap and may lead to bacterial resistance [83]. Hands should be washed before preparing food, eating, attending to the sick or injured; and after preparing raw meat and poultry, using the toilet, changing babies, touching animals or their accoutrements, blowing noses, treating wounds or the sick, and handling contaminated waste [83–85]. Children should be supervised when hand washing [83].
Commercial food production: control to minimize E. colicontamination
The Food and Agricultural Organization (FAO) has produced guidelines to assist countries strengthen national systems to ensure food safety and quality [86]. These guidelines also ensure that exported/imported food comply with the international regulations relevant in a globalized food industry. As consumers take more interest in the provenance of their food, nations develop guidelines and regulations to minimize contamination during production. The FAO guidelines provide recommendations to protect public health and prevent food adulteration through improvement of food control systems, including legislation and infrastructure [86]. These can be adapted by individual countries to their own circumstances. The European Community (EC) established the European Food Safety Authority (ESFA) to protect food safety by providing general requirements for laws on food. Since food is freely transported within the EC, it was essential to ensure that legislation was consistent throughout the EC [87].
Potential contamination of food by STEC may occur at any stage in the production chain – including contamination of seeds (a particular problem with salad sprouts) or of foodstuffs during packing, transport and distribution [88]. Hence, microbiological testing of food for E. coli is recommended at all relevant stages of production. Because there have been more than ten serious outbreaks of food poisoning connected with salad sprouts in the USA, the US Food and Drug Administration classifies alfalfa sprouts as a high-risk food. The definitive way to remove EHEC during food production is by bactericidal treatment including cooking, pasteurization or irradiation [89] (Table 3).
Illustrative case 3. Contaminated Sprouts in Japan
Outbreak: A large outbreak of EHEC O157 gastroenteritis occurred in Japanese school children, in 1996[13]. Over 12,000 children became ill and 121 developed HUS of whom three died.
Detection: When epidemiological evidence implicated hydroponic radish sprouts in school lunches, laboratory analysis of sprout samples identified E. coli O157: H7 contamination[13]. Investigations could not confirm the source of contamination. After additional outbreaks in 1997 involving radish sprouts, it was found that the seeds were the source of contamination. On further investigation, sprouts grown from seeds or sprout roots experimentally contaminated with E. coli O157: H7, were found to be contaminated with E. coli O157: H7 both on outer surfaces and in inner tissues, due to rapid bacterial growth during germination.
Public health response: To prevent future outbreaks, the Japanese Government developed new guidelines and regulations on growing, processing and shipping of radish sprouts. Their focus was on sterilization of both the water supply and the seeds. They also developed protocols for maintaining hygienic facilities and equipment and for examining radish sprouts for EHEC[112]. Guideline additions tightened regulations on production of hydroponically grown lettuce[112].
Illustrative case 4. Contaminated Sprouts in Germany 2011
Outbreak: The 2011 outbreak in Germany of STEC infection resulted in over 4000 cases of severe gastroenteritis and over 850 cases of HUS, with 49 deaths.
Detection: After investigating cases, salad greens were identified as the potential source of infection, cucumbers from Spain having been incorrectly implicated initially. Epidemiological investigation implicated a 15000 kg shipment of fenugreek seeds, imported from Egypt in 2009 for growing sprouts, as the probable source of the outbreak which affected mainly adults,[97], even though the lethal STEC 0101:H4 involved was not detected on farms. The high proportion of cases progressing to HUS may reflect the STEC’s virulence characteristics[113].
Public Health response: The EC banned importation of fenugreek seeds from Egypt and the UKHPA updated guidelines on the management and treatment of acute bloody diarrhea in children, particularly in relation to STEC infection[114].
Meat and meat products
Many STEC outbreaks are related to meat products, particularly beef from feedlot cattle, so improving the safety of meat after slaughter by controlling E. coli O157: H7 contamination is an active areas of research [115].
Dry cured salami
Outbreaks of E. coli O157: H7 infection, occurring in Washington and California in1994, were traced back to commercially distributed dry cured salami. In response, the USA Centers for Disease Control and Prevention issued specific advice on preventing recurrence [116].
Illustrative case 5. Contaminated Mettwurst
Outbreak: In Australia in 1995, an outbreak of HUS caused by E. coli O111:H1 resulted in 21 HUS cases, with one death. Eighteen children required dialysis and complications included colonic necrosis, cerebral hemorrhage, convulsions and death. After one year, five children had renal function impairment[59].
Detection: Within two weeks the dietary habits of patients were investigated[117]. Patient samples and suspect foods were tested, using Shiga-like toxin gene assays. The infection source was rapidly identified as a locally produced dry-fermented sausage (mettwurst)[12]. Samples from 19 of the 21 HUS patients and 7 of 8 mettwurst samples collected from their homes tested positive for the organism.
Public health response : The Australia New Zealand Food Authority updated legislation on the production of fermented, uncooked comminuted meat products, requiring that the products be cooked at a core temperature of 65°C for 10 minutes during production, so as not to rely on consumers cooking the products at home[118].
Hamburgers
American guidelines give specific advice on preparation of hamburgers, aimed at decreasing outbreaks of E. coli O157 infection from ingestion of contaminated mincemeat [11, 91]. Mince or hamburgers should reach an internal temperature of 70°C to be safe to ingest, regardless of color. To ensure this temperature is reached, a food thermometer should be used, since color is not a sufficiently reliable indicator that harmful bacteria such E. coli O157: H7 have been killed. Eating undercooked hamburger mince poses a significant risk that can lead to serious illness or even death, particularly in the young, the aged, and people with immune deficiency. Under-cooked hamburgers should be sent back to the kitchen and served with a new bun on a clean plate. The 2007 CDC guidelines reinforce recommendation from the WHO and FAO.
Venison
Wildlife meat, such as deer, wild boar and hare, have been identified as a reservoir and potential source of pathogenic STEC infections [119]. Venison, which may be highly contaminated with fecal bacteria, is usually hung at ambient temperatures, allowing bacteria present to multiply [6]. In contrast, fresh beef is generally chilled rapidly. To protect public health, guidelines for handling game should similar to those for commercially slaughtered meat [120]. The US Department of Agriculture's Food Safety (USDA) and Inspection Service monitors commercial production of jerky, a dehydrated meat product [120]. US guidelines were also formulated for domestic production of jerky, following an outbreak of E. coli O157 infection in 11 people who ate homemade venison jerky [6]. The USDA recommends pre-cooking the meat to 70°C before dehydration to ensure decontamination.
Guidelines for the retail food industry
Despite guidelines, there continue to be outbreaks of STEC infection and HUT that can be traced back to contaminated food. Outbreaks sometimes result in development of new guidelines or revision of recommendations. Examples include revision of the food production code for mettwurst sausage following an HUS outbreak in Australia [12] and guidelines developed for businesses from Food Safety Australian [121] and others in the USA [122] and UK [123].
Illustrative case 6. Contaminated spinach in USA
Outbreak: In 2006, a large E. coli O157: H7 outbreak in the USA was associated with contaminated baby spinach. This caused 205 cases of diarrhea and three deaths: 51% of those infected were hospitalized and 16% developed HUS[50].
Detection: Government agencies determined bagged spinach to be the probable source of the outbreak. Contaminated spinach bags were collected from patients, and the packaging plant which processed the bags. Using bag product codes and DNA fingerprinting of bacteria from the bags, the outbreak strain was eventually matched to environmental E. coli O157: H7 samples from one agricultural field. Potential contamination sources of this field included wild pigs, irrigation wells and waterways exposed to cattle and wildlife feces. Due to the many potential sources of contamination, including animals, humans, and water, the way in which the E. coli O157: H7 contaminated the spinach was never elucidated.
Public health response: New guidelines were developed to minimize microbial contamination during processing of fresh-cut produce[124].
Guidelines on preventing and controlling E. coli O157 infections are updated as new scientific evidence emerges. Recommendations include ways to prevent acquisition and spread of infection, especially within institutions where cross infection is more likely to occur and for people at increased risk of acquiring and transmitting infection, including food handlers and the young, elderly and infirm [125]. Preventative measures also include public health and education campaigns about food preparation and storage, commercially and at home; legislation applicable to food production; prevention of environmental contamination; and programs for monitoring food and water quality, including swimming facilities. Revisions are often instigated after investigations of HUS outbreaks.
The CDC’s advice can be summarized in five points. Wash hands thoroughly after: the bathroom, changing babies, contact with animals and their environment; and before preparing or eating food. Cook meat thoroughly to a minimum internal temperature of 70°C. Avoid unpasteurized milk, dairy products and juices such as fresh apple cider. Avoid swallowing water from swimming pools, paddling pools, lakes or rivers. Wash hands, surfaces, boards and utensils after preparing raw meat to prevent cross contamination [126].
Discussion
Our aim was to review the medical literature and public health guidelines regarding prevention of diarrhea-associated HUS. We identified avenues for prevention of STEC infection and HUS, based on high quality evidence from SRs and RCTs. In animals, vaccination [28] and improved farming and feeding practices including dietary manipulation (e.g. probiotics and sodium chlorate feed additives [26]), cohorting of animals and dry bedding and soil solarization reduce STEC carriage and fecal shedding in animals, and hence the risk of STEC transmission to humans.
Appropriate treatment of STEC diarrhea in humans, including withdrawal from school and isolation within institutions will minimize spread of infections. There is strong evidence that personal hygiene, particularly hand washing, is crucial to prevent acquisition and spread of STEC infections in the community, hence decreasing the risk of HUS [45].
Public health guidelines and legislation to safeguard food and water against STEC contamination and ensure appropriate production, preparation and storage of food are also important, as is community education. Treatment of STEC diarrhea with antibiotics and Shiga-toxin binding agents does not influence risk of developing HUS, based on limited evidence from RCTs.
Despite evidence to support these prevention strategies and numerous evidence-based guidelines and policies, outbreaks of STEC diarrhea and HUS continue to occur. These are often traced to farms and particularly cattle, which are a major source of STEC infection, since ruminant animals act as a natural reservoir of E. coli 0157: H7 [27]. Thus strategies to reduce fecal E. coli O157: H7 shedding in cattle could reduce STEC infection in humans. E. coli 0157: H7 TTSP and SRP vaccines are effective in reducing fecal E. coli O157 shedding [28, 127]. However, cattle infected with E. coli O157 are not ill, hence subsidies for farmers may be required to promote vaccination as a public health measure to decrease the risk of animal to human transmission. Vaccinating the majority of cattle in a feedlot pen also provides herd immunity [128]. If E. coli O157: H7 carriage and shedding can be reduced in cattle, environmental contamination will also be reduced, as will contamination of meat during processing [129].
Changes in gut fermentation may also affect fecal E. coli O157 shedding, since E. coli O157 multiplies rapidly in the gut [130]. Hence, altering intestinal conditions with different feeds has been investigated as a means of reducing fecal E. coli 0157: H7 shedding [131]. Some studies show that reducing WDGS feeds 56 days prior to harvest significantly reduces fecal shedding of E. coli 0157: H7 [34] and there is evidence that cattle fed hay rather than grain for a brief period before slaughter have significantly reduced fecal shedding of pathogenic E. coli[132]. However, other researchers have found no relation between E. coli 0157: H7 shedding and feed type [30].
Some STEC strains from cattle have developed antibiotic resistance and in one study resistance was found in 34% fecal samples from animals and also in isolates from hamburger mince [133]. Research is required to address antibiotic resistance.
Education about the risk factors for STEC infection, methods for rapidly identifying the infection source to prevent further spread, and isolation of symptomatic children and adults with STEC infection may help contain outbreaks and limit potential cases of HUS. In one RCT, treatment with a Shiga toxin binding agent was delayed until STEC was isolated in the stool, often days after onset of symptoms. Rapid, reliable diagnostic tests for STEC would enable early initiation of treatment and supportive care.
Appropriate management of STEC infections, once acquired, may also decrease the risk of developing HUS, including monitoring of fluid balance, early use of parenteral volume expansion to minimize renal damage [90], monitoring for complications and avoiding anti-diarrheal and anti-motility agents [1, 64]. There is insufficient evidence to warrant use of antibiotics, dialysis or Shiga-toxin binders for early treatment of STEC infection, although these have been proposed as measures to prevent progression from STEC diarrhea to HUS. Indeed there is some concern about the potential harm associated with antibiotic treatment of STEC diarrhea. In a prospective cohort study, antibiotic treatment of STEC infections increased the risk of developing HUS and this has changed clinical practice for treatment of enteritis [134]. Participants in the study were children with confirmed stool E. coli O157: H7 and the RR for developing HUS in the antibiotic treated group compared to controls was 17.3 (95% CI 2.2-137, P = 0.007). In 1996 425 Japanese children hospitalized during a huge outbreak of STEC infection were treated with antibiotics. Although 12 children developed HUS, all recovered without significant complications [13]. Antibiotic treatment of E. coli infection [134] also introduces the potential for development of antibiotic resistance [133, 135].
This is the first systematic review on this topic include both the human and animal literature and public health guidelines. It provides useful information for clinicians and public health professionals on the prevention of STEC infection and HUS. High quality evidence from RCTs and SRs is available to inform guidelines and medical and veterinarian practice. This value of the review is limited by the low number of relevant RCTs and their small sample size, which restricts our ability to draw meaningful conclusions.
Because HUS is a rare event, large multi-centered trials are required to provide sufficient power address some controversial questions, including the role of antibiotics for the treatment of STEC in the prevention of HUS. Outcome measures should including the frequency and severity of HUS and adverse effects of treatment and study power must be sufficient power to detect real benefits or harms. We eagerly await an ongoing RCT evaluating the role of monoclonal antibodies in inactivating Shiga-toxins 1 and 2 in children with STEC diarrhea [48]. Studies are also required to investigate the role of new antibiotics, new vaccines and new therapies for binding Shiga-toxin. The development of a human vaccine to prevent STEC infection may eventually provide herd immunity and protect against HUS and would be particularly valuable in low-income settings where bacterial gastroenteritis is common.
Conclusions
Potential means of preventing HUS include minimizing fecal STEC shedding in animals and transmission of infection to humans. Public health measures to safeguard food and water from contamination are essential as is personal hygiene and care with food preparation and storage. This is the first comprehensive review of this topic and includes data from the medical and veterinarian literature and from public health guidelines. It provides useful information for clinicians and public health professionals on the prevention of HUS.
Authors’ information
DET: Scientific Director, Centre for Evidence-Based Paediatrics Gastroenterology and Nutrition, Paediatrics and Child Health, Sydney Medical School,
The University of Sydney; KRI, The Children's Hospital at Westmead
EJE: Professor, Pediatrics and Child Health, Sydney Medical School,
The University of Sydney; Consultant Pediatrician, The Children's Hospital at Westmead; Director, Centre for Evidence-Based Paediatrics Gastroenterology and Nutrition
Abbreviations
- EHEC:
-
Enterohemorrhagic E. coli
- HUS:
-
Hemolytic uremic syndrome
- STEC:
-
Shiga-toxigenic E. coli
- CCTR:
-
Cochrane Controlled Trials Register
- TM:
-
Trimethoprim-sulfamethoxazole
- OR:
-
Odds ratio
- NNT:
-
Number needed to treat
- CI:
-
Confidence intervals
- SRP:
-
Siderophore receptor and porin proteins
- TTSP:
-
Type III secreted protein
- VTEC:
-
Verotoxin-producing E. coli.
References
Tarr PI, Gordon CA, Chandler WL: Shiga-toxin-producing Escherichia coli and haemolytic uraemic syndrome. Lancet. 2005, 365 (9464): 1073-1086.
Verweyen HM, Karch H, Allerberger F, Zimmerhackl LB: Enterohemorrhagic Escherichia coli (EHEC) in pediatric hemolytic-uremic syndrome: a prospective study in Germany and Austria. Infect. 1999, 27 (6): 341-347. 10.1007/s150100050040.
Siegler RL, Milligan MK, Burningham TH, Christofferson RD, Chang SY, Jorde LB: Long-term outcome and prognostic indicators in the hemolytic-uremic syndrome. J Pediatr. 1991, 118 (2): 195-200. 10.1016/S0022-3476(05)80482-2.
Spizzirri FD, Rahman RC, Bibiloni N, Ruscasso JD, Amoreo OR: Childhood hemolytic uremic syndrome in Argentina: long-term follow-up and prognostic features. Pediatr Nephrol. 1997, 11 (2): 156-160. 10.1007/s004670050248.
Callaway TR, Carr MA, Edrington TS, Anderson RC, Nisbet DJ: Diet, Escherichia coli O157: H7, and cattle: a review after 10 years. Curr Issues Mol Biol. 2009, 11 (2): 67-79.
Keene WE, Sazie E, Kok J, Rice DH, Hancock DD, Balan VK, Zhao T, Doyle MP: An outbreak of Escherichia coli O157: H7 infections traced to jerky made from deer meat. JAMA. 1997, 277 (15): 1229-1231. 10.1001/jama.1997.03540390059036.
Chapman PA, Siddons CA, Gerdan Malo AT, Harkin MA: A 1-year study of Escherichia coli O157 in cattle, sheep, pigs and poultry. Epidemiol Infect. 1997, 119 (2): 245-250. 10.1017/S0950268897007826.
CDC: Outbreak of Escherichia coli O157: H7 and Campylobacter among attendees of the Washington County Fair-New York, 1999. MMWR Morb Mortal Wkly Rep. 1999, 48 (36): 803-805.
Keene WE, McAnulty JM, Hoesly FC, Williams LP, Hedberg K, Oxman GL, Barrett TJ, Pfaller MA, Fleming DW: A swimming-associated outbreak of hemorrhagic colitis caused by Escherichia coli O157: H7 and Shigella sonnei. N Engl J Med. 1994, 331 (9): 579-584. 10.1056/NEJM199409013310904.
McCarthy TA, Barrett NL, Hadler JL, Salsbury B, Howard RT, Dingman DW, Brinkman CD, Bibb WF, Cartter ML: Hemolytic-Uremic Syndrome and Escherichia coli O121 at a Lake in Connecticut, 1999. Pediatr. 2001, 108 (4): E59-10.1542/peds.108.4.e59.
Bell BP, Goldoft M, Griffin PM, Davis MA, Gordon DC, Tarr PI, Bartleson CA, Lewis JH, Barrett TJ, Wells JG, et al: A multistate outbreak of Escherichia coli O157: H7-associated bloody diarrhea and hemolytic uremic syndrome from hamburgers. The Washington experience. JAMA. 1994, 272 (17): 1349-1353. 10.1001/jama.1994.03520170059036.
Paton AW, Ratcliff RM, Doyle RM, Seymour-Murray J, Davos D, Lanser JA, Paton JC: Molecular microbiological investigation of an outbreak of hemolytic-uremic syndrome caused by dry fermented sausage contaminated with Shiga-like toxin-producing Escherichia coli. J Clin Microbiol. 1996, 34 (7): 1622-1627.
Fukushima H, Hashizume T, Morita Y, Tanaka J, Azuma K, Mizumoto Y, Kaneno M, Matsuura M, Konma K, Kitani T: Clinical experiences in Sakai City Hospital during the massive outbreak of enterohemorrhagic Escherichia coli O157 infections in Sakai City, 1996. Pediatr Int. 1999, 41 (2): 213-217. 10.1046/j.1442-200X.1999.4121041.x.
Ackers ML, Mahon BE, Leahy E, Goode B, Damrow T, Hayes PS, Bibb WF, Rice DH, Barrett TJ, Hutwagner L, et al: An outbreak of Escherichia coli O157: H7 infections associated with leaf lettuce consumption. J Infect Dis. 1998, 177 (6): 1588-1593. 10.1086/515323.
CDC: Outbreak of Escherichia coli O157: H7 infections associated with drinking unpasteurized commercial apple juice - British Columbia, California, Colorado, and Washington, October 1996. MMWR Morb Mortal Wkly Rep. 1996, 45 (44): 975-
Heuvelink AE, van Heerwaarden C, Zwartkruis-Nahuis JT, van Oosterom R, Edink K, van Duynhoven YT, de Boer E: Escherichia coli O157 infection associated with a petting zoo. Epidemiol Infect. 2002, 129 (2): 295-302.
Elliott EJ, Robins-Browne RM: Hemolytic uremic syndrome. Curr Probl Pediatr Adolesc Health Care. 2005, 35 (8): 310-330. 10.1016/j.cppeds.2005.06.002.
Epidemiologic Summary of Shiga toxin-producing Escherichia coli (STEC)-related infections and illnesses in California. 2001, http://www.cdph.ca.gov/data/statistics/Documents/stec-episummary.pdf, –2008,
O'Brien AD, Holmes RK: Shiga and Shiga-like toxins. Microbiol Rev. 1987, 51 (2): 206-220.
Carter AO, Borczyk AA, Carlson JA, Harvey B, Hockin JC, Karmali MA, Krishnan C, Korn DA, Lior H: A severe outbreak of Escherichia coli O157: H7–associated hemorrhagic colitis in a nursing home. N Engl J Med. 1987, 317 (24): 1496-1500. 10.1056/NEJM198712103172403.
Frenzen P, Drake A, Angulo F: Economic cost of illness due to Escherichia coli O157 infections in the United States. J Food Prot. 2005, 68 (12): 2623-2630.
Moher D, Cook DJ, Eastwood S, et al: Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta-analyses. Lancet. 1999, 354: 1896-1900. 10.1016/S0140-6736(99)04149-5.
Jadad AR, Moore RA, Carroll D, et al: Assessing the quality of reports of randomized clinical trials: is blinding necessary?. Controlled Clin Trials. 1996, 17: 1-12. 10.1016/0197-2456(95)00134-4.
Schulz KF, Chalmers I, Hayes RJ, et al: Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA. 1995, 273: 408-412. 10.1001/jama.1995.03520290060030.
Snedeker KG, Campbell M, Sargeant JM: A systematic review of vaccinations to reduce the shedding of Escherichia coli O157 in the faeces of domestic ruminants. Zoonoses Public Health. 2012, 59 (2): 126-138. 10.1111/j.1863-2378.2011.01426.x.
Sargeant JM, Amezcua MR, Rajic A, Waddell L: Pre-harvest interventions to reduce the shedding of E. coli O157 in the faeces of weaned domestic ruminants: a systematic review. Zoonoses Public Health. 2007, 54 (6–7): 260-277.
Callaway TR, Edrington TS, Anderson RC, Genovese KJ, Poole TL, Elder RO, Byrd JA, Bischoff KM, Nisbet DJ: Escherichia coli O157: H7 populations in sheep can be reduced by chlorate supplementation. J Food Prot. 2003, 66 (2): 194-199.
Allen K, Rogan D, Finlay B, Potter A, Asper D: Vaccination with type III secreted proteins leads to decreased shedding in calves after experimental infection with Escherichia coli O157. Can J Vet Res. 2011, 75: 98-105.
Wileman BW, Thomson DU, Olson KC, Jaeger JR, Pacheco LA, Bolte J, Burkhardt DT, Emery DA, Straub D: Escherichia coli O157: H7 shedding in vaccinated beef calves born to cows vaccinated prepartum with Escherichia coli O157: H7 SRP vaccine. J Food Prot. 2011, 74 (10): 1599-1604. 10.4315/0362-028X.JFP-11-034.
Jacob ME, Fox JT, Drouillard JS, Renter DG, Nagaraja TG: Evaluation of Feeding Dried Distiller's Grains with Solubles and Dry-Rolled Corn on the Fecal Prevalence of Escherichia coli O157: H7 and Salmonella spp. in Cattle. Foodborne Pathog Dis. 2009, 6 (2): 145-153. 10.1089/fpd.2008.0159.
Wells JESS, Berry ED, Kalchayanand N, Guerini MN, Varel VH, Arthur TM, Bosilevac JM, Freetly HC, Wheeler TL, et al: Prevalence and level of Escherichia coli O157: H7 in feces and on hides of feedlot steers fed diets with or without wet distillers grains with solubles. J Food Prot. 2009, 72 (8): 1624-1633.
Edrington TS, MacDonald JC, Farrow RL, Callaway TR, Anderson RC, Nisbet DJ: Influence of wet distiller's grains on prevalence of Escherichia coli O157: H7 and Salmonella in feedlot cattle and antimicrobial susceptibility of generic Escherichia coli isolates. Foodborne Pathog Dis. 2010, 7 (5): 605-608. 10.1089/fpd.2009.0417.
Durso LM, Wells JE, Harhay GP, Rice WC, Kuehn L, Bono JL, Shackelford S, Wheeler T, Smith TP: Comparison of bacterial communities in faeces of beef cattle fed diets containing corn and wet distillers’ grain with solubles. Lett Appl Microbiol. 2012, 55 (2): 109-114. 10.1111/j.1472-765X.2012.03265.x.
Wells JE, Shackelford SD, Berry ED, Kalchayanand N, Bosilevac JM, Wheeler TL: Impact of reducing the level of wet distillers grains fed to cattle prior to harvest on prevalence and levels of Escherichia coli O157: H7 in feces and on hides. J Food Prot. 2011, 74 (10): 1611-1617. 10.4315/0362-028X.JFP-11-160.
Stephens TP, Loneragan GH, Karunasena E, Brashears MM: Reduction of Escherichia coli O157 and Salmonella in feces and on hides of feedlot cattle using various doses of a direct-fed microbial. J Food Prot. 2007, 70 (10): 2386-2391.
Peterson RE, Klopfenstein TJ, Erickson GE, Folmer J, Hinkley S, Moxley RA, Smith DR: Effect of Lactobacillus acidophilus strain NP51 on Escherichia coil O157: H7 fecal shedding and finishing performance in beef feedlot cattle. J Food Prot. 2007, 70 (2): 287-291.
Younts-Dahl SM, Osborn GD, Galyean ML, Rivera JD, Loneragan GH, Brashears MM: Reduction of Escherichia coli O157 in finishing beef cattle by various doses of Lactobacillus acidophilus in direct-fed microbials. J Food Prot. 2005, 68 (1): 6-10.
Stanford K, McAllister TA, Niu YD, Stephens TP, Mazzocco A, Waddell TE, Johnson RP: Oral delivery systems for encapsulated bacteriophages targeted at Escherichia coli O157: H7 in feedlot cattle. J Food Prot. 2010, 73 (7): 1304-1312.
Edrington TS, Farrow RL, Mackinnon KM, Callaway TR, Anderson RC, Nisbet DJ: Influence of vitamin D on fecal shedding of Escherichia coli O157: H7 in naturally colonized cattle. J Food Prot. 2012, 75 (2): 314-319. 10.4315/0362-028X.JFP-11-335.
Paddock ZD, Walker CE, Drouillard JS, Nagaraja TG: Dietary monensin level, supplemental urea, and ractopamine on fecal shedding of Escherichia coli O157: H7 in feedlot cattle. J Anim Sci. 2011, 89 (9): 2829-2835. 10.2527/jas.2010-3793.
Ellis-Iversen J, Smith R, Van Winden S, Paiba G, Watson E, Snow L, Cook A: Farm practices to control E. coli O157 in young cattle - a randomised controlled trial. Vet Res. 2008, 39: 3-10.1051/vetres:2007041.
Berry ED, Wells JE: Soil solarization reduces Escherichia coli O157: H7 and total Escherichia coli on cattle feedlot pen surfaces. J Food Prot. 2012, 75 (1): 7-13. 10.4315/0362-028X.JFP-11-283.
Safdar N, Said A, Gangnon RE, Maki DG: Risk of hemolytic uremic syndrome after antibiotic treatment of Escherichia coli O157: H7 enteritis: a meta-analysis. JAMA. 2002, 288 (8): 996-1001. 10.1001/jama.288.8.996.
Panos GZ, Betsi GI, Falagas ME: Systematic review: are antibiotics detrimental or beneficial for the treatment of patients with Escherichia coli O157: H7 infection?. Aliment Pharmacol Ther. 2006, 24 (5): 731-742. 10.1111/j.1365-2036.2006.03036.x.
Ejemot RI, Ehiri JE, Meremikwu MM, Critchley JA: Hand washing for preventing diarrhoea. Cochrane Database Syst Rev. 2008, 1: CD004265
Proulx F, Turgeon JP, Delage G, Lafleur L, Chicoine L: Randomized, controlled trial of antibiotic therapy for Escherichia coli O157: H7 enteritis. J Pediatr. 1992, 121 (2): 299-303. 10.1016/S0022-3476(05)81209-0.
Rowe PC, Milner R, Orrbine E, Klassen TP, Mackenzie AM, Wells GA: A phase ll randomized controlled trial of SYNSORB Pk for prevention of hemolytic uremic syndrome in children with verotoxin producing E. coli (STEC) gastroenteritis [abstract]. Pediatr Res. 1997, 41: 283A-
Taylor C, Bitzan M, Reymond D: Shigatec: a Phase II study assessing monoclonal antibodies against Shiga toxin 1 and 2 in Shiga toxin-producing E.coli-infected children. Pediatr Nephrol. 2011, 26: 1595-1596.
Callaway TR, Elder RO, Keen JE, Anderson RC, Nisbet DJ: Forage feeding to reduce preharvest Escherichia coli populations in cattle, a review. J Dairy Sci. 2003, 86 (3): 852-860. 10.3168/jds.S0022-0302(03)73668-6.
FDA Finalizes Report on. 2006, http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2007/ucm108873.htm, Spinach Outbreak,
Investigation Update: Multistate Outbreak of E. coli O157: H7 Infections Associated with Cheese. http://www.cdc.gov/ecoli/2010/cheese0157/index.html,
Jacob ME, Fox JT, Narayanan SK, Drouillard JS, Renter DG, Nagaraja TG: Effects of feeding wet corn distillers grains with solubles with or without monensin and tylosin on the prevalence and antimicrobial susceptibilities of fecal foodborne pathogenic and commensal bacteria in feedlot cattle. J Anim Sci. 2008, 86 (5): 1182-1190.
Arthur TM, Bosilevac JM, Kalchayanand N, Wells JE, Shackelford SD, Wheeler TL, Koohmaraie M: Evaluation of a direct-fed microbial product effect on the prevalence and load of Escherichia coli O157: H7 in feedlot cattle. J Food Prot. 2010, 73 (2): 366-371.
Queensland Health: Shiga toxin-producing Escherichia coli (STEC) infection. June 2013, http://www.health.qld.gov.au/cdcg/index/stec.asp
Outbreak Control EHEC Information Center: http://www.outbreakcontrol.com/en/leftnav/ehec-information-center,
Pavia AT, Nichols CR, Green DP, Tauxe RV, Mottice S, Greene KD, Wells JG, Siegler RL, Brewer ED, Hannon D, et al: Hemolytic-uremic syndrome during an outbreak of Escherichia coli O157: H7 infections in institutions for mentally retarded persons: clinical and epidemiologic observations. J Pediatr. 1990, 116 (4): 544-551. 10.1016/S0022-3476(05)81600-2.
Allaby MA, Mayon-White R: Escherichia coli O 157: outbreak in a day nursery. Commun Dis Rep CDR Rev. 1995, 5 (1): R4-R6.
Al-Jader L, Salmon RL, Walker AM, Williams HM, Willshaw GA, Cheasty T: Outbreak of Escherichia coli O157 in a nursery: lessons for prevention. Arch Dis Child. 1999, 81 (1): 60-63. 10.1136/adc.81.1.60.
Henning PH, Tham EB, Martin AA, Beare TH, Jureidini KF: Haemolytic-uraemic syndrome outbreak caused by Escherichia coli O111:H-: clinical outcomes. Med J Aust. 1998, 168 (11): 552-555.
APHL STEC Work Group: Guidance for Public Health laboratories on the isolation and characterization of shiga toxin-producing Escherichia coli (STEC) from clinical specimens. . 2012, http://www.aphl.org/AboutAPHL/publications/Documents/FS_2012April_Guidance-for-PHLs-Isolation-and-Characterization-of-Shiga-Toxin-Producing-Escherichia-coli-STEC-from-Clinical.pdf, April ,
Preventing person-to-person spread following gastrointestinal infections: guidelines for public health physicians and environmental health officers. http://www.hpa.org.uk/cdph/issues/CDPHvol7/No4/guidelines2_4_04.pdf,
Advice if you are a patient or care for a patient. http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/EscherichiaColiO157/PatientCarer/?printable=true,
Bender JN: Compendium of Measures To Prevent Disease Associated with Animals in Public Settings. MMWR CDC. 2005, 54: RR-4-
Bell BP, Griffin PM, Lozano P, Christie DL, Kobayashi JM, Tarr PI: Predictors of hemolytic uremic syndrome in children during a large outbreak of Escherichia coli O157: H7 infections. Pediatr. 1997, 100 (1): E12-10.1542/peds.100.1.e12.
Five keys to safer food. http://www.who.int/foodsafety/publications/consumer/en/5keys_en.pdf,
Dunn J: National Association of State Public Health Veterinarians IN: Compendium of Measures to Prevent Disease Associated with Animals in Public Settings. 2011, 1-24. http://www.cdc.gov/mmwr/preview/mmwrhtml/rr6004a1.htm,
Avoiding infection on farm visits. Advice for the public. http://www.hpa.org.uk/web/HPAwebFile/HPAweb_C/1270122184581,
Warshawsky B, Gutmanis I, Henry B, Dow J, Reffle J, Pollett G, Ahmed R, Aldom J, Alves D, Chagla A, et al: Outbreak of Escherichia coli 0157: H7 related to animal contact at a petting zoo. Can J Infect Dis. 2002, 13 (3): 175-181.
Brewster DH, Brown MI, Robertson D, Houghton GL, Bimson J, Sharp JC: An outbreak of Escherichia coli O157 associated with a children's paddling pool. Epidemiol Infect. 1994, 112 (3): 441-447. 10.1017/S0950268800051141.
Hildebrand JM, Maguire HC, Holliman RE, Kangesu E: An outbreak of Escherichia coli O157 infection linked to paddling pools. Commun Dis Rep CDR Rev. 1996, 6 (2): R33-R36.
Guidelines for safe recreational waters. http://www.who.int/water_sanitation_health/bathing/en/,
Draft - Guidelines for Disinfecting Public Swimming Pools and Spa Pools. http://www.health.nsw.gov.au/environment/factsheets/Pages/disinfection-pools.aspx,
Managing health and safety in swimming pools. http://www.hse.gov.uk/pubns/books/hsg179.htm,
Recommended Operating Guidelines for Swimming Pools in BC. http://www.bcrpa.bc.ca/recreation_parks/aquatics/documents/bc-pool-operationsguidelinesFINAL.pdf,
Samadpour M, Stewart J, Steingart K, Addy C, Louderback J, McGinn M, Ellington J, Newman T: Laboratory investigation of an E. coli O157: H7 outbreak associated with swimming in Battle Ground Lake, Vancouver, Washington. J Environ Health. 2002, 64: 16-20.
Guidelines for Managing Risks in Recreational Water. http://www.nhmrc.gov.au/_files_nhmrc/publications/attachments/eh38.pdf,
Whitman RL, Przybyla-Kelly K, Shively DA, Nevers MB, Byappanahalli MN: Hand-mouth transfer and potential for exposure to E. coli and F + coliphage in beach sand, Chicago, Illinois. J Water Health. 2009, 7 (4): 623-629. 10.2166/wh.2009.115.
Yamahara KM, Layton BA, Santoro AE, Boehm AB: Beach sands along the California coast are diffuse sources of fecal bacteria to coastal waters. Environ Sci Technol. 2007, 41 (13): 4515-4521. 10.1021/es062822n.
Holme R: Drinking water contamination in Walkerton, Ontario: positive resolutions from a tragic event. Water Sci Technol. 2003, 47 (3): 1-6.
Canadian Drinking Water Guidelines. http://www.hc-sc.gc.ca/ewh-semt/water-eau/drink-potab/guide/index-eng.php,
Australian Drinking Water Guidelines. http://www.nhmrc.gov.au/publications/synopses/eh19syn.htm,
Clean hands protect against infection. http://www.who.int/gpsc/clean_hands_protection/en/index.html,
Hand-washing. http://www.mayoclinic.com/health/hand-washing/HQ00407,
Infection control - UK handwashing guidelines. http://www.nice.org.uk/guidance/CG2,
Hand washing. http://www.nhmrc.gov.au/_files_nhmrc/file/guidelines/consult/consultations/ICG_draft_10jan10.pdf,
Assuring food safety and quality: Guidelines for strengthening national food control systems. http://www.who.int/foodsafety/publications/capacity/en/Englsih_Guidelines_Food_control.pdf,
Regulation (EC) no 178/2002 of the European Parliament and of the Council of 28 January2002 laying down the general principles and requirements of food law, establishing the European Food Safety Authority and laying down procedures in matters of food safety. http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2002:031:0001:0024:EN:PDF,
Deadly E coli outbreak in Germany should be a warning. http://live.psu.edu/story/53862,
Enterohaemorrhagic Escherichia coli (EHEC). http://www.who.int/mediacentre/factsheets/fs125/en/,
Multistate Outbreak of E. coli O157: H7 Infections Associated with Beef from Fairbank Farms. http://www.cdc.gov/ecoli/2009/1124.html,
Investigation of Multistate Outbreak of E. coli O157: H7 Infections. http://www.fsis.usda.gov/Fsis_Recalls/,
Multistate Outbreak of E. coli O157 Infections Linked to Topp's Brand Ground Beef Patties. http://www.fsis.usda.gov/PDF/Recall_040_2007_Exp_Update.pdf,
Multistate Outbreak of E. coli O157: H7 Infections Associated with Beef from JBS Swift Beef Company. http://www.cdc.gov/ecoli/2009/0701.html,
Multistate Outbreak of E. coli O157: H7 Infections Associated with Beef from National Steak and Poultry. http://www.cdc.gov/ecoli/2010/0105.html,
Caprioli A, Luzzi I, Rosmini F, Resti C, Edefonti A, Perfumo F, Farina C, Goglio A, Gianviti A, Rizzoni G: Community-wide outbreak of hemolytic-uremic syndrome associated with non-O157 verocytotoxin-producing Escherichia coli. J Infect Dis. 1994, 169 (1): 208-211. 10.1093/infdis/169.1.208.
Investigation of Outbreak of Human Infections Caused by E. coli O157: H7. http://www.cdc.gov/ecoli/2007/october/103107.html,
Tracing seeds, in particular fenugreek (Trigonella foenum-graecum) seeds, in relation to the Shiga toxin-producing E. coli (STEC) O104:H4. 2011, http://www.efsa.europa.eu/en/supporting/pub/176e.htm, Outbreaks in Germany and France,
Investigation Update: Multistate Outbreak of Human E. coli O145 Infections Linked to Shredded Romaine Lettuce from a Single Processing Facility. http://www.cdc.gov/ecoli/2010/ecoli_o145/index.html,
Update on Multi-State Outbreak of E. coli O157: H7 Infections From Fresh Spinach, October 6. 2006, http://www.cdc.gov/foodborne/ecolispinach/100606.htm,
Deschenes G, Casenave C, Grimont F, Desenclos JC, Benoit S, Collin M, Baron S, Mariani P, Grimont PA, Nivet H: Cluster of cases of haemolytic uraemic syndrome due to unpasteurised cheese. Pediatr Nephrol. 1996, 10 (2): 203-205.
CDC: Outbreak of Escherichia coli O157: H7 infection associated with eating fresh cheese curds--Wisconsin, June 1998. JAMA. 2000, 284 (23): 2991-2992.
Multistate Outbreak of E. coli O157: H7 Infections Linked to Eating Raw Refrigerated, Prepackaged Cookie Dough. http://www.cdc.gov/ecoli/2009/0630.html,
From the Centers for Disease Control and Prevention: Outbreak of Escherichia coli O157: H7 infections associated with drinking unpasteurized commercial apple juice--British Columbia, California, Colorado, and Washington, October 1996. JAMA. 1996, 276 (23): 1865-
Keene WE, Hedberg K, Herriott DE, Hancock DD, McKay RW, Barrett TJ, Fleming DW: A prolonged outbreak of Escherichia coli O157: H7 infections caused by commercially distributed raw milk. J Infect Dis. 1997, 176 (3): 815-818. 10.1086/517310.
Goh S, Newman C, Knowles M, Bolton FJ, Hollyoak V, Richards S, Daley P, Counter D, Smith HR, Keppie N: E. coli O157 phage type 21/28 outbreak in North Cumbria associated with pasteurized milk. Epidemiol Infect. 2002, 129 (3): 451-457. 10.1017/S0950268802007835.
Bielaszewska M, Janda J, Blahova K, Minarikova H, Jikova E, Karmali MA, Laubova J, Sikulova J, Preston MA, Khakhria R, et al: Human Escherichia coli O157: H7 infection associated with the consumption of unpasteurized goat's milk. Epidemiol Infect. 1997, 119 (3): 299-305. 10.1017/S0950268897008297.
Guh A, Phan Q, Nelson R, Purviance K, Milardo E, Kinney S, Mshar P, Kasacek W, Cartter M: Outbreak of Escherichia coli O157 associated with raw milk, Connecticut, 2008. Clin Infect Dis. 2010, 51 (12): 1411-1417. 10.1086/657304.
Milne LM, Plom A, Strudley I, Pritchard GC, Crooks R, Hall M, Duckworth G, Seng C, Susman MD, Kearney J, et al: Escherichia coli O157 incident associated with a farm open to members of the public. Commun Dis Public Health. 1999, 2 (1): 22-26.
O'Brien SJ, Adak GK, Gilham C: Contact with farming environment as a major risk factor for Shiga toxin (Vero cytotoxin)-producing Escherichia coli O157 infection in humans. Emerg Infect Dis. 2001, 7 (6): 1049-1051. 10.3201/eid0706.010626.
Crump JA, Sulka AC, Langer AJ, Schaben C, Crielly AS, Gage R, Baysinger M, Moll M, Withers G, Toney DM, et al: An outbreak of Escherichia coli O157: H7 infections among visitors to a dairy farm. N Engl J Med. 2002, 347 (8): 555-560. 10.1056/NEJMoa020524.
Bruce MG, Curtis MB, Payne MM, Gautom RK, Thompson EC, Bennett AL, Kobayashi JM: Lake-associated outbreak of Escherichia coli O157: H7 in Clark County, Washington, August 1999. Arch Pediatr Adolesc Med. 2003, 157 (10): 1016-1021. 10.1001/archpedi.157.10.1016.
Hygiene practice manual for radish sprouts production in Japan. http://www.fao.org/docrep/meeting/004/x6923e.htm,
Bielaszewska M, Mellmann A, Zhang W, Kock R, Fruth A, Bauwens A, Peters G, Karch H: Characterisation of the Escherichia coli strain associated with an outbreak of haemolytic uraemic syndrome in Germany, 2011: a microbiological study. Lancet Infect Dis. 2011, 11 (9): 671-676.
Information for Public Health Professionals. http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/EscherichiaColiO157/PublicHealth/,
Human Illness caused by E. coli O157: H7 from food and non-food sources. http://fri.wisc.edu/docs/pdf/FRIBrief_EcoliO157H7humanillness.pd,
CDC: Escherichia coli O157: H7 outbreak linked to commercially distributed dry-cured salami--Washington and California, 1994. JAMA. 1995, 273 (13): 985-986.
ABC health report. http://www.daff.gov.au/biosecurity/quarantine/legislation/imp-food-control/app-h,
Uncooked fermented meats. http://www.foodstandards.gov.au/foodstandards/proposals/proposalp217uncookedunfermentedmeats/uncookedfermentedmea1148.cfm,
Miko A, Pries K, Haby S, Steege K, Albrecht N, Krause G, Beutin L: Assessment of Shiga toxin-producing Escherichia coli isolates from wildlife meat as potential pathogens for humans. Appl Environ Microbiol. 2009, 75 (20): 6462-6470. 10.1128/AEM.00904-09.
Meat preparation: Food safety of Jerky. http://www.fsis.usda.gov/wps/portal/fsis/topics/food-safety-education/getanswers/food-safety-fact-sheets/meat-preparation/jerky-and-food-safety,
Food Safety:Guidance on skills and knowledge for food businesses. http://www.foodstandards.gov.au/industry/safetystandards/safetypractices/Pages/default.aspx,
Safe food handling. http://www.fsis.usda.gov/wps/portal/fsis/topics/food-safety-education/get-answers/food-safety-factsheets/safe-food-handling,
Safer food, better business. http://www.food.gov.uk/foodindustry/regulation/foodlaw/,
Guide to Minimize Microbial Food Safety Hazards of Fresh-cut Fruits and Vegetables. http://www.fda.gov/downloads/Food/GuidanceComplianceRegulatoryInformation/GuidanceDocuments/ProduceandPlanProducts/UCM169112.pdf,
PHLS: Guidelines for the control of infection with Vero cytotoxin producing Escherichia coli (VTEC). Commun Dis Public Health. 2000, 3 (1): 14-23.
Escherichia coli O157: H7 and other Shiga toxin-producing Escherichia coli (STEC). http://www.cdc.gov/ecoli/general/index.html#what_shiga,
Snedeker KG, Campbell M, Sargeant JM: A Systematic Review of Vaccinations to Reduce the Shedding of Escherichia coli O157 in the Faeces of Domestic Ruminants. Zoonoses Public Health. 2012, 59: 126-138. 10.1111/j.1863-2378.2011.01426.x.
Peterson RE, Klopfenstein TJ, Moxley RA, Erickson GE, Hinkley S, Rogan D, Smith DR: Efficacy of dose regimen and observation of herd immunity from a vaccine against Escherichia coli O157: H7 for feedlot cattle. J Food Prot. 2007, 70 (11): 2561-2567.
New vaccines may help thwart E. coli O157: H7. http://www.ars.usda.gov/is/pr/2009/091217.htm,
Fox JT, Depenbusch BE, Drouillard JS, Nagaraja TG: Dry-rolled or steam-flaked grain-based diets and fecal shedding of Escherichia coli O157 in feedlot cattle. J Anim Sci. 2007, 85 (5): 1207-1212. 10.2527/jas.2006-079.
Cernicchiaro N, Pearl DL, McEwen SA, Zerby HN, Fluharty FL, Loerch SC, Kauffman MD, Bard JL, LeJeune JT: A randomized controlled trial to assess the impact of dietary energy sources, feed supplements, and the presence of super-shedders on the detection of Escherichia coli O157: H7 in feedlot cattle using different diagnostic procedures. Foodborne Pathog Dis. 2010, 7 (9): 1071-1081. 10.1089/fpd.2009.0531.
Diez-Gonzalez F, Callaway TR, Kizoulis MG, Russell JB: Grain feeding and the dissemination of acid-resistant Escherichia coli from cattle. Sci. 1998, 281 (5383): 1666-1668.
Meng J, Zhao S, Doyle MP, Joseph SW: Antibiotic resistance of Escherichia coli O157: H7 and O157:NM isolated from animals, food, and humans. J Food Prot. 1998, 61 (11): 1511-1514.
Wong CS, Jelacic S, Habeeb RL, Watkins SL, Tarr PI: The risk of the hemolytic-uremic syndrome after antibiotic treatment of Escherichia coli O157: H7 infections. N Engl J Med. 2000, 342 (26): 1930-1936. 10.1056/NEJM200006293422601.
U.S. calls antibiotics wrong step on E. coli. http://www.nytimes.com/2011/06/03/health/03treatment.html,
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2458/13/799/prepub
Acknowledgements
Ruth Mitchell assisted with the searches and search strategy. Elizabeth Elliott is supported by an Australian National Health and Medical Research Council Practitioner Fellowship (ID 457084).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
Both authors drafted and wrote the manuscript, revised it critically for intellectual content and read and approved the final manuscript. Both authors read and approved the final manuscript.
Electronic supplementary material
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Thomas, D.E., Elliott, E.J. Interventions for preventing diarrhea-associated hemolytic uremic syndrome: systematic review. BMC Public Health 13, 799 (2013). https://doi.org/10.1186/1471-2458-13-799
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2458-13-799