Abstract
Background
Cardio-metabolic diseases (CMDs) are a growing public health problem, but data on incidence, trends, and costs in developing countries is scarce. Comprehensive and standardised surveillance for non-communicable diseases was recommended at the United Nations High-level meeting in 2011.
Aims: To develop a model surveillance system for CMDs and risk factors that could be adopted for continued assessment of burdens from multiple perspectives in South-Asian countries.
Methods
Design: Hybrid model with two cross-sectional serial surveys three years apart to monitor trend, with a three-year prospective follow-up of the first cohort.
Sites: Three urban settings (Chennai and New Delhi in India; Karachi in Pakistan), 4000 participants in each site stratified by gender and age.
Sampling methodology: Multi-stage cluster random sampling; followed by within-household participant selection through a combination of Health Information National Trends Study (HINTS) and Kish methods.
Culturally-appropriate and methodologically-relevant data collection instruments were developed to gather information on CMDs and their risk factors; quality of life, health-care utilisation and costs, along with objective measures of anthropometric, clinical and biochemical parameters. The cohort follow-up is designed as a pilot study to understand the feasibility of estimating incidence of risk factors, disease events, morbidity, and mortality.
Results
The overall participant response rate in the first cross-sectional survey was 94.1% (Chennai 92.4%, n = 4943; Delhi 95.7%, n = 4425; Karachi 94.3%, n = 4016). 51.8% of the participants were females, 61.6% < 45years, 27.5% 45–60years and 10.9% >60 years.
Discussion
This surveillance model will generate data on prevalence and trends; help study the complex life-course patterns of CMDs, and provide a platform for developing and testing interventions and tools for prevention and control of CMDs in South-Asia. It will also help understanding the challenges and opportunities in establishing a surveillance system across countries.
Similar content being viewed by others
Background
Cardio-metabolic diseases (CMDs) broadly comprise of diabetes mellitus, cardiovascular diseases (CVD), chronic kidney disease (CKD) and their common interconnected risk factors such as obesity, insulin resistance, glucose intolerance, dyslipidaemia, and hypertension. They are a growing public health problem worldwide [1] accompanying socioeconomic and nutrition transitions [2–4]. Coronary heart disease (CHD), cerebrovascular disease, and diabetes together account for 30% of global mortality and 80% of these deaths occur in low-and-middle-income countries (LMICs) [2, 5–7]. In 2010, globally, 4,000,000 deaths were due to diabetes, the highest in absolute numbers was (1,008,000) in India [8]. The largest fraction of deaths from CHD (37%) and stroke (30%) attributable to high blood glucose were in South-Asia [9]. Further, in people of South-Asian origin, onset of diabetes [10–12], other cardio-metabolic risk factors [13, 14], and late-stage disease events [15, 16] occur at lower body mass indices and younger ages than other ethnic groups [16–23].
Key recommendations of the 2011 United Nations high-level meeting on non-communicable diseases (NCDs) and the US Institute of Medicine are initiation and strengthening of surveillance for NCDs [24] and the creation of integrated, comprehensive, sustainable, on-going nationwide surveillance systems [25]. In South-Asia, current efforts are limited to local surveys with vast state-wise heterogeneity and variable data quality [26–28]. Furthermore, projections of national income losses related to CMDs are based on models using inputs from limited local studies [29]; data on individual and household costs and social burdens are also scarce [30]. Current efforts by the Governments of India and Pakistan in setting up nationwide surveillance of NCDs are limited to self-reported surveys [31, 32]. A robust surveillance system would need to be representative of the population of interest, utilise standardised methods that are not solely reliant on self-reporting, be amenable to scaling up, would be sustainably financed by the country/region itself, and also become a platform for further research opportunities and policy guidance (much like the role of the Centres for Disease Control and Prevention [CDC] in the United States) [33, 34].
We present the design and methods of a model surveillance system for CMDs, the CARRS (Centre for cArdiometabolic Risk Reduction in South-Asia)-Surveillance Study, which could be adopted for continuing assessments of burdens in South-Asian countries. The CARRS-Surveillance study builds on the WHO STEPS (World Health Organisation stepwise Approach to Surveillance) model [35] to capture prevalence of risk factors, CMDs, and their socioeconomic impact in serial representative surveys to understand trends, but goes a step further to convert the cross-sectional survey into a large, urban, sub-continent wide prospective cohort at lower-costs, to understand the incidence of risk factors, diseases, complications, and mortality. Thus, apart from estimating burdens, it can be used to develop South-Asian assessment and clinical management systems to tailor care and preventive approaches.
Methods
Study design
This is a hybrid cohort-modelled cross-sectional multi-centre surveillance study to be conducted over a period of four years. Two cross-sectional surveys conducted three years apart on standalone representative samples of each of the three city-wide populations, using objective measures will permit estimation of the prevalence and trends of CMDs and their risk factors. Those enrolled in the first cross-sectional survey will be followed as a cohort in a three-year study to estimate (i) the incidence of new risk factors (such as obesity, hypertension, diabetes,); (ii) incidence of later-stage target organ diseases such as peripheral vascular disease, stroke, myocardial infarction, congestive heart failure, chronic stable angina, CKD, retinopathy, neuropathy, and amputation; (iii) assessment of health service utilisation and costs including hospitalisation and outpatient use and (iv) morbidity and mortality associated with CMDs.
The first cross-sectional survey has been completed with ongoing first year of cohort-follow-up. The survey was comprehensive, undertaking assessments of quality of Life (QoL), and socioeconomic burdens on individuals and families with regards to these diseases. Participants underwent anthropometric measurements, blood pressure (BP) assessment, and provided biochemical specimens. The cohort follow-up was limited to patient reports with recording of BP and anthropometry. CMDs and their complications were diagnosed using standard definitions and coded using the International Classification of Diseases 10 (ICD-10) codes.
The study sites are metropolitan urban settings with large, growing (due to continued births and migration from various parts of the country), and heterogeneous populations. Estimates suggest that population size in Chennai (4.68 million) [36], Karachi (13 million) [37], and Delhi (16.3 million) [36], and the diversity in their composition make these cities current and future archetypes of rapid socio-economic, demographic, epidemiologic, and nutrition/lifestyle transitions in the South-Asian region.
Sample size estimation
Utilising risk factor prevalence estimates from previously published Indian and Pakistani studies and anticipating a response rate of 80% with a design effect factor of 1.5 (to account for cluster sampling), the sample size estimates were generated for males and females in three age strata in each urban setting. As shown in table 1, the highest required sample size (3983 rounded-off to 4000 participants) permits each site to reliably estimate one or more of the CMD risk factors for each of the gender and age strata leading to a total sample size of 12,000.
With regards to the cohort follow-up, separate consent has been taken from participants to be followed up for three years or longer. An overall 15 - 25% loss-to-follow-up by the 3-year data collection time-period is anticipated due to the high probability of migration among the young population for job opportunities, marriage (in case of females), etc. Retention efforts (in the form of maintaining updated contact information; collecting contact details of friends and relatives; periodic reminder calls; courtesy calls/visits) have been put in place to keep track of participants and minimise loss-to-follow-up. Although the study at present is not powered to estimate incidence of CMDs and their risk factors, it has the potential to determine such incidence rates if the follow-up period is increased and the study is scaled up by adding follow up of subsequent cross-sectional samples.
Sampling method
Households were selected in each of the three cities using a multi-stage cluster random sampling technique. Each city has its own distinctive municipal sub-divisions, encompassing municipal corporations, wards and Census Enumeration Blocks (CEB), which were used sequentially as sampling frames to randomly select households. While wards were the primary sampling units (PSUs) for Chennai and Delhi, CEBs or clusters were the PSUs for Karachi. STATA version 10.1 (Statacorp, TX) [38] and data from the most recent census were used to randomly select the wards, CEBs, and households (defined below.). To give each household an equal chance of being selected for the study and to identify households constructed after the last census survey, manual listing and mapping of all households in each CEB was done before randomly selecting them.
Two participants, one male and one female, aged 20 years or older, were selected from each household based on inclusion and exclusion criteria given below. Two methods were used for within household sampling – (i) for households with one to two adults (≥20 years), the sampling strategy described in the 2002 Health Information National Trends Study (HINTS) in the USA was used [39]. According to HINTS, one or both individuals (one male and one female) were selected and enrolled into the study based on eligibility criteria and informed consent; (ii) for households with more than two eligible adults, the “Kish method” used in the WHO’s STEPS surveys [35] was applied. Recruitment of participants, and data and specimen collection were conducted through three visits to each participant’s place of residence, respectively (Visit-0, Visit-1, and Visit-2).
Inclusion and exclusion criteria for CARRS – Surveillance Study
Inclusion criteria
Any individual aged ≥20 years and permanently residing in the selected household.
For the purpose of this study, a permanent resident was defined as a person living in the selected household, was related to the household head and ate at least 3 meals in a week with the family.
Households were defined as “a group of people who live together, usually pool their income and eat at least one meal together a day when they are at home. This does not include people who have migrated permanently or are considered visitors” [(Integrated Disease Surveillance Project (IDSP)][31].
Exclusion criteria
Pregnant women were not included in the study since their biochemical parameters would vary from the normal physiology due to pregnancy, further their patterns of diet and physical activity would also be different from usual.
Bed-ridden individuals were excluded because of the difficulty in taking anthropometric measurements in these individuals. However, reasons for being confined to bed were collected from such individuals to estimate prevalence of CMDs among this excluded group (since CMDs can be the cause for being bed-ridden).
Surveillance indicators and study instruments
To provide consistency and reproducibility of the results across multiple sites, comprehensive and uniform data collection instruments were used to capture measurements (table 2). Household data were collected through interviewer administered paper questionnaires in English or the preferred local languages (Hindi, Tamil, and Urdu). Validated questions were derived from English questionnaires used in the WHO Multinational MONItoring of trends and determinants in CArdiovascular disease (MONICA) study [40], WHO STEPS studies [35], and from previous regional and national surveys. Using these, culturally-appropriate and methodologically-relevant closed-questions, an instrument for South-Asia was developed and pilot tested for face and construct validity prior to use in the study. Several sections of the baseline questionnaire (such as the QoL, CMD history, tobacco and alcohol consumption questions) were based on validated questionnaires that already exist in regional languages (Tamil, Hindi and Urdu). Questionnaires to elicit medical and treatment history, costs and QoL are being used to collect incident events during the ongoing cohort follow-up. Further, verbal autopsy is being performed using a reliable instrument to ascertain cause of death of participants who die during the course of follow-up and for whom either death certificate was unavailable or cause of death not certified. For the adapted instruments collecting a variety of CMD risks and diseases (e.g. tobacco, history of CMD, heart failure, and Chronic Obstructive Pulmonary Disease), the subjective history provided by participants was validated against laboratory and other diagnostic gold standards (e.g., salivary cotinine for tobacco consumption). These in-built steps to validate the self-reported data distinguishes the CARRS-Surveillance as a stronger model compared to the IDSP [31] and the INDEPTH network (International Network of field sites for continuous Demographic Evaluation of Populations and Their Health in developing countries (http://www.indepth-network.org) [41].
Biological sample collection and storage
Biological sample collection involved drawing 15 ml of blood (in fasting state) from each participant, collecting urine (early morning void), and 1000 to 2000 μl of saliva (fasting) in Salivettes. While blood and urine were collected from all participants, saliva was collected from 5% of the study participants (i.e. 200 participants per site). The samples were transported from field sites in cold chain to the laboratories for analysis. Sample aliquots were also stored in cryo-vials at - 80 degrees Celsius for future studies. The methods of analysis and external quality control have been standardised for all biological samples across the study sites (table 3). There is one exception in that Apolipoprotein A and B analyses were not conducted in Karachi due to lack of required laboratory facilities for the test.
Clinical and anthropometric assessments
Two clinical (BP and pulse rate) and eight anthropometric measurements of participants were taken during the visits: Clinical measurements - BP and Pulse rate. Anthropometric measurements - Mid-arm circumference, Waist circumference, Hip circumference, Triceps skin-fold, Sub-scapular skin-fold, Supra-patellar skin-fold, Height (Standing) and Body composition analysis by Bio-impedance.
The equipment and methods used for BP and anthropometric measurements were standardised and certified, and have been used in other epidemiological studies in the South-Asian population. BP was measured using electronic sphygmomanometer; Omron HEM-7080 and HEM-7080IT-E; Omron Corporation, Tokyo, Japan (certified by the British Hypertensive Society and the American association for Advancement of Medical Instrumentation [AAMI] protocols). Skinfold Calipers (Holtain Ltd., UK) and non-stretch measuring tape (Gulick II, Country Technology, Gays Mills, WI) were used to measure skin-fold thickness and body circumferences, respectively. Height was measured using a portable Stadiometer (SECA Model 213, SecaGmbh Co, Hamburg, Germany). Apart from these, body-composition analysers (instrument which measures body fat by sending out weak electric currents to measure impedance/electrical resistance by different tissues of the body); Tanita BC-418 in Delhi and Chennai, and BC-545 in Karachi were used to measure compartmental body fat distribution. To ensure standardisation, both instruments were tested in 50 male and 50 female participants to compare the parameters measured; i.e. weight, body mass index, basal metabolic rate, body fat and visceral fat. The results showed that all measured parameters were highly co-related for both males and females (r > 0.95, p < 0.05) between the two instruments, except body fat in males (r = 0.67, p = 0.67). Methods for BP measurement and anthropometric measures were based on the recommendation of the American Heart Association’s Council on High Blood Pressure Research [42] and the third National Health and Nutrition Examination Survey (NHANES-III) [43].
Data management
An online system was developed in an ‘open source’ platform PHP (Hypertext PreProcessor, scripting language for the web page/front end) and MySQL (My Structured Query Language) for data entry and database management at each site. This online database has been programmed to have automated in-built checks for logic which are ‘clinically reasonable’ (such as ranges, absolute and relative values, context and structure). It provides an efficient means of data entry, storage, and quality control. Data are available at the coordinating site for immediate feedback and timely corrections. The data have been stored in pass-word protected files and questionnaires in locked cabinets in all study sites, and only the study personnel have access to these. All information related to participant identification was de-linked from the data files before analysis to maintain anonymity.
Quality control strategies
Quality control (QC) strategies were applied using a framework which comprehensively considers each phase of the study and applies inter-related themes to every level of the study and are described in table 4. Apart from standardisation of laboratory methods (table 3), QC involved laboratory procedure assessment at two levels. Level-1, internal quality control: Local laboratories attached with the study centre followed their own internal quality control standard operating procedures (SOPs) to ensure accuracy, precision, and reproducibility. Level-2; external quality control: Irrespective of the nature of existing laboratory accreditation and / or SOP’s, all study site laboratories were enrolled into an external quality assessment program for clinical chemistry, HbA1c (glycated haemoglobin), lipid and human urine. This was implemented with support from the Randox International Quality Assurance Scheme (RIQAS), UK. The frequency of external quality control sample was two per month for clinical chemistry, lipid and urine, and one per month for HbA1c.
Results
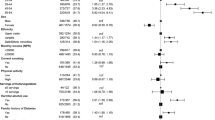
The first cross-sectional study was conducted between September 2010 and November 2011. A total of 14, 215 individuals in 8, 115 households were approached in the three study sites (5348 participants in Chennai, 4609 in Delhi, and 4258 in Karachi). From these, a total of 13,384 participants were recruited (4943 Chennai, 4425 Delhi, and 4016 Karachi). A total of 831 eligible participants in the three sites refused to participate in the study; overall response rate thus was 94.1% at the participant level (Chennai 92.4%, Delhi 95.7%, Karachi 94.3%). About eighty-one percent of the participants recruited into the study contributed biospecimens (Chennai 83.9%, Delhi 79.8% and Karachi 87.2%). Overall, 51.8% of the participants were females; a large proportion of the sample, 61.6% was below the age of 45 years, 27.5% in the 45–60 years age group and 10.9% > 60 years of age. In addition, the study provides an understanding of the existing political and social challenges in establishing a sustainable surveillance system for CMDs in the two countries and evidences of context specific successful measures that can be adopted to overcome most of these challenges (summarised in table 5).
Discussion
The CARRS-Surveillance model has been established in Chennai and New Delhi in India, and Karachi in Pakistan with successful completion of the first cross-sectional survey and initiation of the first year of cohort follow-up. The response rate for the first cross-sectional survey was more than 90% in all study sites with an overall rate of 94%. The combined cross-sectional and longitudinal study design lends it the advantages of:
-
(i)
serial cross-sectional survey based models such as the NHANES [43] and the Behaviour Risk Factor Surveillance Surveys (BRFSS) in the USA [44] and Jordan [45], and the national NCD risk factor examination surveys in Seychelles [46] and Cuba [47];
-
(ii)
longitudinal prospective models such as the SCORE (Systematic COronary Risk Evaluation) project which helped to develop a risk scoring system for management of CVD in Europe [48] and other longitudinal studies which helped to estimate the psychosocial risk factors of CHD [49].
CMDs are among the top ten most costly diseases [50], but have the advantage of being largely predictable through identification of distal and intermediate risk factors, and also substantially preventable through changes in lifestyle and/or use of preventive pharmacology [1, 51, 52]. The surveillance model if scaled up has the potential to estimate secular trends and incidence rates of mortality and morbidity due to CMDs, their complications and risk factors, thereby providing means of prioritizing and measuring the impact of public health interventions.
In a recent review of prevailing methods of NCD surveillance, particularly of CVD in India, the authors reiterate the need for harmonising all existing efforts, at least in measurement tools and quality assurance methods, to establish an integrated, comprehensive, and standardised surveillance system [53]. CARRS-Surveillance provides an understanding of the challenges in establishing such a surveillance system for CMDs, and elucidates the means to address them. However, we suggest that such an effort should not be limited to individual countries, but should be consolidated for South-Asia as a whole because the entire region is experiencing an epidemiological transition leading to increased incidence of CMDs and their risk factors. Also, there are shared demographic, socio-economic, behavioural, and physiological determinants among South-Asians. One such multi-site collaborating surveillance network is INDEPTH which regularly collates cross-sectional survey data from 34 sites in 17 LMICs [41]. However, these are based on the self-selected samples of Health and Demographic Surveillance Systems (HDSS) in each site and are only representative of a district, therefore, the findings cannot be generalised to the region or the country [41].
Strengths and limitations
Apart from robust study methods and quality control mechanisms, the sample population recruited in our study conforms to the current age profile of the population in the two countries; about 65% of the population in India and 75% of population in Pakistan are below the age of 35 years [36, 54]. This demonstrates the success of the sampling strategy employed and has implications for the generalisability of findings. However, a limitation of the CARRS model is that the study setting is urban and does not include the larger rural population where the burden of CMD is also growing. An urban model, however, would anticipate the growth of urban areas the world over, and also provide insights into operational aspects of surveillance systems, and empirical evidence of successful implementation at lower costs. The New York City Health and Nutrition Examination Survey (NYC HANES) provides an aspirational model suggesting that surveillance in such metropolitan cities with diverse populations might provide a reasonable reflection of diverse and growing cities to each individual nation’s disease burdens [55].
Several LMICs have some structure to estimate the burden of NCDs, but a recent study by the WHO in 23 high burden countries (which includes India) showed that the existing systems are deficient in standardised data collection tools and often lack accuracy and quality [56]. The CARRS-Surveillance model addresses these technical standardisation and quality challenges in setting up national and regional CMD surveillance systems in South-Asia, but the task of scaling up will require political commitment, funds, and human resources. Although challenging, this is achievable and has been accomplished by a few LMICs. For example, the Ministry of Health in Jordan, in partnership with WHO and CDC, established the Jordan BRFSS in 2002 which conducts cross-sectional surveys every two to three years [45]. The national examination survey of NCD risk factors in Seychelles has been collecting data for planning and evaluating interventions since 1989 [46], and the Cuban system since 1995–96 [47]. Eleven Latin American countries (Argentina, Brazil, Chile, Colombia, Dominican Republic, Guatemala, Mexico, Panama, Peru, Uruguay and Venezuela) have new or emerging systems for serial national NCD and risk factor surveys in various stages of development [57]. These countries have demonstrated the utility of continuous surveillance in identifying high risk communities, planning interventions, and evaluating the effects of existing policies, thereby creating an evidence-base for steering national policies on NCD prevention and health promotion [45–47, 57].
COE-CARRS Surveillance Investigators’ Group
Steering Committee: Dorairaj Prabhakaran, K. M. Venkat Narayan, K Srinath Reddy, Nikhil Tandon, V. Mohan, Muhammed M. Kadir, Mohammed K. Ali, Vamadevan S Ajay
Operations: Dorairaj Prabhakaran, Nikhil Tandon, K. M. Venkat Narayan, Mohammed K Ali, Muhammed M. Kadir, S. Roopa, Hassan M. Khan, R. Pradeepa, M. Deepa, Vamadevan S Ajay, Dimple Kondal, Ruby Gupta, Pragya Sharma
Coordinating Centre (Delhi): Dorairaj Prabhakaran, Nikhil Tandon, S. Roopa, Vamadevan S Ajay, Manisha Nair, Nivedita Devasenapathy, Divya Pillai
Development of questionnaires and manual of operations: Dorairaj Prabhakaran, Nikhil Tandon, K. M. Venkat Nararayan, Mohammed K. Ali, Manisha Nair, Nivedita Devasenapathy, R. Pradeepa , Ed Gregg, Anwar Merchant, Romaina Iqbal
Data management and statistical team: Dimple Kondal, Shivam Pandey, Praggya, Naveen
Laboratory: Lakshmy Ramakrishnan, Ruby Gupta, Savita
Information Technology: Ramanathan K, Ansel J D’Cruz, Gnanashekaran K.
Online data entry software: Mahesh Dorairaj
Data collection team
Chennai:
Field supervisor: Rahul T
Field interviewers: Alagarsamy, Anthony JV, Arul Dass.A, Arul Pitchai.S, Ashok Kumar, Balaji V, Dhanasekar L, KalaiVani D, Kumar M, Nandhakumar, Prathiban K, Sampath, Saravana Kumar P, SaravananR, Senthil RajaR, ShenbagaValliE, SivamanikandanK, SureshT, Uma Sankari G
Laboratory assistants: Geetha Priya L, Gowri, Irin Jayakumari A, Padmapriya, Ramakrishnan R, Revathy, Satish Raj S, Sudha M, Suresh, Vijay Baskar S
Data entry operators: Narayanan, Nirmala
Delhi:
Field supervisor: Liladhar Dorlikar
Field interviewers: Parag Jyoti Das, Kulwant Kaur, Sweta Kumari, Meena Thakur, Garima Rautela, Avijeet Malik, Anita Yadav, Makhan, Rishi Garg, Arun
Laboratory assistants: Priyanka Nautiyal, Sunil Dogra, Geetha
Data entry operators: Naveen Kaushik, Avnish
Karachi:
Field supervisor: Mehboob John Samuel
Field interviewers & laboratory assistants: Yousuf Sadiq, Shukrat Khan, Shahirah Ziarat Khan, Nadia Khan, Noureen Khan, Naseem Sehar, Asif Shabaz, Fakhrah Perveen, Karan Inayat, Tajir Hussain, Tariq Hussain, Nasreen Khan
Data entry operator: Sayed Arif Hussain Kazmi
Ethics approval
CARRS-surveillance study has been approved by the Institutional Review Boards (IRBs) of Public Health Foundation of India, New Delhi, All India Institute of Medical Sciences, New Delhi, Madras Diabetes Research Foundation, Chennai, India, Aga Khan University, Karachi, Pakistan, and Emory University, Atlanta, USA. In addition the study has received regulatory approval from the National Heart, Lung, and Blood Institute (NHLBI), National Institutes of Health (NIH), USA and the Health Ministry Screening Committee of India, New Delhi.
Abbreviations
- AAMI:
-
American Association for Advancement of Medical Instrumentation
- BMI:
-
Body Mass Index
- BP:
-
Blood pressure
- BRFSS:
-
Behaviour Risk Factor Surveillance Surveys
- CARRS:
-
Centre for Cardiometabolic Risk Reduction in South-Asia
- CDC:
-
Centres for Disease Control and Prevention
- CEB:
-
Census enumeration blocks
- CHD:
-
Coronary heart disease
- CKD:
-
Chronic kidney disease
- CMDs:
-
Cardio-metabolic diseases
- CVD:
-
Cardiovascular diseases
- DM:
-
Diabetes mellitus
- HbA1c:
-
Glycated haemoglobin
- HDSS:
-
Health and Demographic Surveillance Systems
- HINTS:
-
Health Information National Trends Study
- ICD-10:
-
International Classification of Diseases 10 codes
- IDSP:
-
Integrated Disease Surveillance Project
- LMICs:
-
Low-and-middle-income countries
- MONICA:
-
Multinational MONItoring of trends and determinants in CArdiovascular disease
- MySQL:
-
My structured query language
- NCDs:
-
Non-communicable diseases
- NHANES-III:
-
National Health and Nutrition Examination Survey - third
- NYC HANES:
-
New York City Health and Nutrition Examination Survey
- PHP:
-
Hypertext preprocessor, scripting language for the web page/front end
- PSUs:
-
Primary sampling units
- QC:
-
Quality control
- QoL:
-
Quality of Life
- RIQAS:
-
Randox International Quality Assurance Scheme
- SCORE:
-
Systematic COronary Risk Evaluation
- SOPs:
-
Standard operating procedures
- UK:
-
United Kingdom
- USA:
-
United States of America
- WHO:
-
World Health Organisation
- WHO STEP:
-
World Health Organisation STEPwise approach to surveillance.
References
Kraushaar L, Kramer A: Are we losing the battle against cardiometabolic disease? The case for a paradigm shift in primary prevention. BMC Publ Health. 2009, 9 (1): 64-10.1186/1471-2458-9-64.
Economic Intelligence Unit: The silent epidemic: An economic study of diabetes in developed and developing countries. 2007, New York, London: Hong Kong: The Economist
Diabetes Atlas. http://www.eatlas.idf.org/media, 3,
Gupta R, Joshi P, Mohan V, Reddy K, Yusuf S: Epidemiology and causation of coronary heart disease and stroke in India. Heart. 2008, 94 (1): 16-26. 10.1136/hrt.2007.132951.
World Health Organisation: Global status report on non-communicable diseases. 2011, Geneva: World Health Organisation
Mathers C, Lopez A, Murray C: The Burden of Disease and Mortality by Condition: Data, Methods, and Results for 2001. Global Burden of Disease and Risk Factors. Edited by: Lopez A, Mathers C, Ezzati M, Jamison D, Murray C. 2006, Oxford University Press, New York
The human, social & economic impact of diabetes. http://www.idf.org/home/index.cfm?node=41,
Roglic G, Unwin N: Mortality attributable to diabetes: Estimates for the year 2010. Diabetes Res Clin Pract. 2010, 87 (1): 15-19. 10.1016/j.diabres.2009.10.006.
Danaei G, Lawes CMM, Van der Hoorn S, Murray CJL, Ezzati M: Global and regional mortality from ischaemic heart disease and stroke attributable to higher-than-optimum blood glucose concentration: comparative risk assessment. Lancet. 2006, 368 (9548): 1651-1659. 10.1016/S0140-6736(06)69700-6.
Ramachandran A, Wan Ma RC, Snehalatha C: Diabetes in Asia. Lancet. 375 (9712): 408-418.
Chan JCN, Malik V, Jia W, Kadowaki T, Yajnik CS, Yoon K-H, Hu FB: Diabetes in Asia. JAMA. 2009, 301 (20): 2129-2140. 10.1001/jama.2009.726.
Anjana RM, Pradeepa R, Deepa M, Datta M, Sudha V, Unnikrishnan R, Bhansali A, Joshi SR, Joshi PP, Yajnik CS, et al: Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: Phase I results of the Indian Council of Medical Research-INdia DIABetes (ICMR-INDIAB) study. Diabetologia. 2011, 54: 3022-3027. 10.1007/s00125-011-2291-5.
Ramachandran A, Snehalatha C, Latha E, Satyavani K, Vijay V: Clustering of cardiovascular risk factors in urban Asian Indians. Diabetes Care. 1998, 21 (6): 967-971. 10.2337/diacare.21.6.967.
Pradeepa R, Mohan V: The changing scenario of the diabetes epidemic: implications for India. Indian J Med Res. 2002, 116: 121-132.
Hughes L, Raval U, Raftery E: First myocardial infarctions in Asian and white men. BMJ. 1989, 298 (6684): 1345-1350. 10.1136/bmj.298.6684.1345.
McKeigue P, Ferrie J, Pierpoint T, Marmot M: Association of early-onset coronary heart disease in South Asian men with glucose intolerance and hyperinsulinemia. Circulation. 1993, 87 (1): 152-161. 10.1161/01.CIR.87.1.152.
Ghaffar A, Reddy K, Singhi M: Burden of non-communicable diseases in South Asia. BMJ. 2004, 328 (7443): 807-810. 10.1136/bmj.328.7443.807.
Chambers J, Elliott P, Zabaneh D, LYZ W, Froguel P, Balding D, Scott J, Kooner J: Common genetic variation near MC4R is associated with waist circumference and insulin resistance. Nat Genet. 2008, 40 (6): 716-718. 10.1038/ng.156.
Yajnik C: Early life origins of insulin resistance and type 2 diabetes in India and other Asian countries. J Nutr. 2004, 134 (1): 205-210.
Joshi P, Islam S, Pais P, Reddy S, Dorairaj P, Kazmi K, Pandey M, Haque S, Mendis S, Rangarajan S, et al: Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA. 2007, 297 (3): 286-294. 10.1001/jama.297.3.286.
Diaz V, Mainous A, Baker R, Carnemolla M, Majeed A: How does ethnicity affect the association between obesity and diabetes?. Diabet Med. 2007, 24 (11): 1199-1204. 10.1111/j.1464-5491.2007.02244.x.
McKeigue P, Marmot M, Court YS, Cottier D, Rahman S, Riemersma R: Diabetes, hyperinsulinaemia, and coronary risk factors in Bangladeshis in east London. Br Heart J. 1988, 60 (5): 390-396. 10.1136/hrt.60.5.390.
McKeigue P, Shah B, Marmot M: Relation of central obesity and insulin resistance with high diabetes prevalence and cardiovascular risk in South Asians. Lancet. 1991, 337 (8738): 382-386. 10.1016/0140-6736(91)91164-P.
World Health Organisation: UN high-level meeting on NCDs (New York, 19–20 September 2011). Summary report of the discussions at the round tables. 2011, New York: United Nations
Institute of Medicine: A nationwide framework for surveillance of cardiovascular and chronic lung diseases. 2011, Washington, DC: Institute of Medicine
Eiseman E, Fossum D: The Challenges of Creating a Global Health Resource Tracking System. 2005, Santa Monica, CA: RAND Corporation
Heathfield H, Pitty D, Hanka R: Evaluating information technology in health care: barriers and challenges. BMJ. 1998, 316 (7149): 1959-1961. 10.1136/bmj.316.7149.1959.
Gupta R: Recent Trends in Coronary Heart Disease Epidemiology in India. Indian Heart J. 2008, Suppl B: B4-B18.
Abegunde D, Mathers C, Adam T, Ortegon M, Strong K: The burden and costs of chronic diseases in low-income and middle-income countries. Lancet. 2007, 370 (9603): 1929-1938. 10.1016/S0140-6736(07)61696-1.
Engelgau MM, El-Saharty S, Kudesia P, Rajan V, Rosenhouse S, Okamoto K: Capitalizing on the Demographic Transition: Tackling Noncommunicable Diseases in South Asia. 2011, Washington, D.C: The World Bank, 204-
Integrated Disease Surveillance Project (IDSP). http://idsp.nic.in/,
Nishtar S, Bile KM, Ahmed A, Amjad S, Iqbal A: Integrated Population-Based Surveillance of Noncommunicable Diseases: The Pakistan Model. American Journal of Preventive Medicine. 2005, 29 (5, Supplement 1): 102-106. 10.1016/j.amepre.2005.07.034.
Morris A, Boyle D, MacAlpine R, Emslie-Smith A, Jung R, Newton R, MacDonald T: The diabetes audit and research in Tayside Scotland (darts) study: electronic record linkage to create a diabetes register. BMJ. 1997, 315 (7107): 524-528. 10.1136/bmj.315.7107.524.
Joshy G, Simmons D: Diabetes information systems: a rapidly emerging support for diabetes surveillance and care. Diabetes Technol Ther. 2006, 8 (5): 587-597. 10.1089/dia.2006.8.587.
STEPwise approach to surveillance (STEPS). http://www.who.int/chp/steps/manual/en/index.html,
Census of India. 2011, http://censusindia.gov.in/,
World Population Prospects: The. 2006, http://esa.un.org/unup, Revision and World Urbanization Prospects: The 2007 Revision,
StataCorp: Statistical Software: Release 10.1 College Station. 2008, College Station, TX: StataCorp LP
Rizzo L, Brick J, Park I: A minimally intrusive method for sampling persons in Random Digit Dial surveys. Public Opin Q. 2004, 68 (2): 267-274. 10.1093/poq/nfh014.
The WHO MONICA Project. http://www.ktl.fi/monica/index.html,
Ng N, Minh HV, Juvekar S, Razzaque A, Bich TH, Kanungsukkasem U, Ashraf A, Ahmed SM, Soonthornthada K: Using the INDEPTH HDSS to build capacity for chronic non-communicable disease risk factor surveillance in low and middle-income countries. Global Health Action. 2009, 2 (NCD Supplement): 7-18.
Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ: Recommendations for blood pressure measurement in humans and experimental animals: Part 1: blood pressure measurement in humans: a statement for professionals from the subcommittee of professional and public education of the American Heart Association Council on High Blood Pressure Research. Hypertension. 2005, 45: 142-161.
National Health and Nutrition Examination Survey. http://www.cdc.gov/nchs/nhanes.htm,
Thacker SB, Stroup DF, Rothenberg RB: Public health surveillance for chronic conditions: a scientific basis for decisions. Stat Med. 1995, 14 (5–7): 629-641.
Al-Nsour M, Zindah M, Belbeisi A, Hadaddin R, Brown DW, Walke H: Prevalence of selected chronic, noncommunicable disease risk factors in jordan: results of the 2007 jordan behavioral risk factor surveillance survey. Prev Chronic Dis. 2012, 9: E25-
Bovet P, Viswanathan B, Shamlaye C, Romain S, Gedeon J: Addressing non-communicable diseases in the Seychelles: towards a comprehensive plan of action. Glob Health Promot. 2010, 17 (2 suppl): 37-40. 10.1177/1757975910363930.
MS GR: New Survey Results Enhance Cuba’s NCD Surveillance: Mariano Bonet MD Director, National Hygiene, Epidemiology and Microbiology Institute. MEDICC Rev. 2011, 13: 11-13.
Conroy RM, Pyörälä K, Fitzgerald AP, Sans S, Menotti A, De Backer G, De Bacquer D, Ducimetière P, Jousilahti P, Keil U, et al: Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. 2003, 24 (11): 987-1003. 10.1016/S0195-668X(03)00114-3.
Hemingway H, Marmot M: Psychosocial factors in the aetiology and prognosis of coronary heart disease: systematic review of prospective cohort studies. BMJ. 1999, 318 (7196): 1460-1467. 10.1136/bmj.318.7196.1460.
Cohen JW, Krauss NA: Spending And Service Use Among People With The Fifteen Most Costly Medical Conditions, 1997. Health Aff. 2003, 22 (2): 129-138. 10.1377/hlthaff.22.2.129.
Malekzadeh F, Marshall T, Pourshams A, Gharravi M, Aslani A, Nateghi A, Rastegarpanah M, Khoshnia M, Semnani S, Salahi R: A pilot double-blind randomised placebo-controlled trial of the effects of fixed-dose combination therapy ("polypill") on cardiovascular risk factors. Int J Clin Pract. 2010, 64 (9): 1220-1227. 10.1111/j.1742-1241.2010.02412.x.
Mohan V: Effects of a polypill (Polycap) on risk factors in middle-aged individuals without cardiovascular disease (TIPS): a phase II, double-blind, randomised trial. Lancet. 2009, 373 (9672): 1341-1351.
Shah B, Mathur P: Surveillance of cardiovascular disease risk factors in India: The need & scope. Indian J Med Res. 2010, 132 (5): 634-642.
National Institute of Population Studies (NIPS) [Pakistan] aMII: Pakistan Demographic and Health Survey 2006–07. 2008, Islamabad, Pakistan: National Institute of Population Studies and Macro International Inc
Wilson PWF, Narayan KMV: New York City Health and Nutrition Examination Survey: A model for urban health surveillance. Diabetes Care. 2009, 32 (1): 204-205. 10.2337/dc08-1807.
Alwan A, MacLean DR, Riley LM, d’Espaignet ET, Mathers CD, Stevens GA, Bettcher D: Monitoring and surveillance of chronic non-communicable diseases: progress and capacity in high-burden countries. The Lancet. 2010, 376 (9755): 1861-1868. 10.1016/S0140-6736(10)61853-3.
Choi BCK, Corber SJ, McQueen DV, Bonita R, Zevallos JC, Douglas KA, Barceló A, Gonzalez M, Robles S, Stachenko S, et al: Enhancing regional capacity in chronic disease surveillance in the Americas. Rev Panam Salud Publica/Pan Am J Public Health. 2005, 17: 130-141.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2458/12/701/prepub
Acknowledgements
This study is coordinated by CoE-CARRS (Center of Excellence - Center for CArdio-metabolic Risk Reduction in South Asia ) based at Public Health Foundation of India (PHFI), New Delhi, India in collaboration with Centre for Chronic Disease Control (CCDC), New Delhi, Emory University, Atlanta, U.S.A, All India Institute of Medical Sciences (AIIMS), New Delhi, Madras Diabetes Research Foundation (MDRF), Chennai, India and Aga Khan University, Karachi, Pakistan. We hereby, acknowledge the contributions of the field and research staff of the “CARRS Surveillance Investigators’ Group” (a list of all members is included above).
This project is funded in whole or in part by the National Heart, Lung, and Blood Institute, National Institutes of Health (NIH), Department of Health and Human Services, under Contract No. HHSN268200900026C, and the United Health Group, Minneapolis, Mn, USA.
Several members of the research team at PHFI, Emory University, and CCDC were/are supported by the Fogarty International Clinical Research Scholars – Fellows programme (FICRS-F) through Grant Number 5R24TW007988 from NIH, Fogarty International Center (FIC) through Vanderbilt University, Emory’s Global Health Institute, and D43 NCDs in India Training Program through Award Number D43HD05249 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD) and FIC. However, the contents of this paper are solely the responsibility of the writing group and do not necessarily represent the official views of FIC, Vanderbilt University, Emory University, PHFI, NICHD, or the NIH.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that there are no competing interests financial or non-financial with regards to this study. The interpretation of data and presentation of information is not influenced by any personal or financial relationship with any individual or organization.
Authors’ contributions
All authors listed in the paper have contributed sufficiently to fulfil the criteria for authorship. Apart from this there is no other individual who has contributed sufficiently and who fulfil the criteria for authorship but has not been included as an author for this paper. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Nair, M., Ali, M.K., Ajay, V.S. et al. CARRS Surveillance study: design and methods to assess burdens from multiple perspectives. BMC Public Health 12, 701 (2012). https://doi.org/10.1186/1471-2458-12-701
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2458-12-701