Abstract
Background
Persistent arterial dysfunction in patients with a history of Kawasaki disease (KD) and an integral role of oxidative stress in the development of cardiovascular disease are increasingly recognized. We sought to test the hypothesis that oxidative stress is increased in KD patients and related to carotid atherosclerotic changes and stiffness.
Methods
We compared the serum levels of oxidative stress biomarkers, carotid intima-media thickness (IMT), and carotid stiffness index among KD patients with coronary aneurysms (n = 32), those without coronary complications (n = 19), and controls (n = 32).
Results
Compared with controls, patients with coronary aneurysms had significantly higher serum levels of malonaldehyde (2.62 ± 0.12 μM vs 2.22 ± 0.07 μM, p = 0.014) and hydroperoxides (26.50 ± 1.13 μM vs 22.50 ± 0.62 μM, p = 0.008). A linear trend of the magnitude of oxidative stress in relation to inflammatory damage was observed for malonaldehyde (p = 0.018) and hydroperoxides (p = 0.014) levels. Serum malonaldehyde and hydroperoxide levels correlated positively with carotid IMT (p < 0.001 and p = 0.034, respectively) and stiffness index (p = 0.001 and p = 0.021, respectively). Multiple linear regression analysis identified serum malonaldehyde level as a significant determinant of carotid IMT (β = 0.31, p = 0.006) and stiffness (β = 0.27, p = 0.008).
Conclusion
Our findings suggest oxidative stress is increased in KD patients with coronary aneurysms and is associated with carotid intima-media thickening and stiffening.
Similar content being viewed by others
Background
Since its first description in 1967 [1], Kawasaki disease (KD) has become the most common acquired heart disease in children in developed countries [2]. Patients diagnosed with KD in the sixties and early seventies have reached middle age. Previous studies have demonstrated persistent coronary arterial dysfunction in patients with persistent and regressed coronary aneurysm [3–5]. Importantly, endothelial dysfunction and stiffening of both the coronary [3–5] and systemic [6–9] arteries that characterize the arterial dysfunction are themselves risk factors for premature atherosclerosis and cardiovascular disease. Indeed, we [10] and others [7] have found a significant increase in carotid intima-media thickness (IMT), a marker of atherosclerosis [11], in KD patients with or without coronary complications late after the acute illness. While growing data suggest premature atherosclerosis in patients with a history of KD, the underlying mechanisms remain unclear.
Accumulating evidence suggests that oxidative stress plays an integral role in the development of atherosclerosis and cardiovascular disease. Reactive oxygen species are increasingly recognized to play an important role in compromising endothelial function, including modulation of vasomotor tone [12, 13]. Oxidized low-density lipoprotein is pro-inflammatory [14, 15], causes inhibition of endothelial nitric oxide synthase [16], promotes retention of macrophages in the arterial wall [17], and stimulates vascular smooth muscle cells proliferation [15]. Furthermore, F2-isoprostanes, a biomarker marker of lipid peroxidation [18], have been found to localize in foam cells in atherosclerotic lesions of humans [19] and a mouse model of atherosclerosis [20].
Given the persistent arterial dysfunction and risk of premature atherosclerosis in KD patients as well as the increasingly recognized integral role of oxidative stress in the development of cardiovascular disease, we hypothesized that oxidative stress was increased in KD patients and related to carotid atherosclerotic changes and stiffness. To test the hypothesis, we compared the levels of two markers of oxidative stress, malonaldehyde and hydroperoxides, in patients with a history of KD with those of healthy controls and determined the correlations between levels of these oxidative stress markers and carotid IMT and stiffness index.
Methods
Subjects
Patients with a history of KD were recruited from the paediatric cardiac clinic. Those diagnosed with KD within 12 months of study were excluded to minimize potential confounding influence relating to subacute inflammation. From the case records, the age at diagnosis, the interval from disease onset to the time of study, and the coronary artery status were noted. Coronary aneurysms were documented by serial two-dimensional echocardiography in all of the patients. None of the patients required cardiac catheterization. Diagnosis of KD was based on the classic clinical criteria [21], while diagnosis of coronary aneurysms was based on the Japanese Ministry of Health criteria [22]. Healthy age-matched subjects were recruited as controls were recruited as control subjects. These were healthy children previously discharged from our clinic with a diagnosis of a functional heart murmur and their healthy siblings. The body weight and height were measured, and body mass index was calculated accordingly. The blood pressure in the right arm was measured twice using an automated oscillometric device (Dinamap, Critikon, Inc), and the average of the 2 readings was taken. The institutional Ethics Committee approved the study and parents of all subjects gave written, informed consent.
Measurement of carotid IMT and stiffness
A 7–15 MHz linear-array transducer, interfaced to a Hewlett-Packard Sonos 5500 ultrasound machine, was used to image the right carotid artery at about 1 cm proximal to the carotid bifurcation. The IMT of the right common carotid artery far wall was measured offline using the QLAB analysis software (Philips, Bothell, USA). The QLAB IMT plug-in detects automatically the intima-media pixel pairs along the far wall of the carotid artery and provides a spatially averaged measurement of IMT over a preset of 10 mm region of interest. The average of three measurements was used for subsequent analysis.
The carotid artery stiffness was assessed by calculating the stiffness index as reported previously [23]. The end-diastolic (Dd) and systolic (Ds) diameters were measured. The carotid arterial stiffness index was then calculated as: ln (SBP/DBP)/[(Ds-Dd)/Dd], where SBP and DBP are systolic and diastolic blood pressure, respectively. The average of the right carotid arterial stiffness index derived from the values of three consecutive cardiac cycles was used for subsequent analyses.
Blood investigations
Venous blood was withdrawn for measurement of fasting lipid profiles, malonaldehyde and hydroperoxide levels in patients and controls. Serum total cholesterol level was determined enzymatically using a Hitachi 912 analyzer (Roche Diagnostics, GmbH, Mannheim, Germany). High-density lipoprotein (HDL) cholesterol was measured using a homogenous method with polyethylene glycol modified enzymes and sulphated α-cyclodextrin. Low-density lipoprotein (LDL) cholesterol was calculated by the Friedewald equation.
Under oxidative stress, lipid peroxidation serves as an important contributor to cell injury. The degree of lipid peroxidation in plasma was determined by measuring thiobarbituric acid reactive substances (TBARS) [24, 25]. In brief, an aliquot of serum (100 μL) was added to 10% phosphotungstic acid (500 μL) and incubated at room temperature for 10 minutes. The mixture was centrifuged at 2000 g for 10 minutes. After removal of supernatant, thiobarbituric acid (0.67%) was added to the pellet and incubated at 95°C for 1 hour. The amount of malonaldehyde formed in the reaction mixture was measured by spectrophotometer at absorbance of 532 nm. Malonaldehyde was used as the standard. The amount of malonaldehyde detected correlates to the level of lipid peroxides in the serum.
Serum hydroperoxide levels were measured by modified FOX assay [26, 27]. In brief, an aliquot of plasma (100 μL) was added to FOX2 reagent and incubated at room temperature for 30 minutes. The reaction mixture was then centrifuged at 12,000 g for 5 minutes. Absorbance (at 560 nm) of the supernatant was measured. Hydrogen peroxide was used as standard.
Data analysis
Data are presented as mean ± SEM. Differences in demographic data between patients and control subjects were compared using unpaired Student's t test. The malonaldehyde and hydroperoxides levels among patients with coronary aneurysms, patients without coronary complications, and control subjects were compared using simple analysis of variance, with posthoc comparisons by Tukey test. For the entire cohort, Pearson correlation analysis was used to assess for possible relationships between levels of oxidative stress markers and carotid IMT and stiffness index. Stepwise multiple linear regression was used to identify significant determinants of carotid IMT and stiffness. A p value of less than 0.05 was considered statistically significant. All statistical analyses were performed using SPSS version 10.0 (SPSS, Inc., Chicago, Illinois).
Results
A total of 83 Chinese patients living in Hong Kong were studied, comprising 51 patients with KD and 32 controls subjects. Those patients were studied at 10.5 ± 0.68 years after initial diagnosis of KD. Of the 51 patients, 32 had coronary aneurysms, which were persistent in 26 and had regressed in 6. All of the patients were asymptomatic, none required coronary arterial interventions, and 26 patients whom had persistent coronary aneurysms were maintained on long-term aspirin therapy. None of the patients were smokers and none had family history of premature cardiovascular disease. Table 1 shows the demographic and clinical data of the patients and controls. There were no significant differences in age, sex distribution, body mass index, blood pressure and cholesterol levels between patients and controls.
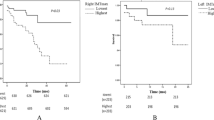
Compared with controls, patients with coronary aneurysms had significantly greater carotid IMT than those without aneurysm (p = 0.024) and controls (p = 0.006) (Figure 1a). Likewise, the stiffness index was greater in patients with than those without coronary aneurysm (p = 0.088) and controls (p < 0.001) (Figure 1b).
The serum levels of malonaldehyde and hydroperoxides, biomarkers of oxidative stress, in patients with or without coronary aneurysm and controls are shown in Figure 2. Compared with controls, patients with coronary aneurysms had significantly higher levels of malonaldehyde (2.62 ± 0.12 μM vs 2.22 ± 0.07 μM, p = 0.014) and hydroperoxides (26.50 ± 1.13 μM vs 22.50 ± 0.62 μM, p = 0.008). By contrast, the levels of malonaldehyde (2.58 ± 0.15 μM vs 2.77 ± 0.17 μM, p = 0.22) and hydroperoxides (27.2 ± 1.2 μM vs 23.3 ± 3.2 μM) were similar between patients with persistent aneurysm and those with regressed ones.
The possibility of a linear trend of the magnitude of oxidative stress was further determined using linear regression analysis of in the three cohorts: patients with coronary aneurysms, patients without coronary aneurysms, and controls. A significant trend was observed for malonaldehyde (P = 0.018) and hydroperoxides (p = 0.014) levels.
Correlations between levels of oxidative stress markers and carotid IMT and stiffness index are shown in Figures 3 and 4. The malonaldehyde level correlated positively with both the carotid IMT (p < 0.001) and stiffness index (p = 0.001). Similarly, the hydroperoxide level correlated positively with the carotid IMT (p = 0.034) and stiffness index (p = 0.021).
Multiple linear regression analysis of the entire cohort was used to identify significant determinants of carotid IMT and stiffness index. The independent variables included age, sex, body mass index, subject grouping (patients with coronary aneurysms as the referent group with 2 dummies for patients without coronary complications and controls), systolic and diastolic blood pressures, total cholesterol, LDL and HDL cholesterols, and malonaldehyde and hydroperoxides level. Significant determinants of carotid IMT were subject grouping (β = -0.24, p = 0.025) and malonaldehyde level (β = 0.31, p = 0.006) (model R2 = 0.20), while significant determinants of carotid stiffness were subject grouping (β = -0.35, p = 0.001), body mass index (β = 0.26, p = 0.01), and malonaldehyde level (β = 0.27, p = 0.008) (model R2 = 0.29).
Discussion
The novel findings of the present study are (1) a significant increase in the plasma levels of oxidative stress markers late after the acute illness in patients with a history of KD and coronary aneurysms and (2) positive correlations between markers of oxidative stress and carotid IMT and stiffness. As one of the most sensitive targets for attacks of oxidative stress are unsaturated fatty acids of cellular lipid membranes, we measured the levels of hydroperoxides and malonaldehyde, the latter being one of the widely used indices of oxidative stress.
Previous studies have provided clues for possible existence of increased oxidative stress in patients after KD. Deng and colleagues have demonstrated the restoration of systemic arterial endothelial dysfunction in patients with and without coronary aneurysms at 1 to 10 years after initial diagnosis of KD by acute intravenous administration of vitamin C [28]. They hypothesized that the antioxidant action of vitamin C might be responsible for the beneficial effect [29]. Furthermore, endothelin-1, which could induce superoxide production [30], has been shown to be increased in KD in the plasma in the acute and recovery stage [31]. To the best of our knowledge, the present study is the first to provide direct evidence of increased oxidative stress in KD patients with coronary aneurysms, which shed light on the possible underlying mechanisms of the previously reported, but hitherto unexplained, arterial dysfunction and intima-media thickening in these patients.
Arterial dysfunction is increasingly recognized as a long-term sequel of KD, even in patients without coronary aneurysms [3–8]. Impaired coronary vasodilatory response to intracoronary injection of acetylcholine [4, 5] and nitroglycerine [3, 5] has been demonstrated at sites of persistent and regressed aneurysms. Concerns have also been raised with regard to the possibility of impaired acetylcholine-induced vasodilation at sites with apparently normal coronary arteries [32]. On the other hand, impaired brachial flow-mediated dilation [6] and increased conduit arterial stiffness [8] have been shown in KD patients with and without coronary complications. Importantly, endothelial dysfunction and arterial stiffening that characterize the arterial abnormalities in KD patients are risk factors for cardiovascular disease and atherosclerosis. Over the past two decades, accumulating evidence suggests that endothelial dysfunction may be caused by accelerated inactivation of nitric oxide by reactive oxygen species, which reduces bioavailability of nitric oxide [33]. In adult patients with coronary artery disease [34], non-insulin-dependent diabetes mellitus [35], and hypertension [36], administration of vitamin C has similarly been shown to improve endothelial dysfunction. While vascular damage with consequent structural alteration might in part account for arterial stiffening in patients with a history of KD [8], the alteration of vasomotor tone secondary to endothelial dysfunction might also be a culprit [6]. The association between oxidative stress and arterial elasticity has recently also been demonstrated by Kals and coworkers in adult patients with peripheral arterial disease [37]. In their patients, inverse associations exist between large and small artery elasticity and urinary 8-iso-prostaglandins F2α generated as a result of free radical-mediated peroxidation of arachidonic acid [38]. Proposed mechanisms include modulation of matrix metalloproteinases associated with destruction of arterial elastic laminae [39], enhancement of smooth muscle tone [40], and promotion of smooth muscle cell proliferation [41] by reactive oxygen species. In adults with renovascular hypertension, an inverse relationship between urinary excretion of 8-hydroxy-2'-deoxygnanosine and acetylcholine-induced forearm blood flow has been reported [42]. A recent study has further provided evidence that local oxidative stress as assessed by net production of isoprostane across the left anterior descending artery territory has a role in the reduction of nitric oxide bioavailability in humans with coronary endothelial dysfunction [43]. Hence, it is tempting to speculate that oxidative stress in KD patients with coronary aneurysms as shown in the present study might in part account for the observed long-term systemic arterial dysfunction, albeit the latter is being documented also in patients without coronary complications [6, 8, 28].
The next logical question to address is the source of oxidative stress in KD patients. We [44] and others [45] have shown that high-sensitivity C-reactive protein is elevated in KD patients with coronary aneurysms late after the acute illness and implicate the persistence of chronic low-grade inflammation in these patients. C-reactive protein has been reported to induce superoxide production in human aortic endothelial cells as well as in smooth muscle cells [46], possibly through activation of vascular nicotinamide adenine dinucleotide/nicotinamide adenine dinucleotide phosphate oxidase system [47]. The association of inflammation and increased oxidative stress amplifies the cascade that results in vascular damage [48]. Depletion of L-arginine in inflammatory sites has further been shown to trigger inducible nitric oxide synthase (iNOS) in macrophages to generate functionally important amounts of superoxide anion [49]. Indeed, we have previously demonstrated that the serum of patients with a history of KD induces expression iNOS in THP-1 macrophages in vitro [50]. Although the role of iNOS in atherosclerosis remains to be defined, genetic deficiency in iNOS has been reported to result reduce atherosclerosis in apolipoprotein E-deficient mice [51] and that chronic treatment of iNOS inhibitors has been shown to limit progression of preexisting atherosclerosis in hypercholesterolaemic rabbits [52]. Undoubtedly, these speculations of potential sources of oxidative stress in KD patients require further studies for clarification.
Our findings of increased oxidative stress in KD patients and its relation with arterial stiffening and intima-media thickening have important therapeutic implications. Notwithstanding the reported acute improvement of endothelial function with intravenous vitamin C administration in KD patients [28], the usefulness of antioxidant vitamins to prevent cardiovascular disease in adults with and without hypercholesterolaemia, end-stage renal disease, atherosclerosis has been controversial [53, 54]. Further studies are necessary to elucidate the optimum dose and type of antioxidants and the impact of long-term antioxidant supplementation on the arterial IMT and stiffness in KD patients.
A limitation to this study is the potential confounding influence of aspirin prescribed to KD patients with coronary aneurysms on the levels of oxidative stress markers. Nonetheless, in a rat model, aspirin has been shown to attenuate the elevation in aortic superoxide anion levels induced by angiotensin II [55]. Thus, in patients with persistent coronary aneurysms, if aspirin were to have any influence on the levels of oxidative markers, the chance of detecting a significant difference among groups would be minimized rather than exaggerated.
Conclusion
Increased oxidative stress occurs in patients with a history of KD late after the acute illness and is associated with arterial stiffening and intima-medial thickening. Further research to determine the potential benefits of antioxidants in these patients at risk of premature atherosclerosis and cardiovascular disease is warranted.
References
Kawasaki T: Acute febrile mucocutaneous syndrome with lymphoid involvement with specific desquamation of the fingers and toes in children. Clinical observation of 50 patients. Jpn J Allergy. 1967, 16: 178-222.
Tauber KA, Rowley AH, Shulman ST: Seven-year national survey of Kawasaki disease and acute rheumatic fever. Pediatr Infect Dis J. 1994, 13: 704-708.
Sugimura T, Kato H, Inoue O, Takagi J, Fukuda T, Sato N: Vasodilatory response of the coronary arteries after Kawasaki disease: evaluation by intracoronary injection of isosorbide dinitrate. J Ped. 1992, 121: 684-688. 10.1016/S0022-3476(05)81893-1.
Yamakawa R, Ishii M, Sugimura T, Akagi T, Eto G, Iemura M, Tsutsumi T, Kato H: Coronary endothelial dysfunction after Kawasaki disease: Evaluation by intracoronary injection of Acetylcholine. J Am Coll Cardiol. 1998, 31: 1074-1080. 10.1016/S0735-1097(98)00033-3.
Iemura M, Ishii M, Sugimura T, Akagi T, Kato H: Long term consequences of regressed coronary aneurysms after Kawasaki disease with vascular wall morphology and function. Heart. 2000, 83: 307-311. 10.1136/heart.83.3.307.
Dhillon R, Clarkson P, Donald AE, Powe AJ, Nash M, Novelli V, Dillon MJ, Deanfield JE: Endothelial dysfunction late after Kawasaki disease. Circulation. 1996, 94: 2103-2106.
Noto N, Okada T, Yamasuge M, Taniquchi K, Karasawa K, Ayusawa M, Sumitomo N, Harada K: Noninvasive assessment of the early progression of atherosclerosis in adolescents in Kawasaki disease and coronary artery lesions. Pediatrics. 2001, 107: 1095-1099. 10.1542/peds.107.5.1095.
Cheung YF, Yung TC, Tam SCF, Ho MHK, Chau AKT: Novel and traditional cardiovascular risk factors in children after Kawasaki disease: Implications for premature atherosclerosis. J Am Coll Cardiol. 2004, 43: 120-124. 10.1016/j.jacc.2003.08.030.
Senzaki H, Chen CH, Ishido H, Masutani S, Matsunaga T, Taketazu M, Yokote Y, Kobayashi T, Sasaki N, Kyo S: Arterial hemodynamics in patients after Kawasaki disease. Circulation. 2005, 111: 2119-2125. 10.1161/01.CIR.0000162483.51132.25.
Cheung YF, Wong SJ, Ho MH: Relationship between carotid intima-media thickness and arterial stiffness in children after Kawasaki disease. Arch Dis Childhood. 2007, 92: 43-47. 10.1136/adc.2006.096628.
Slyper AH: What vascular ultrasound testing has revealed about pediatric atherogenesis, and a potential clinical role for ultrasound in pediatric risk assessment. J Clin Endocrinol Metab. 2004, 89: 3089-3095. 10.1210/jc.2003-030644.
Rueckschloss U, Duerrschmidt N, Morawietz H: NADPH oxidase in endothelial cells: impact on atherosclerosis. Antioxid Redox Signal. 2003, 5: 171-180. 10.1089/152308603764816532.
Rueckschloss U, Quinn MT, Holtz J, Morawietz H: Dose-dependent regulation of NAD(P)H oxidase expression by angiotensin II in human endothelial cells: protective effect of angiotensin II type 1 receptor blockade in patients with coronary artery disease. Arterioscler Thromb Vasc Biol. 2002, 22: 1845-1851. 10.1161/01.ATV.0000035392.38687.65.
Madamanchik N, Vendrov A, Runge M: Oxidative stress and vascular disease. Arterioscler Thomb Biol. 2005, 25: 29-38.
Stocker R, Keaney JF: Role of oxidized modifications in atherosclerosis. Physiol Rev. 2001, 84: 1381-1478. 10.1152/physrev.00047.2003.
Liao J, Shin W, Lee W, Clark S: Oxidized low-density lipoprotein decreases the expression of endothelial nitric oxide synthase. J Biol Chem. 1995, 270: 319-324. 10.1074/jbc.270.1.319.
Jialal I: Evolving lipoprotein risk factors: lipoprotein (a) and oxidized low-density lipoprotein. Clin Chem. 1998, 44: 1827-1832.
Cracowski JL, Durand T, Bessard G: Isoprostanes as a biomarker of lipid peroxidation in humans: physiology, pharmacology and clinical implications. Trends Pharmacol Sci. 2002, 23: 360-366. 10.1016/S0165-6147(02)02053-9.
Practico D, Iuliano L, Mauriello A, Spagnoli L, Lawson JA, Rokach J, Maclouf J, Violi F, Fitzgerald GA: Localization of distinct F2-isoprostances in human atherosclerotic lesions. J Clin Invest. 1997, 100: 2028-2034. 10.1172/JCI119735.
Pratico D, Tangirala RK, Rader DJ, Rokach J, FitzGerald GA: Vitamin E suppresses iso-prostane generation in vivo and reduces atherosclerosis in ApoE-deficient mice. Nat Med. 1998, 4: 1189-1192. 10.1038/2685.
Newburger JW, Takahashi M, Gerber MA, Gewitz MH, Tani LY, Burns JC, Shulman ST, Bolger AF, Ferrieri P, Baltimore RS, Wilson WR, Baddour LM, Levison ME, Pallasch TJ, Falace DA, Taubert KA, Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association: Diagnosis, treatment, and long-term management of Kawasaki disease : a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Pediatrics. 2004, 115: 1708-1733. 10.1542/peds.2004-2182.
Research Committee on Kawasaki Disease: Report of Subcommittee on Standardization of Diagnostic Criteria and Reporting of Coronary Artery Lesions in Kawasaki Disease. 1984, Tokyo, Japan: Ministry of Health and Welfare
Hirai T, Sasayama S, Kawasaki T, Yagi S: Stiffness of systemic arteries in patients with myocardial infarction: a noninvasive method to predict severity of coronary atherosclerosis. Circulation. 1989, 80: 78-86.
Yagi K: A simple fluorometric assay for lipoperoxide on blood plasma. Biochem Med. 1976, 15: 212-216. 10.1016/0006-2944(76)90049-1.
Sung FL, Zhu TY, Au Yeung KK, Siow YL, O K: Enhanced MCP-1 expression during ischemia reperfusion injury is mediated by oxidative stress and NF-kappa B. Kidney Int. 2002, 62: 1160-1170. 10.1111/j.1523-1755.2002.kid577.x.
Nourooz-Zadeh J, Tajaddini-Sarmadi J, Wolff SP: Measurement of plasma hydroperoxide concentrations by the ferrous oxidation-xylenol orange assay in conjunction with triphenylophosphine. Anal Biochem. 1994, 220: 403-409. 10.1006/abio.1994.1357.
Hermes-Lima M, Willmore WG, Storey KB: Quantification of lipid peroxidation in tissue extracts based on Fe(III) xylenol orange complex formation. Free Radic Biol Med. 1995, 19: 271-280. 10.1016/0891-5849(95)00020-X.
Deng Y, Li T, Xiang H, Chang Q, Li C: Impaired endothelial function in the brachial artery after Kawasaki disease and the effects of intravenous administration of vitamin C. Pediatr Infect Dis J. 2003, 22: 34-39. 10.1097/00006454-200301000-00011.
Frei B, England L, Ames MN: Ascorbate is an outstanding antioxidant in human blood plasma. Proc Natl Acad Sci USA. 1989, 86: 6377-6381. 10.1073/pnas.86.16.6377.
Wedgwood S, Dettman RW, Black SM: ET-1 stimulates pulmonary arterial smooth muscle cell proliferation via induction of reactive oxygen species. Am J Physiol Lung Cell Mol Physiol. 2001, 281: 1058-1067.
Ogawa S, Zhang J, Yuge K, Watanabe M, Fukazawa R, Kamisago M, Seki T, Hirayama T: Increased plasma endothelin-1 concentration in Kawasaki disease. J Cardiovasc Pharmacol. 1993, 22: S364-366.
Mitani Y: Coronary endothelial dysfunction after Kawasaki disease. J Am Coll Cardiol. 2000, 35: 821-822. 10.1016/S0735-1097(99)00622-1.
Cai H, DG Harrison: Endothelial dysfunction in cardiovascular disease. The role of oxidant stress. Circ Res. 2000, 87: 840-844.
Levine GN, Frei B, Koulouris SN, Gerhard MD, Keaney JF, Vita JA: Ascorbic acid reverses endothelial vasomotor dysfunction in patients with coronary artery disease. Circulation. 1996, 93: 1107-1113.
Ting HH, Timmimi FK, Boles KS, Creager SJ, Ganz P, Creager MA: Vitamin C improves endothelium-dependent vasodilation in patients with non-insulin-dependent diabetes mellitus. J Clin Invest. 1996, 97: 22-28. 10.1172/JCI118394.
Solzbach U, Hornig B, Jeserich M, Just H: Vitamin C improves endothelial dysfunction of epicardial coronary arteries in hypertensive patients. Circulation. 1997, 96: 1513-1519.
Kals J, Kampus P, Kals M, Zilmer K, Kullisaar T, Teesalu R, Pulges A, Zilmer M: Impact of oxidative stress on arterial elasticity in patients with atherosclerosis. Am J Hypertens. 2006, 19: 902-908. 10.1016/j.amjhyper.2006.02.003.
Morrow JD: Quantification of isoprostanes as indices of oxidant stress and the risk of atherosclerosis in humans. Arterioscler Thromb Vasc Biol. 2005, 25: 279-286. 10.1161/01.ATV.0000152605.64964.c0.
Rajagopalan S, Meng XP, Ramasamy S, Harrison DG, Galis ZS: Reactive oxygen species produced by macrophage-derived foam cells regulate the activity of vascular matrix metalloproteinases in vitro. Implications for atherosclerotic plaque stability. J Clin Invest. 1996, 98: 2572-2579. 10.1172/JCI119076.
Peng X, Haldar S, Deshpande S, Irani K, Kass DA: Wall stiffness suppresses Ake/e NOS and cytoprotection in pulse-perfused endothelium. Hypertension. 2003, 41: 378-381. 10.1161/01.HYP.0000049624.99844.3D.
Stocker R, Keaney JF: Role of oxidative modifications in atherosclerosis. Physiol Rev. 2004, 84: 1381-1478. 10.1152/physrev.00047.2003.
Higashi Y, Sasaki S, Nakagawa K, Matsuura H, Oshima T, Chayama K: Endothelial function and oxidative stress in renovascular hypertension. N Eng J Med. 2002, 25: 1954-1962. 10.1056/NEJMoa013591.
Lavi S, Yang EH, Prasad A, Mathemw V, Barness GW, Rihal CS, Lerman LO, Lerman A: The interaction between coronary endothelial dysfunction, local oxidative stress, and endogenous nitric oxide in humans. Hypertension. 2008, 51: 127-133. 10.1161/HYPERTENSIONAHA.107.099986.
Cheung YF, Ho MH, Tam SC, Yung TC: Increased high sensitivity C-reactive protein concentration and incrased areterial stifnfness in children with a history of Kawasaki disease. Heart. 2004, 90: 1281-1285. 10.1136/hrt.2003.018507.
Mitani Y, Sawada H, Hayakawa H, Aoki A, Ohashi H, Matsumura M, Kuroe K, Shimpo H, Nakano M, Komada Y: Elevated levels of high-sensitivity C-reactive protein and serum amyloid-A late after Kawasaki disease: association between inflammation and late coronary sequelae in Kawasaki disease. Circulation. 2005, 111: 38-43. 10.1161/01.CIR.0000151311.38708.29.
Venugopal SK, Devaraj S, Jialal I: C-reactive protein decreases prostacyclin release from human aortic endothelial cells. Circulation. 2003, 108: 1676-1678. 10.1161/01.CIR.0000094736.10595.A1.
Singh U, Jialal I: Oxidative stress and atherosclerosis. Pathophysiology. 2006, 13: 129-142. 10.1016/j.pathophys.2006.05.002.
Minuz P, Fava C, Cominacini L: Oxidative stress, antioxidantsm, and vascular damage. Br J Clin Pharmacol. 2006, 61: 774-777. 10.1111/j.1365-2125.2006.02681.x.
Yong X, Zweier JL: Superoxide and peroxynitrite generation from inducible nitric oxide synthase in macrophages. Proc Natl Acad Sci USA. 1997, 94: 6954-6958. 10.1073/pnas.94.13.6954.
Cheung YF, Karmin O, Tam SC, Siow YL: Induction of MCP1, CCR2 and iNOS expression in THP-1 macrophages by serum of children late after Kawasaki disease. Pediatr Res. 2005, 58: 1306-1310. 10.1203/01.pdr.0000183360.79872.1c.
Kuhlencordt PJ, Chen J, Huang PL: Genetic deficiency of inducible nitric oxide synthase reduces atherosclerosis and lowers plasma lipid peroxides in apolipoprotein E-knockout mice. Circulation. 2001, 103: 3099-3104.
Behr-Roussel D, Rupin A, Simonet S, Bonhomme E, Coumailleau S, Cordi A, Serkiz B, Fabiani JN, Verbeuren TJ: Effect of chronic treatment with the inducible nitric oxide synthase inhibitor N-iminoethyl-L-lysine or with L-arginine on progression of coronary and aortic atherosclerosis in hypercholesterolemic rabbits. Circulation. 2000, 102: 1033-1038.
Jialal I, Devaraj S: Antioxidants and atherosclerosis: don't throw out the baby with the bath water. Circulation. 2003, 107: 926-928. 10.1161/01.CIR.0000048966.26216.4C.
Patterson C, Madamanchi NR, Runge MS: The oxidative paradox: another piece in the puzzle. Circ Res. 2000, 87: 1074-1076.
Wu R, Laplante M-A, de Champlain J: Prevention of angiotensin II induced hypertension, cardiovascular hypertrophy and oxidative stress by acetylsalicylic acid in rats. J Hypertens. 2004, 22: 793-802. 10.1097/00004872-200404000-00023.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2431/8/20/prepub
Acknowledgements
The authors declare that they have no one to acknowledge.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
YFC and KO participated in the design of the study, analysis of data, and drafting of the manuscript. CWHW, SA, and YLS performed the laboratory assay of oxidative stress markers and participated in statistical analysis of laboratory results, while PCC and EWYC coordinated the study of patients and performed the echocardiographic studies. All authors have read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Cheung, Yf., O, K., Woo, C.W. et al. Oxidative stress in children late after Kawasaki disease: relationship with carotid atherosclerosis and stiffness. BMC Pediatr 8, 20 (2008). https://doi.org/10.1186/1471-2431-8-20
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2431-8-20