Abstract
Background
Glucocorticoids are often used in the treatment of nonhematologic malignancy. This review summarizes the clinical evidence of the effect of glucocorticoid therapy on nonhematologic malignancy.
Methods
A systematic review of clinical studies of glucocorticoid therapy in patients with nonhematologic malignancy was undertaken. Only studies having endpoints of tumor response or tumor control or survival were included. PubMed, EMBASE, the Cochrane Register/Databases, conference proceedings (ASCO, AACR, ASTRO/ASTR, ESMO, ECCO) and other resources were used. Data was extracted using a standard form. There was quality assessment of each study. There was a narrative synthesis of information, with presentation of results in tables. Where appropriate, meta-analyses were performed using data from published reports and a fixed effect model.
Results
Fifty four randomized controlled trials (RCTs), one meta-analysis, four phase l/ll trials and four case series met the eligibility criteria. Clinical trials of glucocorticoid monotherapy in breast and prostate cancer showed modest response rates. In advanced breast cancer meta-analyses, the addition of glucocorticoids to either chemotherapy or other endocrine therapy resulted in increased response rate, but not increased survival. In GI cancer, there was one RCT each of glucocorticoids vs. supportive care and chemotherapy +/- glucocorticoids; glucocorticoid effect was neutral. The only RCT found of chemotherapy +/- glucocorticoids, in which the glucocorticoid arm did worse, was in lung cancer. In glucocorticoid monotherapy, meta-analysis found that continuous high dose glucocorticoids had a detrimental effect on survival. The only other evidence, for a detrimental effect of glucocorticoid monotherapy, was in one of the two trials in lung cancer.
Conclusion
Glucocorticoid monotherapy has some benefit in breast and prostate cancer. In advanced breast cancer, the addition of glucocorticoids to other therapy does not change the long term outcome. In GI cancer, glucocorticoids most likely have a neutral effect. High dose continuous glucocorticoids have a detrimental effect in nonhematologic malignancy. Glucocorticoid therapy might have a deleterious impact in lung cancer.
Similar content being viewed by others
Background
Glucocorticoids are frequently used in the treatment of nonhematologic malignancy to relieve symptoms of cancer and its treatment. For example, glucocorticoids prevent vomiting and allergic reactions associated with cancer therapy. Glucocorticoids decrease edema in CNS malignancy, and can decrease pain secondary to cancer.
Glucocorticoids are part of the treatment of some cancers. Glucocorticoids, as monotherapy and in combination with ketoconazole or chemotherapy, are used in prostate cancer. They are an option for postmenopausal women with breast cancer. Thymomas are another indication for glucocorticoids. Lymphoma and multiple myeloma can respond to glucocorticoids.
The effect of glucocorticoids on the treatment of solid tumors has been reviewed. In both reviews, the possibility, that combination therapy with glucocorticoids could be detrimental, was raised. In both reviews, there was no mention of prospective clinical studies [1, 2].
Glucocorticoids are commonly used; the prospect of glucocorticoids having an unfavorable effect on cancer therapy has been brought up. With this in mind, a systematic review was done of clinical research concerning glucocorticoids in nonhematologic malignancy. The data regarding the effects of glucocorticoids, as monotherapy and in combination with other therapies (chemotherapy, hormonal therapy, radiotherapy, surgery), on nonhematologic malignancy was studied. The purpose is to make medical practice recommendations and suggest future research directions.
Methods
All RCTs found of glucocorticoids in nonhematologic malignancy that looked at any of the endpoints of tumor response, tumor control (time to disease progression, time to treatment failure, progression free survival) or overall survival were included. A trial was considered randomized if it was described as such in the manuscript. All such trials that compared a glucocorticoid arm to a nonglucocorticoid arm or compared two glucocorticoid arms were included. All meta-analyses of such randomized controlled trials were included. All phase l/ll trials found of glucocorticoid monotherapy in nonhematologic malignancy, other than breast or prostate cancer, were included. All case series found of glucocorticoid monotherapy in nonhematologic malignancy, other than breast cancer or prostate cancer or thymoma, that contained tumor response data were included. All case reports in nonhematologic malignancy, that showed either tumor suppression or enhancement in response to glucocorticoid monotherapy, were included. In breast cancer, prostate cancer and thymoma, case reports of tumor shrinkage in response to glucocorticoid monotherapy were excluded. Trials, that were unpublished or published in abstract form only, were included.
A literature search was performed using the National Library of Medicine PubMed database (1950-September 25, 2007), EMBASE (1974–2007, week 38), Cochrane Central Register of Controlled Trials (to third quarter 2007), Cochrane Database of Systematic Reviews (to third quarter 2007), Cochrane Database of Abstracts of Reviews of Effects (to third quarter 2007), ACP Journal Club (1991-September/October 2007), Index Medicus (1949–1965), Excerpta Medica (1947–1979), CINAHL (1977-September Week 3 2007), and reference lists in published papers. See Additional file 1 for the search strategies of PubMed, EMBASE, the Cochrane Library (including ACP Journal Club) and CINAHL. The Related Articles feature of PubMed was used to search for additional articles. Science Citation Index was used to check for articles citing the publications making up the systematic review. Conference proceedings of AACR (1953–2007), ASCO (1974–2007), ASTRO/ASTR (1977–2006), ESMO (1977–2006), ECCO (1991–2005) and other relevant conferences were hand searched. The National Guidelines Clearinghouse was used to check for guidelines under the disease category neoplasms available as of September 24, 2007. The literature was searched for randomized controlled trials, meta-analyses, phase l/ll trials, other clinical observational studies, practice guidelines and reviews (systematic and nonsystematic). There was no language restriction on the literature search. For some trials, authors were contacted to obtain more information. Authors, who had published more recently in this field, were contacted to see if they were aware of any unpublished case series, clinical trials or meta-analyses. Textbooks of medical oncology, radiation oncology and palliative care were reviewed to obtain further references. Ongoing trials (as of September 27, 2007) were searched for at the Clinical Trials section of the NCI website (cancer.gov) using the drug names cortisone, dexamethasone, methylprednisolone, prednisolone, prednisone and therapeutic hydrocortisone.
The author determined the eligibility of the RCTs, meta-analysis, phase l/ll trials, case series and case reports that resulted from the search. Information, regarding trial design, patient characteristics, therapy, results and quality criteria were extracted from the eligible studies by the author. Data was extracted using a standard form.
For RCTs, the quality criteria published by Jaddad et al were used. In this instrument, 0 to 2 points are assigned for randomization, 0 to 2 points are assigned for double blinding and 0 to 1 points are assigned for the description of withdrawals and dropouts. This gives a score ranging from 0 to 5 with a higher score being better [3]. For phase l trials, phase ll trials and case series, the quality criteria are those described by the Centre for Reviews and Dissemination for case series [4]. No published quality criteria for meta-analyses were found, so one was devised.
Information from the clinical trials, case series and the meta-analysis is presented in tables, with the results being synthesized in a narrative manner.
Where RCTs were similar enough in patient characteristics, therapy and endpoints, meta-analyses were performed. Response definitions were those used by the authors of each RCT; only complete and partial responses were included as responses. Followup was assumed to be complete. Survival at selected time points was extrapolated from graphs. If survival graphs were not provided, exponential survival was assumed and the median survival was used to generate survival data. Within trials, the response rates and survival in the two arms formed 2 by 2 tables for which odds ratios and their corresponding 95% confidence intervals and between trial comparisons were made using logistic regression. Homogeneity of the odds ratios across trials was evaluated using a Breslow-Day χ2 test. Odds ratio estimates and between-group comparisons for the combined trials were made using the Mantel-Haenszel fixed effect model. A result had to have a p value of less than 0.05 to be considered statistically significant.
Results
Results of Literature Search
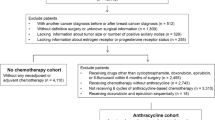
The literature was searched for clinical studies of glucocorticoids. Studies were eligible if patients had nonhematologic malignancy, and if there were endpoints of tumor response or tumor control or survival. For RCTs and meta-analyses, trials comparing two glucocorticoid arms or a glucocorticoid arm to a nonglucocorticoid arm were eligible. After excluding duplicate publications of the same trial, fifty four RCTs met the eligibility criteria ([5–54] and [55–61]); one meta-analysis met the eligibility criteria [62]. In nonhematologic malignancy other than breast or prostate cancer, four phase l/ll (nonrandomized) trials of glucocorticoid monotherapy were found [63–66]. In nonhematologic malignancy other than breast cancer or prostate cancer or thymoma, four case series of glucocorticoid monotherapy with tumor response data were identified [67–70]. One of the case series is a clinical trial; however, tumor response rate was not a preplanned endpoint, so it is presented as a case series [67]. Three clinical trials, with no available results, were identified [71–73]. Nine case reports of glucocorticoid monotherapy, other than breast cancer or prostate cancer or thymoma regressing in response to glucocorticoid monotherapy, were found [74–83]. No article was excluded due to quality.
Glucocorticoids are commonly given as premedication with chemotherapy to prevent nausea and vomiting. In the chemotherapy trials mentioned in this review, there are two trials where it is clear whether glucocorticoids were used as premedication in patients not on the glucocorticoid arm [23, 28]. In the other chemotherapy trials, there is no mention of whether such usage was permitted or not.
Case Reports
There are case reports of nonhematologic malignancy either regressing or having increased growth in response to glucocorticoids. It is reasonably well documented in the literature that thymoma can sometimes respond to glucocorticoids [84]. In melanoma, 2 doses of 100 mg of intravenous hydrocortisone 8 hours apart caused tumor lysis syndrome in a patient with melanoma [74]. There are case reports where glucocorticoids apparently stimulated the growth of melanoma [75, 76]. There is a case report of liver metastasis of thymic carcinoid responding to prednisolone [77]. Metastatic renal cell carcinoma might have shown a complete response to glucocorticoids in two patients[78, 79]. There are case reports where glucocorticoids apparently stimulated the growth of breast cancers [80–83].
Case Series
The four case series of glucocorticoid monotherapy are shown in Table 1[67–70]. They included patients with a variety of cancers, such as lung cancer, GI cancer, breast cancer and sarcoma. No tumor regression, objective improvement or relief of pain was noted. Glucocorticoid doses were not dissimilar taking into account relative glucocorticoid activities (Table 2). For any particular tumor type, the number of cases is small: the one exception is the 255 lung cancer patients in the case series of de Camp [69].
With regards to quality, two case series were from tertiary care centers; the two that were not originated from secondary care institutions [67, 69]. Three of the four case series had less than 50 patients [67, 68, 70]. None of the case series were multi-institutional. Three of the four case series did not describe eligibility criteria [68–70]. In one case series, patients were similar with regards to the state of cancer progression; in the other studies, not enough information was provided to assess similarity [67]. In one case series, followup was long enough to assess whether glucocorticoids could cause cancer to decrease in size; in the other studies, it was unclear if followup was sufficient to assess this [70]. In none of the case series was reduction in tumor size assessed using objective criteria.
Phase l and Phase ll (Nonrandomized) Trials
In phase l/ll (nonrandomized) trials, responses have been noted. Based on responses lasting at least 28 days, responses in the four trials were 0% [63], 6% [64], 6% [65] and 6% [66]. In the largest trial (407 patients), 13 of the 24 responses were in breast and prostate cancer with the 2 complete responses being in breast and prostate cancer [66]. The next largest trial was 94 patients with no responses [63]. The phase l/ll (nonrandomized) clinical trials are presented in Table 3.
The two glucocorticoids used in these clinical trials were fluorometholone and NSC-17256. Fluorometholone may have progestational properties [22]. One hundred mg of NSC-17256 is equivalent to 50–67 mg of prednisone; however, it also has sex steroid properties.
With regards to quality, all the clinical trials were from tertiary care centers. All clinical trials had more than 50 patients. Three of the four trials were multi-institutional [63, 65, 66]. One of the trials did not describe eligibility criteria [65]. In one trial, patients were similar with regards to the state of cancer progression; in the other trials, not enough information was provided to assess similarity [64]. In two trials, followup was long enough to assess whether glucocorticoids could cause cancer to regress in size; in the other two trials, it was unclear if followup was sufficient to assess this [64, 66]. Reduction in tumor size was assessed using objective criteria in three of the studies [64–66]; this was unclear in the other study.
Randomized Controlled Trials of Glucocorticoids in the Endocrine Therapy of Advanced Breast Cancer
There are two types of trials in this category. In the first type, glucocorticoids are given as monotherapy and compared to other endocrine therapies given as monotherapy. There are ten trials of this type, which tend to be small and often use endocrine therapies that are no longer given. In these trials, the vast majority of patients were postmenopausal or enrolment was limited to postmenopausal patients. The results show that glucocorticoids have modest activity in postmenopausal women. A description of these trials is given in Table 4[5, 15, 18, 19, 22, 38, 47, 55, 56]. The three earliest trials used response criteria that are not readily comparable to presently used response criteria [5, 19, 22].
The second type of trial is of an endocrine agent +/- glucocorticoids. These trials tend to be larger, more recent and limited to women who are postmenopausal or who received ovarian irradiation. There are four trials in this category: three are of tamoxifen +/- glucocorticoids and one is of aminoglutethimide +/- glucocorticoids. Results are presented in Table 4[7, 24, 37, 46]. As these trials were more similar in nature, meta-analyses of response rates and survival were undertaken. As seen in Figure 1, the addition of glucocorticoids to another endocrine therapy resulted in an increased response rate. Figure 2 shows that this addition does not change one year survival rates. However, there was evidence for a lack of homogeneity among the four studies in Figure 2, as shown by the chi-square test and its p value. The meta-analysis was repeated, except that the trial which was furthest from the other three trials in response rate and survival was omitted [24]. The result of the omission was that the addition of glucocorticoids did not change one year survival rates, although the lack of homogeneity disappeared (odds ratio of 0.91 95% CI 0.77–1.08, X2 2 = 3.389 p = 0.184).
One unpublished trial of hormonal therapy +/- glucocorticoids, with no available results, was found [72].
Randomized Controlled Trials of Glucocorticoids in the Endocrine Therapy of Breast Cancer in the Adjuvant Setting
In this setting, there are trials of endocrine therapy +/- glucocorticoids and trials of glucocorticoid monotherapy compared to no therapy: they are summarized in Table 5. The trials of endocrine therapy +/- glucocorticoids consist of two trials of tamoxifen +/- glucocorticoids in postmenopausal women; these trials are negative [6, 9]. This is consistent with the results from the advanced breast cancer setting.
In the first of the two trials of glucocorticoid monotherapy, glucocorticoids weren't beneficial in the postmenopausal group; they might have been beneficial in the premenopausal group, who were treated with ovarian irradiation [44]. In the second trial of glucocorticoid monotherapy, premenopausal women were randomly treated with chemotherapy or ovarian ablation followed by a second randomization to glucocorticoids versus no glucocorticoids. Regardless of whether a woman received chemotherapy or ovarian ablation, glucocorticoids were not beneficial. In the 81% of patient in whom ER status was known, chemotherapy tended to be more effective than ovarian ablation in those with low ER concentrations whereas the opposite was true in those with higher ER concentrations. No such relationship was noted when the no prednisolone/prednisolone arms were compared [13].
One feature that complicates interpretation of the second trial is that glucocorticoids were started at the time of oophorectomy or at the start of chemotherapy, and were to be given for 5 years unless relapse occurred. Those in the chemotherapy arm got glucocorticoids during their 24 weeks of chemotherapy. This means that this trial could also be considered a chemotherapy +/- glucocorticoids trial. Glucocorticoid administration resulted in less bone marrow suppression during chemotherapy [13].
Randomized Controlled Trials of Chemotherapy +/- Glucocorticoids in Advanced Breast Cancer
There are eight trials of chemotherapy +/- glucocorticoids in advanced breast cancer [16, 17, 21, 25, 28, 31, 40, 48]; results are presented in Table 6. Decreased thrombocytopenia [21, 40] and increased administered chemotherapy dose [21, 40, 48] were associated with glucocorticoid administration in several of these trials.
In six of these trials, response rates are given; in four of these trials, survival data is given. It was felt that there was enough similarity in these trials to perform meta-analyses. Meta-analyses of response rates and survival are presented in Figures 3 and 4 respectively. The addition of glucocorticoids to chemotherapy in the advanced breast cancer setting resulted in an increased response rate. However, there was no effect on one year survival.
Randomized Controlled Trials of Chemotherapy +/- Glucocorticoids of Breast Cancer in the Adjuvant Setting
There are two trials in this category. Both are relatively large trials of CMF+/-prednisone, and both are negative. This is consistent with what has been found in the advanced breast cancer setting. At the time of enrolment, none of the participants were postmenopausal. In comparison to trials that enroll postmenopausal women, this might lessen the possible impact of glucocorticoids as endocrine therapy. However, many women on these trials subsequently developed amenorrhea. In the trial of Tormey et al, 20% subsequently became postmenopausal. In the trial of the Ludwig Breast Cancer Study Group, 85% subsequently became postmenopausal. A description of these trials is given in Table 7[12, 53, 85].
As in the randomized controlled trials of chemotherapy +/- glucocorticoids in the advanced breast cancer setting, there is evidence of decreased leukopenia [53], decreased thrombocytopenia [12], increased chemotherapy dose [53], and increased chemotherapy dose intensity [12] in the glucocorticoid arms.
In one of the trials, there was a significant increase in bone, alone or in combination with other sites, as the site of first relapse in the chemotherapy plus prednisone arm (relative risk of 2.06, 95% CI of 0.91 to 12.31, p = 0.09). The authors postulated that the increased rate of bone metastases as a first relapse site in this arm might be due to cytokine inhibition, which might reduce a putative anti-cancer process in bone, or to increased bone absorption [53].
Randomized Controlled Trials of Glucocorticoids in Prostate Cancer
In prostate cancer, there are two RCTs of glucocorticoids in untreated patients [43, 59]. Both are trials of orchiectomy versus orchiectomy plus glucocorticoids versus orchiectomy plus cyproterone acetate. The small numbers enrolled preclude analysis, other than it is improbable that glucocorticoids worsen outcome when added to orchiectomy. Both trials used response criteria that are not readily comparable to presently used response criteria.
There are five randomized controlled trials of glucocorticoids in patients with hormone refractory prostate cancer [8, 32, 33, 35, 36, 54, 60]. These are all trials comparing glucocorticoid monotherapy to other monotherapies. When glucorticoids are compared to other hormonal therapies (progestational agents and flutamide), little difference was noted. When glucocorticoids were compared to liarozole (a retinoic acid stimulating agent), glucocorticoids resulted in a better outcome. In the three oldest trials, the response criteria used are not readily comparable to presently used response criteria [8, 33, 35].
There is one randomized controlled trial of chemotherapy +/- glucocorticoids in prostate cancer [50]. This small trial has been published in abstract form only; it is difficult to draw conclusions based on the information presented.
See Table 8 for a description of these trials.
There are two ongoing randomized controlled trials of chemotherapy +/- glucocorticoids in hormone refractory prostate cancer; results are not available [71, 73].
Randomized Controlled Trials of Glucocorticoids in GI Cancer
There is one trial comparing glucocorticoid monotherapy to placebo in GI cancer; no difference in survival was found [26].
There are two trials of chemotherapy +/- glucocorticoids in GI cancer [11, 20]. One of the two trials used response criteria that are not readily comparable to those presently used. In that trial, fluorometholone monotherapy had a response rate of 9%. The addition of fluorometholone to 5-FU did not change the response rate of 13% [20]. In the other trial of chemotherapy +/- glucocorticoids (FUDR +/- dexamethasone), the addition of glucocorticoids resulted in an increased response rate and a borderline improvement in survival (p = 0.06). However, FUDR dose, as the mean percentage of planned FUDR dose, was 61% and 52% in the FUDR/dexamethasone arm and FUDR arm respectively (p = 0.13). At least in part, the increased dose of FUDR in the FUDR/dexamethasone arm was due to the decreased biliary toxicity associated with concurrent dexamethasone administration resulting in less FUDR dose reductions. The chemoprotective property of dexamethasone, allowing a greater FUDR dose, may have contributed to the improved results in the combined arm [11]. Other postulated reasons are a potentiation of FUDR cytotoxicity by dexamethasone and a potential antiangiogenic property of dexamethasone [86, 87].
There are two trials of preoperative glucocorticoids in patients scheduled to undergo esophagectomy; there was no effect on survival [51, 58].
A description of the GI trials is given in Table 9.
Randomized Controlled Trial of Glucocorticoids in Patients with Primary CNS Neoplasms
The one RCT of glucocorticoids in primary CNS neoplasms is described in Table 10. This trial uses a higher dose of glucocorticoids than any other trial described in this review; however, administration was on an intermittent, rather than a continuous, basis. This trial compared methyprednisolone versus BCNU versus BCNU plus methylprednisolone versus procarbazine. The addition of methylprednisolone to BCNU had a neutral effect on survival. Infection was significantly greater in the BCNU plus methylprednisolone arm than the other arms; information on the type and severity of infection is not available. The mean number of courses of chemotherapy was identical in the BCNU and BCNU + methylprednisolone arms. The mean radiotherapy dose +/- SE (rads) was 5701 +/- 79 in the methylprednisolone arm and 5589 +/- 96 in the BCNU + methylprednisolone arm [23].
Randomized Controlled Trials of Glucocorticoids in Patients with GU Neoplasms
No trials were found in this category.
Randomized Controlled Trials and Meta-analysis of Glucocorticoids in Patients with a Variety of Cancers
There are five randomized controlled trials of glucocorticoid monotherapy in patients with a variety of cancers; these trials are dissimilar in nature.
The first two trials used glucocorticoid doses higher than any other trial in this review, with the exception of the previously mentioned randomized controlled trial in CNS neoplasms. However, glucocorticoid administration was continuous in these two trials. Also, administration was intravenous; the bioavailability of oral methyprednisolone is 82% [88]. The two trials are very similar, except that enrolment was limited to females with the second trial [30, 39]. With this in mind, a survival meta-analysis was performed, with the results presented in Figure 5. Figure 5 shows that this high dose continuous gluccorticoid schedule had a detrimental effect on mortality. In the first trial, the cause for the difference in mortality was unknown. In the second trial, there were significantly more gastrointestinal and cardiovascular adverse events in the glucocorticoid arm; the severity and outcome of these events did not significantly differ. Infectious complications occurred in 11.8% of the treated patients and 14.8% of the placebo patients [39].
The third trial consists mostly of GI patients, and compared indomethacin to prednisolone to placebo. The results suggest that prednisolone might have a beneficial effect on survival [14].
The fourth trial compares a progestational agent to dexamethasone to an androgen; no difference in survival was observed. The patients were mostly lung and GI cancer patients. Fifty three percent and twenty percent of the patients had planned concurrent chemotherapy and radiation therapy respectively.
The fifth trial compares opioids to opioids plus dexamethasone; no survival difference was found. This was a group of patients with very advanced cancer; no patient lived longer than 45 days [61].
There is a meta-analysis of three small RCTs of glucocorticoids in patients with bowel obstruction secondary to malignancy. The treatment period in these 3 trials lasted from 3–10 days; after the treatment period, glucocorticoids were not prohibited. There was no survival difference [62].
There are two trials of chemotherapy +/- glucocorticoids. In the older of these two trials, glucocorticoids had a neutral effect. In this trial, the remission criteria are not readily comparable to those presently used [27]. In the second trial, glucocorticoids ameliorated the GI toxicity of perifosine resulting in longer duration of treatment in the glucocorticoid arm: glucocorticoids may have acted as a chemoprotective agent [52].
Finally, there is one trial of radiation +/- glucocorticoids in patients with epidural metastases of a carcinoma compressing the spinal cord or cauda equina [29]; there is a second trial comparing two doses of glucocorticoids in patients with spinal cord compression [57]. In both of these trials, a large proportion of patients had breast or prostate cancer. There was no survival difference in either trial.
About the quality of the meta-analysis, the inclusion criteria were objective and explicit. The literature search was thorough. There was quality assessment of the clinical trials that made up the meta-analysis. There was independent data abstraction by two reviewers. Individual patient data was used to obtain survival analysis. However, the meta-analysis is based on the results of 83 patients [62].
A description of these trials and the meta-analysis is given in Table 11.
Randomized Controlled Trials of Glucocorticoids in Lung Cancer
There are two randomized controlled trials of glucocorticoid monotherapy in lung cancer [10, 41, 42], with both being described in Table 12. In the first trial, those in the glucocorticoid arm did worse than those in the placebo arm. As causes of death, rates of pulmonary infection, hemorrhage, heart failure and perforated ulcer were very similar between the placebo and cortisone arms. The authors stated that they were unable to explain why the cortisone arm did worse [41]. In a later publication regarding this trial, it is noted that results were not different between patients, who had received prior to the trial, surgery, radiation therapy or who hadn't received either therapy. Although it is unclear how systematically this was studied, the authors did not observe a difference in the rate of cancer progression between the placebo and cortisone arms based on x-ray and autopsy information [42]. The second trial is a comparison of prednisolone versus megestrol acetate; those in the megestrol acetate arm did significantly worse [10]. As mentioned in Table 12, no radiation with a curative intent or chemotherapy was given in the second trial (F. Macbeth, personal communication).
In lung cancer, there are two randomized controlled trials of chemotherapy +/- glucocorticoids; both are included in Table 12. The first trial was of cyclophosphamide +/-prednisolone; the addition of prednisolone resulted in a lower response rate and decreased survival. Of the planned cyclophosphamide doses, 88% were administered in the cyclophosphamide arm and 69% were administered in the combined arm. As for treatment delays, 4 patients were delayed 1–2 weeks with 3 of these being in the cyclophosphamide arm. No patient died of treatment in the cyclophosphamide arm, but 3 died of infection in the combined arm. Six patients had infections requiring hospitalization in the cyclophosphamide arm, compared to 2 in the combined arm. There was no significant difference in hematologic toxicity between the 2 arms. There was a trend for less leukopenia in the combined arm. In the cyclophosphamide arm, a leukocyte count of less than 1999 cells/mm3 occurred in 43% of patients in cycle 1, 96% in cycle 2 and 100% in cycle 3. In the combined arm, comparable data is 28% in cycle 1, 60% in cycle 2 and 77% in cycle 3 [34]. In the second trial of chemotherapy +/- glucocorticoids, patients were given four cycles of chemotherapy. Those in the chemotherapy + glucocorticoid arms (cohorts 2 and 3) received dexamethasone with the last three cycles; cohort 1 received only chemotherapy. Neutropenia and thrombocytopenia were significantly decreased by the use of glucocorticoids [89].
Discussion
As monotherapy, glucocorticoids are thought to have activity in breast cancer, prostate cancer and thymoma. The evidence found in this review is consistent with that. In Table 2, no responses were observed in case series data. Although the quality of this generally older data is not comparable to that from present clinical trials, it is unlikely that major changes went undetected. In Table 3, there is mention of responses in cancers other than breast, prostate or thymoma in clinical trial data. However, responses in these older trials were determined by physical examination and xrays. If present day imaging had been used in these trials, it would not have been surprising if response rates were lower than those given. In one trial, it was postulated that some tumor responses may have been a consequence of anti-inflammatory activity, rather than anti-tumor activity [64].
A postulated mechanism of action of glucocorticoids in prostate cancer is adrenal androgen suppression [90]. For breast cancer, postulated mechanisms are adrenocortical inhibition and interaction with glucocorticoid receptors [91]. The one breast cancer trial which looked at whether there was a correlation between ER status and the effect of glucocorticoids did not find one [13]. This lack of correlation suggests that glucocorticoid therapy does not act through the ER receptor. If this is true, a patient's menstrual status may be important with regards to the effectiveness of glucocorticoids. This is relevant, because some of the RCTs of glucocorticoids in breast cancer, especially the chemotherapy trials, included premenopausal women.
Meta-analyses of endocrine therapy +/- glucocorticoids in advanced breast cancer were undertaken. An increased response rate was noted, but there was no improvement in survival. A previous meta-analysis of tamoxifen +/- other endocrine therapy in metastatic breast cancer has been published [92]. This meta-analysis included two of the four papers used in the meta-analysis presented in this publication. The previously published meta-analysis also showed an improved response rate, but no improvement in survival
There was heterogeneity noted in the survival meta-analysis of endocrine therapy +/- glucocorticoids in advanced breast cancer. A critical variable in response to endocrine therapy is ER/PR status. In the four older trials used in that meta-analysis, one trial enrolled patients regardless of ER/PR status [24]. In all four trials, patients of unknown receptor status were enrolled; the percentage of patients with unknown receptor status was as high as 47% [37]. Receptor heterogeneity may explain in part the observed statistical heterogeneity.
Meta-analyses of chemotherapy +/- glucocorticoids in advanced breast cancer were undertaken. Once again, an increased response rate was noted, but no improvement in survival. The meta-analysis of tamoxifen +/- other endocrine therapy in metastatic breast cancer also included a meta-analysis of chemotherapy +/- endocrine therapy. That meta-analysis did not include any of the six trials included in this publication's meta-analysis of chemotherapy +/- glucocorticoids. The meta-analysis of chemotherapy +/- endocrine therapy similarly showed an improved response rate, but no change in survival [92].
In several breast cancer trials of chemotherapy +/- glucocorticoids, there was increased chemotherapy dose administered and less hematologic toxicity in the arms receiving glucocorticoids. The information presented in the results section may underestimate these effects, as trials in which there were nonsignificant differences are not mentioned. This decreased hematologic toxicity is consistent with the known effects of glucocorticoids on the hematopoeitic system [93]. In the RCTs of chemotherapy +/- glucocorticoids of breast cancer in the adjuvant setting, increased chemotherapy dose/dose intensity and decreased hematologic toxicity did not translate into improved outcomes. However, the two trials reporting this were trials of 12 months of chemotherapy [12, 85]. With such prolonged chemotherapy, cumulative dose and dose intensity may be less important. Glucocorticoids are commonly given with chemotherapy to patients with metastatic breast cancer as antiemetics; they may be doing more than preventing nausea and vomiting in some patients.
In prostate cancer, glucocorticoids are used in combination with other endocrine therapy (ketoconazole) and chemotherapy. The evidence for this is not strong. If the breast cancer results are applicable to prostate cancer, it is debatable whether such combination therapy is of benefit.
The RCTs of glucocorticoids in GI cancer would suggest that the effect of glucocorticoids is neutral. However, GI cancer includes a diverse group of cancers; one cannot exclude the possibility that glucocorticoids might not have a neutral effect in a particular type of GI cancer. The trial of Lundholm et al is presented in Table 11 because patients with a variety of cancer were eligible; however, 79% of the patients had GI cancer. In that trial, there is a suggestion that glucocorticoids might improve outcome [14].
There were two trials of high dose continuous glucocorticoids compared to placebo in patients with nonhematologic malignancy. There was only one other randomized controlled trial which used a glucocorticoid dose that was greater than the dose used in those two trials. In that trial, patients were on glucocorticoids only one quarter of the time [23]. When the results of the two trials of high dose continous glucocorticoids were combined in a meta-analysis, there was a detrimental effect of glucocorticoids on mortality. This raises the possibility that glucocorticoids, at sufficient dose, may have an adverse effect on patients with nonhematologic malignancy. This is especially relevant to patients with primary and secondary CNS malignancy, where doses of 16 mg per day of dexamethasone are used.
It also raises the question of what is a safe dose of glucocorticoids in patients with nonhematologic malignancy. The answer to this may in part depend on the site of origin of the cancer. In GI cancer, dexamethasone 6 mg daily appears to be safe [26]. In lung cancer, 100 mg daily of cortisone may be unsafe [41]. In the two trials of continuous high dose glucocorticoids, a considerable portion of the patients had breast cancer. In one of the two trials, survival was analyzed according to the origin of the cancer. When the treatment and placebo groups were compared in these analyses, no differences of statistical significance were observed [39].
The only other evidence of glucocorticoids, resulting in a worse outcome than those in the placebo/best supportive care arm, is in the single trial of lung cancer. This 1960 publication gives limited statistical detail. However, it appears that the difference between the glucocorticoid arm and the placebo arm had a p value of 0.02. It is difficult to explain the worse outcome on the dose of glucocorticoid given, as the daily dose was 100 mg of cortisone [41].
The only trial of chemotherapy +/- glucocorticoids, in which the glucocorticoid arm did worse, is in lung cancer. There was a nonsignificant trend for decreased leukopenia in this trial [34]. Others have observed decreased granulocytopenia [94, 95] and decreased thrombocytopenia [94] when glucocorticoids are given with chemotherapy in lung cancer patients. In the lung cancer trial of cyclophosphamide +/- prednisone, the authors postulated that the differences found between the 2 arms might be due to the effect of prednisone on the metabolism of cyclophosphamide; however, they themselves noted that both the animal and human data on this effect are conflicting. In the trials of chemotherapy +/- glucocorticoids in breast cancer, a number of the trials included cyclophosphamide as part of CMF. The dose of glucocorticoids given in the lung cancer trial of chemotherapy +/- glucocorticoids is not greatly different than the dose given commonly as an antiemetic to lung cancer patients on chemotherapy.
It cannot be ruled out that glucocorticoids have an effect on the newer targeted therapies. Glucocorticoids are commonly given with monoclonal antibodies. A postulated mechanism of action of one of those antibodies, trastuzumab, is via antibody-dependent cellular cytotoxicity [96]. There is evidence that glucocorticoid may inhibit antibody-dependent cellular cytotoxicity [97].
There are limitations to the meta-analyses presented in this study. Firstly, there may be unpublished randomized controlled trials that are not included. Secondly, survival was extrapolated from summary graphs and data, and the point estimates are not as accurate as those that could have been derived from the individual patient data. Thirdly, the number of trials and the number of patients in each trial tended to be small; this makes heterogeneity more likely. For each meta-analysis, a chi-square test was used to assess heterogeneity. However, a chi-square test has low power if there are few trials or sample sizes are small.
There is evidence that glucocorticoids have an effect on the natural history of some nonhematologic malignancies. However, that is not the only source of glucocorticoids that a cancer is exposed to. One's own body synthesizes endogenous glucocorticoids. This raises the question of what effect endogenous glucocorticoids have on nonhematologic malignancy. The possible effect of endogenous glucocorticoids on lung cancer is the subject of another review (manuscript in preparation).
Breast cancer, prostate cancer and possibly lung cancer show sensitivity to glucocorticoids. There may be variability within cancers of each type in their sensitivity. This raises the issue of predictive factors, that might assist in assessing glucocorticoid sensitivity. Glucocorticoid receptor status or histologic subtype (in lung cancer) might be relevant. A genomic/proteomic approach to explore this possibility might be useful.
Conclusion
The effect of glucocorticoids in nonhematologic malignancy depend on the primary tumor site. Glucocorticoids have a beneficial effect in breast and prostate cancer as monotherapy. In combination with chemotherapy or other endocrine therapy in breast cancer; glucocorticoids increase response rate, but do not change survival. In GI cancer, they most likely have a neutral effect. High dose continuous glucocorticoids, in patients with nonhematologic malignancy, decrease survival. Such treatment should be avoided in patients with nonhematologic malignancy. Based on ASCO criteria, this is a grade B recommendation based on level ll evidence. In lung cancer, glucocorticoids might have a deleterious effect by themselves and when given with chemotherapy. It is recommended that glucocorticoid use in lung cancer patients be kept to the minimum required. This is a grade B recommendation based on level ll evidence.
Abbreviations
- AV:
-
adriamycin 60 mg/m2 IV day 1 and vincristine 1.2 mg/m2 IV day 1 every 21 days
- BCNU:
-
carmustine
- CI:
-
confidence interval
- CMF:
-
cyclophosphamide 100 mg/m2 po daily days 1–14 and methotrexate 40 mg/m2 IV days 1 and 8 and 5-FU 600 mg/m2 IV days 1 and 8 every 28 days
- CMFP:
-
CMF and prednisone 40 mg/m2/day days 1–14
- CR:
-
complete response
- ER:
-
estrogen receptor
- 5-FU:
-
5-fluorouracil
- FUDR:
-
fluorodeoxyuridine
- IM:
-
intramuscular
- IV:
-
intravenous
- m2 :
-
meters squared
- MPA:
-
medroxyprogesterone acetate
- -ve:
-
negative
- ns:
-
not significant
- NR:
-
not reported
- NSC-17256:
-
6a-methylpreg-4-ene-3,11,20-trione
- NSCLC:
-
nonsmall cell lung cancer
- PD:
-
progressive disease
- +ve:
-
positive
- PR:
-
partial response
- PgR:
-
progesterone receptor
- po:
-
by mouth
- SCLC:
-
small cell lung cancer
- SD:
-
stable disease
- SE:
-
standard error
- vs.:
-
versus
References
Rutz HP: Effects of corticosteroid use on treatment of solid tumours. Lancet. 2002, 360 (9349): 1969-1970. 10.1016/S0140-6736(02)11922-2.
Herr I, Pfitzenmaier J: Glucocorticoid use in prostate cancer and other solid tumours: implications for effectiveness of cytotoxic treatment and metastases. Lancet Oncol. 2006, 7 (5): 425-430. 10.1016/S1470-2045(06)70694-5.
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ: Assessing the quality of reports of randomized clinical trials: is blinding necessary?. Control Clin Trials. 1996, 17 (1): 1-12. 10.1016/0197-2456(95)00134-4.
Undertaking Systematic Reviews of Research on Effectiveness, CRD's Guidance for Those Carrying Out or Commissioning Reviews. CRD Report Number 4. Centre for Reviews and Dissemination, University of York, York, UK, 2
Colsky J: A comparative study of 9alpha-bromo-11beta-keto-progesterone and prednisolone in the treatment of advanced carcinoma of the female breast. Cancer. 1963, 16: 502-505. 10.1002/1097-0142(196304)16:4<502::AID-CNCR2820160410>3.0.CO;2-M.
Fentiman IS, Howell A, Hamed H, Lee SM, Ranson M, Wall J, Chaudary MA, Ash CM, Gregory WM, Sellwood RA, et al: A controlled trial of adjuvant tamoxifen, with or without prednisolone, in post-menopausal women with operable breast cancer. Br J Cancer. 1994, 70 (4): 729-731.
Ingle JN, Mailliard JA, Schaid DJ, Krook JE, Gesme DH, Windschitl HE, Pfeifle DM, Etzell PS, Gerstner JG, Long HJ, et al: A double-blind trial of tamoxifen plus prednisolone versus tamoxifen plus placebo in postmenopausal women with metastatic breast cancer. A collaborative trial of the North Central Cancer Treatment Group and Mayo Clinic. Cancer. 1991, 68 (1): 34-39. 10.1002/1097-0142(19910701)68:1<34::AID-CNCR2820680107>3.0.CO;2-Q.
Patel SR, Kvols LK, Hahn RG, Windschitl H, Levitt R, Therneau T: A phase II randomized trial of megestrol acetate or dexamethasone in the treatment of hormonally refractory advanced carcinoma of the prostate. Cancer. 1990, 66 (4): 655-658. 10.1002/1097-0142(19900815)66:4<655::AID-CNCR2820660409>3.0.CO;2-P.
DiMartino L, Demontis B, Mitchell IP, Hayward SW, Deshpande N: A randomized clinical trial to investigate the usefulness of the addition of prednisolone to tamoxifen as adjuvants to mastectomy in primary breast cancer patients with a high risk of recurrence: a preliminary report. Anticancer Res. 1991, 11 (2): 869-872.
Macbeth F, Gregor A, Cottier B: A randomised study of megestrol acetate (MA) and prednisolone (P) for anorexia and weight loss in patients with lung cancer. Lung Cancer. 1994, 11 (Supplement 1): 334-
Kemeny N, Seiter K, Niedzwiecki D, Chapman D, Sigurdson E, Cohen A, Botet J, Oderman P, Murray P: A randomized trial of intrahepatic infusion of fluorodeoxyuridine with dexamethasone versus fluorodeoxyuridine alone in the treatment of metastatic colorectal cancer. Cancer. 1992, 69 (2): 327-334. 10.1002/1097-0142(19920115)69:2<327::AID-CNCR2820690209>3.0.CO;2-U.
Tormey DC, Gray R, Gilchrist K, Grage T, Carbone PP, Wolter J, Woll JE, Cummings FJ: Adjuvant chemohormonal therapy with cyclophosphamide, methotrexate, 5-fluorouracil, and prednisone (CMFP) or CMFP plus tamoxifen compared with CMF for premenopausal breast cancer patients. An Eastern Cooperative Oncology Group trial. Cancer. 1990, 65 (2): 200-206. 10.1002/1097-0142(19900115)65:2<200::AID-CNCR2820650203>3.0.CO;2-Q.
Adjuvant ovarian ablation versus CMF chemotherapy in premenopausal women with pathological stage II breast carcinoma: the Scottish trial. Scottish Cancer Trials Breast Group and ICRF Breast Unit, Guy's Hospital, London. Lancet. 1993, 341 (8856): 1293-1298.
Lundholm K, Gelin J, Hyltander A, Lonnroth C, Sandstrom R, Svaninger G, Korner U, Gulich M, Karrefors I, Norli B, et al: Anti-inflammatory treatment may prolong survival in undernourished patients with metastatic solid tumors. Cancer Res. 1994, 54 (21): 5602-5606.
Goldenberg IS: Clinical trial of delta-1-testololactone (NSC 23759), medroxy progesterone acetate (NSC 26386) and oxylone acetate (NSC 47438) in advanced female mammary cancer. A report of the cooperative breast cancer group. Cancer. 1969, 23 (1): 109-112. 10.1002/1097-0142(196901)23:1<109::AID-CNCR2820230112>3.0.CO;2-1.
Ramirez G, Klotz J, Strawitz JG, Wilson WL, Cornell GN, Madden RE, Minton JP: Combination chemotherapy in breast cancer: a randomized study of 4 versus 5 drugs. Oncology. 1975, 32 (3–4): 101-108.
Brambilla C, De Lena M, Bonadonna G: Combination chemotherapy with adriamycin (NSC-123127) in metastatic mammary carcinoma. Cancer Chemother Rep. 1974, 58 (2): 251-253.
Gaertner RA, Lewison EF, Finney GG, Montague AC: Combined hormone therapy in advanced breast cancer. Triple-blind study of 68 patients treated with dromostanolone and fluorometholone. Johns Hopkins Med J. 1968, 123 (3): 138-141.
Dao TL, Tan E, Brooks V: A comparative evaluation of adrenalectomy and cortisone in the treatment of advanced mammary carcinoma. Cancer. 1961, 14: 1259-1265. 10.1002/1097-0142(196111/12)14:6<1259::AID-CNCR2820140616>3.0.CO;2-4.
Reitemeier RJ, Moertel CG, Hahn RG: Comparative evaluation of palliation with fluorometholone (NSC-33001), 5-fluorouracil (NSC-19893), and combined fluorometholone and 5-fluorouracil in advanced gastrointestinal cancer. Cancer Chemother Rep. 1967, 51 (2): 77-80.
Tormey DC, Gelman R, Band PR, Sears M, Rosenthal SN, DeWys W, Perlia C, Rice MA: Comparison of induction chemotherapies for metastatic breast cancer. An Eastern Cooperative Oncology Group Trial. Cancer. 1982, 50 (7): 1235-1244. 10.1002/1097-0142(19821001)50:7<1235::AID-CNCR2820500703>3.0.CO;2-L.
Talley RW, Brennan MJ, Vaitkevicius VK, Sandiego EL, Reed ML, Leighton GA: Comparison of 6-Alpha-Methyl-9-Alpha-Fluoro-17-Acetoxy-21-Deoxyprednisolone with Fluoxymesterone and Methylprednisolone in Treatment of Metastatic Breast Cancer. Cancer. 1964, 17: 1063-1066. 10.1002/1097-0142(196408)17:8<1063::AID-CNCR2820170812>3.0.CO;2-T.
Green SB, Byar DP, Walker MD, Pistenmaa DA, Alexander E, Batzdorf U, Brooks WH, Hunt WE, Mealey J, Odom GL, et al: Comparisons of carmustine, procarbazine, and high-dose methylprednisolone as additions to surgery and radiotherapy for the treatment of malignant glioma. Cancer Treat Rep. 1983, 67 (2): 121-132.
Stewart JF, Rubens RD, King RJ, Minton MJ, Steiner R, Tong D, Winter PJ, Knight RK, Hayward JL: Contribution of prednisolone to the primary endocrine treatment of advanced breast cancer. Eur J Cancer Clin Oncol. 1982, 18 (12): 1307-1314. 10.1016/0277-5379(82)90134-1.
Rossi A, Brambilla C, Bonadonna G: Controlled study with 1-phenylalanine mustard (l-PAM) and 5-fluorouracil (5-FU) plus or minus prednisone in advanced breast cancer. Tumori. 1976, 62 (2): 193-196.
Moertel CG, Schutt AJ, Reitemeier RJ, Hahn RG: Corticosteroid therapy of preterminal gastrointestinal cancer. Cancer. 1974, 33 (6): 1607-1609. 10.1002/1097-0142(197406)33:6<1607::AID-CNCR2820330620>3.0.CO;2-V.
Horton J, Olson KB, Hosley HF: Corticosteroids and fluorouracil toxicity. Arch Intern Med. 1966, 117 (6): 775-777. 10.1001/archinte.117.6.775.
Piccart MJ, Klijn J, Paridaens R, Nooij M, Mauriac L, Coleman R, Bontenbal M, Awada A, Selleslags J, Van Vreckem A, et al: Corticosteroids significantly delay the onset of docetaxel-induced fluid retention: final results of a randomized study of the European Organization for Research and Treatment of Cancer Investigational Drug Branch for Breast Cancer. J Clin Oncol. 1997, 15 (9): 3149-3155.
Sorensen S, Helweg-Larsen S, Mouridsen H, Hansen HH: Effect of high-dose dexamethasone in carcinomatous metastatic spinal cord compression treated with radiotherapy: a randomised trial. Eur J Cancer. 1994, 30A (1): 22-27. 10.1016/S0959-8049(05)80011-5.
Della Cuna GR, Pellegrini A, Piazzi M: Effect of methylprednisolone sodium succinate on quality of life in preterminal cancer patients: a placebo-controlled, multicenter study. The Methylprednisolone Preterminal Cancer Study Group. Eur J Cancer Clin Oncol. 1989, 25 (12): 1817-1821. 10.1016/0277-5379(89)90353-2.
Gercovich F, Negro A, Requejo H, Morgenfeld E, Rivarola E, Pasccon G, Botto G, Marantz A, Tessler J, Elli A, et al: 5Fluorouracil, cyclophosphamide and mitoxantrone (fucimix) vs fucimix-prednisone (pdn) for advanced breast cancer (abc). A prospective and randomized trial. Preliminar report. Proceedings of AACR. 1989, 30: 1014-
Fossa SD, Slee PH, Brausi M, Horenblas S, Hall RR, Hetherington JW, Aaronson N, de Prijck L, Collette L: Flutamide versus prednisone in patients with prostate cancer symptomatically progressing after androgen-ablative therapy: a phase III study of the European organization for research and treatment of cancer genitourinary group. J Clin Oncol. 2001, 19 (1): 62-71.
Fossa SD, Jahnsen JU, Karlsen S, Ogreid P, Haveland H, Trovag A: High-dose medroxyprogesterone acetate versus prednisolone in hormone-resistant prostatic cancer. A pilot study. Eur Urol. 1985, 11 (1): 11-16.
Thatcher N, Wagstaff J, Wilkinson P, Palmer M, Crowther D: Intermittent high-dose cyclophosphamide with and without prednisolone: a study of the relationships between toxicity, response and survival in metastatic lung cancer. Cancer. 1982, 50 (6): 1051-1056. 10.1002/1097-0142(19820915)50:6<1051::AID-CNCR2820500605>3.0.CO;2-X.
Datta SN, Thomas K, Matthews PN: Is prednisolone as good as flutamide in hormone refractory metastatic carcinoma of the prostate?. J Urol. 1997, 158 (1): 175-177. 10.1097/00005392-199707000-00056.
Sabbatini P, Larson SM, Kremer A, Zhang ZF, Sun M, Yeung H, Imbriaco M, Horak I, Conolly M, Ding C, et al: Prognostic significance of extent of disease in bone in patients with androgen-independent prostate cancer. J Clin Oncol. 1999, 17 (3): 948-957.
Cocconi G, Bisagni G, Ceci G, Bacchi M, Boni C, Brugia M, Carpi A, Di Costanzo F, Franciosi V, Gori S, et al: Low-dose aminoglutethimide with and without hydrocortisone replacement as a first-line endocrine treatment in advanced breast cancer: a prospective randomized trial of the Italian Oncology Group for Clinical Research. J Clin Oncol. 1992, 10 (6): 984-989.
Jakobsen A, Frederiksen PL, Moller KA, Andersen AP, Brincker H, Dombernowsky P, Hansen PV, Hesselius I, Kjaer M: Medroxyprogesterone acetate and prednisone in advanced breast cancer. A randomized trial. Eur J Cancer Clin Oncol. 1986, 22 (9): 1067-1072. 10.1016/0277-5379(86)90007-6.
Popiela T, Lucchi R, Giongo F: Methylprednisolone as palliative therapy for female terminal cancer patients. The Methylprednisolone Female Preterminal Cancer Study Group. Eur J Cancer Clin Oncol. 1989, 25 (12): 1823-1829. 10.1016/0277-5379(89)90354-4.
Tashiro H, Nomura Y: Mitomycin C, methotrexate, and vincristine with medroxyprogesterone acetate or prednisolone for doxorubicin resistant advanced breast cancer--a randomized control study. Anticancer Res. 1995, 15 (5B): 2229-2237.
Wolf J, Spear P, Yesner R, Patno ME: Nitrogen mustard and the steroid hormones in the treatment of inoperable bronchogenic carcinoma. Am J Med. 1960, 29: 1008-1016. 10.1016/0002-9343(60)90081-4.
Wolf J, Spear P, Yesner R, Patno ME: The Sex Hormones and Cortisone in the Treatment of Inoperable Bronchogenic Carcinoma. Biological activities of steroids in relation to cancer. Edited by: Pincus G, Vollmer EP. 1960, New York: Academic Press, 413-426.
Sander S, Nissen-Meyer R, Aakvaag A: Orchiectomy combined with cyproterone acetate or prednisone in the treatment of advanced prostatic carcinoma. A randomized clinical and endocrine study. Scand J Urol Nephrol. 1982, 16 (3): 193-197.
Meakin JW, Hayward JL, Panzarella T, Allt WE, Beale FA, Bulbrook RD, Bush RS, Clark RM, Fitzpatrick PJ, Hawkins NV, et al: Ovarian irradiation and prednisone following surgery and radiotherapy for carcinoma of the breast. Breast Cancer Res Treat. 1996, 37 (1): 11-19. 10.1007/BF01806627.
Rinehart JJ, Davidson S, Deshazo M, Cloud M, Busby L, Robert F: Phase l Trial of Dexamethasone (Dex), Carboplatin (C) and Gemcitabine (G) in Untreated Non-Small Cell Lung Cancer (NSCLC). Proceedings of ASCO. 2005, 23 (16S): 7111-
Rubens RD, Tinson CL, Coleman RE, Knight RK, Tong D, Winter PJ, North WR: Prednisolone improves the response to primary endocrine treatment for advanced breast cancer. Br J Cancer. 1988, 58 (5): 626-630.
Kristensen B, Ejlertsen B, Holmegaard SN, Krarup-Hansen A, Transbol I, Mouridsen H: Prednisolone in the treatment of severe malignant hypercalcaemia in metastatic breast cancer: a randomized study. J Intern Med. 1992, 232 (3): 237-245.
Tormey D, Gelman R, Falkson G: Prospective evaluation of rotating chemotherapy in advanced breast cancer. An Eastern Cooperative Oncology Group Trial. Am J Clin Oncol. 1983, 6 (1): 1-18.
Loprinzi CL, Kugler JW, Sloan JA, Mailliard JA, Krook JE, Wilwerding MB, Rowland KM, Camoriano JK, Novotny PJ, Christensen BJ: Randomized comparison of megestrol acetate versus dexamethasone versus fluoxymesterone for the treatment of cancer anorexia/cachexia. J Clin Oncol. 1999, 17 (10): 3299-3306.
Tombal B, Tourani J-M, Kizazi K, Culine S, Lotz J-P, Kaci M, Coppola F, Kahatt C, Weems G, Cvitkovic E: Randomized phase ll trial of irofulven (IROF) with or without prednisone in hormone -refractory prostate cancer (HRPC) patients (pts). Proceedings of ASCO. 2003, 22: 1636-
Sato N, Koeda K, Ikeda K, Kimura Y, Aoki K, Iwaya T, Akiyama Y, Ishida K, Saito K, Endo S: Randomized study of the benefits of preoperative corticosteroid administration on the postoperative morbidity and cytokine response in patients undergoing surgery for esophageal cancer. Ann Surg. 2002, 236 (2): 184-190. 10.1097/00000658-200208000-00006.
Bernhardt B, Nemunaitis JJ, Ebrahimi B, Cervera A, Birch R, Richards DA, Smith GB, Allerton JP, Henderson IC: The addition of prednisone (Pr) to the combination of docetaxel (T) and perifosine (P) decreases the severity of gastrointestinal (GI) toxicity. Proceedings of ASCO. 2006, 24 (18S): 13142-
Marini G, Murray S, Goldhirsch A, Gelber RD, Castiglione-Gertsch M, Price KN, Tattersall MH, Rudenstam CM, Collins J, Lindtner J, et al: The effect of adjuvant prednisone combined with CMF on patterns of relapse and occurrence of second malignancies in patients with breast cancer. International (Ludwig) Breast Cancer Study Group. Ann Oncol. 1996, 7 (3): 245-250.
Oncologic Drugs Advisory Committee, Fifty-Third Meeting, Center for Drug Evaluation and Research, Food and Drug Administration Bethesda, MD. 1997, 1-192. [http://www.fda.gov/ohrms/dockets/ac/97/transcpt/3289t2.pdf]
Mercer PM, Ebbs SR, Fraser SC, Coltart RS, Bates T: Trial of aminoglutethimide vs hydrocortisone as second-line hormone treatment of advanced breast cancer. Eur J Surg Oncol. 1993, 19 (3): 254-258.
Wander HE, Kleeberg UR, Essers U, Blossey HC, Nagel GA: Aminoglutethimide plus high-dose medroxyprogesterone acetate versus aminoglutethimide plus cortisone in therapy of metastasizing breast cancer. An AIO phase III study. Onkologie. 1987, 10 (5): 321-323.
Graham PH, Capp A, Delaney G, Goozee G, Hickey B, Turner S, Browne L, Milross C, Wirth A: A pilot randomised comparison of dexamethasone 96 mg vs 16 mg per day for malignant spinal-cord compression treated by radiotherapy: TROG 01.05 Superdex study. Clin Oncol (R Coll Radiol). 2006, 18 (1): 70-76.
Yano M, Taniguchi M, Tsujinaka T, Fujiwara Y, Yasuda T, Shiozaki H, Monden M: Is preoperative methylprednisolone beneficial for patients undergoing esophagectomy?. Hepatogastroenterology. 2005, 52 (62): 481-485.
Williams G, Asopa R, Abel PD, Smith C: Pituitary adrenal and gonadal endocrine suppression for the primary treatment of prostate cancer. Br J Urol. 1990, 65 (5): 504-508.
Tyrrell C: Liazal Versus Cyproterone Acetate (CPA) or Prednisone in Hormone-Resistant Prostate Cancer: Results of Two Clinical Trials. Annals of Oncology. 1996, 7 (Supplement 5): 57-
Mercadante SL, Berchovich M, Casuccio A, Fulfaro F, Mangione S: A prospective randomized study of corticosteroids as adjuvant drugs to opioids in advanced cancer patients. Am J Hosp Palliat Care. 2007, 24 (1): 13-19. 10.1177/1049909106295431.
Feuer DJ, Broadley KE: Systematic review and meta-analysis of corticosteroids for the resolution of malignant bowel obstruction in advanced gynaecological and gastrointestinal cancers. Systematic Review Steering Committee. Ann Oncol. 1999, 10 (9): 1035-1041. 10.1023/A:1008361102808.
Mass RE: Clinical Evaluation Of Oxylone (NSC-33001). Cancer Chemother Rep. 1964, 38: 49-60.
Moertel CG, Reitemeier RJ, Hahn RG, Blackburn CM: Fluorometholone (NSC-33001) As A Palliative In Advanced Gastrointestinal Carcinoma. Cancer Chemother Rep. 1964, 43: 25-27.
Johnson R, Bisel H, Andrews N, Wilson W, Rochlin D, Segaloff A, Krementz E, Aust J, Ansfield F: Phase l Clinical Study of 6α-Methylpregn-4-ene-3,11,20-trione (NSC-17256). Cancer Chemother Rep. 1966, 50 (9): 671-673.
Ramirez G, Weiss AJ, Rochlin DB, Bisel HF: Phase II study of 6 -methylpregn-4-ene-3,11,20-trione (NSC-17256). Cancer Chemother Rep. 1971, 55 (3): 265-268.
Bruera E, Roca E, Cedaro L, Carraro S, Chacon R: Action of oral methylprednisolone in terminal cancer patients: a prospective randomized double-blind study. Cancer Treat Rep. 1985, 69 (7–8): 751-754.
Postlethwait RW, Moseley V, McKee KT, Murdoch JH, McCord WM: ACTH and cortisone in advanced carcinoma of the digestive tract. Cancer. 1951, 4 (5): 984-987. 10.1002/1097-0142(195109)4:5<984::AID-CNCR2820040512>3.0.CO;2-B.
De Camp G: Corticosteroid therapy in bronchial carcinoma and other malignant tumors in the thorax. Munch Med Wochenschr. 1961, 103: 2026-2030.
Plengvanit U, Viranuvatti V: Treatment Of Primary Carcinoma Of The Liver With Nitrogen Mustard And Prednisolone: Report Of 51 Cases. Am J Gastroenterol. 1964, 42: 521-528.
Rinehart JJ: Randomized Phase ll Trial of Doxil With or Without Dexamethasone for Metastatic Hormone Refractory Prostate Cancer. ClinicalTrials.gov . [http://clinicaltrials.gov/show/NCT00176293]
Mouridsen H: Phase ll Randomized Second-Line Endocrine Therapy with AG/HC vs AG vs Low-Dose AG vs Low-Dose AG/HC in Patients with Advanced Breast Cancer EORTC-10861.
CellGenesys : Docetaxel in Combination with GVAX Vaccine Versus Docetaxel and Prednisone in Prostate Cancer Patients. ClinicalTrials.gov . [http://clinicaltrials.gov/show/NCT00133224]
Habib GS, Saliba WR: Tumor lysis syndrome after hydrocortisone treatment in metastatic melanoma: a case report and review of the literature. Am J Med Sci. 2002, 323 (3): 155-157. 10.1097/00000441-200203000-00007.
Chaudhuri PK, Das Gupta TK, Beattie CW, Walker MJ: Glucocorticoid-induced exacerbation of metastatic human melanoma. J Surg Oncol. 1982, 20 (1): 49-52. 10.1002/jso.2930200112.
Varella AD, Bandiera DC, de Amorim AR, Calvis LA, Santos IO, Escaleira N, Gentil F: Treatment of disseminated malignant melanoma with high-dose oral BCG. Cancer. 1981, 48 (6): 1353-1362. 10.1002/1097-0142(19810915)48:6<1353::AID-CNCR2820480617>3.0.CO;2-N.
Hayashi R, Hanyu N, Moriyama S: Efficacy of steroid therapy on liver metastasis of thymic carcinoid. Intern Med. 1994, 33 (1): 45-47. 10.2169/internalmedicine.33.45.
Omland H, Fossa SD: Spontaneous regression of cerebral and pulmonary metastases in renal cell carcinoma. Scand J Urol Nephrol. 1989, 23 (2): 159-160.
Tanaka M, Fukuda H, Higashi Y: A case of complete regression of metastatic renal cell carcinoma following corticosteroid treatment. Hinyokika Kiyo. 2003, 49 (4): 225-228.
Farber S, Downing V, Schwachman H, Toch R, Appleton R, Heald F, King JP, Feriozi D: The Action of ACTH and Cortisone on Children with Disseminated Cancer. Second Clinical ACTH Conference. Edited by: Mote JR. 1951, The Blakiston Company, 226-234.
Jadresic A, Pabst I, Lazo M: Do corticoids favour dissemination of breast cancer?. Lancet. 1963, 2: 306-307. 10.1016/S0140-6736(63)90215-0.
Dao T, Moore GE: Clinical observations of conditions which apparently enhance malignant cell survival. Surg Gynecol Obstet. 1961, 112: 191-195.
Pelner L: Host-tumor antagonism. XII. Possible effect of the cortisone drugs on the development of metastases in patients with carcinoma. J Am Geriatr Soc. 1959, 7 (5): 428-439.
Tomiak EM, Evans WK: The role of chemotherapy in invasive thymoma: a review of the literature and considerations for future clinical trials. Crit Rev Oncol Hematol. 1993, 15 (2): 113-124. 10.1016/1040-8428(93)90051-5.
A randomized trial of adjuvant combination chemotherapy with or without prednisone in premenopausal breast cancer patients with metastases in one to three axillary lymph nodes. Ludwig Breast Cancer Study Group. Cancer Res. 1985, 45 (9): 4454-4459.
Kemeny N, Conti JA, Cohen A, Campana P, Huang Y, Shi WJ, Botet J, Pulliam S, Bertino JR: Phase II study of hepatic arterial floxuridine, leucovorin, and dexamethasone for unresectable liver metastases from colorectal carcinoma. J Clin Oncol. 1994, 12 (11): 2288-2295.
Arisawa Y, Sutanto-Ward E, Fortunato L, Sigurdson ER: Hepatic artery dexamethasone infusion inhibits colorectal hepatic metastases: a regional antiangiogenic therapy. Ann Surg Oncol. 1995, 2 (2): 114-120. 10.1007/BF02303625.
Al-Habet SM, Rogers HJ: Methylprednisolone pharmacokinetics after intravenous and oral administration. Br J Clin Pharmacol. 1989, 27 (3): 285-290.
Leggas M, Kuo K, Cloud G, Li M, Wang H, Zhang R, Robert F, Rinehart JJ: Effects of Dexamethasone (Dex) Pretreatment on Toxicity and Efficacy of Carboplatin and Gemcitabine (Carb/Gem) in Patients with Non-Small Cell Lung Cancer (NSCLC). Proceedings of ASCO. 2007, 25 (18S): 18124-
Plowman PN: Glucocorticoids and prostate cancer in castrate men. J Clin Oncol. 1999, 17 (12): 3856-3860.
Minton MJ, Knight RK, Rubens RD, Hayward JL: Corticosteroids for elderly patients with breast cancer. Cancer. 1981, 48 (4): 883-887. 10.1002/1097-0142(19810815)48:4<883::AID-CNCR2820480404>3.0.CO;2-V.
Fossati R, Confalonieri C, Torri V, Ghislandi E, Penna A, Pistotti V, Tinazzi A, Liberati A: Cytotoxic and hormonal treatment for metastatic breast cancer: a systematic review of published randomized trials involving 31,510 women. J Clin Oncol. 1998, 16 (10): 3439-3460.
Axelrod L: Corticosteroid Therapy. Principles and Practice of Endocrinology. Edited by: Becker KL. 2001, Philadelphia: Lippincott Williams and Wilkins, 745-755. 3
Rinehart J, Keville L, Neidhart J, Wong L, DiNunno L, Kinney P, Aberle M, Tadlock L, Cloud G: Hematopoietic protection by dexamethasone or granulocyte-macrophage colony-stimulating factor (GM-CSF) in patients treated with carboplatin and ifosfamide. Am J Clin Oncol. 2003, 26 (5): 448-458. 10.1097/01.coc.0000027268.23258.7D.
Murray N, Osoba D, Shah A, Page R, Karsai H, Little C: Brief intensive chemotherapy for metastatic non-small-cell lung cancer: a phase II study of the weekly CODE regimen. J Natl Cancer Inst. 1991, 83 (3): 190-194. 10.1093/jnci/83.3.190.
Valabrega G, Montemurro F, Aglietta M: Trastuzumab: mechanism of action, resistance and future perspectives in HER2-overexpressing breast cancer. Ann Oncol. 2007
Nair MP, Schwartz SA: Immunomodulatory effects of corticosteroids on natural killer and antibody-dependent cellular cytotoxic activities of human lymphocytes. J Immunol. 1984, 132 (6): 2876-2882.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2407/8/84/prepub
Acknowledgements
I would like to thank Rob Hall for critically reviewing the manuscript. I would like to thank Kim Aslett, Christina Wallace and other librarians for their assistance. I would like to thank the libraries of the following institutions for their help: Sault Area Hospital, Windsor Regional Hospital, Northern Ontario School of Medicine, Wayne State University, Michigan State University, University of Windsor, University of Michigan and the NCI. I would like to thank Larry Stitt for the statistical analysis. I would like to thank Olga Karkalas and other translators for their work.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Electronic supplementary material
12885_2007_1022_MOESM1_ESM.doc
Additional file 1: Search strategies. Provides the search strategies for PubMed, EMBASE, the Cochrane Library (including ACP Journal Club) and CINAHL. (DOC 39 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Keith, B.D. Systematic review of the clinical effect of glucocorticoids on nonhematologic malignancy. BMC Cancer 8, 84 (2008). https://doi.org/10.1186/1471-2407-8-84
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2407-8-84