Abstract
Background
To assess progression-free survival (PFS) as the appropriate end-point for phase II trials for anaplastic gliomas (AGs) and to determine the impact of PFS on survival-based phase III trials.
Methods
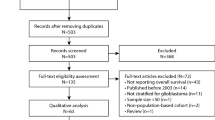
Combined data from 16 phase II studies (N = 529 patients) were analyzed to determine progression-free survival (PFS) at 6, 9, and 12 months and the impact of age, Karnofsky performance score (KPS), number of prior chemotherapies, and response to treatment on PFS.
Results
The specific chemotherapy used was the major effector of PFS at 6, 9, and 12 months. Age, KPS, treatment response rate, and number of prior chemotherapies did not affect PFS to the same extent. Hierarchical cluster analyses and linear least squares fitting of PFS9 v PFS12 demonstrated the existence of three therapeutic efficacy groups with PFS rates at 6, 9, and 12 months ranging from lowest (A) to highest (C). The PFS6 was 15% in group A and 41% in group C (p < .0001); the PFS12 was 9% in group A and 33% in group C (p < .0001). Further, 80% of patients at recurrence had a 23% likelihood that each chemotherapy would provide > 1 year of additional life.
Conclusion
Based on PFS rates at 6, 9, and 12 months for AG patients, a differential of 1.5 to 2 years is the norm and could invalidate overall survival as an end-point for phase III studies in patients with AG. PFS is a more reliable end-point because it reflects the true antitumor benefit of the chemotherapy.
Similar content being viewed by others
Background
Anaplastic gliomas (AGs) constitute a group of WHO grade III primary brain tumors that include anaplastic astrocytoma (AA), anaplastic oligodendroglioma, [1] anaplastic mixed oligoastrocytoma (AOA), and anaplastic ependymoma. [2–4] As a group, the incidence of these tumors is approximately 1.6/100,000, which translates into about 4400 patients who are diagnosed with the tumor yearly in the U.S. [5, 6]
AGs typically infiltrate (invade) adjacent brain. However, in patients with the different types of AG, chemotherapy agents show a discrepant ability to traverse the normal vasculature as well as tumor capillary beds and to achieve therapeutic levels in and surrounding infiltrating tumor cells. To date, most agents considered "active" in patients with these tumors are lipophilic alkylating agents such as BCNU (carmustine), CCNU (lomustine), procarbazine, and temozolomide. [7–21] While there has been much progress in the treatment of AG over the years, with the median survival time seen just a few years ago going from 13 to 19 months in patients treated with surgery and irradiation [22, 23] to 6.5 years in patients in a recent randomized trial of alpha-difluoromethylornithine (DFMO, eflornithine) plus procarbazine, CCNU, and vincristine (PCV) v PCV, [24] curative treatments with reduced regional and systemic toxicity are still very much needed.
However, one of the hindrances to the introduction of new agents for AGs, and in particular AAs and AOAs, into clinical use is that many of the phase II studies of single-agent therapy and drug combinations in patients with AAs and AOAs have shown a considerable disconnect between the percentage of patients whose disease responds to or stabilizes (i.e., does not progress) in response to treatment and the durability of the treatment response, defined as the time-to-tumor progression (TTP) or as progression-free survival (PFS). For example, complete response (CR), partial response (PR), minor response, and stable disease rates of 0% to 83% have been reported, with a median time to tumor progression (MTP) of 6 to 49 weeks and with only a modest correlation between the rates of response, stable disease, and MTP. [18, 25–37] Thus, it is difficult to draw firm conclusions from these studies with regard to the effectiveness of the treatment under study. On the basis of these and other observations, we believe that the PFS rate at a specified time point between 6 and 12 months provides a realistic time frame for trials evaluating agents for AG. That is, the use of PFS as the primary end-point in phase II trials has the advantage of enabling trials to be shorter in duration, plus PFS is a practical and achievable surrogate indicator of actual long-term prognosis. PFS rates at 6, 9, and 12 months (PFS6, PFS9, and PFS12) are also good end-points, both for drugs that cause tumor shrinkage and for those that just delay TTP.
We will demonstrate that PFS is a more realistic and accurate end-point than overall survival (OS) for chemotherapy trials of today's new agents in patients with mid- and high-grade gliomas. [24] In this report, we will also describe the value of PFS6, PFS9, and PFS12 and how these end-points might be applied so that the clinical development of effective new drugs and drug combinations can be accelerated.
Methods
To better define whether there would be any benefit to studying PFS6, PFS9, or PFS12 and to evaluate the impact of age, Karnofsky performance score (KPS), and number of prior chemotherapies on PFS, covariates typically associated with survival outcome, we collated a large retrospective database of patients with AA or AOA treated on phase II studies. Patients with anaplastic ependymoma were excluded because of the relative rarity of this tumor. Patients with AOs were also excluded because these tumors are relatively more sensitive to chemotherapy and radiation therapy, and thus these patients should be analyzed separately from those with AA or AOA.
Data in the database were obtained from the following sources: the same patient database used in an earlier study [38]; reports of single-agent therapy with imatinib (Gleevec) [39] or temozolomide [21, 40]; portions of randomized trials of interferon-beta v interferon-beta with isotretinoin [38, 41], carboplatin and isotretinoin [42], and carboplatin, 5-fluorouracil, and procarbazine [43]; a trial of DFMO performed at The University of Texas M. D. Anderson Cancer Center (UTMDACC) and the University of California San Francisco [37]; a published trial of temozolomide and marimastat [44], and the institutional database for a number of additional trials conducted at UTMDACC and generated by Data Management Services at UTMDACC from 1999 through 2004 [45]. The UTMDACC database consists of data from sequential phase II studies. Some study findings were published only in abstracts and others were from cooperative group studies. In all cases, the computer database was available for interrogation for these analyses. Aside from the number of previous chemotherapies, these studies had common eligibility criteria, and one of us [39] was an investigator in each study. The latter dataset was verified, to the extent possible, by (a) requiring that the tumor pathology be reviewed prior to the study by a UTMDACC neuropathologist; (b) using common MRI criteria for the determination of response and tumor progression [46]; (c) removing patients from the analysis with biopsy and/or strong radiological evidence of radiation necrosis [47–49]; (d) including only patients treated on phase II studies whose full prior treatments could be fully documented; (e) including only patients annotated evaluable in the database; and (f) including only patients for whom full follow up information was available. The entry requirements for all studies were also similar: KPSs of ≥ 60 at study entry, unequivocal radiographic evidence of recurrence (progression), age ≥ 16 years, absolute neutrophil count ≥ 1500, platelet count ≥ 125,000, and results of chemistry and liver function tests within 1.5 to 2.0 times the normal value, depending on the protocol. All patients had signed an IRB-approved consent form agreeing to a formal protocol treatment and/or the use of their computer-based record.
Results
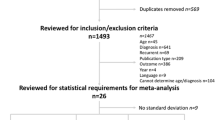
Data on patients from 16 phase II studies conducted between 1995 and 2004 were collected. A total of 529 patients were included in the database for analysis. For all studies and the MDACC database, complete and partial response were determined based on the brain MRI using the Macdonald criteria [46]. Comparison of the 16 therapy groups showed no differences among the groups in terms of age and the KPS (Table 1). Table 2 summarizes the mean, SEM, and range for the mean age, KPS, response (CR+PR) rates, and number of prior chemotherapy treatments for each treatment group from Table 1. In addition, t-tests for each covariate found no differences among the 16 protocols from the standpoint of patient age, KPS, treatment response, and number of prior chemotherapies.
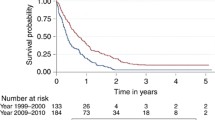
To better discriminate the PFS data in Table 1, we plotted PFS6 v PFS12, PFS6 v PFS9, and PFS9 v PFS12 to determine goodness of linear fit. The worst fit to the linear model was seen for PFS6 v PFS12 (r2 = .64), and the best fit to the linear model was seen for PFS9 v PFS12 (Fig. 1; r2 = .90). We then analyzed the PFS data at 6, 9, and 12 months together with age and KPS using hierarchical cluster analyses with complete linkage and Euclidean distances (Statistica for Windows, version 5.5). This analysis yielded three groups, which we designated A, B, and C, shown graphically in Figure 1. The respective protocol groups, the number of patients in the groups, and the respective weighted mean PFS6, PFS9, and PFS12 for groups A through C are summarized in Table 2. Of the 529 patients in the dataset, 20% were in Group A, 65% were in Group B, and 15% were in Group C.
From Table 3 and Figures 1 and 2, it appears that Group A is markedly inferior to groups B and C in terms of PFS. To test the statistical significance of this observation, we performed a Cox regression analysis using covariates of age, prior chemotherapy, and treatment group. KPS could not be used as a covariate in this analysis since time- and patient-coupled KPS data were incomplete. This analysis, the results of which are summarized in Table 4, showed that age at treatment was a significant factor (p = .006) but that membership in treatment groups B and C was a more significant factor, with treatment groups B and C superior to group A from the standpoint of PFS (p < .0001).
Discussion
What are the implications of this study for phase II and phase III chemotherapy trials? At one level, we wanted to define what represented a "good" outcome from the standpoint of PFS9 and PFS12. To that end, we were able to define an indicator of efficacy in a phase II trial in AG patients; we found that a therapy that produces a PFS6 of ≤15%, regardless of the number of prior chemotherapies, is not likely to be worth pursuing further. Of the remaining 80% of patients who made up groups B and C, PFS6 was similar for the two groups (37% vs. 41%); the PFS9 and PFS12 for the two groups, however, differed by 13% (25% vs. 38%) and 12% 21% vs. 33%). The difference between PFS9and PFS12 was only 4% for Group B and only 5% for Group C. Thus, for all practical purposes, we believe clinical trial investigators can easily set the PFS bar at 6 months or 9 months and be confident that this will distinguish inferior from adequate trial outcomes based on the values in Table 3.
From our own clinical experience and the experience of investigators in clinical phase II trials published over the years, the value of treatment response in determining the value of a new therapy for recurrent AGs remains problematic. Our current study supports that position, in that the use of the overall response rate, the historical phase II criterion, would have inadequately predicted the true benefit and limitations of many of the therapies analyzed in this study. This disconnect between the response rate and the durability of response (see Tables 1 and 2 and Fig. 1) is not a new concern for those conducting clinical trials in patients with high-grade gliomas. One reason for this disconnect is undoubtedly the limited antitumor activity of today's chemotherapy agents. Another reason proposed in the past is that the central nervous system does not rapidly remove dead glioma tumor cells. [50] Thus, the time before tumor cell kill can be visualized may be considerably delayed and lost in the process of a clinical follow up, unless meticulously sought. [51] This makes it difficult to pinpoint the actual rate or durability of response.
Furthermore, there is a mistaken belief that determining response is easier than determining tumor progression in patients with AG, but also that response is the only true indicator of drug effect for phase II trials. Historically, however, determining a response has frequently been more difficult than determining tumor progression (treatment failure). [49] This becomes even more of a problem, however, when pharmaceutical companies insist that patients not be entered into phase II trials until their initial therapy has failed, which for patients with AG could be the time it takes to develop postoperative gliosis or a radiation effect. Such a practice has the potential to lead to a disturbing false-positive response rate because the effectiveness of treatment is based on the resolution of postoperative changes and not the effects of treatment. While the same could be said for defining tumor progression in the face of radiation effects, the definition of therapeutic failure appears to be more reliable. [46, 52] Hence, it is the current belief of many clinical trial neuro-oncologists that PFS is a much better indicator of treatment efficacy than the response rate. Certainly it is our hope that future therapies will be so effective that complete responses will be seen regularly and the therapeutic bar will be raised even higher, but until that time, it is important to consider PFS a legitimate measure for studies of single agents and drug combinations for the purpose of community usage but also, in some cases, for marketing approval.
How treatment-defining phase III clinical chemotherapy trials for patients with malignant gliomas are designed and conducted is a concern. Currently, OS is considered the benchmark for assessing the benefit of new chemotherapy, radiotherapy, or chemoradiation regimens in phase III trials conducted in patients with glioblastomas (WHO grade 4). This end-point is reasonable and acceptable in this setting at this time, since, for the most part, the Kaplan-Meier probability of surviving declines exponentially and survival in patients treated with current agents minimally deviates from this expectation. In phase III trials in patients with AG, however, OS is arguably the wrong study end-point. This is because, as shown in Table 3, there are a number of chemotherapy treatments that can significantly prolong life after first tumor progression and thereby lengthen OS, independently of the phase III trial regimen being tested. For example, by extrapolating from Table 3, one could predict that 80% of patients in our phase II studies have, on average, a 23% (21% to 33%) chance of living more than 1 year for each treatment protocol they receive. How, then, might this impact the interpretation of a recent randomized phase III study of an effective agent?
To answer this question, we examined our findings from the current study of PFS in phase II studies in light of the results from the recent phase III randomized trial of DFMO-PCV v PCV alone for patients with AG tumors. [24] In that study, there was a marked difference in the median PFS between the two treatment arms, but there was far less of a difference in the median OS between the two treatment arms. [24] In particular, the median PFS was 71 months and the median OS was 76 months in the DFMO-PCV group, but the median PFS was only 38 months while the median OS was 61 months in the PCV group. We reviewed this study in May 2006 to determine how many patients had had disease progression and what treatment options they had then elected. We found that 46% of the DFMO-PCV patients and 41% of the PCV patients had been censored during the 13 years since study inception. Furthermore, among non-censored patients, we found that 34% of patients received an average of 1.6 chemotherapies after tumor progression, 22% underwent 1.1 further surgeries, 3% underwent 1.0 re-irradiation, and 15% of patients were treated with more than one modality. Thus, no matter how careful the randomization, one could not account prospectively for the fact that one group required more therapies at recurrence than did the other group. The fact that a number of contemporary phase II trials of chemotherapies for AGs produce substantial palliation (21% to 33% PFS12) means that OS as an end-point would not truly reflect the benefit of the primary phase III regimen. In the case of the DFMO-PCV trial discussed above, only 23 months (OS – PFS) of successful phase II chemotherapies would have been needed. In addition, in the cited example above, reoperation and repeat irradiation were also used after tumor progression.
For these reasons, we strongly question whether phase III studies with OS as the primary end-point can or should be conducted in patients with AGs at this time. We argue that OS as an end-point for phase III AG studies today is a flawed objective and that its use will result in new and effective regimens tested in phase III trials being judged ineffective (false negative) for the treatment of AG.
Conclusion
We conclude from our analysis that PFS is a much more valuable and reliable end-point for phase III studies than overall survival, because it reflects the true antitumor benefit of the chemotherapy being studied. Since the median survival of AG patients can range from 4 to 6 years, focusing on PFS in phase III studies would also allow studies to be performed and concluded in possibly half that time. It is hoped that this article will help to convince clinical trial investigators, the pharmaceutical industry, and government regulators to develop robust strategies that utilize PFS as the primary end-point in trials of much-needed therapies for patients with AGs.
References
Ren XR, Du QS, Huang YZ, Ao SZ, Mei L, Xiong WC: Regulation of CDC42 GTPase by proline-rich tyrosine kinase 2 interacting with PSGAP, a novel pleckstrin homology and Src homology 3 domain containing rhoGAP protein. J Cell Biol. 2001, 152 (5): 971-983. 10.1083/jcb.152.5.971.
Berger MS, Leibel SA, Bruner JM, Finlay JL, Levin VA: Primary Cerebral Tumors. Cancer in the Nervous System. Edited by: Levin VA. 2002, New York: Oxford University Press, 75-148. Second
Burger PC, Scheithauer BW, Vogel FS: Surgical Pathology of the Nervous System and its Coverings. 1991, New York: Churchill Livingstone, 3
Kleihues P, Louis DN, Scheithauer BW, Rorke LB, Reifenberger G, Burger PC, Cavenee WK: The WHO classification of tumors of the nervous system. J Neuropathol Exp Neurol. 2002, 61 (3): 215-225. discussion 226–219.
CBTRUS: Statistical Report: Primary Brain Tumors in the United States, 1995–1999. 2002, Central Brain Tumor Registry of the United States, 45-
Walker AE, Robins M, Weinfeld FD: Epidemiology of brain tumors: the national survey of intracranial neoplasms. Neurology. 1985, 35 (2): 219-226.
Baker SD, Wirth M, Statkevich P, Reidenberg P, Alton K, Sartorius S, Dugan M, Cutler D, Batra V, Rowinsky E: Absorption, metabolism and excretion of 14C-temozolomide in patients with advanced cancer. Proc Annu Meet Am Soc Clin Oncol. 1999, 5 (2): 309-317.
Brada M, Moore S, Judson I, Batra VJ, Quartey P, Dugan M: A phase I study of SCH 52365 (temozolomide) in adult patients with advanced cancer. Proc Annu Meet Am Soc Clin Oncol. 1995, 14: A1521-
Devineni D, Klein-Szanto A, Gallo JM: Uptake of temozolomide in a rat glioma model in the presence and absence of the angiogenesis inhibitor TNP-470. Cancer Research. 1996, 56 (9): 1983-1987.
Eckardt JR, Weiss GR, Burris HA, Rodriguez GI, Fields SM, Rinaldi DA, Drengler RL, Dugan MH, Batra VJ, Von Hoff DD: Phase I and pharmacokinetic trial of SCH52365 (temozolomide) given orally daily ×5 days. Proc Annu Meet Am Soc Clin Oncol. 1995, 14: A1579-
Hammond LA, Eckardt JR, Baker SD, Eckhardt SG, Dugan M, Forral K, Reidenberg P, Statkevich P, Weiss GR, Rinaldi DA, et al: Phase I and pharmacokinetic study of temozolomide on a daily-for-5-days schedule in patients with advanced solid malignancies. J Clin Oncol. 1999, 17 (8): 2604-2613.
Levin VA: Pharmacological principles of brain tumor chemotherapy. Adv Neurol. 1976, 15: 315-325.
Levin VA: Relationship of octanol/water partition coefficient and molecular weight to rat brain capillary permeability. J Med Chem. 1980, 23 (6): 682-684. 10.1021/jm00180a022.
Levin VA: Pharmacokinetics and CNS chemotherapy. Fundamentals of cancer chemotherapy. Edited by: Hellmann K, Carter SK. 1986, New York: McGraw-Hill, 28-
Levin VA, Crafts DC, Wilson CB, et al: Imidazole carboxamides: Relationship of lipophilicity to activity against intracerebral murine glioma 26 and preliminary phase II clinical trial of 5-(3,3-bis chlorethyl)-1-troazeno)-imidazole-4-carboxamide (NSC-82196) in primary and secondary brain tumors. Cancer Chemother Rep. 1975, 59: 107-
Levin VA, Kabra P: Effectiveness of the nitrosoureas as a function of their lipid solubility in the chemotherapy of experimental rat brain tumors. Cancer Chemother Rep – Part 1. 1974, 58 (6): 787-792.
Levin VA, Edwards MS, Wright DC, Seager ML, Schimberg TP, Townsend JJ, Wilson CB: Modified procarbazine, CCNU, and vincristine (PCV 3) combination chemotherapy in the treatment of malignant brain tumors. Cancer Treat Rep. 1980, 64 (2–3): 237-244.
Levin VA, Resser KJ, McGrath L, Vestnys P, Nutik S, Wilson CB: PCNU treatment for recurrent malignant gliomas. Cancer Treat Rep. 1984, 68 (7–8): 969-973.
Levin VA, Shapiro WR, Clancy TP, Oliverio VT: The uptake, distribution, and antitumor activity of 1-(2-chloroethyl)-3-cyclohexyl-1-nitrosourea in the murine glioma. Cancer Res. 1970, 30 (10): 2451-2455.
Patel M, McCully C, Godwin K, Balis F: Plasma and cerebrospinal fluid pharmacokinetics of temozolomide. Proc Annu Meet Am Soc Clin Oncol. 1995, 14: A1485-
Yung WK, Prados MD, Yaya-Tur R, Rosenfeld SS, Brada M, Friedman HS, Albright R, Olson J, Chang SM, O'Neill AM, et al: Multicenter phase II trial of temozolomide in patients with anaplastic astrocytoma or anaplastic oligoastrocytoma at first relapse. Temodal Brain Tumor Group. J Clin Oncol. 1999, 17 (9): 2762-2771.
Leibel SA, Sheline GE, Wara WM, Boldrey EB, Nielsen SL: The role of radiation therapy in the treatment of astrocytomas. Cancer. 1975, 35 (6): 1551-1557. 10.1002/1097-0142(197506)35:6<1551::AID-CNCR2820350612>3.0.CO;2-V.
Thomas D, Brada M, Stenning S: Randomized trial of procarbazine, lomustine, and vincristine in the adjuvant treatment of high-grade astrocytoma: A medical research council trial. J Clin Oncol. 2001, 19 (2): 509-518.
Levin VA, Hess KR, Choucair A, Flynn PJ, Jaeckle KA, Kyritsis AP, Yung WK, Prados MD, Bruner JM, Ictech S, et al: Phase III randomized study of postradiotherapy chemotherapy with combination alpha-difluoromethylornithine-PCV versus PCV for anaplastic gliomas. Clin Cancer Res. 2003, 9 (3): 981-990.
Elliott TE, Buckner JC, Cascino TL, Levitt R, O'Fallon JR, Scheithauer BW: Phase II study of ifosfamide with mesna in adult patients with recurrent diffuse astrocytoma. J Neuro-Oncol. 1991, 10 (1): 27-30. 10.1007/BF00151244.
Chamberlain MC, Prados MD, Silver P, Levin VA: A phase II trial of oral melphalan in recurrent primary brain tumors. Am J Clin Oncol. 1988, 11 (1): 52-54. 10.1097/00000421-198802000-00011.
Sexauer CL, Khan A, Burger PC, Krischer JP, van Eys J, Vats T, Ragab AH: Cisplatin in recurrent pediatric brain tumors. A POG Phase II study. A Pediatric Oncology Group Study. Cancer. 1985, 56 (7): 1497-1501. 10.1002/1097-0142(19851001)56:7<1497::AID-CNCR2820560703>3.0.CO;2-7.
Decker DA, Al Sarraf M, Kresge C, Austin D, Wilner HI: Phase II study of aziridinylbenzoquinone (AZQ: NSC-182986) in the treatment of malignant gliomas recurrent after radiation. preliminary report. J Neuro-Oncol. 1985, 3 (1): 19-21. 10.1007/BF00165167.
Schold SC, Mahaley MS, Vick NA, Friedman HS, Burger PC, DeLong ER, Albright RE, Bullard DE, Khandekar JD, Cairncross JG, et al: Phase II diaziquone-based chemotherapy trials in patients with anaplastic supratentorial astrocytic neoplasms. J Clin Oncol. 1987, 5 (3): 464-471.
Schold SC, Friedman HS, Bjornsson TD, Falletta JM: Treatment of patients with recurrent primary brain tumors with AZQ. Neurology. 1984, 34 (5): 615-619.
Rodriguez LA, Prados M, Silver P, Levin VA: Reevaluation of procarbazine for the treatment of recurrent malignant central nervous system tumors. Cancer. 1989, 64 (12): 2420-2423. 10.1002/1097-0142(19891215)64:12<2420::AID-CNCR2820641204>3.0.CO;2-B.
Chamberlain MC, Prados MD, Silver P, Levin VA: A phase I/II study of 24 hour intravenous AZQ in recurrent primary brain tumors. J Neurooncol. 1988, 6 (4): 319-323. 10.1007/BF00177426.
Yung WK, Simaga M, Levin VA: 13-cis-retinoic acid: a new and potentially effective agent for recurrent malignant astrocytomas (Meeting abstract). Fourth International Congress on Anti-cancer Chemotherapy, February 2–5, 1993, Paris, France. 1993, 117-
Yung WK, Prados M, Levin VA, Fetell MR, Bennett J, Mahaley MS, Salcman M, Etcubanas E: Intravenous recombinant interferon beta in patients with recurrent malignant gliomas: a phase I/II study. J Clin Oncol. 1991, 9 (11): 1945-1949.
Kaba SE, Kyritsis AP, Conrad C, Gleason MJ, Newman R, Levin VA, Yung WKA: The treatment of recurrent cerebral gliomas with all-trans-retinoic acid (tretinoin). J Neurooncology. 1997, 34 (2): 145-151. 10.1023/A:1005743707803.
Bertolone SJ, Baum ES, Krivit W, Hammond GD: A phase II study of cisplatin therapy in recurrent childhood brain tumors. A report from the Childrens Cancer Study Group. J Neurooncol. 1989, 7 (1): 5-11. 10.1007/BF00149372.
Levin VA, Prados MD, Yung WK, Gleason MJ, Ictech S, Malec M: Treatment of recurrent gliomas with eflornithine. J Natl Cancer Inst. 1992, 84 (18): 1432-1437. 10.1093/jnci/84.18.1432.
Wong ET, Hess KR, Gleason MJ, Jaeckle KA, Kyritsis AP, Prados MD, Levin VA, Yung WKA: Outcomes and prognostic factors in recurrent glioma patients enrolled onto phase II clinical trials. J Clin Oncol. 1999, 17 (8): 2572-2578.
Wen PY, Yung WKA, Lamborn K, Peng B, DeAngelis LM, Cloughesy T, Fink K, Gilbert M, Chang S, Junck L, et al: Phase I/II Study of Imatinib Mesylate (Gleevec; STI571) For Patients With Recurrent Malignant Gliomas and Meningiomas (NABTC 99-08). Neuro-oncol. 2004, 6 (4): 385-
Yung WK, Prados MD, Yaya-Tur R, Rosenfeld SS, Brada M, Friedman HS, Albright R, Olson J, Chang SM, O'Neill AM, et al: Multicenter phase II trial of temozolomide in patients with anaplastic astrocytoma or anaplastic oligoastrocytoma at first relapse. Temodal Brain Tumor Group. J Clin Oncol. 1999, 17 (9): 2762-2771.
Yung WK, Levin VA, Kyritsis A, Jaeckle K, Winn R, Baidas S, Martuza R, Vaickus L: Phase II study of rhIFN-beta +/- cRA in recurrent gliomas. Proc Annu Meet Am Soc Clin Oncol. 1995, 14: A288-
Kunschner LJ, Yung WKA, Levin VA, Jaeckle KA: Carboplatin and 13-cis-retinoic acid for recurrent glioblastoma multiforme. Neuro-Oncology. 1999, 1: 320-
Flowers A, Gleason MJ, Levin VA, Yung WKA: Combination chemotherapy with carboplatin, 5-fluorouracil, and procarbazine for recurrent malignant gliomas. Proc Annu Meet Am Assoc Cancer Res. 1993, 12: 180-
Groves MD, Puduvalli VK, Conrad CA, Gilbert MR, Yung WK, Jaeckle K, Liu V, Hess KR, Aldape KD, Levin VA: Phase II trial of temozolomide plus marimastat for recurrent anaplastic gliomas: A relationship among efficacy, joint toxicity and anticonvulsant status. J Neurooncol. 2006, 80 (1): 83-90. 10.1007/s11060-006-9160-y.
MDACC: The University of Texas M. D. Anderson Cancer Center Brain Tumor Center 1991–2004 database search of phase II studies of patients with anaplastic astrocytoma and oligoastrocytoma. Houston, TX: The University of Texas M. D. Anderson Cancer Center Brain Tumor Center; 1991–2004 database search of phase II studies of patients with anaplastic astrocytoma and oligoastrocytoma. 2004
Macdonald DR, Cascino TL, Schold SC, Cairncross JG: Response criteria for phase II studies of supratentorial malignant glioma. J Clin Oncol. 1990, 8 (7): 1277-1280.
Van Tassel P, Bruner JM, Maor MH, Leeds NE, Gleason MJ, Yung WK, Levin VA: MR of toxic effects of accelerated fractionation radiation therapy and carboplatin chemotherapy for malignant gliomas. AJNR Am J Neuroradiol. 1995, 16 (4): 715-726.
Wong ET, Jackson EF, Hess KR, Schomer DF, Hazle JD, Kyritsis AP, Jaeckle KA, Yung WK, Levin VA, Leeds NE: Correlation between dynamic MRI and outcome in patients with malignant gliomas. Neurology. 1998, 50 (3): 777-781.
Kumar AJ, Leeds NE, Fuller GN, Van Tassel P, Maor MH, Sawaya RE, Levin VA: Malignant gliomas: MR imaging spectrum of radiation therapy- and chemotherapy-induced necrosis of the brain after treatment. Radiology. 2000, 217 (2): 377-384.
Rosenblum MK, Knebel KD, Vasquez DA, Wilson CB: Brain-tumor therapy. Quantitative analysis using a model system. J Neurosurg. 1977, 46 (2): 145-154.
Murovic J, Turowski K, Wilson CB, Hoshino T, Levin V: Computerized tomography in the prognosis of malignant cerebral gliomas. J Neurosurg. 1986, 65 (6): 799-806.
Levin VA, Crafts DC, Norman DM, Hoffer PB, Spire JP, Wilson CB: Criteria for evaluating patients undergoing chemotherapy for malignant brain tumors. J Neurosurg. 1977, 47 (3): 329-335.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2407/7/106/prepub
Acknowledgements
We would like to thank Beth Notzon for editorial assistance and suggestions and Melissa McLane for manuscript preparation. We also wish to thank the Alan Gold Memorial Fund for partial support of this study. Parts of this paper were presented at the 42nd Annual Meeting of the American Society of Clinical Oncology, Atlanta, GA, June 5, 2006.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
VAL conceived of the study, performed some of the statistical analyses, and wrote the paper. SI collated the datasets and verified the MDACC internal database to the extent that patients or their families were contacted for long-tem follow up status. KRH proposed statistical approaches and computed some of the analyses and provided editorial comments regarding their interpretation and figure presentations. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Levin, V.A., Ictech, S. & Hess, K.R. Impact of phase II trials with progression-free survival as end-points on survival-based phase III studies in patients with anaplastic gliomas. BMC Cancer 7, 106 (2007). https://doi.org/10.1186/1471-2407-7-106
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2407-7-106