Abstract
Background
There are two dimensions of quality of maternity care, namely quality of health outcomes and quality as perceived by clients. The feasibility of using clinical audit to assess and improve the quality of maternity care as perceived by women was studied in Malawi.
Objective
We sought to (a) establish standards for women friendly care and (b) explore attitudinal barriers which could impede the proper implementation of clinical audit.
Methods
We used evidence from Malawi national guidelines and World Health Organisation manuals to establish local standards for women friendly care in three districts. We equally conducted a survey of health care providers to explore their attitudes towards criterion based audit.
Results
The standards addressed different aspects of care given to women in maternity units, namely (i) reception, (ii) attitudes towards women, (iii) respect for culture, (iv) respect for women, (v) waiting time, (vi) enabling environment, (vii) provision of information, (viii) individualised care, (ix) provision of skilled attendance at birth and emergency obstetric care, (x) confidentiality, and (xi) proper management of patient information. The health providers in Malawi generally held a favourable attitude towards clinical audit: 100.0% (54/54) agreed that criterion based audit will improve the quality of care and 92.6% believed that clinical audit is a good educational tool. However, there are concerns that criterion based audit would create a feeling of blame among providers (35.2%), and that manager would use clinical audit to identify and punish providers who fail to meet standards (27.8%).
Conclusion
Developing standards of maternity care that are acceptable to, and valued by, women requires consideration of both the research evidence and cultural values. Clinical audit is acceptable to health professionals in Malawi although there are concerns about its negative implications to the providers.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
There are two broad dimensions of quality of maternity care, namely quality of health outcomes and quality as experienced by women receiving the care [1]. Both dimensions are crucial in measuring and improving the quality of care which in turn affects utilisation of maternal health services. In some settings women's experience of care may be more important than the health outcomes because childbirth is a culturally and emotionally sensitive area [2]. This is particularly true since most users of maternity care are healthy women who need only basic care, although some users will develop conditions requiring a higher level of care [3].
There are many tools used to improve the quality of care in maternity units. These include maternal death audit, criterion-based audit, training, dissemination of practice guidelines, plan-do-study-act (PDSA) cycles, tools for process description (client flow analysis, process mapping, and cause-effect analysis), tools for data collection (direct observation, exit interviews, and focus group discussion), tools for collaborative work (nominal group technique, facilitative supervision, force-field analysis, benchmarking, and SWOT analysis), and combined models involving a combination of these tools [4–11].
Criterion-based audit (also called clinical audit) is a well known approach for improving the quality of maternity care. It is strongly supported by expert opinion as well as national and international organisations including the World Health Organisation (WHO) and the National Institute of Clinical Excellence (NICE) in the United Kingdom [2, 12]. NICE defines audit as: "A quality improvement process that seeks to improve patient care and outcomes through systematic review of care against explicit criteria and implementation of change. Aspects of structure, processes, and outcomes of care are selected and systematically evaluated against explicit criteria. Where indicated, changes are implemented at individual, team, or service level and further monitoring is used to confirm improvement in healthcare delivery" [12].
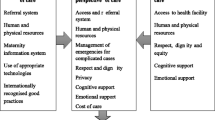
The five classic steps of the clinical audit cycle are presented in Figure 1. The first step is the development of standards. Traditionally standards have been developed by systematic reviews to identify sets of criteria that constitute optimal care. Once standards have been developed, actual practice is measured and compared with standards (best practice). Gaps in current practice are identified, recommendations are made and implemented, and progress is evaluated
Previous studies on criterion-based audit in maternity units have focused on improving the outcomes of emergency obstetric complications, ignoring quality as perceived by clients [13–15]. Criterion based audit for emergency obstetric complications has just recently been introduced in a few developing countries, including Uganda, Ghana and Jamaica [13–15]. To the best of our knowledge there are no published studies on the use of criterion based audit to improve women friendly care in a developing country setting.
Developing standards for women-friendly care is complex because (a) acceptable and valued behaviour may not be documented and (b) cultural values vary between countries or ethnic groups. Therefore systematic reviews may not capture what women consider good quality of care. This is particularly challenging in settings were traditional values strongly shape how quality of care is perceived by clients. Unfortunately this important area has been given very little attention especially in developing countries. The high maternal mortality in resource-limited settings is partly due to the poor attitudes of health providers which lead to reduced utilisation of maternity care services [16].
As part of a collaborative programme to reduce maternal mortality in Malawi, we sought to introduce criterion based audit to improve women friendly care in maternity units. This paper describes how standards for women friendly care were developed in Malawi, and attitudes of health care providers that could influence the implementation of criterion based audit.
Methods
We developed standards for women friendly care in three districts (Salima, Kasungu, Lilongwe) in the Central Region of Malawi. The three districts have a population of 2,812,183 people with 73 health facilities (9 hospitals and 64 health centres). Standards for women friendly care were established and refined during three workshops that brought together participants from the three districts. This study was approved by the Reproductive Health Unit of the Malawi Ministry of Health.
Establishing standards for women friendly care
Workshop 1: Establish standards for women friendly care
We used evidence from existing guidelines, namely Malawi national guidelines and WHO manuals [17, 18]. Where necessary this was supplemented by evidence from the Cochrane database, standard textbooks and articles from peer-reviewed journals. Local standards were established during a workshop that brought together 32 participants including maternal health experts, policy makers and women's group representatives from three districts. Reproductive Health Unit of the Ministry of Health and all hospitals in the three districts were represented. The workshop was facilitated by two UK based experts who have several years of experience in sub-Saharan Africa. The participants referred to relevant publications on women friendly care throughout the standard development process. The standards were agreed by simple consensus and where there was disagreement, they refer to the WHO manuals and National guidelines. For most participants the concept of standards of care was new. The participants discussed how standards are derived and how they are 'translated' for use by stating a clear objective and working out the structure, process and outcome criteria for each objective. The participants worked through this process during facilitated (small) group work. The participants discussed lively and debated openly on subjects such as: what is feasible in our own setting, what is the Ministry of Health policy, what is current evidence based/best practice? At the end of this two day workshop, the participants agreed on eleven objectives and developed the structure, process and outcome criteria for each objective.
Workshop 2: Review and finalise the standards initially developed
The second workshop brought together 62 participants from health centres, hospitals, Reproductive Health Unit of the Ministry of Health and women's group representatives from the three districts. The participants reviewed the standards developed during the first workshop and agreed on a final list of criteria. During this review process, the participants considered evidence from research synthesis, relevance to the three districts and cultural values. The standards consist of 136 criteria (Table 1).
Workshop 3: Select criteria to audit
The third workshop brought together 60 participants. From the list 136 criteria, 14 criteria were selected to be audited within the next six months in order to assess and improve women friendly care in maternity units in the three districts.
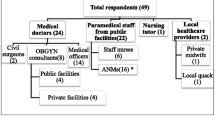
A survey of providers' attitudes towards criterion based audit
In order to assess attitudinal barriers that could impede the proper implementation of criterion-based audit, we conducted a survey of health care providers in the three districts (Salima, Kasungu, Lilongwe) of Malawi. We carried out this survey during a quality improvement workshop that brought together 54 participants from 9 hospitals and 18 health centres in three districts of Malawi. We collected data using an anonymous, self-administered questionnaire after verbal informed consent. Part one of the questionnaire consisted of seven "Yes or No" questions. Part two consisted of two open ended questions: first question was on the perceived challenges of implementing criterion based audit and second question was on the possible ways of overcoming the challenges. We entered and analysed the data with the Statistical Package for Social Sciences (SPSS) software programme (version 14.0, Chicago, IL, USA).
Results
Agreed standards for women friendly care
The standards developed for women friendly care consisted of eleven objectives, each with structure, process and outcome criteria (Table 1). The eleven objectives addressed different aspects of care given to women in maternity units: (i) reception, (ii) attitude towards women, (iii) respect for culture, (iv) respect for women, (v) waiting time, (vi) enabling environment, (vii) provision of information, (viii) individualised care, (ix) provision of skilled attendance at birth and emergency obstetric care, (x) confidentiality, and (xi) proper management of patient information.
Criteria selected to audit in the first six months
Fourteen criteria were selected to be audited in the next six months (Table 2). The selection was based on perceived deficiencies of women friendly care in maternity units. The criteria addressed different aspects of care such as greetings, self-introduction, companionship during labour, privacy, cleanliness, provision of basic facilities (e.g. bathroom, toilets), birthing positions, communication skills, respect for women, and client satisfaction.
Attitudes of health professionals towards criterion based audit
The health professionals generally held a favourable attitude towards criterion based audit: 100.0% (54/54) believe that clinical audit and feedback will improve the quality of care and 92.6% believe that audit and feedback is a good educational tool. However, there were concerns that audit and feedback would create a feeling of blame among providers (35.2%), manager would use audit to identify and punish providers who fail to meet standards (27.8%), audit and feedback could not be done routinely because it is time-consuming (13.0%), and the potential role of audit in reducing health care costs was questioned (see Table 3).
Discussion
This article describes the development of standards for women friendly care and the attitudes of health professionals towards criterion based audit in Malawi. A multidisciplinary team developed standards taking into consideration evidence from research synthesis and cultural values. Standards for obstetric complications address health outcomes while standards for women friendly care address women satisfaction in the care they receive [7]. Although client perception and provider perception are usually complementary, there are situations were the two perceptions can be antagonistic [18]. Optimal standards for women friendly care are those that are valued by women, and yet do not oppose evidence-based practice as perceived by health professionals. Traditionally, standards have been developed by a panel of experts and then implemented by a multidisciplinary team [13]. In obstetrics, the panel of experts is often made up of obstetricians while midwives who are usually excluded from the early stages of criterion based audit [15]. We involved all grades of health professionals (including midwives) from the very beginning of standards development process, and we hope that this will promote ownership and sustainability. We equally involved managers and policy-makers from the first step of criterion based audit, and we hope that this will facilitate the implementation of recommendations that require extra resources (e.g. finance and staff) and approval of hierarchy.
The criteria developed for women friendly care have some limitations. The list of agreed criteria is long and it might not be feasible to audit all the criteria simultaneously. Some authors have suggested that the criteria be limited to a short list that can easily be audited [4]. The participants agreed that the long list be maintained for reference, and that the criteria to be audited should be selected based on their relevance and level of priority. Alternatively the providers could audit each objective in turn until all the objectives have been audited. The participants also noted that some criteria appear under two or more objectives, e.g. greeting the client. Nevertheless they agreed that this was acceptable since the criteria address different objectives. In addition some criteria were agreed were not based on evidence (e.g. greeting) but on cultural norms and values.
Conclusion
A survey of the health professionals in Malawi showed that they held a favourable opinion about clinical audit. However there are some areas of concerns that should not be overlooked. For instance a third of providers believe that clinical audit will create a feeling of blame among providers who fail to meet standards, and more than a quarter believe that managers will use clinical audit to identify and punish health care providers. Some challenges identified by health care providers that could hinder the implementation of standards include shortage of staff, high workload and inadequate knowledge and skills. Many of the providers surveyed suggested some possible solutions: active involvement of managers in criterion based audit, and making it crystal clear that information from audit will not be used as a basis of disciplinary sanctions.
This paper describes the first step of a clinical audit cycle: establishing standards for women friendly care. The paper also explores attitudinal barriers which could impede effective implementation of clinical audit. Developing standards is a very crucial step that lays the foundation for the remaining steps of a clinical audit cycle. A successful completion of the next steps will determine whether criterion based audit can improve women friendly care in health facilities in resource-limited countries. Our plan is to follow up and monitor the implementation of these standards using the before-and-after study design. The major challenge will be to change current practice as other authors have reported that it is easy to change knowledge and skills, but very difficult to change clinical practice [19].
References
Pittrof R, Campbell OM, Filippi VG: What is quality in maternity care? An international perspective. Acta Obstet Gynecol Scand. 2002, 81: 277-283. 10.1034/j.1600-0412.2002.810401.x.
Kroposki M, Alexander JW: Correlation among client satisfaction, nursing perception of outcomes, and organizational variables. Home Healthc Nurse. 2006, 24: 87-94. 10.1097/00004045-200602000-00006.
Hulton AL, Mathews Z, Stones RW: A framework for the evaluation of quality of care in maternity services. Southampton: University of Southampton, 2000. (Accessed on November 12, 2007), [http://www.scocstats.soton.ac.uk/choices]
World Health Organisation: Beyond the Numbers: Reviewing Maternal Deaths and Complications to Make Pregnancy Safer. 2004, Geneva: Department of Reproductive Health and Research, WHO
Frederick L, Kallal T, Krook H: Quality through metrics. Qual Assur. 1999, 7: 5-16.
Lynam PF, Smith T, Dwyer J: Client flow analysis: a practical management technique for outpatient clinic settings. Int J Qual Health Care. 1994, 6: 179-186.
Speroff T, O'Connor GT: Study designs for PDSA quality improvement research. Qual Manag Health Care. 2004, 13: 17-32.
Sullivan TM, Sophia N, Maung C: Using evidence to improve reproductive health quality along the Thailand-Burma border. Disasters. 2004, 28: 255-268. 10.1111/j.0361-3666.2004.00257.x.
Qian X, Smith H, Zhou L, Liang J, Garner P: Evidence based obstetrics in four hospitals in China: an observational study to explore clinical practice, women's preferences and provider's views. BMC Pregnancy and Childbirth. 2001, 1: 1-10.1186/1471-2393-1-1.
Wang CC, Wang Y, Zhang K, Fang J, Liu W, Luo S, Tang S, Wang S, Li V: Reproductive health indicators for China's rural areas. Soc Sci Med. 2003, 57: 217-225. 10.1016/S0277-9536(02)00341-6.
Schieber BA: Quetzaltenango Maternal and neonatal health project: lessons learned in Mothercare Country project description 1989–1993: 33–38. Arlington: MotherCare. 1994
National Institute for Clinical Excellence: Principles for Best Practice in Clinical Audit. 2002, Abingdon: Radcliffe Medical Press
Graham W, Wagaarachchi P, Penney G, McCaw-Binns A, Yeboah Antwi K, Hall MH: Criteria for clinical audit of the quality of hospital-based obstetric care in developing countries. Bull World Health Organ. 2000, 78: 614-620.
Wagaarachchi PT, Graham WJ, Penney GC, McCaw-Binns A, Yeboah Antwi K, Hall MH: Holding up a mirror: changing obstetric practice through criterion-based clinical audit in developing countries. Int Gynecol Obstet. 2001, 74: 119-130. 10.1016/S0020-7292(01)00427-1.
Weeks AD, Alia G, Ononge S, Mutungi A, Otolorin EO, Mirembe FM: Introducing criteria based audit into Ugandan maternity units. BMJ. 2003, 327: 1329-1331. 10.1136/bmj.327.7427.1329.
Say L, Raine R: A systematic review of inequalities in the use of maternal health care in developing countries: examining the scale of the problem and the importance of context. Bull World Health Organ. 2007, 85: 812-819.
Ministry of Health and Population (Malawi), JHPIEGO: Malawi National Reproductive Health Services Delivery Guidelines. 2001, Lilongwe: Ministry of Health and Population, Malawi
World Health Organisation: Integrated Management of Pregnancy and Childbirth series (IMPAC). 2005, Geneva: WHO, (retrieved April 20, 2007), [http://www.euro.who.int/pregnancy/esscare/20051103_3?language=german]
Gülmezoglu AM, Langer A, Piaggio G, Lumbiganon P, Villar J, Grimshaw J: Cluster randomised trial of an active, multifaceted educational intervention based on the WHO Reproductive Health Library to improve obstetric practices. BJOG. 2007, 114 (1): 16-23. 10.1111/j.1471-0528.2006.01091.x.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2393/8/28/prepub
Acknowledgements
We wish to thank the Health Foundation for the financial support for this study. We are also very grateful for Prof Justus Hofmeyr and Prof Robert Pattinson for their comments given during the peer-review process.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
EJK conceived the topic, collected the data, prepared and finalised all versions of the manuscript. NvdB reviewed the manuscript for intellectual content. All authors read and approved the final manuscript. EJK is the guarantor.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Kongnyuy, E.J., van den Broek, N. Criteria for clinical audit of women friendly care and providers' perception in Malawi. BMC Pregnancy Childbirth 8, 28 (2008). https://doi.org/10.1186/1471-2393-8-28
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2393-8-28