Abstract
Background
Epidermal nevi (EN) represent benign congenital skin lesions following the lines of Blaschko. They result from genetic mosaicism, and activating FGFR3 and PIK3CA mutations have been implicated.
Case presentation
We report a female patient with a systemic keratinocytic nevus also involving the oral mucosa. Molecular genetic analysis revealed a mosaicism of the FGFR3 hotspot mutation R248C in the EN lesions of the skin and of the oral mucosa. The detection of the R248C mutation in a proportion of blood leukocytes and a slight scoliosis suggest an EN syndrome.
Conclusions
Our results show that activating FGFR3 mutations can also affect the oral mucosa and that extracutaneous manifestations of EN syndrome can be subtle. We highlight the theoretical risk of the patient having an offspring with thanatophoric dysplasia as gonadal mosaicism for the R248C mutation cannot be excluded.
Similar content being viewed by others
Background
Epidermal nevi (EN) are benign hamartomas of the skin arising from the embryonic ectoderm. Depending on the involved components of the epidermis, EN are further divided into organoid and non-organoid (keratinocytic) types [1]. They are usually present at birth or develop during the first years of life, and their incidence is estimated to be 1-3 per 1000 live births [2]. Keratinocytic nevi typically follow the lines of Blaschko. Systemic keratinocytic nevi are characterized by an extensive involvement of large skin areas and may be associated with skeletal, cerebral or ocular abnormalities, resulting in various types of EN syndromes [1, 2]. EN represent genetic mosaicism of the skin and activating FGFR3 (Fibroblast Growth Factor Receptor 3) and PIK3CA point mutations have recently been identified in keratinocytic nevi [3–6].
We report a patient with systemic EN associated with a slight scoliosis, who displayed mosaicism of the R248C FGFR3 mutation in epidermis, oral mucosa and blood leukocytes.
Case presentation
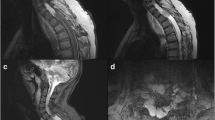
A 17-year old girl was referred with widespread EN (Figure 1 A+B). She was otherwise healthy apart from a tendency to back pain. Her parents recalled the first appearance of the EN when she was 4 months old. The EN initially presented as hyperpigmented linear streaks which gradually increased in size and thickness, becoming more elevated and verrucous. The brown, papillomatous and velvety EN followed the lines of Blaschko, with streaks and whorls on her body stopping abruptly at the ventral midline. The EN extended to her neck, scalp and extremities and was present on her face (Figure 2). She had intraoral mammilated lesions inside her lower lip (Figure 3) and at the buccal mucosa close to her oral angles. Laterally at the hard palate she had cobblestone-like thickening of the mucosa. She did not show any dysmorphic features and her face, trunk and extremities appeared symmetric with normal proportions, although a radiologic examination of the spine revealed a minimal thoracic scoliosis of 5 degrees. An eye examination was unremarkable and neurological examination was normal.
After informed consent of the patient and her parents, a 4 mm punch biopsy was taken from the chest. On histological examination, the biopsy showed a slightly papillomatous surface with non-specific laminated hyperkeratosis and acanthosis, typical of EN.
The patient was diagnosed with a bilateral, systemic keratinocytic nevus of the non-epidermolytic subtype. Maceration in the intertriginous areas was troublesome, but repeated laser (carbondioxide and Nd:YAG) treatments were without great success, as the skin lesions either relapsed or formed disfiguring scars.
Genetic analysis
Skin biopsies were taken from the EN on the abdomen and from adjacent normal skin after informed consent of the patient according to the guidelines of the local ethics committee and the Declaration of Helsinki. Separate fibroblast cultures were established from these biopsies. DNA was extracted directly from the skin biopsies as well as from cultured fibroblasts. In addition, formalin-fixed paraffin-embedded biopsy material, blood leukocytes, buccal brushings from lesional mucosa, scalp hair roots, and urothelial cells from urine sediment were available for analysis (Table 1). DNA was extracted from these tissues and cells using standard protocols. FGFR3 and PIK3CA mutations were analyzed using SNaPshot® assays as described previously [6, 7]. We identified the FGFR3 hotspot mutation R248C in EN tissue, but not in the adjacent normal skin (Figure 4). The R248C mutation was also detected in the EN tissue of the buccal mucosa harvested by buccal brushings. In contrast, the R248C mutation was not found in cultured fibroblasts from either affected or normal skin, nor in hair roots from affected skin of the scalp or in the urothelial cells. No mutations in the PIK3CA gene were found in any of the tissue samples.
Immunohistochemical staining of the EN tissue with FGFR3 antibody (Santa Cruz Biotechnology, Santa Cruz, USA) revealed expression of FGFR3 protein in the complete epidermal layer, but the staining intensity was comparable with a normal skin control.
The results indicate that the systemic keratinocytic nevus syndrome in the present patient is caused by mosaicism of the R248C FGFR3 mutation. This mosaicism has extended to the oral mucosa, and caused intraoral lesions. The genetic mosaicism can be limited to the epidermis, but may also extend to other tissues, resulting in EN syndromes [1, 2]. The proportion of EN patients with additional abnormalities of other organ systems is not known, and may vary depending on the different subtypes of EN. One comprehensive study identified an EN syndrome in 33% of 119 EN patients [8].
In keratinocytic nevi, activating point mutations in FGFR3 and PIK3CA genes have been identified in about 40% of patients [5, 6]. Interestingly, the mutational spectrum is restricted to hotspots, including R248C for FGFR3 and E545G for PIK3CA. The same mutations have been identified in sporadic malignant tumors, and confer oncogenic properties to cells in vitro [9, 10]. A non-mosaic constitutional R248C FGFR3 mutation causes thanatophoric dysplasia, a typically lethal skeletal dysplasia [11]. Obviously, surviving patients with the R248C FGFR3 mutation must be mosaics [12].
FGFR3 and PIK3CA mutations have also been identified in seborrheic keratoses which are benign epidermal skin tumors arising in adult patients with an increasing age-related incidence [5, 13–15]. Although the identified FGFR3 and PIK3CA mutations are oncogenic [10, 16, 17] and can activate downstream signalling pathways [18, 19], neither EN nor seborrheic keratoses bear a significant risk of malignant transformation.
In the patient of this case report, the R248C FGFR3 hotspot mutation was identified in the EN tissue of the skin and buccal mucosa (ectoderm) as well as a substantial proportion of blood leukocytes (mesoderm). With the involvement of two embryologic tissues, one might conclude that the mutation had happened at a very early stage, in a cell whose descendant population included skin and hematogenous precursor cells. The early occurrence of the mutation might be the reason for the widespread skin involvement.
To the best of our knowledge, we could show for the first time that the mosaic FGFR3 mutation can be associated with intraoral EN lesions, an otherwise uncommon observation [20]. The wildtype sequence of unaffected skin, hair roots and cultured fibroblasts in our patient confirms that the R248C mutation occurred in a mosaic form restricted to the epithelium and absent from the stromal component of skin. We propose that this case represents an EN syndrome, given the presence of the mutation in blood leukocytes indicating bone marrow involvement. Even her slight scoliosis may be part of the syndrome, although the finding could be coincidental and independent from the mosaicism. Hitherto the R248C FGFR3 mutation has been identified in two cases of an EN syndrome: - one with facial dysmorphism, and the other patient with cerebral involvement [21, 22]. A preliminary designation of "FGFR3 EN syndrome" has been proposed, while acknowledging that a genetic heterogeneity may underlie the clinical phenotype of this syndrome [1, 22]. For patients with extensive EN, a work-up for EN syndrome is indicated even without obvious extracutaneous features, as in our case.
Furthermore, it is important to be aware that these patients may have a predisposition towards malignancies of internal organs, especially low grade urothelial carcinomas [23–25]. As yet, there has been no report identifying FGFR3 mutations in a patient with EN associated with urothelial cancer or other malignancies [26]. However, FGFR3 mutations are involved in the pathogenesis of bladder tumors, cervix carcinoma, and multiple myeloma [9, 27]. The risk for the present patient is difficult to assess, although the absence of the FGFR3 mutation in urothelial cells suggests that at least for bladder cancer, it may be low. The risk for malignant transformation of an EN lesion (e.g., basal cell carcinoma or squamous cell carcinoma) appears likewise to be low, although occasional incidences have been reported [28–30].
If the FGFR3 mosaicism involves the gonad, our patient is at risk of having offspring with thanatophoric dysplasia. There is precedent for this, in a female patient with extensive mosaicism of the R248C FGFR3 mutation, including widespread acanthosis nigricans of the skin and skeletal dysplasia [31].
Conclusions
We show that a mosaicism of the R248C FGFR3 mutation can cause a systemic EN with involvement of the oral mucosa. For patients with extensive EN, a work-up for "EN syndrome" is indicated, as extracutaneous manifestations of the EN syndrome can be subtle. As gonadal mosaicism for the R248C FGFR3 mutation cannot be entirely excluded, a risk of having offspring with thanatophoric dysplasia exists. Prenatal diagnosis for the R248C mutation will therefore be offered in future pregnancies of our patient.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Acknowledgements and Funding
We thank Eva Herschberger for excellent technical support. This work was supported partly by a grant to C.H. from the Deutsche Forschungsgemeinschaft (DFG HA 5531/1).
References
Happle R: The group of epidermal nevus syndromes Part I. Well defined phenotypes. J Am Acad Dermatol. 2010, 63: 1-22. 10.1016/j.jaad.2010.01.017.
Sugarman JL: Epidermal nevus syndromes. Semin Cutan Med Surg. 2007, 26: 221-230. 10.1016/j.sder.2008.03.006.
Happle R: Mosaicism in human skin. Understanding the patterns and mechanisms. Arch Dermatol. 1993, 129: 1460-1470. 10.1001/archderm.129.11.1460.
Happle R, Rogers M: Epidermal nevi. Adv Dermatol. 2002, 18: 175-201.
Hafner C, López-Knowles E, Luis NM, Toll A, Baselga E, Fernández-Casado A, Hernández S, Ribé A, Mentzel T, Stoehr R, et al: Oncogenic PIK3CA mutations occur in epidermal nevi and seborrheic keratoses with a characteristic mutation pattern. Proc Natl Acad Sci USA. 2007, 104: 13450-13454. 10.1073/pnas.0705218104.
Hafner C, van Oers JM, Vogt T, Landthaler M, Stoehr R, Blaszyk H, Hofstaedter F, Zwarthoff EC, Hartmann A: Mosaicism of activating FGFR3 mutations in human skin causes epidermal nevi. J Clin Invest. 2006, 116: 2201-2207. 10.1172/JCI28163.
Hurst CD, Zuiverloon TC, Hafner C, Zwarthoff EC, Knowles MA: A SNaPshot assay for the rapid and simple detection of four common hotspot codon mutations in the PIK3CA gene. BMC Res Notes. 2009, 2: 66-10.1186/1756-0500-2-66.
Rogers M, McCrossin I, Commens C: Epidermal nevi and the epidermal nevus syndrome. A review of 131 cases. J Am Acad Dermatol. 1989, 20: 476-488. 10.1016/S0190-9622(89)70061-X.
Cappellen D, De Oliveira C, Ricol D, de Medina S, Bourdin J, Sastre-Garau X, Chopin D, Thiery JP, Radvanyi F: Frequent activating mutations of FGFR3 in human bladder and cervix carcinomas. Nat Genet. 1999, 23: 18-20.
Gymnopoulos M, Elsliger MA, Vogt PK: Rare cancer-specific mutations in PIK3CA show gain of function. Proc Natl Acad Sci USA. 2007, 104: 5569-5574. 10.1073/pnas.0701005104.
Tavormina PL, Shiang R, Thompson LM, Zhu YZ, Wilkin DJ, Lachman RS, Wilcox WR, Rimoin DL, Cohn DH, Wasmuth JJ: Thanatophoric dysplasia (types I and II) caused by distinct mutations in fibroblast growth factor receptor 3. Nat Genet. 1995, 9: 321-328. 10.1038/ng0395-321.
Happle R: Lethal genes surviving by mosaicism: a possible explanation for sporadic birth defects involving the skin. J Am Acad Dermatol. 1987, 16: 899-906. 10.1016/S0190-9622(87)80249-9.
Hafner C, van Oers JM, Hartmann A, Landthaler M, Stoehr R, Blaszyk H, Hofstaedter F, Zwarthoff EC, Vogt T: High Frequency of FGFR3 Mutations in Adenoid Seborrheic Keratoses. J Invest Dermatol. 2006, 126: 2404-2407. 10.1038/sj.jid.5700422.
Logié A, Dunois-Lardé C, Rosty C, Levrel O, Blanche M, Ribeiro A, Gasc JM, Jorcano J, Werner S, Sastre-Garau X, et al: Activating mutations of the tyrosine kinase receptor FGFR3 are associated with benign skin tumors in mice and humans. Hum Mol Genet. 2005, 14: 1153-1160. 10.1093/hmg/ddi127.
Hafner C, Vogt T: Seborrheic keratosis. J Dtsch Dermatol Ges. 2008, 6: 664-677. 10.1111/j.1610-0387.2008.06788.x.
Bernard-Pierrot I, Brams A, Dunois-Lardé C, Caillault A, Diez de Medina SG, Cappellen D, Graff G, Thiery JP, Chopin D, Ricol D, et al: Oncogenic properties of the mutated forms of fibroblast growth factor receptor 3b. Carcinogenesis. 2006, 27: 740-747.
Bader AG, Kang S, Vogt PK: Cancer-specific mutations in PIK3CA are oncogenic in vivo. Proc Natl Acad Sci USA. 2006, 103: 1475-1479. 10.1073/pnas.0510857103.
Hafner C, Di Martino E, Pitt E, Stempfl T, Tomlinson D, Hartmann A, Landthaler M, Knowles M, Vogt T: FGFR3 mutation affects cell growth, apoptosis and attachment in keratinocytes. Exp Cell Res. 2010, 316: 2008-2016. 10.1016/j.yexcr.2010.04.021.
Hafner C, Toll A, Fernández-Casado A, Earl J, Marqués M, Acquadro F, Méndez-Pertuz M, Urioste M, Malats N, Burns JE, et al: Multiple oncogenic mutations and clonal relationship in spatially distinct benign human epidermal tumors. Proc Natl Acad Sci USA. 2010, 107: 20780-20785. 10.1073/pnas.1008365107.
Haberland-Carrodeguas C, Allen CM, Lovas JG, Hicks J, Flaitz CM, Carlos R, Stal S: Review of linear epidermal nevus with oral mucosal involvement--series of five new cases. Oral Dis. 2008, 14: 131-137. 10.1111/j.1601-0825.2006.01355.x.
Collin B, Taylor IB, Wilkie AO, Moss C: Fibroblast growth factor receptor 3 (FGFR3) mutation in a verrucous epidermal naevus associated with mild facial dysmorphism. Br J Dermatol. 2007, 156: 1353-1356. 10.1111/j.1365-2133.2007.07869.x.
García-Vargas A, Hafner C, Pérez-Rodríguez AG, Rodriguez-Rojas LX, González-Esqueda P, Stoehr R, Hernández-Torres M, Happle R: An epidermal nevus syndrome with cerebral involvement caused by a mosaic FGFR3 mutation. Am J Med Genet A. 2008, 2275-2279. 146A
Rongioletti F, Rebora A: Epidermal nevus with transitional cell carcinomas of the urinary tract. J Am Acad Dermatol. 1991, 25 (5 Pt 1): 856-858.
Rosenthal D, Fretzin DF: Epidermal nevus syndrome: report of association with transitional cell carcinoma of the bladder. Pediatr Dermatol. 1986, 3: 455-458. 10.1111/j.1525-1470.1986.tb00650.x.
García de Jalón A, Azúa-Romeo J, Trivez MA, Pascual D, Blas M, Rioja LA: Epidermal naevus syndrome (Solomon's syndrome) associated with bladder cancer in a 20-year-old female. Scand J Urol Nephrol. 2004, 38: 85-87. 10.1080/00365590310017316.
Hernández S, Toll A, Baselga E, Ribé A, Azua-Romeo J, Pujol RM, Real FX: Fibroblast growth factor receptor 3 mutations in epidermal nevi and associated low grade bladder tumors. J Invest Dermatol. 2007, 127: 1664-1666.
Chesi M, Nardini E, Brents LA, Schröck E, Ried T, Kuehl WM, Bergsagel PL: Frequent translocation t(4;14)(p16.3;q32.3) in multiple myeloma is associated with increased expression and activating mutations of fibroblast growth factor receptor 3. Nat Genet. 1997, 16: 260-264. 10.1038/ng0797-260.
Ichikawa T, Saiki M, Kaneko M, Saida T: Squamous cell carcinoma arising in a verrucous epidermal nevus. Dermatology. 1996, 193: 135-138. 10.1159/000246229.
Hafner C, Klein A, Landthaler M, Vogt T: Clonality of basal cell carcinoma arising in an epidermal nevus. New insights provided by molecular analysis. Dermatology. 2009, 218: 278-281. 10.1159/000189209.
Sugarman JL: Epidermal nevus syndromes. Semin Cutan Med Surg. 2004, 23: 145-157. 10.1016/j.sder.2004.01.008.
Hyland VJ, Robertson SP, Flanagan S, Savarirayan R, Roscioli T, Masel J, Hayes M, Glass IA: Somatic and germline mosaicism for a R248C missense mutation in FGFR3, resulting in a skeletal dysplasia distinct from thanatophoric dysplasia. Am J Med Genet A. 2003, 120: 157-168.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2350/12/79/prepub
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
AB was responsible for the clinical work-up and wrote the draft of the manuscript. CF performed the genetic counselling, arranged fibroblast cultures and DNA extraction from skin and blood, and participated in discussing the results. OC took part in the histopathological classification and discussion, and supplied material for DNA extraction from paraffin blocks and urine. BF participated in the genetic analysis. CH performed the genetic analyses, immunohistochemistry and participated in discussing the results and writing the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Bygum, A., Fagerberg, C.R., Clemmensen, O.J. et al. Systemic epidermal nevus with involvement of the oral mucosa due to FGFR3mutation. BMC Med Genet 12, 79 (2011). https://doi.org/10.1186/1471-2350-12-79
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2350-12-79