Abstract
Background
The primitive hypoglossal artery (PHA) is a rare vascular anomaly, which belongs to the group of carotid-basilar anastomosis that may occur in adults.
Case presentation
Herein is presented a case of a patient with a PHA, who had undergone a cerebral angiography due to investigation of subarachnoid hemorrhage. Additionally, the diagnostic alternatives for detection and assessment of PHA and the spectrum of diseases related to its presence are discussed.
Conclusions
The presence of a persistent PHA can be recognized as an incidental finding in a cerebral angiography without any other clinical implication or may be associated with certain clinical entities such as aneurysm formation and atherosclerotic disease.
Similar content being viewed by others
Case report
A 51-year old man admitted to the emergencies of our Hospital, due to an episode of loss of consciousness. The chest X-ray (CXR), electrocardiogram (ECG) and first laboratory findings were normal and his medical history was remarkable for arterial hypertension, hypercholesterolemia and cigarette smoking. The patient underwent an unenhanced emergency cranial CT scan during the first hour of his admission, which revealed moderate subarachnoid hemorrhage (Fig. 1). The patient recovered completely after some hours and scheduled for a cerebral digital subtraction angiography, in order to exclude the presence of an aneurysm or an arteriovenous malformation.
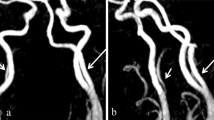
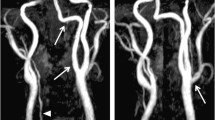
The angiography performed by Seldiger percutaneous puncture of the right femoral artery and selective catheterization of the right and left carotid artery and both vertebral arteries. There was no aneurysm or arteriovenous malformation demonstrated at this study. Instead, the selective catheterization of the left carotid artery disclosed a large persistent PHA originating from the internal carotid artery at the level of C2, which continued as basilar artery (Fig. 2). The catheterisation of the left subclavian artery demonstrated absence of the left vertebral artery whereas the right vertebral artery appeared hypoplastic (Fig 3). The right carotid artery appeared normal. Both posterior communicating arteries were visualised. The first angiogram in this particular patient did not reveal any vascular pathology. The patient repeated the angiography three weeks later, without any new other finding. Based on the findings of the two angiograms, the PHA was considered as an incidental finding and the etiology of the stroke in this patient was attributed to "nonaneurysmal" SAH.
Discussion
The primitive hypoglossal artery (PHA) belongs to the group of segmental arteries, which establish the dorsoventral anastomosis during the early fetal life. In the embryo, this dorsoventral anastomosis exists between an anterior arterial system, corresponding to the ventral aorta and a posterior one, located anteriorly in the midline of the neural tube [1]. Segmental arteries at the level of the brainstem are named after the cranial nerves with which they course, and include the trigeminal, otic and hypoglossal artery. Their involution coincides with the development of the posterior communicating artery, which takes place from the 30th to the 40th day of the fetal life. Although these segmental arteries obliterate normally after the 40th day, sporadically such an artery remains patent resulting in a carotid-basilar anastomosis during the adult life, as in the case herein presented. A persistent PHA is related with alterations to the anatomy of cerebral circulation and, although it can be observed as an incidental finding in cerebral angiography, its presence has been associated with clinical implications [2].
The PHA represents a rare carotid-basilar anastomosis, with a reported incidence between 0.03 and 0.26% on cerebral angiography [2, 3]. The PHA is the second most frequent after the persistent trigeminal artery, which makes up the vast majority of persistent primitive connections, whereas the persistent otic and proatlantal intersegmental arteries (type 1, corresponding to the first segmental artery and type 2, corresponding to the second segmental artery) are less frequent. The characteristics which constitute the criteria for identification of the PHA are described as follows: a) the PHA arises from the cervical part of the internal carotid artery at the C1-C2 level, b) together with the XIIth cranial nerve enters the posterior cranial fossa via the hypoglossal canal, c) the basilar trunk arises from the branch of PHA and d) the ipsilateral vertebral artery may be hypoplastic [1].
Although conventional angiography has been considered as the reference standard for the detection and evaluation of vascular structures, there are diagnostic alternatives with different advantages. CT angiography is a noninvasive examination, which has the advantage of multiplanar demonstration of the PHA by the use of 3D reconstraction techniques. Therefore, CT angiography provides excellent anatomic localization of PHA in all its parts and depicts clearly its entrance to the hypoglossal canal [4].
MR imaging and MR angiography in particular is able to sufficiently demonstrate the PHA, withour any contrast medium. MR angiography, by using a maximum-intensity-projection (MIP) program is able to show the complete carotid-basilar anastomosis without superimposition of other vessels [3–5]. Both CT and MR angiography are diagnostic alternatives, which have already been reported in the literature in cases of PHA detection and evaluation of certain pathologic conditions. Thus, stenosis due to atherosclerotic plaque or aneurysm formation can be depicted by 3D CT or MR angiography [6, 7].
Since the presence of PHA may be completely asymptomatic, it may appear as an incidental finding in a cerebral angiogram performed for another diagnostic purpose. However, its identification is clinically important before carotid endarterctomy or skull base surgery [8]. This is obviously related with the fact that both the anterior and posterior cerebral circulation is dependent on the arterial supply of internal carotid artery. The existance of PHA has also been related with increased incidence of aneurysms, arteriovenous malformations and atheroslerotic disease [5–7, 9, 10]. The later may present as a plaque extending from the distal carotid artery into the internal carotid artery (ICA) or as an isolated stenosis near the PHA takeoff. The group of persistent primitive arteries, in which PHA belongs to, is implicated in cases of moyamoya and quasi-moyamoya disease as well [11, 12].
The recognition of PHA as a member of the group of carotid-basilar connections and the reported incidence of related diseases has led to some pathogenetic considerations. There is a hypothesis related to the formation of atherosclerotic plaques affecting the PHA lumen. Because the origin of the PHA from the ICA forms analogous flow dynamics as at the carotid bulb, the development of an atherosclerotic plaque can be expected [7]. Another implication is that in cases of atherosclerotic disease, the clinical assessment of a patient with a PHA may lead to some confusion, due to atypical distribution of cerebral emboli. In addition to that, it has already been suggested that the PHA may be associated with anomalous structure of the vessel wall and exposes the basilar trunk to unusual haemodynamic stress, predisposing to the onset of aneurysms [6]. However, since the above theories have not been yet established, it would be interesting to be investigated in the setting of a multi-center study.
The detection and investigation of an uncommon vascular anomaly, such as the PHA, by an interventional or a non-interventional approach, is of clinical importance, since its presence has been related with a spectrum of diseases. In addition to that, CT and MR angiography due to their 3D capabilities have considerably facilitated the demonstration of the PHA as an anatomic variation.
References
Lasjaunias P, Doyon D: The ascending pharyngeal artery and the blood supply of the lower cranial nerves. J Neuroradiol. 1978, 5: 287-301.
De Caro R, Parenti A, Munari PF: The persistent primitive hypoglossal artery: a rare anatomic variation with frequent clinical implications. Anat Anz. 1995, 177: 193-198.
Chaljub G, Guinto FCJ, Crow WN: Persistent Hypoglossal Artery: MRI and MRA findings. J Comp Ass Tomog. 1995, 19: 668-671.
Oelerich M, Schuierer G: Primitive hypoglossal artery: demonstration with digital subtaction-, MR- and CT angiography. Eur Radiol. 1997, 7: 1492-1494. 10.1007/s003300050322.
Hahnel S, Hartmann M, Jansen O, Sartor K: Persistent hypoglossal artery: MRI, MRA and digital subtraction angiography. Neuroradiol. 2001, 43: 767-769. 10.1007/s002340100566.
Kanai H, Nagai H, Wakabayashi S, Hashimoto N: A large aneurysm of the persistent primitive hypoglossal artery. Neurosurg. 1992, 30: 794-797.
Wagner AL: Isolated stenosis of a persistent hypoglossal artery visualized at 3D CT angiography. Am J Neurorad. 2001, 22: 1613-1614.
Fantini GA, Reilly LM, Stoney RJ: Persistent hypoglossal artery: Diagnostic and therapeutic considerations concerning carotid thromboendarterectomy. J Vasc Surg. 1994, 20: 995-999.
Shibata Y, Hyodo A, Saito A, Yoshii Y, Nose T: Large arteriovenous malformation associated with persistent primitive hypoglossal artery-case report. Neurol Med Chir. 1991, 31: 804-808.
Katoh M, Kamiyama H, Kobayashi N, Makino K, Takano K, Tokumitsu N, Takamura H: Severe stenosis of internal carotid artery presenting as loss of consciousness due to presence of primitive hypoglossal artery; case report. Surg Neurol. 1999, 51: 310-312. 10.1016/S0090-3019(98)00053-6.
Komiyama M, Nakajima H, Yasui T, Kitano S, Sakamoto H, Fu Y: High incidence of persistent primitive arteries in moyamoya and quasi-moyamoya disease. Neurol Med Chir. 1999, 39: 416-420.
Katayama W, Eromoto T, Yanaki K, Nose T.: Moyamaya disease associated woth persistent primiteve hypoglossal artery: a case report. Ped Neurosurg. 2001, 35: 262-265. 10.1159/000050433.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2342/3/2/prepub
Author information
Authors and Affiliations
Corresponding author
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Vlychou, M., Georganas, M., Spanomichos, G. et al. Angiographic findings and clinical implications of persistent primitive hypoglossal artery. BMC Med Imaging 3, 2 (2003). https://doi.org/10.1186/1471-2342-3-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2342-3-2