Abstract
Background
When Staphylococcus aureus is isolated in urine, it is thought to usually represent hematogenous spread. Because such spread might have special clinical significance, we evaluated predictors and outcomes of S. aureus bacteriuria among patients with S. aureus bacteremia.
Methods
A case-control study was performed at John H. Stroger Jr. Hospital of Cook County among adult inpatients during January 2002-December 2006. Cases and controls had positive and negative urine cultures, respectively, for S. aureus, within 72 hours of positive blood culture for S. aureus. Controls were sampled randomly in a 1:4 ratio. Univariate and multivariable logistic regression analyses were done.
Results
Overall, 59% of patients were African-American, 12% died, 56% of infections had community-onset infections, and 58% were infected with methicillin-susceptible S. aureus (MSSA). Among 61 cases and 247 controls, predictors of S. aureus bacteriuria on multivariate analysis were urological surgery (OR = 3.4, p = 0.06) and genitourinary infection (OR = 9.2, p = 0.002). Among patients who died, there were significantly more patients with bacteriuria than among patients who survived (39% vs. 17%; p = 0.002). In multiple Cox regression analysis, death risks in bacteremic patients were bacteriuria (hazard ratio 2.9, CI 1.4-5.9, p = 0.004), bladder catheter use (2.0, 1.0-4.0, p = 0.06), and Charlson score (1.1, 1.1-1.3, p = 0.02). Neither length of stay nor methicillin-resistant Staphylococcus aureus (MRSA) infection was a predictor of S. aureus bacteriuria or death.
Conclusions
Among patients with S. aureus bacteremia, those with S. aureus bacteriuria had 3-fold higher mortality than those without bacteriuria, even after adjustment for comorbidities. Bacteriuria may identify patients with more severe bacteremia, who are at risk of worse outcomes.
Similar content being viewed by others
Background
Bacteriuria with Staphylococcus aureus is postulated to occur through a limited number of mechanisms--primarily ascending spread after instrumentation (e.g., urologic procedures or urethral catheterization) or hematogenous seeding of the genitourinary tract. The finding by Lee et al., that bacteremia is strongly associated with bacteriuria among patients infected with S. aureus, supports the notion that bacteremia is an important precursor for bacteriuria [1]. What is less clear, however, is whether in patients with S. aureus bacteremia, the finding of S. aureus in the urine holds any prognostic significance.
Among patients with S. aureus bacteremia, there are many prognostic factors, including host factors or comorbidities (age [2–10], Charlson score [2, 11], immunosuppression [4], alcoholism [4], hemodialysis [4], acute renal failure [4], diabetes mellitus [8], recent hospitalization [11], mechanical ventilation [5], and acute severity of illness [12]); pathogen-specific factors (MRSA [3, 13] superantigenic toxin production [14]); or characteristics of clinical presentation or management (meningitis [13] or altered mental status [11, 12], community-acquired infection [4], severe sepsis or septic shock [3, 4, 6, 7], lack of an infectious disease consult [4, 15], prior antibiotic therapy [6], unknown [8] or persisting foci of infection [16], daily dose of penicillinase-stable penicillin < 4 grams [16], and inappropriate empiric treatment [6, 12] or duration of treatment < 14 days [16]). The relation of occurrence of bacteriuria to outcome has been postulated [17], but the interactions with other risk factors warrant investigation. That bacteriuria might be a predictor of worse outcome in S. aureus bacteremia has biologic plausibility. For example, several innate defense mechanisms exist that prevent the development of urinary tract seeding in bacteremic patients: defensins, Toll-like receptor 4, and chemokine receptor CXCR1 [18, 19], and these innate defenses may be overcome and the urinary tract seeded in the setting of higher bacterial loads [20].
Over the last 20 years, MRSA has emerged as an important cause of nosocomial bacteremia [21], and significant increases in the incidence of MRSA infections in community patients have been observed in the past few years [22–24]. Methicillin-resistance is a major risk for increased morbidity and mortality in S. aureus infection. Given the increasing burden of infection by community-associated MRSA (CA-MRSA) infections [22–24] and the suggestion that CA-MRSA strains may have greater virulence, predictors of morbidity and mortality are essential for allocation of clinical infections.
We hypothesized that for patients with S. aureus bacteremia, bacteriuria is an important marker of disease severity and predictor of worse outcomes. We examined this hypothesis by evaluating outcomes of S. aureus bacteremia in patients with and without bacteriuria. We also examined the impact of methicillin-resistance on outcomes among patients with S. aureus bacteremia with and without bacteriuria. Finally, using our cohort, we examined the predictors of bacteriuria.
Methods
Setting
A case-control study was performed for patients admitted to John H. Stroger Jr. Hospital of Cook County, a 464-bed inner-city safety-net hospital in Chicago, Illinois. The institutional review board reviewed the study and deemed it exempt from review.
Study Design and Definitions
Our study included in-patients during January 2002 through December 2006. Cases were patients who had a positive urine culture for S. aureus within 72 hours of a positive blood culture for S. aureus. Controls were patients who had a negative urine culture for S. aureus within 72 hours of a positive blood culture S. aureus. Control patients were randomly sampled from all eligible patients with S. aureus bacteremia but without bacteriuria (i.e., with negative urine cultures), with the aim of 4 controls per case. Subsequently, chart reviews were performed and exclusion criteria were applied to sampled putative cases and controls to create a cohort for analysis.
Patients who were younger than age 18 years, who were seen only in the emergency department or in the clinic, or who did not have a urine culture performed within 72 hours of the positive blood cultures, were excluded. Only the first episode of S. aureus bacteremia per admission was assessed.
Using electronic data and chart review, we collected demographic and clinical data including mortality, ICU admission, length of stay, age, race, sex, Charlson score [25], comorbidities (HIV, diabetes mellitus, end stage renal disease requiring hemodialysis), alcoholism, intravenous drug use, presence of indwelling bladder catheter at the time of culture, previous urological procedure, duration of fever, duration of bloodstream infection, urinary symptoms, duration of chief complaint, organs and sites infected by S. aureus decided by the clinician, evidence of foreign material, susceptibilities of S. aureus, and time to appropriate antimicrobial therapy. For patients who died during their hospitalization, death was attributed to the bacteremia if so noted by the patient's discharge diagnosis or when there was a positive blood culture within 1 week preceding death.
S. aureus was deemed hospital-acquired if illness had onset > 72 hours after hospital admission. Cultures that turned positive within 72 hours of admission--community-onset--were divided into 2 groups: healthcare-associated infection was defined based on history of hospitalization, surgery, dialysis, or residence in a long-term care facility within 1 year or a presence of an indwelling catheter or percutaneous medical device (e.g., tracheostomy tube, gastrostomy tube, or bladder catheter) or a prior MRSA infection; patients with community-acquired infection did not have any of these risk factors [26].
Statistical Methods
Categorical variables were examined with chi-square analysis and continuous variables were analyzed with the independent samples t test. For multivariable analysis, statistically important factors with p values <0.10 on univariate analysis were included in initial models, and Charlson score was included a priori based on the strong association between comorbidities and death, and our desire to appropriately adjust for comorbidities in our analysis. We used Cox proportional hazards regression analysis to assess the association of bacteriuria with time to S. aureus death or hospital discharge, adjusted for suspected effect modifiers as identified in univariate analysis. Explanatory variables were evaluated for adherence to the proportional hazards assumption. To assess the multivariable predictors of bacteriuria, logistic regression was used. Data analysis was performed using SPSS software (version 15.0, Chicago, IL).
Results
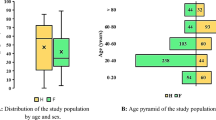
During 5 years (January 1, 2002, through December 31, 2006), 67 patients with S. aureus bacteremia and bacteriuria were identified, and control sampling yielded 268 bacteremic, non - bacteriuric patients. Following chart reviews and application of exclusion criteria, there were 61 cases and 247 controls. Of all 308 episodes of bacteremia, 128 (41.6%) were due to MRSA.
The mean age of pooled dataset, created by joining case and control patients was 48.3 years; 68.5% were male, 181 (58.8%) were African-American, and 37 (12.0%) died during hospital admission. Sites involved by bacteremia were cardiac valves [31 (10.7%)], vascular catheters [59 (19.2%)], skin/soft tissue [57 (18.5%)], bone/joints [27 (8.8%)], lungs [41 (13.3%)], genitourinary tracts [22 (7.1%)], and other sites [11 (3.6%)]; for 106 (36.7%) patients, there was no documented organ involvement other than bloodstream.
Hospital mortality rates were higher in S. aureus bacteremia patients with bacteriuria compared to patients without bacteriuria (39% vs 17%, respectively, p = 0.002) (table 1). In multiple Cox regression (table 2), significant predictors of death were positive urine culture (Hazard ratio 2.9; 95% CI, 1.4-5.9, p = 0.004), indwelling bladder catheter (2.0; 95% CI, 0.97-4.0, p = 0.06), and Charlson score (1.2; 95% CI, 1.1-1.3, p = 0.02); vascular catheter infection or phlebitis was associated with lower risk of death (0.27; 95% CI, 0.060-1.2, p = 0.09). Cox regression showed a significantly higher mortality rate in case than in control patients (figure 1). Neither methicillin-resistance nor the specific strain types of MRSA were predictors of mortality in univariate or multivariable analysis.
More positive urine cultures were seen in community-onset (both community-acquired and healthcare-associated) compared to hospital-acquired bacteremia (46% vs 23%, respectively, p < 0.001); in HIV-positive patients compared to HIV-negative patients (19% vs 10%, p = 0.05); and in patients with recent urological surgery (11% vs 3%, p = 0.03) or genitourinary infection (21% vs 4%, p < 0.001) compared with those without genitourinary problems (table 3). In multivariable analysis (table 4), urological surgery (OR 4.5, p = 0.045) and genitourinary infection (OR 5.7, p = 0.002) were significantly associated with positive urine cultures.
Discussion
In our case-control study, patients who had S. aureus bacteremia and a positive urine culture for S. aureus had significantly higher mortality than did bacteremic patients with a negative urine culture. This was true even after adjustment for multiple covariates including use of bladder catheters, presence or absence of lower urinary tract symptoms, or recent urological surgeries, which are known risk factors for a positive urine culture, significant factor in the multivariable analysis such as presence of line infection or phlebitis or presence of comorbidities as measured by the Charlson score [2, 11]. The conclusion that S. aureus bacteriuria patients have worse prognosis compared to patients without S. aureus bacteriuria among S. aureus bacteremia patients may be useful to clinicians when deciding whether to monitor a patient on the ward or the ICU and when explaining the prognosis of the illness to the patient and his family.
S. aureus is a common pathogen in the community and in hospitals. S aureus causes significant mortality and morbidity but is an infrequent cause of urinary tract infection [27]. In patients with S. aureus bacteremia, a positive urine culture is typically attributed to ascending infection or to hematogenous spread. Predictors of a positive urine culture for S. aureus include presence of indwelling bladder catheters, urinary tract obstruction, instrumentation, or surgery [27, 28]. We hypothesized that S. aureus appears in the urine in bacteremic patients because of higher burden of organisms and thus may portend worse outcome.
A recent study examining the relationship of bacteriuria with mortality found a two-fold increased risk of death in patients with concomitant S. aureus bacteriuria and bacteremia [17]. The current study adds to published literature by including significant numbers of methicillin-resistant isolates and by using statistical methods appropriate for varying time at risk. The association of bacteriuria with increased risk of mortality even after adjustment for comorbidities was similar in both studies, suggesting that bacteriuria provides useful prognostic information in the setting of S. aureus bacteremia. In addition, based on our findings, it appears that this is an effect independent of methicillin-resistance and that secular trends in incidence of MRSA are unlikely to alter this association.
There are several limitations to our study. The patients in the study were cared for at a single center and it may be difficult to generalize our findings to other hospitals. The Cook County Bureau of Health Services is the largest provider of indigent care in Cook County and has seen large increases in rates of community-associated S. aureus infection, and our estimates likely represent robust measures of risk for mortality. A second limitation is that this was a retrospective study and depended on documentation in the chart, which may have resulted in misclassification errors in assessing comorbidities and other covariates. Non-differential misclassification tends to bias towards the null, which suggests that our estimates of risk are likely conservative. In addition, electronic data were used in this study and were prospectively collected at the time of care; these data were not subject to problems inherent in reviews of written documentation Finally, in our study, we had an overall mortality rate of 12% which was at the lower end of published mortality rates--12-46% [3–13, 27, 29, 30]--in this setting, suggesting that our cohort may have had fewer comorbidities and lower attributable mortality that in other published data. This may be a result of the significant burden of CA-MRSA in our patient population.
Conclusions
In patients with S. aureus bacteremia, a positive urine culture for S. aureus may be used to identify patients at higher risk of death. Patients who have S. aureus bacteremia and more comorbidities are at increased risk for higher mortality rate.
References
Lee BK, Crossley K, Gerding DN: The association between Staphylococcus aureus bacteremia and bacteriuria. Am J Med. 1978, 65 (2): 303-306. 10.1016/0002-9343(78)90824-0.
Lesens O, Methlin C, Hansmann Y, Remy V, Martinot M, Bergin C, Meyer P, Christmann D: Role of comorbidity in mortality related to Staphylococcus aureus bacteremia: a prospective study using the Charlson weighted index of comorbidity. Infect Control Hosp Epidemiol. 2003, 24 (12): 890-896. 10.1086/502156.
Shurland S, Zhan M, Bradham DD, Roghmann MC: Comparison of mortality risk associated with bacteremia due to methicillin-resistant and methicillin-susceptible Staphylococcus aureus. Infect Control Hosp Epidemiol. 2007, 28 (3): 273-279. 10.1086/512627.
Kaech C, Elzi L, Sendi P, Frei R, Laifer G, Bassetti S, Fluckiger U: Course and outcome of Staphylococcus aureus bacteraemia: a retrospective analysis of 308 episodes in a Swiss tertiary-care centre. Clin Microbiol Infect. 2006, 12 (4): 345-352. 10.1111/j.1469-0691.2005.01359.x.
Blot SI, Vandewoude KH, Hoste EA, Colardyn FA: Outcome and attributable mortality in critically Ill patients with bacteremia involving methicillin-susceptible and methicillin-resistant Staphylococcus aureus. Arch Intern Med. 2002, 162 (19): 2229-2235. 10.1001/archinte.162.19.2229.
Soriano A, Martinez JA, Mensa J, Marco F, Almela M, Moreno-Martinez A, Sanchez F, Munoz I, Jimenez de Anta MT, Soriano E: Pathogenic significance of methicillin resistance for patients with Staphylococcus aureus bacteremia. Clin Infect Dis. 2000, 30 (2): 368-373. 10.1086/313650.
Jensen AG, Wachmann CH, Poulsen KB, Espersen F, Scheibel J, Skinhoj P, Frimodt-Moller N: Risk factors for hospital-acquired Staphylococcus aureus bacteremia. Arch Intern Med. 1999, 159 (13): 1437-1444. 10.1001/archinte.159.13.1437.
Mylotte JM, Tayara A: Staphylococcus aureus bacteremia: predictors of 30-day mortality in a large cohort. Clin Infect Dis. 2000, 31 (5): 1170-1174. 10.1086/317421.
McClelland RS, Fowler VG, Sanders LL, Gottlieb G, Kong LK, Sexton DJ, Schmader K, Lanclos KD, Corey R: Staphylococcus aureus bacteremia among elderly vs younger adult patients: comparison of clinical features and mortality. Arch Intern Med. 1999, 159 (11): 1244-1247. 10.1001/archinte.159.11.1244.
Laupland KB, Church DL, Mucenski M, Sutherland LR, Davies HD: Population-based study of the epidemiology of and the risk factors for invasive Staphylococcus aureus infections. J Infect Dis. 2003, 187 (9): 1452-1459. 10.1086/374621.
Bader MS: Staphylococcus aureus bacteremia in older adults: predictors of 7-day mortality and infection with a methicillin-resistant strain. Infect Control Hosp Epidemiol. 2006, 27 (11): 1219-1225. 10.1086/507924.
Gomez J, Garcia-Vazquez E, Banos R, Canteras M, Ruiz J, Banos V, Herrero JA, Valdes M: Predictors of mortality in patients with methicillin-resistant Staphylococcus aureus (MRSA) bacteraemia: the role of empiric antibiotic therapy. Eur J Clin Microbiol Infect Dis. 2007, 26 (4): 239-245. 10.1007/s10096-007-0272-x.
Romero-Vivas J, Rubio M, Fernandez C, Picazo JJ: Mortality associated with nosocomial bacteremia due to methicillin-resistant Staphylococcus aureus. Clin Infect Dis. 1995, 21 (6): 1417-1423.
Desachy A, Lina G, Vignon P, Hashemzadeh A, Denis F, Etienne J, Francois B, Ploy MC: Role of superantigenic strains in the prognosis of community-acquired methicillin-susceptible Staphylococcus aureus bacteraemia. Clin Microbiol Infect. 2007, 13 (11): 1131-1133. 10.1111/j.1469-0691.2007.01810.x.
Fowler VG, Sanders LL, Sexton DJ, Kong L, Marr KA, Gopal AK, Gottlieb G, McClelland RS, Corey GR: Outcome of Staphylococcus aureus bacteremia according to compliance with recommendations of infectious diseases specialists: experience with 244 patients. Clin Infect Dis. 1998, 27 (3): 478-486. 10.1086/514686.
Jensen AG, Wachmann CH, Espersen F, Scheibel J, Skinhoj P, Frimodt-Moller N: Treatment and outcome of Staphylococcus aureus bacteremia: a prospective study of 278 cases. Arch Intern Med. 2002, 162 (1): 25-32. 10.1001/archinte.162.1.25.
Huggan PJ, Murdoch DR, Gallagher K, Chambers ST: Concomitant Staphylococcus aureus bacteriuria is associated with poor clinical outcome in adults with S. aureus bacteraemia. J Hosp Infect. 2008, 69 (4): 345-349. 10.1016/j.jhin.2008.04.027.
Ganz T: Defensins in the urinary tract and other tissues. J Infect Dis. 2001, 183 (Suppl 1): S41-42. 10.1086/318838.
Svanborg C, Bergsten G, Fischer H, Godaly G, Gustafsson M, Karpman D, Lundstedt AC, Ragnarsdottir B, Svensson M, Wullt B: Uropathogenic Escherichia coli as a model of host-parasite interaction. Curr Opin Microbiol. 2006, 9 (1): 33-39. 10.1016/j.mib.2005.12.012.
De NS: Experimental pyelonephritis in the rabbit produced by staphylococcal infection. J Pathol Bacteriol. 1950, 62 (3): 429-436. 10.1002/path.1700620315.
National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2003, issued August 2003. Am J Infect Control. 2003, 31 (8): 481-498. 10.1016/j.ajic.2003.09.002.
Fridkin SK, Hageman JC, Morrison M, Sanza LT, Como-Sabetti K, Jernigan JA, Harriman K, Harrison LH, Lynfield R, Farley MM: Methicillin-resistant Staphylococcus aureus disease in three communities. N Engl J Med. 2005, 352 (14): 1436-1444. 10.1056/NEJMoa043252.
Hota B, Ellenbogen C, Hayden MK, Aroutcheva A, Rice TW, Weinstein RA: Community-associated methicillin-resistant Staphylococcus aureus skin and soft tissue infections at a public hospital: do public housing and incarceration amplify transmission?. Arch Intern Med. 2007, 167 (10): 1026-1033. 10.1001/archinte.167.10.1026.
King MD, Humphrey BJ, Wang YF, Kourbatova EV, Ray SM, Blumberg HM: Emergence of community-acquired methicillin-resistant Staphylococcus aureus USA 300 clone as the predominant cause of skin and soft-tissue infections. Ann Intern Med. 2006, 144 (5): 309-317.
Deyo RA, Cherkin DC, Ciol MA: Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992, 45 (6): 613-619. 10.1016/0895-4356(92)90133-8.
Naimi TS, LeDell KH, Como-Sabetti K, Borchardt SM, Boxrud DJ, Etienne J, Johnson SK, Vandenesch F, Fridkin S, O'Boyle C, et al: Comparison of community- and health care-associated methicillin-resistant Staphylococcus aureus infection. JAMA. 2003, 290 (22): 2976-2984. 10.1001/jama.290.22.2976.
Demuth PJ, Gerding DN, Crossley K: Staphylococcus aureus bacteriuria. Arch Intern Med. 1979, 139 (1): 78-80. 10.1001/archinte.139.1.78.
Arpi M, Renneberg J: The clinical significance of Staphylococcus aureus bacteriuria. J Urol. 1984, 132 (4): 697-700.
Hawkins C, Huang J, Jin N, Noskin GA, Zembower TR, Bolon M: Persistent Staphylococcus aureus bacteremia: an analysis of risk factors and outcomes. Arch Intern Med. 2007, 167 (17): 1861-1867. 10.1001/archinte.167.17.1861.
Mylotte JM, McDermott C, Spooner JA: Prospective study of 114 consecutive episodes of Staphylococcus aureus bacteremia. Rev Infect Dis. 1987, 9 (5): 891-907.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2334/10/225/prepub
Acknowledgements
We thank Izumi Chihara for assistance with statistical analysis.
Financial support: This study was funded in part by the CDC Chicago Epi-Center Grant Number 5U01CI000327.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
Bala Hota is a member of the speaker's bureau for Pfizer. All other authors have no competing interests.
Authors' contributions
SC participated in the design of the study, performed the chart reviews, participated in some statistical analysis and drafted the manuscript. KJP participated in obtaining the data for the study and proofreading the manuscript. RAW participated in the design of the study and proofreading the manuscript. BH participated in the design of the study, performed statistical analysis and proofread the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Chihara, S., Popovich, K.J., Weinstein, R.A. et al. Staphylococcus aureus bacteriuria as a prognosticator for outcome of Staphylococcus aureus bacteremia: a case-control study. BMC Infect Dis 10, 225 (2010). https://doi.org/10.1186/1471-2334-10-225
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2334-10-225