Abstract
Background
Mucoceles resulting from cystadenomas of the appendix are uncommon. Although rare, rupture of the mucoceles can occur with or without causing any abdominal complaint. There are several reports associating colonic malignancy with cystadenomas of the appendix. Herein, we report an unusual and interesting case of right inguinal hernia associated with left colon cancer.
Case presentation
A case of ruptured mucocele resulting from cystadenoma of the appendix was presented as right inguinal hernia in a 70-year-old male. The patient underwent colonoscopy, x-ray, ultrasound and computed tomography. Localized pseudomyxoma peritonei associated with adenocarcinoma of the descending colon was diagnosed. The patient underwent segmental resection of the colon, appendectomy, debridement of pseudomyxoma and closure of the internal ring of right inguinal canal. He is free of symptoms in one year follow-up.
Conclusion
Synchronous colon cancer may occur in patients with appendiceal mucoceles. In such patients, the colon should be investigated and colonoscopy can be performed meticulously in cases of ruptured mucoceles and localized pseudomyxoma peritonei. Surgical intervention is the current choice of management.
Similar content being viewed by others
Background
The incidence of mucocele ranges from 0.2–0.3% of all appendectomies and mucoceles resulting from cystadenomas of the appendix are very rare [1]. Although rare, rupture of the mucocele can occur with or without causing any abdominal complaint [2–4]. There are several reports associating colonic malignancy with mucocele of appendiceal cystadenoma [5–9]. We present a very unusual case of ruptured cystadenoma of the appendix with localized pseudomyxoma peritonei presenting as right inguinal hernia in a patient with left colon cancer.
Case report
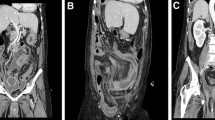
A 70 year-old male presented with a right inguinal mass and dragging sensation over it for 2 months before admission to the hospital. He was on medication for hypertension and moderate aortic regurgitation for years with good control. We palpated a non-tender, irreducible and doughy mass over the right inguinal region. The laboratory data was within the normal limits including the tumor marker(CEA). Abdominal ultrasound showed an irregular cystic hypoechoic lesion over the right lower quadrant. CT scan revealed an irregular hypodense lesion with fat stranding near the cecum without obviously enlarged lymph nodes(Figure 1). The right inguinal canal was occupied by a heterogenous lesion with adjacent fat stranding suggestive of appendiceal mucocele with rupture(Figure 2). We noted that no leakage of oral intake of iodinated, water-soluble contrast medium from the cecum or appendix into the peritoneal cavity(Figure 3). We postulated no persistent leakage of mucin from the appendix. A gentle colonoscopic examination was performed. It revealed a 2 cm in diameter sessile polyp in the descending colon(Figure 4). Polypectomy was performed and the pathology revealed moderately differentiated adenocarcinoma with muscle layer invasion(Figure 5). At laparotomy, a segmental resection of the descending colon with excision of the mesenteric lymph nodes, appendectomy(Figure 6), removal of yellowish mucoid jelly(Figure 7) and closure of the internal ring of the right inguinal canal were performed. Pathology revealed cystadenoma of the appendix(Figure 8) and moderately differentiated adenocarcinoma of the descending colon, without regional lymph node metastases. The hospital course was uneventful. The patient is free of symptoms at one year follow-up.
Discussion
Appendiceal mucocele causes the mucinous distention of the appendiceal lumen. The pathologic entity includes retention cyst, mucosal hyperplasia, cystadenoma and cystadenocarcinoma [10]. Symptomatic lesions are associated with malignant diseases more common than asymptomatic ones [11]. There are reports of other tumors associated with appendiceal mucoceles, including gastrointestinal tract, ovary, breast and kidney tumors, which might occur in up to one-third of the patients [12]. Pitiakoudis et al. have reported synchronous colonic cancer associated with appendiceal cystadenocarcinoma [13]. An increased incidence of colonic cancer in patients with appendiceal mucocele has been reported [14]. We reviewed other ten patients with appendiceal mucoceles undergoing appendectomies in our hospital during the past 13 years. Three of them had presented ruptured lesions. We recalled some of them for the colonoscopic examination at outpatient department. For the other patients who refused further colonoscopy, we investigated the history of colonic surgery, colonoscopic examination or bowel habit change during the past period. At presentation, we had no evidence of occurrence of concomitant colonic cancer in the patients. The concomitant pathologies are often clinically silent [1]. The present patient was also asymptomatic before the rupture of the mucocele and its presentation as right inguinal hernia. There are also reports associating ruptured appendiceal mucoceles with or without colonic cancer [2, 3, 14]. However, none of them presented as inguinal hernia. To the best of our knowledge, no such case has ever been reported. The more advanced lesions are associated with higher incidence of concomitant lesions [15]. Synchronous colonic lesions should also be looked for and these are more common in advanced lesions [16–18]. Therefore, colonoscopy is recommended as mandatory before surgery when possible [19]. However, colonoscopy can sometimes cause severe and fatal complications [20–22] and there are techniques recommended to perform the procedure meticulously [23, 24]. We did not find oral intake of contrast medium leaking from the cecum on the CT scans. Therefore, we performed the procedure and found the distal colonic malignancy. The patient underwent surgery according the recommendation of others [12, 25–27].
Conclusion
Synchronous colon cancer may occur in patients with appendiceal mucoceles. In such patients, the colon should be investigated. In patients with ruptured mucoceles and localized pseudomyxoma peritonei, the colonoscopy can be performed meticulously. Surgery is the recommended method of treatment.
References
Pitiakoudis M, Tsaroucha AK, Mimidis K, Polychronidis A, Minopoulos G, Simopoulos C: Mucocele of the appendix: a report of five cases. Tech Coloproctol. 2004, 8 (2): 109-112.
Yonei Y, Kameda T, Ozawa Y, Ueno H, Tsukada N, Inagaki Y, Miyamoto K, Suzuki O, Okawa H, Kiryu Y: A case of appendiceal mucocele showing massive mucus production with concomitant colonic cancer. Gastroenterol Jpn. 1993, 28 (1): 102-109.
Hernandez CA, Ruiz ME, Urdaneta MT: Pseudomyxoma peritonei associated with appendiceal mucinous cystadenoma. Report of a case and review of the literature. GEN. 1994, 48 (3): 157-162.
Kusuyama T, Fujita M: Appendiceal mucinous cystadenoma associated with pseudomyxoma peritonei and multicystic peritoneal mesothelioma: report of a case. Surg Today. 1995, 25 (8): 745-749.
Versaci A, Rossitto M, Giuffre M, Leonello G, Pagano G, Terranova M: A case of appendiceal mucocele associated with adenocarcinoma of the left colon. G Chir. 1999, 20 (10): 397-401.
Vicenzi L, Moser A, Mazzola F, Rizzo S, Bonomo S, Bottura D, Castellini C, Ballarin A, Tosi D, Rosa G: Appendiceal mucocele associated with colonic neoplasm. Reports of 2 cases and review of the literature. Chir Ital. 2001, 53 (3): 420-424.
Fujiwara T, Hizuta A, Iwagaki H, Matsuno T, Hamada M, Tanaka N, Orita K: Appendiceal mucocele with concomitant colonic cancer. Report of two cases. Dis Colon Rectum. 1996, 39 (2): 232-236.
Ohta H, Komibuchi T, Oe S, Hanafusa T, Ukikusa M, Awane H, Shintaku M: Incidental 67Ga uptake into an appendiceal mucocele in a patient with sigmoid colon cancer. Ann Nucl Med. 1996, 10 (2): 257-259.
Zullo A, Botto G, Pastormerlo M: A case of appendiceal mucocele associated with cancer of the colon. Minerva Chir. 1995, 50 (12): 1095-1098.
Sasaki K, Ishida H, Komatsuda T, Suzuki T, Konno K, Ohtaka M, Sato M, Ishida J, Sakai T, Watanabe S: Appendiceal mucocele: Sonographic findings. Abdom Imaging. 2003, 28: 15-18.
Lakatos PL, Gyori G, Halasz J, Fuszek P, Papp J, Jaray B, Lukovich P, Lakatos L: Mucocele of the appendix: An unusual cause of lower abdominal pain in a patient with ulcerative colitis. A casereport and review of literature. World J Gastroenterol. 2005, 11 (3): 457-459.
Stocchi L, Wolff BG, Larson DR, Harrington JR: Surgical treatment of appendiceal mucocele. Arch Surg. 2003, 138: 585-589.
Pitiakoudis M, Argyropoulou PI, Tsaroucha AK, Prassopoulos P, Simopoulos C: Cystadenocarcinoma of the appendix: an incidental imaging finding in a patient with adenocarcinomas of the ascendingand the sigmoid colon. BMC Gastroenterol. 2003, 3: 30-
Zissin R, Gayer G, Fishman A, Edelstein E, Shapiro-Feinberg M: Synchronous mucinous tumors of the ovary and the appendix associated with pseudomyxoma peritonei: CT findings. Abdom Imaging. 2000, 25 (3): 311-316.
Hammer K, Hammer J, Oesterreicher C, Potzi R: Advanced distal colonic lesions as predictors of advanced lesions in the proximal colon. Medicine. 2000, 79 (3): 127-134.
du Boulay CE, Roche WR: Benign epithelial neoplasms of the appendix: classification and clinical associations. Histopathology. 1992, 21 (5): 447-451.
Wolff M, Ahmed N: Epithelial neoplasms of the vermiform appendix (exclusive of carcinoid). I Adenocarcinoma of the appendix. Cancer. 1976, 37 (5): 2493-2510.
Wolff M, Ahmed N: Epithelial neoplasms of the vermiform appendix (exclusive of carcinoid). II Cystadenomas, papillary adenomas, and adenomatous polyps of the appendix. Cancer. 1976, 37 (5): 2511-2522.
Fujiwara T, Hizuta A, Iwagaki H, Matsuno T, Hamada M, Tanaka N, Orita K: Appendiceal mucocele with concomitant colonic cancer. Reports of two cases. Dis Colon Rectum. 1996, 39 (2): 232-236.
Volchok J, Cohn M: Rare complications following colonoscopy: case reports of splenic rupture and appendicitis. JSLS. 2006, 10 (1): 114-116.
Shah PR, Raman S, Haray PN: Splenic rupture following colonoscopy: rare in the UK?. Surgeon. 2005, 3 (4): 293-295.
Simon Janes, Ian Cowan, Birgit Dijkstra: A life threatening complication after colonoscopy. BMJ. 2005, 330: 889-890.
Woltjen JA: A retrospective analysis of cecal barotraumacaused by colonoscope air flow and pressure. Gastrointest Endosc. 2005, 61 (1): 37-45.
Kozarek RA, Sanowski RA: Use of pressure release valve to prevent colonic injury during colonoscopy. Gastrointest Endosc. 1980, 26 (4): 139-142.
Aranha GV, Reyes CV: Primary epithelial tumors of the appendix and a reappraisal of the appendiceal ''mucocele''. Dis Colon Rectum. 1979, 22 (7): 472-476.
Martinez-Gonzalez MD, Takahashi T, Robles-Atayde JA, Lome C, Gamboa-Dominguez A, Bezaury P, Garcia-Blanco MC, Leon K, de la Garza-Villasenor L: Mucocele of the vermiform appendix. Rev Gastroenterol Mex. 1996, 61 (4): 366-370.
Zagrodnik DF, Rose DM: Mucinous cystadenoma of the appendix: diagnosis, surgical management, and follow-up. Curr Surg. 2003, 60 (3): 341-343.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-230X/6/32/prepub
Acknowledgements
I appreciate Dr HS Wu and MH Huang for the consultation, Dr MC Hung and YS Hwang for helping me in doing the surgery and Dr Lin for the consultation and the exact report of the pathology. We thank the patient for giving us written consent for publishing this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
YT Lee was in charge of the patient and did the surgery mainly. HS Wu and MH Huang were the consultants of the surgical plan. MC Hung and YS Hwang assisted the surgery. ST Lin was the reporter of pathology. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Lee, YT., Wu, HS., Hung, MC. et al. Ruptured appendiceal cystadenoma presenting as right inguinal hernia in a patient with left colon cancer: A case report and review of literature. BMC Gastroenterol 6, 32 (2006). https://doi.org/10.1186/1471-230X-6-32
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-230X-6-32