Abstract
Background
Women presenting with symptoms of acute uncomplicated urinary tract infection (UTI) are often prescribed antibiotics. However, in 25 to 50% of symptomatic women not taking antibiotics, symptoms recover spontaneously within one week. It is not known how many women are prepared to delay antibiotic treatment. We investigated how many women presenting with UTI symptoms were willing to delay antibiotic treatment when asked by their general practitioner (GP).
Methods
From 18 April 2006 until 8 October 2008, in a prospective cohort study, patients were recruited in 20 GP practices in and around Amsterdam, the Netherlands. Healthy, non-pregnant women who contacted their GP with painful and/or frequent micturition for no longer than seven days registered their symptoms and collected urine for urinalysis and culture. GPs were requested to ask all patients if they were willing to delay antibiotic treatment, without knowing the result of the culture at that moment. After seven days, patients reported whether their symptoms had improved and whether they had used any antibiotics.
Results
Of 176 women, 137 were asked by their GP to delay antibiotic treatment, of whom 37% (51/137) were willing to delay. After one week, 55% (28/51) of delaying women had not used antibiotics, of whom 71% (20/28) reported clinical improvement or cure. None of the participating women developed pyelonephritis.
Conclusions
More than a third of women with UTI symptoms are willing to delay antibiotic treatment when asked by their GP. The majority of delaying women report spontaneous symptom improvement after one week.
Similar content being viewed by others
Background
Acute uncomplicated urinary tract infections (UTIs) are infections of the lower urinary tract in otherwise healthy, non-pregnant, adult women without known anatomical or functional abnormalities of the urinary tract. The symptoms are bothersome and have a negative impact on quality of life [1–4]. Although empiric antibiotic treatment of all women with urinary symptoms has been reported to be cost-effective [5, 6], bacterial resistance is rising [7–10] and strategies to reduce antibiotic use are needed.
Placebo arms of randomized trials have shown that 25 to 50% of women presenting with UTI symptoms will have recovered in one week without using antibiotics [11–13]. Moreover, qualitative research has suggested that these women often want to avoid taking antibiotics and may prefer delayed antibiotic treatment [14]. Therefore, antibiotic use might be reduced if all women with UTI were asked to delay treatment.
We investigated how many women with UTI symptoms were willing to delay antibiotic treatment when asked by their general practitioner (GP). In addition, we explored how many of these women reported not to have used antibiotics after one week and whether their symptoms had improved.
Methods
Design and setting
From 18 April 2006 until 8 October 2008, in a prospective cohort study, patients were recruited in 20 GP practices in and around Amsterdam, the Netherlands, as part of the Amsterdam Cystitis / Urinary Tract Infection Study (ACUTIS) [15]. These practices serve a population of approximately 47000 people.
Participants
Eligible were female patients over 12 years of age, contacting their GP with painful and/or frequent micturition. The symptoms had to be present for no longer than seven days.
Exclusion criteria were: pregnancy, lactation, signs of pyelonephritis, having used antibiotics or having undergone a urological procedure in the past two weeks, known anatomical or functional abnormalities of the urogenital tract, and being immunocompromised (with the exception of diabetes mellitus).
Assessments
Included patients filled in a questionnaire to record presence and severity of signs and symptoms on a 4-point scale, each individual symptom being scored as ‘absent’, ‘a little’, ‘considerable’ or ‘very much’, In addition, they collected a urine sample for urinalysis and culture according to pre-specified criteria [15]. In line with the national guideline of the Dutch College of General Practitioners [16], no instructions for the urine collection method were given, since these have been reported to have no consequences for the extent of contamination [17–19]. The result of the baseline culture became known after the follow-up period of one week, ≥103 colony-forming units (CFU) of a single uropathogen per milliliter (mL) being defined as a positive culture according to international guidelines [20]. If two organisms were grown, a culture was considered positive if ≥103 CFU/mL of a primary uropathogen (Escherichia coli or Staphylococcus saprophyticus) were found, according to the same guidelines.
After performance of clinical history and urinalysis, GPs were requested to ask all patients whether they were willing to delay antibiotic treatment as long as possible. During this period, participating patients could still change to antibiotic treatment at any time. After one week, patients were asked to report whether they had used any antibiotics (yes/no) and whether their symptoms had been cured, had improved, were unchanged or had deteriorated.
Analysis
Key characteristics from history and urinalysis were compared between patients who were asked by their GP to delay antibiotic treatment and patients who were not. For patients who were asked to delay, we determined how many were willing to do so and how many were not. We crosstabulated the data on clinical cure and baseline culture in women who were willing to delay antibiotic treatment and had not used any antibiotics during the following week. If no follow-up data on antibiotic use were available, patients were analyzed as having used antibiotics. Analyses were performed in Stata/SE, version 10.1.
Ethics and informed consent
The study procedure was approved by the Medical Research Ethics Committee of the Academic Medical Center in Amsterdam. Participating women received a letter with information about the study and provided written informed consent. For patients under the age of 18, written parental authorization was obtained.
Results
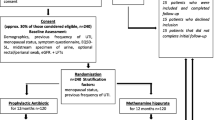
In total 205 women were eligible, of whom 29 were excluded (Figure 1). GPs participating in one of the 20 GP practices did not ask any of their 25 patients to delay antibiotic treatment, because they disagreed in principle with this approach. No differences in main patient characteristics (age, socioeconomic status, number of diagnosed UTIs in the past) were present between patients of this non-participating practice and those of the other practices. For four patients, GPs did not report whether they had been asked to delay.
Flow chart In total, 205 women were eligible. For principal reasons, one participating GP surgery did not ask any of their 25 patients to delay antibiotic treatment. For four patients, the GP did not report whether they were asked to delay. Of the remaining 176 patients, 137 were asked by their GP to delay antibiotic treatment. Of these patients, 37% (51/137) were willing to delay, of whom 55% (28/51) did not use any antibiotics during the following week.
Of the remaining 176 patients, 137 were asked by their GP to delay antibiotic treatment and 39 were not. For these two groups, median numbers of recruited patients per practice were 5 (range 0–33) and 1 (range 0–9), respectively. Table 1 shows the main characteristics of the two groups. Overall UTI prevalence was 59% (103/176). Women who reported at least considerable pain and women who thought they had a UTI were more likely to be asked to delay antibiotic treatment. Of those asked, 37% (51/137) were willing to delay (Figure 1). To investigate the variation between practices with respect to the proportions of women willing to delay, we calculated a weighted mean proportion across practices (random-effects meta-analysis), which yielded a similar result (39% (95% CI 27-52%)). Severity of symptoms did not differ significantly between women willing to delay and women not willing to delay (Table 2). The median number of recruited patients per practice was 2 for women willing to delay (range 0–18) and 4 for women not willing to delay (range 0–15).
After one week, 55% (28/51) of women who were willing to delay reported not to have used antibiotics and 71% (20/28) of these women reported clinical improvement or cure (Table 3). Of these patients, 35% (7/20) had a positive baseline culture. Of the eight women not reporting clinical improvement or cure after one week, two turned out to have had a positive culture at baseline.
Of the 51 women willing to delay, 15 (29%) had used an antibiotic after one week, of whom all reported clinical improvement or cure and 13 had a positive baseline culture. Eight of the 51 women (16%) did not report on their antibiotic use.
Of women who had been asked by their GP to delay treatment, 25% (34/137) reported not to have used antibiotics after one week, against 15% (6/39) of women who had not been asked, yielding a difference of 10% (95% CI −6 to 21%). Of the six women not being asked to delay, five had cure or improvement of symptoms, of whom one had a positive baseline culture. Of the 137 women who were asked to delay, 30 did not report on antibiotic use after one week (Figure 1), 22 of whom belonged to the group not willing to delay at baseline. Of the 39 women who were not asked to delay, one did not report on antibiotic use.
The result of the baseline culture was known only after the follow-up period of one week. It turned out to be positive for 51% (26/51) of the delaying women and for 67% (58/86) of the non-delaying women (risk difference 16% (95% CI 0-33%)) (Table 2).
No patients developed pyelonephritis during the follow-up period of one week, implying a 95% CI of 0-12% for the 28 delaying women who had not used antibiotics after one week.
Discussion
Our results suggest that more than a third of women with UTI symptoms are willing to delay antibiotic treatment when asked by their GP. More than half of these women (28/51) will not have used antibiotics after one week, of whom more than 70% (20/28) will have improvement of their symptoms.
The proportion of women reporting the use of antibiotics was 10% lower in the group that had been asked to delay as compared to those that had not been asked. The true reduction may be somewhat higher, since in the group asked to delay 30 patients were analyzed as having used antibiotics because no follow-up data were available. However, it should be taken into account that not all baseline characteristics were similar between these two groups (in the group asked to delay, more women reported at least considerable pain and/or thought they had a UTI).
As far as we know, this is the first study that describes the proportion of women with UTI symptoms that are willing to delay antibiotic treatment. Our findings are consistent with the results from a qualitative study by Leydon et al., which revealed that patients do not always want to use antibiotics, although clinicians often assume that they do [14]. This misinterpretation by clinicians might be illustrated by the fact that not all eligible patients in our study were asked to delay antibiotic treatment by their GP.
In addition to the 28 women willing to delay treatment, six women not willing to delay had not used antibiotics after one week. Although being asked to delay might have stimulated these six women in changing their minds to not using antibiotics, we did not obtain information on their motives. For five of these women, symptoms were cured or improved, one having had a positive baseline culture.
We had no further information on reasons for GPs not to enquire after their patients’ willingness to delay, which may be seen as the main limitation of our study. However, patients who were excluded by their GP did not have worse baseline characteristics than those who were included. On the contrary: women who reported at least considerable pain and women who thought they had a UTI were more likely to be included. This suggests that the GPs’ decisions whether to ask patients to delay or not may be based more on their personal attitude towards antibiotic prescriptions than on patient characteristics, which is in line with the previously mentioned findings of the study by Leydon et al [14]. In addition, patient attitudes (e.g. demanding personality) and previous experiences (e.g. problematic UTI history) might influence the GPs’ decisions.
Another limitation is the large number of missing data in the group of patients who were not willing to delay antibiotic treatment. More than a third of these patients did not report on antibiotic use and symptom improvement after one week. We consider it likely that most of these patients were cured and therefore did not feel inclined to report on follow-up results.
Due to cultural differences, our results might not be completely generalisable to other countries, where women may be less willing to delay antibiotic treatment than in the Netherlands. However, similar patient attitudes towards antibiotic prescriptions have been reported for the United Kingdom and Hong Kong [14, 21, 22].
Whereas we evaluated improvement of symptoms after a week, we did not obtain follow-up urine samples. Therefore we can not draw any conclusions on microbiological cure.
An uncommon but severe complication of UTIs is pyelonephritis, which may be a reason to treat all women with a suspected UTI. However, placebo arms of randomized trials suggest that cystitis seldom progresses to pyelonephritis [11–13]. Similarly, no women developed pyelonephritis in our study population.
Since in clinical practice the result of the urine culture is not available at the moment that a treatment decision is taken, we included all patients with symptoms, independent of the result of their urine culture. We consider this a more pragmatic approach than including only patients with microbiologically proven UTI.
Our findings imply that antibiotic use might be considerably reduced by simply asking women with UTI symptoms whether they are willing to delay antibiotic treatment. Besides, most of delaying women will have symptom improvement after one week. This is in line with results from a randomized trial by Little et al., in which a treatment strategy of delayed prescription reduced antibiotic use by 20% while yielding the same symptom control when compared to a strategy of immediate antibiotics [23]. A potentially promising strategy being currently under investigation is initial treatment with pain medication instead of immediate antibiotics [24, 25].
Conclusions
Our results support previous findings that women with UTI symptoms may be more receptive to delayed antibiotic prescriptions than is assumed by many clinicians. If all of these women were asked to delay antibiotic treatment, antibiotic use might be substantially reduced without negatively impacting clinical recovery. As a safe alternative to antibiotics (without the risk of bacterial resistance), symptomatic treatment may be offered.
Abbreviations
- UTI:
-
Uncomplicated urinary tract infection
- GP:
-
General practitioner
- CFU/mL:
-
Colony-forming units per millilitre.
References
Clayson D, Wild D, Doll H, Keating K, Gondek K: Validation of a patient-administered questionnaire to measure the severity and bothersomeness of lower urinary tract symptoms in uncomplicated urinary tract infection (UTI): the UTI Symptom Assessment questionnaire. BJU Int. 2005, 96: 350-359. 10.1111/j.1464-410X.2005.05630.x.
Colgan R, Keating K, Dougouih M: Survey of symptom burden in women with uncomplicated urinary tract infections. Clin Drug Investig. 2004, 24: 55-60. 10.2165/00044011-200424010-00007.
Ellis AK, Verma S: Quality of life in women with urinary tract infections: is benign disease a misnomer?. J Am Board Fam Pract. 2000, 13: 392-397.
Malterud K, Baerheim A: Peeing barbed wire. Symptom experiences in women with lower urinary tract infection. Scand J Prim Health Care. 1999, 17: 49-53. 10.1080/028134399750002908.
Barry HC, Ebell MH, Hickner J: Evaluation of suspected urinary tract infection in ambulatory women: a cost-utility analysis of office-based strategies. J Fam Pract. 1997, 44: 49-60.
Fenwick EA, Briggs AH, Hawke CI: Management of urinary tract infection in general practice: a cost-effectiveness analysis. Br J Gen Pract. 2000, 50: 635-639.
Chomarat M: Resistance of bacteria in urinary tract infections. Int J Antimicrob Agents. 2000, 16: 483-487. 10.1016/S0924-8579(00)00281-8.
Gupta K, Scholes D, Stamm WE: Increasing prevalence of antimicrobial resistance among uropathogens causing acute uncomplicated cystitis in women. JAMA. 1999, 281: 736-738. 10.1001/jama.281.8.736.
Hooton TM, Besser R, Foxman B, Fritsche TR, Nicolle LE: Acute uncomplicated cystitis in an era of increasing antibiotic resistance: a proposed approach to empirical therapy. Clin Infect Dis. 2004, 39: 75-80. 10.1086/422145.
Kahlmeter G: An international survey of the antimicrobial susceptibility of pathogens from uncomplicated urinary tract infections: the ECO.SENS Project. J Antimicrob Chemother. 2003, 51: 69-76. 10.1093/jac/dkg028.
Christiaens TC, De Meyere M, Verschraegen G, Peersman W, Heytens S, De Maeseneer JM: Randomised controlled trial of nitrofurantoin versus placebo in the treatment of uncomplicated urinary tract infection in adult women. Br J Gen Pract. 2002, 52: 729-734.
Ferry SA, Holm SE, Stenlund H, Lundholm R, Monsen TJ: Clinical and bacteriological outcome of different doses and duration of pivmecillinam compared with placebo therapy of uncomplicated lower urinary tract infection in women: the LUTIW project. Scand J Prim Health Care. 2007, 25: 49-57. 10.1080/02813430601183074.
Richards D, Toop L, Chambers S, Fletcher L: Response to antibiotics of women with symptoms of urinary tract infection but negative dipstick urine test results: double blind randomised controlled trial. BMJ. 2005, 331: 143-10.1136/bmj.38496.452581.8F.
Leydon GM, Turner S, Smith H, Little P: Women’s views about management and cause of urinary tract infection: qualitative interview study. BMJ. 2010, 340: c279-10.1136/bmj.c279.
Knottnerus BJ, Bindels PJ, Geerlings SE, van Charante EP Moll, ter Riet G: Optimizing the diagnostic work-up of acute uncomplicated urinary tract infections. BMC Fam Pract. 2008, 9: 64-10.1186/1471-2296-9-64.
Van Haaren KAM, Visser HS, Van Vliet S, Timmermans AE, Yadava R, Geerlings SE, Ter Riet G, Van Pinxteren B: NHG-Standaard Urineweginfecties (tweede herziening). Huisarts Wet. 2005, 8: 341-352.
Baerheim A, Laerum E: Home-voided urine specimens in women. Diagnostic agreement with clean-catch midstream specimens. Scand J Prim Health Care. 1990, 8: 207-211. 10.3109/02813439008994960.
Leisure MK, Dudley SM, Donowitz LG: Does a clean-catch urine sample reduce bacterial contamination?. N Engl J Med. 1993, 328: 289-290. 10.1056/NEJM199301283280420.
Lifshitz E, Kramer L: Outpatient urine culture: does collection technique matter?. Arch Intern Med. 2000, 160: 2537-2540. 10.1001/archinte.160.16.2537.
European Confederation of Laboratory Medicine: Scand J Clin Lab Invest. 2000, 231: 1-96.
Butler CC, Rollnick S, Pill R, Maggs-Rapport F, Stott N: Understanding the culture of prescribing: qualitative study of general practitioners’ and patients’ perceptions of antibiotics for sore throats. BMJ. 1998, 317: 637-642. 10.1136/bmj.317.7159.637.
Chan CS: What do patients expect from consultations for upper respiratory tract infections?. Fam Pract. 1996, 13: 229-235. 10.1093/fampra/13.3.229.
Little P, Moore MV, Turner S, Rumsby K, Warner G, Lowes JA, Smith H, Hawke C, Leydon G, Arscott A: Effectiveness of five different approaches in management of urinary tract infection: randomised controlled trial. BMJ. 2010, 340: c199-10.1136/bmj.c199.
Bleidorn J, Gagyor I, Kochen MM, Wegscheider K, Hummers-Pradier E: Symptomatic treatment (ibuprofen) or antibiotics (ciprofloxacin) for uncomplicated urinary tract infection?–results of a randomized controlled pilot trial. BMC Med. 2010, 8: 30-10.1186/1741-7015-8-30.
Gagyor I, Hummers-Pradier E, Kochen MM, Schmiemann G, Wegscheider K, Bleidorn J: Immediate versus conditional treatment of uncomplicated urinary tract infection - a randomized-controlled comparative effectiveness study in general practices. BMC Infect Dis. 2012, 12: 146-10.1186/1471-2334-12-146.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2296/14/71/prepub
Acknowledgements
We thank the following GPs and health centres for their participation in patient recruitment:
Mr RH Dijkstra, Gezondheidscentrum Diemen-Noord, Gezondheidscentrum Diemen-Zuid, Gezondheidscentrum Gein, Gezondheidscentrum Holendrecht-Noord, Gezondheidscentrum Holendrecht-Zuid, Gezondheidscentrum Klein Gooioord, Gezondheidscentrum Nellestein, Gezondheidscentrum Reigersbos, Huisartsen Monnickendam, Huisartsenpraktijk Badhoevedorp, Huisartsenpraktijk Bouwman, Huisartsenpraktijk HB Burggraaff, Huisartsenpraktijk De Wagenmaker, Huisartsenpraktijk Loenermark 162–164, Huisartsenpraktijk Oude Turfmarkt, Huisartsenpraktijk Purmerend, Mr HC Völke, Mr N Wieringa en Mrs M Wieringa-de Waard.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
All authors participated in the design of the study. BJK coordinated data collection, statistical analysis and reporting of the results. All authors contributed to writing the paper. All authors have read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Knottnerus, B.J., Geerlings, S.E., Moll van Charante, E.P. et al. Women with symptoms of uncomplicated urinary tract infection are often willing to delay antibiotic treatment: a prospective cohort study. BMC Fam Pract 14, 71 (2013). https://doi.org/10.1186/1471-2296-14-71
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2296-14-71