Abstract
Background
There is no more effective intervention for secondary prevention of coronary heart disease than smoking cessation. Yet, evidence about the (cost-)effectiveness of smoking cessation treatment methods for cardiac inpatients that also suit nursing practice is scarce. This protocol describes the design of a study on the (cost-)effectiveness of two intensive smoking cessation interventions for hospitalised cardiac patients as well as first results on the inclusion rates and the characteristics of the study population.
Methods/design
An experimental study design is used in eight cardiac wards of hospitals throughout the Netherlands to assess the (cost-)effectiveness of two intensive smoking cessation counselling methods both combined with nicotine replacement therapy. Randomization is conducted at the ward level (cross-over). Baseline and follow-up measurements after six and 12 months are obtained. Upon admission to the cardiac ward, nurses assess patients’ smoking behaviour, ensure a quit advice and subsequently refer patients for either telephone counselling or face-to-face counselling. The counselling interventions have a comparable structure and content but differ in provider and delivery method, and in duration. Both counselling interventions are compared with a control group receiving no additional treatment beyond the usual care. Between December 2009 and June 2011, 245 cardiac patients who smoked prior to hospitalisation were included in the usual care group, 223 in the telephone counselling group and 157 in the face-to-face counselling group. Patients are predominantly male and have a mean age of 57 years. Acute coronary syndrome is the most frequently reported admission diagnosis. The ultimate goal of the study is to assess the effects of the interventions on smoking abstinence and their cost-effectiveness. Telephone counselling is expected to be more (cost-)effective in highly motivated patients and patients with high SES, whereas face-to-face counselling is expected to be more (cost-)effective in less motivated patients and patients with low SES.
Discussion
This study examines two intensive smoking cessation interventions for cardiac patients using a multi-centre trial with eight cardiac wards. Although not all eligible patients could be included and the distribution of patients is skewed in the different groups, the results will be able to provide valuable insight into effects and costs of counselling interventions varying in delivery mode and intensity, also concerning subgroups.
Trial registration
Dutch Trial Register NTR2144
Similar content being viewed by others
Background
Cardiovascular disease is the leading cause of death and the second largest source of healthcare costs in Western Countries [1]. A third of cardiovascular disease mortality and hospital admissions are caused by coronary heart disease [2, 3]. Smoking cessation after a first coronary event such as a myocardial infarction significantly reduces the risk of mortality, hospitalisation rates and reoccurrence [4–6]. Smoking cessation is thus very relevant to patients with established coronary heart disease. Nevertheless, over half of those patients who were smokers prior to hospitalisation for coronary heart disease continue smoking after hospital discharge [7, 8]. Cardiac patients who continue smoking after hospitalisation are characterised as highly dependent smokers with no or low future intentions to quit [9]. Earlier research showed that providing brief cessation support is not effective enough to help cardiac patients to quit smoking permanently [10, 11]. Hence, there is a need for more intensive smoking cessation interventions for this patient group. Interventions proven to increase smoking cessation rates in hospitalised smokers in general are promising [11, 12]. Compared with the benefits of prevention, and reduced morbidity and mortality, the healthcare costs of these interventions are low [13–19].
In the Netherlands, effective interventions for smoking cardiac patients which also suit nursing practice are scarce. A cardiac minimal intervention strategy (CMIS) meant for ward nurses to help smoking patients to quit was implemented on a large scale in Dutch cardiac wards [20]. Despite the moderate effect of the CMIS on smoking behaviour [10], its public health impact was hindered because of implementation difficulties in practice [21, 22]. Only 28% of all Dutch cardiac ward nurses consistently and adequately used the CMIS [23]. Nurses reported barriers to its adequate implementation in hospital units as the difficulty of providing aftercare, lack of time and other priorities than smoking cessation support [22–27]. Because of the lack of intensive, and feasible interventions, many Dutch patients have continued smoking, resulting in high risks of (re)current coronary events or mortal closure.
Intensive smoking cessation interventions are, in general, recommended to cover the need for new (cost-)effective interventions for smoking cardiac patients [11, 28]. Evidence suggests that interventions combining personalised behavioural counselling with pharmacological treatment are most likely to increase quitting rates in hospitalised (cardiac) patients [11, 29–33]. It is recommended that this treatment begins during hospital admission [34] and continues for more than a month after hospital discharge with numerous contact moments [29, 35]. Preferably, these interventions include quit advice by cardiologists [36], and a counselling approach integrating relapse prevention and motivational interviewing strategies [37–39]. Effectiveness can further be increased by intervening with regard to specific patient characteristics associated with a higher risk of continued smoking after hospitalisation for a cardiac event, such as symptoms of depression, anxiety and a Type D (distressed) personality [40–45].
Nicotine Replacement Therapy (NRT) has been shown to increase quitting rates, either delivered singly [31] or in combination with behavioural counselling [12, 46–49]. The nicotine delivered by NRT has similar or less severe effects than nicotine obtained through cigarette smoking and for cardiac patients it has proved to be safer than smoking [50, 51]. NRT provision is recommended for hospitalised smokers as it aids patients to suppress withdrawal symptoms [31], irrespective of their intention to quit [11, 34, 52].
Reviews of telephone counselling (TC) and face-to-face counselling (FC), both intensive smoking cessation behavioural interventions, concluded that they were equally effective in enhancing quit rates in general populations [11, 32, 33]. The significance of TC for cardiac inpatients is indicated by the fact that it includes multiple telephone sessions during a follow-up period of several months [29, 53]. A study by Reid et al. (2006) reported an increase in smoking abstinence rates in cardiac patients who received TC in addition to usual care consisting of bedside counselling and NRT use in-hospital [54]. An earlier study revealed the efficacy of a nurse-based programme for cardiac inpatients motivated to quit, including bedside counselling and six follow-up calls in the four months after discharge. The cessation rate in the experimental group was twice as high as in the usual care group [55]. The significance of FC for the general population of smokers has been reported [32], though its effectiveness for cardiac patients is less clear. A meta-analysis showed that psycho-educational programmes for cardiac patients were effective, revealing a significant difference in smoking cessation rates between intensive and less-intensive interventions [56].
TC is less intensive than FC and hence might be more convenient for certain smokers [57]. There are strong indications that patients with high quit motivation profit more from TC than those with low quit motivation [33]. Moreover, low socio-economic status (SES) groups, often with low quit motivation, may profit more from FC than higher SES groups [58], although they are recognised as less successful quitters [59]. Previous studies indicated that low SES groups have higher coronary heart disease rates and smoking prevalence than high SES groups [60, 61], and are less likely to quit smoking successfully while generally revealing lower intentions to quit [62, 63].
The study described here started in 2009. It examines within the cardiac inpatient setting the (cost-)effectiveness and feasibility of TC and FC combined with NRT. The studies described above provided the rationale for making such interventions the subject of this evaluation study. TC and FC incorporate the same elements but differ in delivery mode and intensity. This paper describes the aims, hypotheses and design of the study, the intervention components of TC and FC, and the inclusion rates of the study participants and their baseline characteristics. The effectiveness study specifically compares health outcomes and smoking cessation outcomes, whereas the cost-effectiveness study also compares these outcomes with the costs of the interventions, including usual care.
On the basis of previous studies we expect to find 55% quitters at 12 months in both intervention groups against 35% in the control group [10, 29, 35, 64]. Since reviews concluded that both interventions (TC and FC) were equally effective in general populations [32, 33, 65], we expect to find significant differences in smoking abstinence between usual care on the one hand and experimental conditions on the other. We furthermore expect to find differential effects within the experimental conditions: it is hypothesised that low SES groups profit more from FC compared with higher SES groups. It is also hypothesised that FC is more (cost-)effective for patients with low quit motivations, whereas TC is more (cost-)effective for patients with high quit motivations and a higher SES.
Methods/design
Setting
Forty-six cardiac wards of urban, leading clinical and academic hospitals throughout the Netherlands were approached for potential participation. Thirteen of these wards that did not offer any form of smoking cessation intervention to cardiac patients (unlike care as usual) were recruited. Five of these wards were still rejected by the research team because of incomparability with the other wards in terms of their constitution (i.e. they had a combined heart and lung unit). The remaining eight cardiac wards were accepted for the study.
In line with the Dutch Medical Research Ethics Committee (MERC) rules [66] the study protocol was submitted for approval to the MERC of the VU medical center Amsterdam. After approval by this MERC (MEC 2009/215; NL27637.029.09), the MERCs and/or Board of Directors of each hospital endorsed execution of the study. The study was registered with the Dutch Trial Registration (NTR2144).
Design
An experimental study using cross-over randomization at the ward level with a baseline measurement at hospital admission and post-measurements at six and 12 months after baseline was conducted. All cardiac wards first provided care as usual and subsequently the two experimental conditions one after the other. Table 1 shows a schematic representation of the serially implemented conditions. After completion of care as usual, four of the cardiac wards started implementing TC, and after its completion they implemented FC. The other four cardiac wards implemented the experimental conditions in reverse order. After each condition there was a one month period without inclusion of any patient.
Sample size calculations
Power and sample size calculations were conducted for the main outcome, seven-day point prevalence abstinence (PPA) after 12 months. Power calculations (one-sided; p < 0.05, Power = 0.80) showed that 193 patients per condition were needed to detect significant differences in PPA and possible interaction effects of the interventions with motivation to quit and SES. Advanced statistical methods, however, allowed adjustment for potential baseline confounding variables and improved the statistical power. Therefore, the required sample size was reduced by 30% [67], resulting in the need for N = 135 in each condition. Assuming 15% attrition at the 12-month follow up, 155 patients per condition needed to be recruited, totalling 465 patients for the three conditions.
Baseline procedure
After approval was received from the Board of Directors and Ethical Review Committees of each hospital, the face-to-face counsellors (16 in total, i.e. two nurses from each of the cardiac wards that participated in the study) received training to provide FC. Ward nurses and cardiologists received written and oral instructions of the study with a written stepwise protocol and information sheet on the inclusion process of eligible patients, a flowchart with instructions and addresses for referral. Over an 18-month period beginning in December 2009, the nurses asked all patients admitted to the cardiac ward if they had smoked in the month prior to admission. If the answer was yes, the nurses reviewed the information sheet with the inclusion criteria, approached medically stable patients at the bedside, provided the necessary information about the study to patients, and invited eligible smoking patients to take part in the study. If patients agreed to take part, the nurses asked them to sign an informed consent form. Subsequently, at hospital admission, nurses administered the questionnaire to patients and registered relevant patient data on a separate form. Nurses also produced a summary of patients’ prescribed medication from their case history.
Participants: inclusion and characteristics
Inclusion criteria for patients were: smoking on average ≥5 cigarettes per day in the month prior to admission or, if not smoking, having quit smoking less than four weeks before admission; being ≥18 years of age; being admitted to the cardiac ward for less than 96 h and being hospitalised because of a coronary heart disease (acute coronary syndrome, stable angina, and other forms of chronic and acute heart diseases) following the standards of the ICD-10 [68]. Exclusion criteria were language limitations that would impede completion of the self-administered questionnaire, a medically unstable cardiac situation or cognitive impairments.
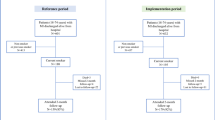
As shown in Figure 1, 245 cardiac patients were included in the usual care condition, 223 in the experimental condition of TC, and 157 cardiac patients in the experimental condition of FC. With inclusion rates varying from 42 to 121 patients per cardiac ward, rates varied considerably per cardiac ward (see Table 2).
As presented in Table 3, patients were predominantly male with a mean age of 57 years. Education levels were relatively equally distributed over low, intermediate and high education. Most of the patients had an admission diagnosis of acute coronary syndrome (ACS) or had been diagnosed with ACS previously and were admitted to the hospital for treatment with a percutaneous coronary intervention (PCI) or a coronary artery bypass graft (CABG). During the six months prior to admission a few patients had been admitted to the hospital owing to a cardiac event. Nicotine dependence was moderate, and patients reported smoking 21 cigarettes on average per day before hospital admission. Although the majority of the patients had not made any quit attempt over the past 12 months, one-third reported on admission that they had not smoked over the past seven days. There were no significant differences between the three groups in terms of demographic characteristics. Nicotine dependence was significantly higher, however, in the control group than in the experimental groups.
Interventions
Standard in-hospital smoking cessation care (usual care)
All patients received standard in-hospital treatment for smoking cessation which consisted of an assessment of their smoking behaviour and a personalised brief quit advice. Quit advice was largely provided by cardiologists (and occasionally by ward nurses) while patients were on the cardiac ward.
Telephone counselling (TC) or face-to-face counselling (FC)
There were two experimental conditions, one consisting of TC and one of FC. The two counselling methods started within one week after the inclusion of the patient and had a comparable structure and content. Nurses on cardiac wards followed the Ask-Advice-Refer strategy [69, 70] prior to the counselling sessions. In accordance with this strategy, patients’ smoking behaviour was first assessed. Second, smoking patients were advised to quit, and third, they were referred to health professionals providing TC or FC outside the ward. Furthermore, nurses provided nicotine patches and information on their necessity and application to eligible patients. The counselling was provided by professional counsellors: in the TC, these were counsellors from the Dutch Expert Centre for Tobacco Control (STIVORO); in the FC, these were cardiac nurses trained in providing smoking cessation counselling. All counsellors received financial compensation. The main differences between the counselling methods were the delivery mode and intensity of the counselling. TC lasted for three months and consisted of seven telephone sessions of 10 to15 min (two hours in total). FC also lasted three months, consisted of six face-to-face sessions of 45 min and ended with a follow-up call eight weeks after the last session (4.75 h in total).
Existing protocols of TC and FC developed by the Dutch Expert Centre for Tobacco Control for the general smoking public were used, though adapted and fine-tuned to the situation of cardiac patients. The protocols focused on important determinants of smoking cessation and relapse such as self-efficacy and smoking-related attitudes [32, 33, 58]. The underlying theoretical methods of the two counselling methods were comparable and incorporated strategies based on the principles of motivational interviewing [38], enhancement of self-efficacy [71, 72], goal-setting [73] and relapse prevention [74]. In contrast to TC, patients who were referred to the FC condition additionally received a workbook from their face-to-face coach. For each session the workbook contained the most relevant information and a few pieces of homework such as developing personalised strategies for dealing with high-risk situations or developing a personalised emergency plan for how to avoid absolute relapse when experiencing a lapse.
The design and main content of the TC and FC sessions are presented in Table 4. In seven successive counselling sessions, the counsellor assisted the patient to become smoke-free and/or maintain his or her smoking abstinence. The underlying theoretical model of the counselling sessions was the Transtheoretical Model by Prochaska and Diclemente [75]. This model posits that health behaviour change involves progress through five stages. The first three stages are pre-action stages (pre-contemplation, contemplation, preparation) where smokers have no or a weak intention to quit or prepare a quit attempt. The last two stages are post-action stages (action, maintenance) where smokers genuinely quit smoking and ideally maintain their abstinence. In line with each of these stages, the counsellor provided stage-matched information and applied strategies tailored to each individual patient in order to move forward from one stage to the next, to arrive finally at the smoking cessation maintenance stage.
Fine-tuning of TC and FC was directed at specific characteristics of cardiac patients previously shown to be impediments to smoking cessation (depression, anxiety, and Type D personality) [41, 76–79], and targeted group-specific predictors of relapse [80–83]. A substantial number of the patients had not smoked since hospital admission. Some of them considered this temporary smoking restriction as a serious quit attempt, whereas others intended to resume smoking as soon as possible. To integrate these features as intervention components, protocols were adapted by the researchers including tips and tricks on the characteristics and particular situation of cardiac patients. The protocol contained information on how the content of the counselling sessions might vary and how it could be adjusted to the particular needs of the patient. An additional three-page information folder was developed and provided to cardiac patients in the intervention groups. This folder provided information and strategies on avoiding and dealing with risk situations for smoking where patients might experience negative affect and social inhibition, key characteristics of a Type D personality.
Counselling combined with nicotine replacement therapy
Reasons for the combination therapy of TC or FC with NRT in the study reported here were that antidepressants for smoking cessation (e.g. Bupropion) cannot be prescribed for all patients [84], NRT has been proven to be safe for cardiac patients [46, 51] and equally effective as medical pharmacotherapy [31, 84]. Cardiologists from the participating cardiac wards agreed on the prescription of transdermal nicotine patches for cardiac patients. The pharmacological therapy was therefore similar for all patients, essential to guarantee validity and enable conclusions to be drawn on the effectiveness of TC and FC. Owing to possible contra-indications in cardiac patients, cardiologists had to approve the delivery of nicotine patches for each individual patient. Eligible patients received NRT when indicated and when they smoked more than 10 cigarettes a day before hospital admission [85]. As treatment of eight weeks has been shown to be as efficacious as longer treatment periods [30], patients received the patches for eight weeks (at no cost).
Recruitment and training of counsellors
Professional telephone counsellors from the Dutch Expert Centre for Tobacco Control provided the TC (n = 4). The researchers provided additional training of four hours to the telephone counsellors. This training was necessary to inform the counsellors about specific patient characteristics.
To recruit face-to-face counsellors from the participating hospitals two cardiac nurses per nursing unit were invited to become professional smoking cessation counsellors (n = 16). An expert team of senior trainers from the Dutch Expert Centre for Tobacco Control provided the training to the cardiac nurses. The training of face-to-face counsellors consisted of eight sessions of four hours spread over four days with a break of six weeks between the first and the last training sessions.
Pilottesting of materials
For a small number of patients (n = 6), face-to-face and telephone counsellors (n = 4) and cardiac nurses of the participating wards (n = 6), materials (questionnaires for patients, additional protocols for nurses and counsellors, workbook for patients, folder for patients) were pilot-tested by means of in-depth interviews. Even though the Dutch Expert Centre for Tobacco Control [58] had already evaluated their training for counsellors in general, the training was evaluated on a small scale, and focused on the counselling of cardiac patients in order to fine-tune the interventions for this target group. The pilot interview with cardiac patients and counsellors resulted in some amendments to the content and the adaptation of some of the materials in terms of sentence structure.
Follow-up procedures
Six months after discharge (T1) patients were interviewed by telephone by members of a professional call agency to obtain follow-up data (see Figure 1). The 12-month follow-up measurements are still in progress (T2). The smoking cessation outcomes are assessed by means of validated reliable questions [86–88]. Telephone interviews are conducted in order to decrease the likelihood of attrition [10, 89]. One postal reminder letter is sent 10 days before each of these telephone interviews. All patients who complete the 12-months interview are also invited to the hospital for biomedical tests of blood pressure, cholesterol and saliva.
Cardiac nurses are responsible for conducting the blood pressure tests, the cholesterol tests and the cotinine tests at the cardiac nursing ward. Cardiac nurses ask patients while conducting the blood pressure test if they have been smoking over the past seven days to assess point-prevalence abstinence. If patients claim not to have smoked any cigarettes, their saliva is tested on cotinine residuals by means of the NicAlert Cotinine Test Strip to test whether the self-reported smoking behavior is accurate. Results can be either positive (no cotinine detected) or negative (cotinine detected). Cardiac nurses register the results of the blood pressure, cholesterol and cotinine tests and send the findings to the research team.
Measures
Effectiveness study: outcome measures
The primary outcome is seven-day point prevalence abstinence from smoking (PPA) after six and 12 months (0 = smoking;1 = non-smoking). PPA is the main outcome since it is considered to be the most sensitive and valid measure of smoking cessation [87]. Secondary outcomes are continued abstinence, quit attempts, and health outcomes. Health outcomes measured at T1 and T2 are new coronary events and hospital readmissions for coronary events. Cholesterol ratio and blood pressure are only assessed at T2 at the patients’ outpatient clinic. Intention to treat analyses will be applied [88] and smoking status is verified at T2 by a saliva sample. For these patients the outcome of the saliva test (detection of cotinine) will be taken as a control variable in the analyses to confirm the self-reported response of the smoking behaviour. This test has been proven to be a valid and reliable method for verification of smoking status [90].
Cost-effectiveness study: Cost factors and resource use
At T1 and T2, information on the other health economic outcomes is assessed for the past three months: visits to the general practitioner, cardiology outpatient visits, health related costs, rehospitalisations in the past six months, informal care costs, and health-related quality of life. Effects on productivity are measured in terms of absence from work owing to illness [91].
Resource use specifically for the interventions was recorded prospectively by the counsellors. This included counsellor time, use of materials, use of nicotine replacement patches and specialist time involved in cessation advice [92–94].
Other measures
A process evaluation was conducted at six-month follow-up in which patients were asked about usefulness of the interventions in total, their separate elements and patients’ adherence to NRT and counselling sessions. The baseline measurement and both post-tests also assess factors that are related to smoking cessation and/or relapse among this patient population. These include demographics; smoking-related factors [95]; disease-related factors; psychological states including depression and anxiety [96], Type D personality [97]; smoking cessation-related cognitions and motivation to quit [10, 98]. To measure smoking-related cognitions and motivation to quit, existing questionnaires are used [86, 99] which are based on previous social-cognitive models [75, 100, 101]. To assess the expected differential effects of the interventions for SES, SES is assessed in terms of education level and income [86].
Statistical analyses
Data is analyzed with SPSS. Descriptive statistics are used to describe the sample, and to compare the groups at baseline, ANOVA analyses and chi-square analyses are applied. In order to determine possible selective loss at follow-up, attrition analyses are conducted. The effects of the interventions on smoking cessation outcomes and possible interaction effects (condition * SES/condition * intention to quit) are tested by means of logistic regression analyses. The hospital group size of eight is inadequate for reliably testing the existence of variation by a multi-level model [102]. Therefore, a fixed-effect regression approach is likely to be used to eliminate possible hospital-level effects. Baseline variables are included as covariates to correct for possible baseline differences, to reduce unexplained variance and to increase the power of the tests. To analyse effects on rehospitalisation, new cardiac events, number of visits to the cardiologist and cardiovascular-related death, multiple regression analyses are used. Effects of the interventions on blood pressure, TC/HDL cholesterol, and intentions to quit are tested by means of repeated measures analyses of covariance. Logistic regression analyses are also used to examine predictors of smoking cessation overall and within subgroups. Patients in the experimental groups are compared by paired sample t-tests for level of appreciation of the intervention. Economic evaluation analyses are performed by applying specific cost-effectiveness calculation formulas. Moreover, a health-economic Markov Model is built to estimate long-term costs and health effects.
Discussion
Two different interventions were designed that combined intensive smoking cessation counselling – either delivered face-to-face or by telephone – and NRT. The interventions were designed to overcome the weaknesses of usual care and minimal interventions being too brief and not including recommended elements of smoking cessation treatment guidelines [30]. To overcome a second drawback of current interventions, i.e. the implementation and feasibility difficulties reported by ward nurses in terms of providing brief support on smoking cessation, the counselling (TC and FC) was delegated to smoking cessation professionals tasked with formal responsibility who had enough time to spare. As nurses applied the Ask-Advice-Refer approach, attention was paid to patients’ smoking behaviour at hospital admission while being referred to external professionals. This approach was assumed to be feasible in busy nursing units where nurses lack time and skills to provide smoking cessation support themselves [69, 70]. Offering smoking cessation treatment as an adjunct to hospital-initiated programmes shortly after hospital discharge lastly overcame the limitation of cardiac rehabilitation programmes which usually do not start within the first four weeks after discharge and only pay very brief attention to smoking cessation.
Study strengths
This study is a multi-centre trial carried out in eight hospital cardiac wards from different geographical regions of the Netherlands. Most randomised controlled trials on preventative interventions for smoking cardiac patients are conducted in only one or a few hospitals, so the information gathered from eight hospital wards improves generalisation of the study results. Cross-over randomisation was conducted at the ward level by sequentially implementing the conditions, which was done to overcome problems related to traditional randomised controlled trials. This design meant contamination between patients was avoided, as well as learning effects on ward nurses. The chosen design also circumvented nurses’ mistakes in performing the interventions. Moreover, the experimental design allowed us to control for confounding effects such as seasonal influences or other extraneous events. Last but not least, a cost-effectiveness study was carried out alongside the standard clinical trial, which allows us to estimate the additional costs and benefits of the interventions compared with a control group receiving usual care.
Methodological considerations
Although we made efforts to include all eligible smoking cardiac patients within the a time frame of one year and to register data on those eligible patients not enrolled in the study, the baseline results suggested that neither task was performed as intended. Nurses were asked to register the refusals of patients not enrolled in the study but this was not well done. There are indications that in some hospitals there were more refusals than in others. The inclusion period was expanded to 18 months as the inclusion of smoking cardiac patients in hospital cardiac wards took longer than expected. Low inclusion rates were related to ward factors such as insufficient patient admissions, few patients who met the inclusion criteria of the research, and limited admission capacities of cardiac wards. Other factors hindering patient inclusion in the study were high workloads on cardiac wards, non-collaborative nursing teams, and little interest in smoking cessation programmes at the general hospital. These factors have previously been shown to impede implementation of smoking cessation interventions in cardiac wards [103–105]. The inclusion rate in the FC group was relatively low which might be related to its time-consuming treatment form, resulting in a skewed distribution of patients with 157 patients in the FC group, 223 in the TC group and 245 in the UC group. Moreover, inclusion rates varied considerably between cardiac wards and this suggests the likelihood of non-representative outcomes of the effectiveness study for those cardiac wards that only included a few patients per group. We also note that there were differences in nicotine dependence between the experimental groups and the usual care group, as nicotine dependence was significantly higher in the experimental groups. Altogether these considerations pose the limitation of a selective sample of cardiac patients, implying the potentially limited generalisability of the study results.
Conclusion
Feasible evidence-based smoking cessation intervention approaches are required to support cardiac patients in quitting smoking in order to reduce future risks of cardiac events. Since subgroups may profit more from a different type of intervention and should receive the most (cost-)effective one, this study compares two intensive counselling methods - one provided face-to-face and the other by telephone - to each other and to usual care on their costs and effects on smoking abstinence. Although the inclusion period was expanded and not all eligible patients could be included, the results of this multi-centre trial will be able to provide valuable insight into the (cost-)effectiveness of both counselling interventions.
Authors’ information
NB is the primary PhD investigator of the current study on the (cost-)effectiveness of two intensive counselling methods for smoking cessation in persons with coronary heart disease. CB is associate professor in health psychology and received her PhD for studies on a minimal smoking cessation intervention strategy for cardiac inpatients. LL is professor in health psychology and has great expertise in and scientific knowledge on developing and evaluating behavioural interventions in general. AM is assistant professor in health psychology and has been involved in many projects on smoking cessation as co-promoter or advisor. FV is cardiologist and has been chair of Dutch Society of Cardiology. HdV is professor in health communication and has done a lot of research on smoking prevention and cessation.
Abbreviations
- SES:
-
Socio-economic status
- CMIS:
-
Minimal intervention strategy for cardiac patients
- NRT:
-
Nicotine replacement therapy
- Type D:
-
Distressed personality type
- FC:
-
Face-to-face counselling
- TC:
-
Telephone counselling
- ICD-10:
-
International Classification of Diseases
- STIVORO:
-
Dutch Expert Centre for Tobacco Control
- PPA:
-
Seven-day point prevalence abstinence from smoking
- TC/HDL cholesterol:
-
Total/high density lipoprotein cholesterol ratio.
References
WHO: WHO Report on the Global Tobacco Epidemic, 2008: The MPOWER package. 2008, World Health Organization, Geneva
De Hollander EAM, Hoeymans N, Melse JM, Van Oers JAM, Polder JJ: Zorg voor Gezondheid: Volksgezondheid Toekomst Verkenning 2006. 2007, RIVM, Bilthoven
Shah AM, Pfeffer MA, Hartley LH, Moye LA, Gersh BJ, Rutherford JD, Lamas GA, Rouleau JL, Braunwald E, Solomon SD: Risk of all-cause mortality, recurrent myocardial infarction, and heart failure hospitalization associated with smoking status following myocardial infarction with left ventricular dysfunction. Am J Cardiol. 2010, 106 (7): 911-916. 10.1016/j.amjcard.2010.05.021.
Van Spall HG, Chong A, Tu JV: Inpatient smoking-cessation counseling and all-cause mortality in patients with acute myocardial infarction. Am Heart J. 2007, 154 (2): 213-220. 10.1016/j.ahj.2007.04.012.
Critchley JA, Capewell S: Mortality risk reduction associated with smoking cessation in patients with coronary heart disease: a systematic review. JAMA. 2003, 290 (1): 86-97. 10.1001/jama.290.1.86.
Mohiuddin SM, Mooss AN, Hunter CB, Grollmes TL, Cloutier DA, Hilleman DE: Intensive smoking cessation intervention reduces mortality in high-risk smokers with cardiovascular disease. Chest. 2007, 131 (2): 446-452. 10.1378/chest.06-1587.
Berndt NC, Bolman C, Mudde AN, Verheugt F, De Vries H, Lechner L: Risk groups and predictors of short-term smoking abstinence in patients with coronary heart disease. Heart Lung. 2012, 41 (4): 332-343. 10.1016/j.hrtlng.2012.03.001.
Scholte op Reimer W, De Swart E, De Bacquer D, Pyörälä K, Keil U, Heidrich J, Deckers JW, Kotseva K, Wood D, Boersma E: Smoking behaviour in European patients with established coronary heart disease. Eur Heart J. 2006, 27: 35-41.
Costa ML, Cohen JE, Chaiton MO, Ip D, McDonald P, Ferrence R: “Hardcore” definitions and their application to a population-based sample of smokers. Nicotine Tob Res. 2010, 12 (8): 860-864. 10.1093/ntr/ntq103.
Bolman C, de Vries H, van Breukelen G: A minimal-contact intervention for cardiac inpatients: long-term effects on smoking cessation. Prev Med. 2002, 35 (2): 181-192. 10.1006/pmed.2002.1036.
Rigotti NA, Munafo MR, Stead LF: Smoking cessation interventions for hospitalized smokers: a systematic review. Arch Intern Med. 2008, 168 (18): 1950-1960. 10.1001/archinte.168.18.1950.
Rice VH, Stead L: Nursing intervention and smoking cessation: meta-analysis update. Heart Lung. 2006, 35 (3): 147-163. 10.1016/j.hrtlng.2006.01.001.
Feenstra TL, Van Baal PHM, Hoogenveen RT, Vijgen SMC, Stolk E, Bemelmans WJE: Cost-effectiveness of interventions to reduce tobacco smoking in the Netherlands. An application of the RIVM Chronic Disease Model. 2005, RIVM, Bilthoven
Van Baal PHM, Vijgen SMC, Bemelmans WJE, Hoogenveen RT, Feenstra TL: Potential health benefits and cost effectiveness of tobacco tax increases and school intervention programs targeted at adolescents in the Netherlands. 2005, RIVM, Bilthoven
CBO:: Dutch Institute for Health care: Guideline Treatment of Tobacco Dependence. Alphen aan den Rijn: Van Zuiden Communications;. 2009
Gordon L, Graves N, Hawkes A, Eakin E: A review of the cost-effectiveness of face-to-face behavioural interventions for smoking, physical activity, diet and alcohol. Chronic Illn. 2007, 3 (2): 101-129. 10.1177/1742395307081732.
Feenstra TL, Hamberg-van Reenen HH, Hoogenveen RT, Rutten-van Molken MP: Cost-effectiveness of face-to-face smoking cessation interventions: a dynamic modeling study. Value Health. 2005, 8 (3): 178-190. 10.1111/j.1524-4733.2005.04008.x.
Quist-Paulsen P, Lydersen S, Bakke PS, Gallefoss F: Cost effectiveness of a smoking cessation program in patients admitted for coronary heart disease. Eur J Cardiovasc Prev Rehabil. 2006, 13 (2): 274-280. 10.1097/01.hjr.0000192742.81231.91.
Ladapo JA, Jaffer FA, Weinstein MC, Froelicher ES: Projected cost-effectiveness of smoking cessation interventions in patients hospitalized with myocardial infarction. Arch Intern Med. 2011, 171 (1): 39-45. 10.1001/archinternmed.2010.479.
Segaar D: Adoption and implementation of smoking cessation support in health care. 2006, Maastricht University, Maastricht
Bolman C, de Vries H, Mesters I: Factors determining cardiac nurses’ intentions to continue using a smoking cessation protocol. Heart Lung. 2002, 31 (1): 15-24. 10.1067/mhl.2002.119834.
Segaar D, Willemsen MC, Bolman C, De Vries H: Nurse adherence to a minimal-contact smoking cessation intervention on cardiac wards. Res Nurs Health. 2007, 30 (4): 429-444. 10.1002/nur.20204.
Segaar D, Bolman C, Willemsen MC, Vries H: Determinants of adoption of cognitive behavioral interventions in a hospital setting: example of a minimal-contact smoking cessation intervention for cardiology wards. Patient Educ Couns. 2006, 61 (2): 262-271. 10.1016/j.pec.2005.04.004.
Sarna L, Bialous SA, Wells M, Kotlerman J, Wewers ME, Froelicher ES: Frequency of nurses’ smoking cessation interventions: report from a national survey. J Clin Nurs. 2009, 18 (14): 2066-2077. 10.1111/j.1365-2702.2009.02796.x.
Hennrikus DJ, Lando HA, McCarty MC, Klevan D, Holtan N, Huebsch JA, Jestus S, Pentel PR, Pine D, Sullivan S, et al: The TEAM project: the effectiveness of smoking cessation intervention with hospital patients. Prev Med. 2005, 40 (3): 249-258. 10.1016/j.ypmed.2004.05.030.
Wetta-Hall R, Ablah E, Frazier LM, Molgaard C, Berry M, Good M: Factors influencing nurses’ smoking cessation assessment and counseling practices. J Addict Nurs. 2005, 16 (3): 131-135. 10.1080/10884600500203655.
Kotz D, van Litsenburg W, van Duurling R, van Schayck CP, Wesseling GJ: Smoking cessation treatment by Dutch respiratory nurses: reported practice, attitudes and perceived effectiveness. Patient Educ Couns. 2008, 70 (1): 40-49. 10.1016/j.pec.2007.09.002.
Rigotti NA: Helping smokers with cardiac disease to abstain from tobacco after a stay in hospital. Cmaj. 2009, 180 (13): 1283-1284. 10.1503/cmaj.090729.
Smith PM, Burgess E: Smoking cessation initiated during hospital stay for patients with coronary artery disease: a randomized controlled trial. Cmaj. 2009, 180 (13): 1297-1303. 10.1503/cmaj.080862.
Fiore MC, Jaén CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ, Dorfman SF, Froelicher ES, Goldstein MG, Healton CG, et al: Treating Tobacco Use and Dependence: 2008 Update. 2008, Department of Health and Human Services, U.S
Stead LF, Perera R, Bullen C, Mant D, Lancaster T: Nicotine replacement therapy for smoking cessation. Cochrane database of systematic reviews (Online). 2008, 146. 1
Lancaster T, Stead LF: Individual behavioural counselling for smoking cessation. Cochrane database of systematic reviews (Online). 2005, 180 (2): 1292.
Stead LF, Perera R, Lancaster T: Smoking cessation initiated during hospital stay for patients with coronary artery disease: a randomized controlled trial. Cmaj. 2006, 3: 2850.
Freund M, Campbell E, Paul C, McElduff P, Walsh RA, Sakrouge R, Wiggers J, Knight J: Smoking care provision in hospitals: a review of prevalence. Nicotine Tob Res. 2008, 10 (5): 757-774. 10.1080/14622200802027131.
Barth J, Critchley J, Bengel J: Psychosocial interventions for smoking cessation in patients with coronary heart disease. Cochrane database of systematic reviews (Online). 2008, 6886. 1
Kotz D, Wagena EJ, Wesseling G: Smoking cessation practices of Dutch general practitioners, cardiologists, and lung physicians. Respir Med. 2007, 101 (3): 568-573. 10.1016/j.rmed.2006.06.016.
Quist-Paulsen P, Gallefoss F: Randomised controlled trial of smoking cessation intervention after admission for coronary heart disease. BMJ. 2003, 327 (7426): 1254-1257. 10.1136/bmj.327.7426.1254.
Heckman CJ, Egleston BL, Hofmann MT: Efficacy of motivational interviewing for smoking cessation: a systematic review and meta-analysis. Tob Control. 2010, 19 (5):
Soria R, Legido A, Escolano C, Lopez Yeste A, Montoya J: A randomised controlled trial of motivational interviewing for smoking cessation. Br J Gen Pract. 2006, 56 (531): 768-774.
Pedersen SS, Deckers JW, van Os F, Erdman RAM: A multifactorial smoking cessation programme for patients with coronary artery disease: experiences and preliminary results. Neth Heart J. 2002, 10: 48-53.
Perez GH, Nicolau JC, Romano BW, Laranjeira R: Depression: a predictor of smoking relapse in a 6-month follow-up after hospitalization for acute coronary syndrome. Eur J Cardiovasc Prev Rehabil. 2008, 15 (1): 89-94. 10.1097/HJR.0b013e3282f4b212.
Thorndike AN, Regan S, McKool K, Pasternak RC, Swartz S, Torres-Finnerty N, Rigotti NA: Depressive symptoms and smoking cessation after hospitalization for cardiovascular disease. Arch Intern Med. 2008, 168 (2): 186-191. 10.1001/archinternmed.2007.60.
Kuhl EA, Fauerbach JA, Bush DE, Ziegelstein RC: Relation of anxiety and adherence to risk-reducing recommendations following myocardial infarction. Am J Cardiol. 2009, 103 (12): 1629-1634. 10.1016/j.amjcard.2009.02.014.
Kawachi I, Sparrow D, Vokonas PS, Weiss ST: Symptoms of anxiety and risk of coronary heart disease. The Normative Aging Study. Circulation. 1994, 90 (5): 2225-2229. 10.1161/01.CIR.90.5.2225.
Pedersen SS, Lemos PA, van Vooren PR, Liu TK, Daemen J, Erdman RA, Smits PC, Serruys PW, van Domburg RT: Type D personality predicts death or myocardial infarction after bare metal stent or sirolimus-eluting stent implantation: a Rapamycin-Eluting Stent Evaluated at Rotterdam Cardiology Hospital (RESEARCH) registry substudy. J Am Coll Cardiol. 2004, 44 (5): 997-1001. 10.1016/j.jacc.2004.05.064.
Reid RD, Pipe AL, Quinlan B: Promoting smoking cessation during hospitalization for coronary artery disease. Can J Cardiol. 2006, 22 (9): 775-780. 10.1016/S0828-282X(06)70294-X.
Narsavage G, Idemoto BK: Smoking cessation interventions for hospitalized patients with cardio-pulmonary disorders. Online J Issues Nurs. 2003, 8 (2): 8-
Boyle RG, Solberg LI, Asche SE, Boucher JL, Pronk NP, Jensen CJ: Offering telephone counseling to smokers using pharmacotherapy. Nicotine Tob Res. 2005, 7 (Suppl 1): S19-S27.
Solomon LJ, Marcy TW, Howe KD, Skelly JM, Reinier K, Flynn BS: Does extended proactive telephone support increase smoking cessation among low-income women using nicotine patches?. Prev Med. 2005, 40 (3): 306-313. 10.1016/j.ypmed.2004.06.005.
McRobbie H, Hajek P: Nicotine replacement therapy in patients with cardiovascular disease: guidelines for health professionals. Addiction. 2001, 96 (11): 1547-1551. 10.1046/j.1360-0443.2001.961115472.x.
Van Berkel TF, Boersma H, Roos-Hesselink JW, Erdman RA, Simoons ML: Impact of smoking cessation and smoking interventions in patients with coronary heart disease. A systematic review. Eur Heart J. 1999, 20 (24): 1773-1782. 10.1053/euhj.1999.1658.
Rigotti NA, Arnsten JH, McKool KM, Wood-Reid KM, Singer DE, Pasternak RC: The use of nicotine-replacement therapy by hospitalized smokers. Am J Prev Med. 1999, 17 (4): 255-259. 10.1016/S0749-3797(99)00095-1.
Smith PM, Burgess E: Intensive smoking cessation programs for hospitalized coronary patients: a proven intervention in need of implementation. JCOM. 2009, 16 (9): 396-397.
Reid RD, Pipe AL, Quinlan B, Oda J: Interactive voice response telephony to promote smoking cessation in patients with heart disease: a pilot study. Patient Educ Couns. 2007, 66 (3): 319-326. 10.1016/j.pec.2007.01.005.
Taylor CB, Houston Miller N, Killen JD, DeBusk RF: Smoking cessation after acute myocardial infarction: effects of a nurse-managed intervention. Annals Intern Med. 1990, 113 (2): 118-123.
Huttunen-Lenz M, Song F, Poland F: Are psychoeducational smoking cessation interventions for coronary heart disease patients effective? Meta-analysis of interventions. Br J Health Psychol. 2010, 15 (4): 749-777. 10.1348/135910709X480436.
Lichtenstein E, Glasgow RE, Lando HA, Ossip-Klein DJ, Boles SM: Telephone counseling for smoking cessation: rationales and meta- analytic review of evidence. Health Educ Res. 1996, 11 (2): 243-257. 10.1093/her/11.2.243.
Van Emst AJ: Persoonlijke coaching bij stoppen met roken: resultaten van een proces en effectstudie. 2007, Dutch Institute for a Smokefree Future, STIVORO, The Hague
Fernandez E, Schiaffino A, Borrell C, Benach J, Ariza C, Ramon JM, Twose J, Nebot M, Kunst A: Social class, education, and smoking cessation: long-term follow-up of patients treated at a smoking cessation unit. Nicotine Tob Res. 2006, 8 (1): 29-36. 10.1080/14622200500264432.
Ramsay SE, Morris RW, Whincup PH, Papacosta O, Rumley A, Lennon L, Lowe G, Wannamethee SG: Socioeconomic inequalities in coronary heart disease risk in older age: contribution of established and novel coronary risk factors. J Thromb Haemost. 2009, 7 (11): 1779-1786. 10.1111/j.1538-7836.2009.03602.x.
Schaap MM, Kunst AE: Monitoring of socio-economic inequalities in smoking: learning from the experiences of recent scientific studies. Public Health. 2009, 123 (2): 103-109. 10.1016/j.puhe.2008.10.015.
Reid JL, Hammond D, Boudreau C, Fong GT, Siahpush M: Socioeconomic disparities in quit intentions, quit attempts, and smoking abstinence among smokers in four western countries: findings from the International Tobacco Control Four Country Survey. Nicotine Tob Res. 2010, 12 (Suppl): S20-S33. 10.1093/ntr/ntq051.
Hiscock R, Judge K, Bauld L: Social inequalities in quitting smoking: what factors mediate the relationship between socioeconomic position and smoking cessation?. J Public Health. 2011, 33 (1): 39-47. 10.1093/pubmed/fdq097.
Chouinard MC, Robichaud-Ekstrand S: The effectiveness of a nursing inpatient smoking cessation program in individuals with cardiovascular disease. Nurs Res. 2005, 54 (4): 243-254.
Willemsen MC, et al: De effectiviteit van stoppen-met-roken methoden die in Nederland beschikbaar zijn. Neth J Med. 2003, 147: 922-927.
Central Committee on Research involving Human Subjects: The review system in the Netherlands.
Roozenbeek B, Maas AI, Lingsma HF, Butcher I, Lu J, Marmarou A, McHugh GS, Weir J, Murray GD, Steyerberg EW: Baseline characteristics and statistical power in randomized controlled trials: selection, prognostic targeting, or covariate adjustment?. Crit Care Med. 2009, 37 (10): 2683-2690. 10.1097/CCM.0b013e3181ab85ec.
International statistical classification of diseases and related health problems. 10th revision. World Health Organization:. 2007
Berndt NC, Bolman C, de Vries H, Segaar D, van Boven I, Lechner L: Smoking Cessation Treatment Practices: Recommendations for Improved Adoption on Cardiology Wards. J Cardiov Nurs. 2011
Orleans CT, Woolf SH, Rothemich SF, Marks JS, Isham GJ: The top priority: building a better system for tobacco-cessation counseling. Am J Prev Med. 2006, 31 (1): 103-106. 10.1016/j.amepre.2006.03.015.
Gwaltney CJ, Metrik J, Kahler CW, Shiffman S: Self-efficacy and smoking cessation: a meta-analysis. Psychol Addict Behav. 2009, 23 (1): 56-66.
Van Zundert RM, Ferguson SG, Shiffman S, Engels RC: Dynamic effects of self-efficacy on smoking lapses and relapse among adolescents. Health Psychol. 2010, 29 (3): 246-254.
Lock EA, Latham GP: Building a practically useful theory of goal setting and task motivation. A 35-year odyssey. Am Psychol. 2002, 57 (9): 705-717.
Marlatt GA, Donovan DM: Relapse prevention: maintainance strategies in the treatment of addictive behaviors. 2005, The Guilford Press, New York
Prochaska JO, DiClemente CC: Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psych. 1983, 51 (3): 390-395.
Thorndike AN, Rigotti NA: A tragic triad: coronary artery disease, nicotine addiction, and depression. Curr Opin Cardiol. 2009, 24 (5): 447-453. 10.1097/HCO.0b013e32832ed645.
Janszky I, Ahnve S, Lundberg I, Hemmingsson T: Early-onset depression, anxiety, and risk of subsequent coronary heart disease: 37-year follow-up of 49,321 young Swedish men. J Am Coll Cardiol. 2010, 56 (1): 31-37. 10.1016/j.jacc.2010.03.033.
Denollet J, Pedersen SS: Anger, depression, and anxiety in cardiac patients: the complexity of individual differences in psychological risk. J Am Coll Cardiol. 2009, 53 (11): 947-949. 10.1016/j.jacc.2008.12.006.
Pedersen SS, Denollet J: Is type D personality here to stay? Emerging evidence across cardiovascular disease patient groups. Curr Cardiol Rev. 2006, 2: 205-213. 10.2174/157340306778019441.
Gerber Y, Koren-Morag N, Myers V, Benyamini Y, Goldbourt U, Drory Y: Long-term predictors of smoking cessation in a cohort of myocardial infarction survivors: a longitudinal study. Eur J Cardiovasc Prev Rehabil. 2011, 18 (3): 533-541. 10.1177/1741826710389371.
Quist-Paulsen P, Bakke PS, Gallefoss F: Predictors of smoking cessation in patients admitted for acute coronary heart disease. Eur J Cardiovasc Prev Rehabil. 2005, 12 (5): 472-477. 10.1097/01.hjr.0000183914.90236.01.
Bolman C, de Vries H: Psycho-social determinants and motivational phases in smoking behavior of cardiac inpatients. Prev Med. 1998, 27 (5): 738-747. 10.1006/pmed.1998.0352.
Berkel TFv, Vlugt MJvd, Boersma H: Characteristics of smokers and long-term changes in smoking behavior in consecutive patients with myocardial infarction. Prev Med. 2000, 31 (6): 732-741. 10.1006/pmed.2000.0755.
Hughes JR, Stead LF, Lancaster T: Antidepressants for smoking cessation. Cochrane database of systematic reviews (Online). 2007, 31. 1
Silagy C, Lancaster T, Stead L, Mant D, Fowler G: Nicotine replacement therapy for smoking cessation. Cochrane database of systematic reviews (Online). 2004, 146. 3
Mudde AN, Willemsen MC, Kremers S, de Vries H: Meetinstrumenten voor onderzoek naar roken en stoppen met roken. 2006, STIVORO voor een rookvrije toekomst, Den Haag
Velicer WF, Prochaska JO: A comparison of four self-report smoking cessation outcome measures. Addict Behav. 2004, 29 (1): 51-60. 10.1016/S0306-4603(03)00084-4.
West R, Hajek P, Stead L, Stapleton J: Outcome criteria in smoking cessation trials: proposal for a common standard. Addiction. 2005, 100 (3): 299-303. 10.1111/j.1360-0443.2004.00995.x.
Bolman C, de Vries H, van Breukelen G: Evaluation of a nurse-managed minimal-contact smoking cessation intervention for cardiac inpatients. Health Educ Res. 2002, 17 (1): 99-116. 10.1093/her/17.1.99.
Cooke F, Bullen C, Whittaker R, McRobbie H, Chen MH, Walker N: Diagnostic accuracy of NicAlert cotinine test strips in saliva for verifying smoking status. Nicotine Tob Res. 2008, 10 (4): 607-612. 10.1080/14622200801978680.
Koopmanschap M, Burdorf A, Jacob K, Meerding WJ, Brouwer W, Severens H: Measuring productivity changes in economic evaluation: setting the research agenda. PharmacoEconomics. 2005, 23 (1): 47-54. 10.2165/00019053-200523010-00004.
Barnett PG, Wong W, Hall S: The cost-effectiveness of a smoking cessation program for out-patients in treatment for depression. Addiction. 2008, 103 (5): 834-840. 10.1111/j.1360-0443.2008.02167.x.
Turner DA, Paul S, Stone MA, Juarez-Garcia A, Squire I, Khunti K: Cost-effectiveness of a disease management programme for secondary prevention of coronary heart disease and heart failure in primary care. Heart (British Cardiac Society). 2008, 94 (12): 1601-1606. 10.1136/hrt.2007.125708.
Gerhards SA, de Graaf LE, Jacobs LE, Severens JL, Huibers MJ, Arntz A, Riper H, Widdershoven G, Metsemakers JF, Evers SM: Economic evaluation of online computerised cognitive-behavioural therapy without support for depression in primary care: randomised trial. Brit J Psychiat. 2010, 196 (4): 310-318. 10.1192/bjp.bp.109.065748.
Heatherton TF, Kozlowski LT, Frecker RC, Fagerstroem KO: The fagerstroem test for nicotine dependence: a revision of the fagerstroem tolerance questionnaire. Br J Addict. 1991, 86 (9): 1119-1127. 10.1111/j.1360-0443.1991.tb01879.x.
Zigmond AS, Snaith RP: The hospital anxiety and depression scale. Acta Psychiat Scand. 1983, 67 (6): 361-370. 10.1111/j.1600-0447.1983.tb09716.x.
Denollet J: DS14: standard assessment of negative affectivity, social inhibition, and Type D personality. Psychosom Med. 2005, 67 (1): 89-97. 10.1097/01.psy.0000149256.81953.49.
Dijkstra A, De Vries H, Bakker M: Pros and cons of quitting, self-efficacy, and the stages of change in smoking cessation. J Consult Clin Psych. 1996, 64 (4): 758-763.
De Vries H, Mudde A, Leijs I, Charlton A, Vartiainen E, Buijs G, Clemente MP, Storm H, Gonzalez Navarro A, Nebot M, et al: The European Smoking Prevention Framework Approach (EFSA): an example of integral prevention. Health Educ Res. 2003, 18 (5): 611-626. 10.1093/her/cyg031.
Fishbein M, Ajzen I: Predicting and Changing Behavior: The Reasoned Action Approach. 2010
De Vries H, Mesters I, Van der Steeg H, Honing C: The general public’s information needs and perceptions regarding hereditary cancer: an application of the integrated change model. Patient Educ Couns. 2005, 56: 154-165. 10.1016/j.pec.2004.01.002.
Maas CJM, Hox JJ: Sufficient sample sizes for multilevel modeling. Methodology. 2005, 1 (3): 86-92.
McCarty MC, Hennrikus DJ, Lando HA, Vessey JT: Nurses’ attitudes concerning the delivery of brief cessation advice to hospitalized smokers. Prev Med. 2001, 33 (6): 674-681. 10.1006/pmed.2001.0944.
McCarty MC, Zander KM, Hennrikus DJ, Lando HA: Barriers among nurses to providing smoking cessation advice to hospitalized smokers. Am J Health Promot. 2001, 16 (2): 85-87. ii.. 10.4278/0890-1171-16.2.85.
Sarna L, Wewers ME, Brown JK, Lillington L, Brecht ML: Barriers to tobacco cessation in clinical practice: report from a National Survey of Oncology Nurses. Nurs Outlook. 2001, 49 (4): 166-172. 10.1067/mno.2001.115448.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2261/12/33/prepub
Acknowledgements
The study was funded by ZonMw, the Dutch Organisation for Health Research and Development (grant number: 50-50110-96-524). The publication of this manuscript in BMC Cardiovascular Disorders was funded by NWO, the Dutch Organisation for Scientific Research. We are grateful for collaboration with the Dutch Expert Centre for Tobacco Control (STIVORO). We would also like to thank hospital officers, nurses and patients for their participation in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
All authors declare that they have no competing interests.
Authors’ contributions
NB carried out the study and had a major role in data collection, data analysis and data interpretation. She also drafted the manuscript. CB conceived of the study, design, coordination and helped to draft the manuscript. LL, AM, FV and HdV revised the manuscript critically for important intellectual content. All authors read and approved the final version of the manuscript to be published.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Berndt, N., Bolman, C., Lechner, L. et al. Effectiveness of two intensive treatment methods for smoking cessation and relapse prevention in patients with coronary heart disease: study protocol and baseline description. BMC Cardiovasc Disord 12, 33 (2012). https://doi.org/10.1186/1471-2261-12-33
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2261-12-33