Abstract
Background
Activin A is a pleiotrophic regulatory cytokine, the ablation of which is neonatal lethal. Healthy human alveolar macrophages (AMs) constitutively express activin A, but AMs of patients with pulmonary alveolar proteinosis (PAP) are deficient in activin A. PAP is an autoimmune lung disease characterized by neutralizing autoantibodies to Granulocyte-Macrophage Colony Stimulating Factor (GM-CSF). Activin A can be stimulated, however, by GM-CSF treatment of AMs in vitro. To further explore pulmonary activin A regulation, we examined AMs in bronchoalveolar lavage (BAL) from wild-type C57BL/6 compared to GM-CSF knockout mice which exhibit a PAP-like histopathology. Both human PAP and mouse GM-CSF knockout AMs are deficient in the transcription factor, peroxisome proliferator activated receptor gamma (PPARγ).
Results
In sharp contrast to human PAP, activin A mRNA was elevated in mouse GM-CSF knockout AMs, and activin A protein was increased in BAL fluid. Investigation of potential causative factors for activin A upregulation revealed intrinsic overexpression of IFNγ, a potent inducer of the M1 macrophage phenotype, in GM-CSF knockout BAL cells. IFNγ mRNA was not elevated in PAP BAL cells. In vitro studies confirmed that IFNγ stimulated activin A in wild-type AMs while antibody to IFNγ reduced activin A in GM-CSF knockout AMs. Both IFNγ and Activin A were also reduced in GM-CSF knockout mice in vivo after intratracheal instillation of lentivirus-PPARγ compared to control lentivirus vector. Examination of other M1 markers in GM-CSF knockout mice indicated intrinsic elevation of the IFNγ-regulated gene, inducible Nitrogen Oxide Synthetase (iNOS), CCL5, and interleukin (IL)-6 compared to wild-type. The M2 markers, IL-10 and CCL2 were also intrinsically elevated.
Conclusions
Data point to IFNγ as the primary upregulator of activin A in GM-CSF knockout mice which in addition, exhibit a unique mix of M1-M2 macrophage phenotypes.
Similar content being viewed by others
Background
Activin A, a pleiotrophic cytokine belonging to the transforming growth factor-beta (TGF-β) superfamily, is synthesized by many cell types throughout the body [1, 2]. The molecular structure is a disulphide-linked, homodimeric glycoprotein composed of two inhibin βA chains. Activin A was first recognized as an endocrine factor, but is now known to be essential to developmental and repair processes, and total ablation is neonatal lethal [3]. Contrasting regulatory roles have been cited for Activin A in inflammation [4]. Human monocytes synthesize activin A upon stimulation with classical M1 macrophage activation inducers such as GM-CSF, LPS, and IFNγ [5, 6]. Exposure of GM-CSF treated macrophages to anti-Activin A reduces M1 markers and enhances alternative M2 phenotype markers such as IL-10 [7]. Activin A also inhibits monocyte production of IL-1β and enhances IL-1 receptor antagonist production [8]. Interestingly, in severe asthma, activin A may be elevated in serum, and data from animal models suggests that activin A may suppress T helper 2 (Th2) mediated allergic responses [9]. Collectively these observations suggest multifunctional roles for activin A in inflammatory processes.
Maintenance of lung homeostasis is a complex process dependent upon a network of interacting cells and cytokines. GM-CSF is required for alveolar macrophage (AM) function and pulmonary homeostasis [10]. In genetically altered mice homozygous for a disrupted GM-CSF gene (GM-CSF knockout), hematopoiesis is normal but there is accumulation of excess lung surfactant [11, 12]. This surfactant pathology mirrors that of human PAP, an autoimmune disease characterized by high levels of autoantibody to GM-CSF [12–14]. Aerosolized GM-CSF resolves the pulmonary pathology of GM-CSF knockout mice, thus demonstrating that surfactant homeostasis can be influenced by local administration of GM-CSF to the respiratory tract [15].
Previously we reported that healthy human AMs synthesize activin A in response to GM-CSF but AMs of patients with PAP are deficient in activin A [16]. In addition, PAP AMs are deficient in the nuclear transcription factor, Peroxisome Proliferator-activated Receptor, (PPARγ), a regulator of lipid and glucose metabolism that is restored by GM-CSF treatment [17]. PPARγ has also been shown to be a negative regulator of inflammation [18, 19]. Interestingly, alveolar macrophages of GM-CSF knockout mice are also deficient in PPARγ [20]. The role of activin A in the lung has not been established. Because of the phenotypic similarities between human PAP and the GM-CSF knockout mouse, this study was undertaken to investigate activin A regulation in the lung. Initially, it was hypothesized that activin A might be impaired in GM-CSF knockout mice based upon previous data from PAP studies [16].
Results
Activin A and IFNγ are intrinsically elevated in GM-CSF knockout mice as compared to wild-type mice
Unlike previous findings of activin A deficiency in human PAP [16], activin A mRNA expression of BAL cells was significantly (p <0.005) elevated in GM-CSF knockout mice compared to wild-type controls (Figure 1A). Quantification of activin A protein in BAL fluids confirmed mRNA findings with significantly (p < 0.05) elevated protein levels in GM-CSF knockout compared to wild-type (Figure 1B). GM-CSF knockout expression of follistatin, an inhibitor of activin A [21], was similar to wild-type mice (data not shown) and thus could not account for the striking elevation of activin A.
Activin A and IFNγ are intrinsically elevated in GM-CSF knockout lung compared to wild-type mice. Expression of mRNA is shown as a relative fold change as calculated from qPCR. (A) Activin A mRNA expression of BAL cells. (B) Levels of activin A protein in BAL fluids were quantified by ELISA. (C) IFNγ mRNA expression of BAL cells. (D) Cytospin preparations of wild-type C57Bl/6 and GM-CSF knockout BAL cells were stained with anti-IFNγ (green) and DAPI (blue), a nuclear counterstain. Elevated IFNγ protein can be seen in GM-CSF knockout BAL cells (right) compared to wild-type (left).
Intrinsic factors that could potentially affect activin A levels were subsequently investigated in GM-CSF knockout mice. Macrophage colony-stimulating factor (M-CSF) has been reported to be upregulated in GM-CSF knockout mice [22]. Examination of M-CSF in the current study, however, indicated no effect on activin A in vitro in either wild-type or GM-CSF knockout AMs (data not shown). Elevated IFNγ has been reported in lungs of GM-CSF knockout mice [23] therefore intrinsic levels of IFNγ were examined. IFNγ mRNA expression was significantly (p < 0.005) elevated in GM-CSF knockout BAL cells compared to wild-type controls (Figure 1C). Immunocytochemistry of GM-CSF knockout BAL cells confirmed mRNA results and indicated markedly increased expression of intracellular IFNγ protein compared to wild-type (Figure 1D).
IFNγ is not elevated in human PAP BAL cells
In contrast to results from GM-CSF knockout mice, examination of IFNγ expression in human BAL cells from PAP patients revealed no significant increase compared to healthy controls (Figure 2).
Activin A levels are enhanced by IFNγ and reduced by IFNγ blockade
IFNγ has been shown to upregulate activin A expression in human monocytes [5] but AMs have not been studied. Results from 24-hour in vitro cultures of wild-type AMs indicated that IFNγ (100 U/ml) significantly (p < 0.05) increased activin A expression (Figure 3A). To determine whether blockade of IFNγ with specific anti-IFNγ antibody would alter intrinsic activin A expression, unstimulated GM-CSF knockout AMs were cultured in vitro for 24 hours with irrelevant immunoglobulin (Ig) or anti-IFNγ. ELISA analysis of conditioned media indicated that anti-IFNγ reduced activin A protein synthesis compared to irrelevant Ig (Figure 3B) confirming that IFNγ blockade reduced intrinsic activin A production.
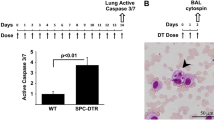
Activin A levels are increased by IFNγ and reduced by IFNγ blockade. (A) IFNγ upregulates activin A mRNA in wild-type alveolar macrophages cultured for 24 hours with IFNγ (100 U/ml) [n = 4]. (B) Antibody to IFNγ represses intrinsic activin A synthesis in GM-CSF knockout alveolar macrophages. GM-CSF knockout alveolar macrophages were cultured with irrelevant IgG or anti-IFNγ for 24 hours and activin A was determined in conditioned media by ELISA (n = 2). (C) BAL cells from GM-CSF knockout mice receiving intratracheal instillation of lentivirus-PPARγ or control lentivirus-EGFP were analyzed for IFNγ and activin A mRNA expression at 10 days post-transduction (n = 5).
Because activin A is intrinsically elevated in PPARγ deficient GM-CSF knockout mice but severely decreased in PPARγ deficient human PAP patients [16], it appeared unlikely that PPARγ would exert a direct effect on activin A. Observations made elsewhere [24] also found no evidence of a PPARγ effect on activin A. We have shown, however, that IFNγ is elevated in macrophage-specific PPARγ knockout mice and significantly reduced after in vivo restoration of PPARγ via a lentivirus vector [25]. We utilized this approach to determine whether PPARγ restoration in GM-CSF knockout mice might reduce IFNγ and thereby reduce activin A. Results supported this action. Ten days post intratracheal inoculation of lentivirus reagents into GM-CSF knockout mice, BAL cell mRNA expression of both IFNγ and activin A was significantly reduced in animals receiving lentivirus-PPARγ compared to controls receiving lentivirus-eGFP (p < 0.05) (Figure 3C).
Human alveolar macrophage activin A is increased by IFNγ
While the above studies clearly defined IFNγ-mediated regulation of activin A in murine alveolar macrophages, it was necessary to confirm this pathway in human alveolar macrophages. In vitro studies demonstrated that IFNγ significantly enhanced activin A protein production (Figure 4) in healthy human alveolar macrophages. Thus activin A synthesis in both human and murine alveolar macrophages is responsive to IFNγ upregulation even though intrinsic activin A levels differ between human and mouse.
GM-CSF BAL cells show intrinsic elevation of both M1 and M2 macrophage phenotypic markers
We and others reported previously that M-CSF gene expression and protein, a cytokine associated with the M2 macrophage phenotype, was elevated in GM-CSF knockout mice [22, 26]. Current data indicate that the M1-associated cytokine, IFNγ (protein and gene expression) is also increased in these mice. Therefore, it was unclear whether GM-CSF knockout BAL cells would express predominantly M1 or M2 profiles. To address this issue, we determined mRNA expression of several M1 and M2 markers in GM-CSF knockout BAL cells. With respect to M1 markers, we examined the IFNγ-regulated target gene, iNOS (Figure 5A), together with CCL5 (Figure 5B), and IL-6 (Figure 5C), and found that all were significantly elevated compared to wild-type mice. The M2 marker, IL-10, has been reported to be suppressed by elevated activin A [7, 27], and in PAP, activin A deficiency is accompanied by elevated IL-10 [16, 28, 29]. Surprisingly, analysis of IL-10 expression in GM-CSF knockout BAL cells revealed significantly elevated levels compared to wild-type mice (Figure 5D). Analysis of another M2-associated marker, CCL2, also indicated significant elevation compared to wild-type mice (Figure 5E). These results suggested that GM-CSF knockout alveolar macrophages might constitute a mixed population of both M1 and M2 phenotypes.
Discussion
The current findings suggest that IFNγ is a major contributory factor to the intrinsic elevation of activin A in AMs. Findings also point out a striking difference in activin A expression in human PAP and GM-CSF knockout mice despite common deficiencies of GM-CSF and PPARγ (summarized in Table 1). In parallel with activin A, GM-CSF knockout mice displayed over-expression of IFNγ [23], a positive regulator of activin A [5]. In contrast, BAL cells of PAP patients do not exhibit elevated IFNγ and activin A is deficient [16].
Elevated IFNγ has been reported previously in the BAL fluids of GM-CSF knockout mice [23]. Our previous studies also found elevated IFNγ expression in macrophage-specific PPARγ knockout mice [25]. Restoration of PPARγ via lentivirus vector in these mice greatly diminished IFNγ expression [25]. In the current study, similar results were seen after PPARγ–lentivirus treatment of GM-CSF knockout mice. Such findings suggest that the PPARγ deficiency present in GM-CSF knockout mice may contribute to elevated IFNγ. GM-CSF has been shown to be a critical upregulator of PPARγ [31, 34]. The total lack of GM-CSF in knockout mice may maintain an extreme PPARγ deficiency which is ineffective at repressing inflammatory mediators such as IFNγ. In human PAP, IFNγ levels are not increased despite PPARγ deficiency, furthermore, GM-CSF is not totally absent [29]. The primary etiology of PAP is considered to be an autoimmune response to GM-CSF in the form of high levels of circulating, neutralizing autoantibody to GM-CSF [13]. It is also possible that additional regulatory mechanisms are present in human lung to help prevent IFNγ buildup in PAP.
The varying characteristics of activated macrophages have led to attempts to categorize activation phenotypes [35–39]. The M1 phenotype is characterized by production of microbial or IFNγ-triggered molecules such as iNOS and IL-12. GM-CSF has been cited as an inducer of M1 phenotypes while M-CSF has been shown to induce the M2 alternative activation phenotype in which IL-10 or TGFβ may be produced [7, 40]. We have shown that M-CSF is elevated in GM-CSF knockout mice [22] and in human PAP [33] which might suggest the presence of an M2 macrophage phenotype (see Table 1). Interestingly, PPARγ, which is deficient in GM-CSF knockout mice, is also a major driver of the M2 phenotype [41]. It has been pointed out however, that macrophage phenotypes were defined by carefully controlled in vitro conditions which may be vastly different from the in vivo milieu [42]. Thus the juxtaposition of both IFNγ and M-CSF in the lungs of GM-CSF knockout mice could produce the novel combination of macrophage activation phenotypes illustrated by elevated M1 (iNOS, CCL5, IL-6) and M2 (IL-10, CCL2) markers (Table 1). Other IFNγ-inducible pro-inflammatory mediators (chemokines CXCL9, CXCL10, and CXCL11) have been noted in the lungs of GM-CSF knockout mice [23]. Previously, we found that MMP-2, a matrix metalloproteinase associated with M-CSF and alternative M2 activation, is also elevated in GM-CSF knockout BAL cells [33].
Conclusions
The current findings extend our previous studies examining pulmonary mechanisms operative in human PAP and the GM-CSF knockout mouse. It is clear that pathways of activin A regulation may utilize GM-CSF or IFNγ as stimulatory factors. In the GM-CSF knockout mouse, lack of GM-CSF may restrict production of sufficient PPARγ to control inflammation. The persistent elevation of both M-CSF and IFNγ may influence AMs to express characteristics of both M1 and M2 phenotypes. The current data emphasize the plasticity of alveolar macrophages in assuming a unique activation phenotype when regulatory pathways become dysfunctional.
Methods
Mice
Animal studies were conducted in conformity with Public Health Service (PHS) Policy on humane care and use of laboratory animals and were approved by the institutional animal care committee. The GM-CSF knockout mice were generated by Dr. Glenn Dranoff and have been previously described [11]. Controls consisted of C57BL/6 wild type mice obtained from Jackson Laboratory (Bar Harbor, ME). BAL cells and fluids were obtained from 8-12 week-old GM-CSF knockout mice and age and gender matched wild-type C57BL/6 controls as previously described [43]. Briefly, cytospins of BAL cells were stained with a modified Wright-Giemsa stain for differentials. A minimum of 100 cells was scored for each lavage. Mean (± SEM) BAL cells from C57BL/6 mice were composed of 98 ± 1% macrophages and 2 ± 1% lymphocytes; GM-CSF knockout BAL cells were composed of 91 ± 2% macrophages and 5 ± 1% lymphocytes. For in vitro studies, BAL cells were plated at 150,000 cells/well in 48-well plates as previously described [25]. Recombinant murine IFNγ was obtained from R&D Systems. Neutralizing anti-IFNγ and control antibodies were purchased from BD Biosciences. For all experiments a minimum of 3 sets of pooled BAL cells from 3-5 mice were used except where indicated.
Human subjects
The protocol was approved by the East Carolina University Institutional Review Board and written informed consent was obtained from all patients and control subjects. Healthy control subjects had no history of lung disease and were not on medication. PAP subjects were recruited from patients undergoing routine clinical evaluation. The diagnosis of idiopathic PAP was confirmed by histopathological examination of material from open lung or transbronchial biopsies as previously described [29]. Alveolar macrophages were derived from bronchoalveolar lavage (BAL) obtained by fiberoptic bronchoscopy as previously described [29]. Differential cell counts were obtained from cytospins stained with a modified Wright’s stain. For PAP patients, the mean BAL cell percentages (means ± SEMs) were: alveolar macrophages, 83 ± 9%, and lymphocytes, 10 ± 5%. Healthy control values were: alveolar macrophages, 93 ± 2% and lymphocytes, 7 ± 2%. For in vitro culture, BAL cells were plated into 24-well plates (300,000 alveolar macrophages per well) or chamber slides (60,000 cells/well) as previously described [16].
RNA purification and analysis
Total RNA was extracted from BAL cells or cultured alveolar macrophages and analyzed by Q-PCR as previously described [25]. RNA specimens were analyzed in duplicate using primer-probe sets for activin A, IL-10, iNOS, CCL2, CCL5, IL-6, IFNγ and GAPDH as previously described [25]. Data were normalized to GAPDH and expressed as fold change in mRNA expression compared to controls values as previously described [44].
Lentivirus plasmid and transduction
The self-inactivating lentivirus expression vector used here has been described previously [45]. Construction of the lentivirus-PPARγ (lenti-PPARγ) and control lentivirus construct has also been described in detail [20, 25]. Control consisted of a lentivirus vector expressing Enhanced Green Fluorescent Protein (eGFP) (lenti-EGFP). Animals received 50 ug of lentivirus vector in 50 μl PBS or PBS alone (sham) by intratracheal instillation. After 10 days, five animals per group were lavaged, BAL differential counts were obtained and RNA was extracted.
Activin A and follistatin protein assays
Activin A or follistatin proteins (pg/ml) in BAL fluids or conditioned media from cultured alveolar macrophages were quantified by ELISA according to the manufacturer’s instructions (Serotec, Raleigh, NC; R&D Systems, Minneapolis, MN).
Immunocytochemistry
Immunocytochemistry for IFNγ was carried out on cytospin samples from freshly isolated BAL cells using rat anti-mouse IFNγ (Santa Cruz Biotechnology,1:100) followed by goat anti-rat IgG (Invitrogen) as described [25]. Slides were counter-stained with DAPI (Invitrogen) to allow nuclear localization.
Statistics
Data were analyzed by student’s t-test using Prism software (GraphPad). Values from treated cells were compared to untreated. Significance was defined as p ≤ 0.05.
Abbreviations
- AM:
-
Alveolar macrophage
- GM-CSF:
-
Granulocyte macrophage colony stimulating factor
- PAP:
-
Pulmonary alveolar proteinosis
- BAL:
-
Bronchoalveolar lavage
- PPARγ:
-
Peroxisome proliferator activated receptor
- IFNγ:
-
Interferonγ
- iNOS:
-
Inducible nitric oxide synthetase.
References
Vale W, Rivier J, Vaughan J, McClintock R, Corrigan A, Woo W: Purification and characterization of an FSH releasing protein from porcine ovarian follicular fluid. Nature. 1986, 321: 776-779. 10.1038/321776a0.
Ling N, Ying SY, Ueno N, Shimasaki S, Esch F, Hotta M: Pituitary FSH is released by a heterodimer of the beta-subunits from the two forms of inhibin. Nature. 1986, 321: 779-782. 10.1038/321779a0.
Matzuk MM, Kumar TR, Vassalli A, Bickenbach JR, Roop DR, Jaenisch R: Functional analysis of activins during mammalian development. Nature. 1995, 374: 354-356. 10.1038/374354a0.
De Kretser DM, O’Hehir RE, Hardy CL, Hedger MP: The roles of activin A and its binding protein, follistatin, in inflammation and tissue repair. Mol Cell Endocrinol. 2012, 359: 101-106. 10.1016/j.mce.2011.10.009.
Shao L, Frigon NL, Sehy DW, Yu AL, Lofgren J, Schwall R: Regulation of production of activin A in human marrow stromal cells and monocytes. Exp Hematol. 1992, 20: 1235-1242.
Abe M, Shintani Y, Eto Y, Harada K, Kosaka M, Matsumoto T: Potent induction of activin A secretion from monocytes and bone marrow stromal fibroblasts by cognate interaction with activated T cells. J Leukoc Biol. 2002, 72: 347-352.
Lacey DC, Achuthan A, Fleetwood AJ, Dinh H, Roiniotis J, Scholz GM: Defining GM-CSF-and macrophage-CSF-dependent macrophage responses by in vitro models. J Immunol. 2012, 188: 5752-5765. 10.4049/jimmunol.1103426.
Ohguchi M, Yamato K, Ishihara Y, Koide M, Ueda N, Okahashi N: Activin A regulates the production of mature interleukin-1beta and interleukin-1 receptor antagonist in human monocytic cells. J Interferon Cytokine Res. 1998, 18: 491-498. 10.1089/jir.1998.18.491.
Karagiannidis C, Hense G, Martin C, Epstein M, Ruckert B, Mantel PY: Activin A is an acute allergen-responsive cytokine and provides a link to TGF-beta-mediated airway remodeling in asthma. J Allergy Clin Immunol. 2006, 117: 111-118. 10.1016/j.jaci.2005.09.017.
Trapnell BC, Whitsett JA: GM-CSF regulates pulmonary surfactant homeostasis and alveolar macrophage-mediated innate host defense. Annu Rev Physiol. 2002, 64: 775-802. 10.1146/annurev.physiol.64.090601.113847.
Dranoff G, Crawford AD, Sadelain M, Ream B, Rashid A, Bronson RT: Involvement of granulocyte-macrophage colony-stimulating factor in pulmonary homeostasis. Science. 1994, 264: 713-716. 10.1126/science.8171324.
Dranoff G, Mulligan RC: Activities of granulocyte-macrophage colony-stimulating factor revealed by gene transfer and gene knockout studies. Stem Cells. 1994, 12 (Suppl 1): 173-182.
Kitamura T, Tanaka N, Watanabe J, Uchida K, Kanegasaki S, Yamada Y: Idiopathic pulmonary alveolar proteinosis as an autoimmune disease with neutralizing antibody against granulocyte/macrophage colony-stimulating factor. J Exp Med. 1999, 190: 875-880. 10.1084/jem.190.6.875.
Trapnell BC, Whitsett JA, Nakata K: Pulmonary alveolar proteinosis. N Engl J Med. 2003, 349: 2527-2539. 10.1056/NEJMra023226.
Reed JA, Ikegami M, Cianciolo ER, Lu W, Cho PS, Hull W: Aerosolized GM-CSF ameliorates pulmonary alveolar proteinosis in GM-CSF-deficient mice. Am J Physiol. 1999, 276: L556-L563.
Bonfield TL, Barna BP, John N, Malur A, Culver DA, Kavuru MS: Suppression of activin A in autoimmune lung disease associated with anti-GM-CSF. J Autoimmun. 2006, 26: 37-41. 10.1016/j.jaut.2005.10.004.
Bonfield TL, Raychaudhuri B, Malur A, Abraham S, Trapnell BC, Kavuru MS: PU.1 regulation of human alveolar macrophage differentiation requires granulocyte-macrophage colony-stimulating factor. Am J Physiol Lung Cell Mol Physiol. 2003, 285: L1132-L1136.
Pascual G, Fong AL, Ogawa S, Gamliel A, Li AC, Perissi V: A SUMOylation-dependent pathway mediates transrepression of inflammatory response genes by PPAR-[gamma]. Nature. 2005, 437: 759-763. 10.1038/nature03988.
Glass CK, Saijo K: Nuclear receptor transrepression pathways that regulate inflammation in macrophages and T cells. Nat Rev Immunol. 2010, 10: 365-376. 10.1038/nri2748.
Thomassen MJ, Barna BP, Malur A, Bonfield TL, Farver CF, Malur A: ABCG1 is deficient in alveolar macrophages of GM-CSF knock-out mice and patients with pulmonary alveolar proteinsosis. J Lipid Res. 2007, 48: 2762-2768. 10.1194/jlr.P700022-JLR200.
Mather JP: Follistatins and alpha 2-macroglobulin are soluble binding proteins for inhibin and activin. Horm Res. 1996, 45: 207-210. 10.1159/000184789.
Shibata Y, Berclaz YP, Chroneos ZC, Yoshida M, Whitsett JA, Trapnell BC: GM-CSF regulates alveolar macrophage differentiation and innate immunity in the lung through PU.1. Immunity. 2001, 15: 557-567. 10.1016/S1074-7613(01)00218-7.
Su YC, Rolph MS, Hansbro NG, Mackay CR, Sewell WA: Granulocyte-macrophage colony-stimulating factor is required for bronchial eosinophilia in a murine model of allergic airway inflammation. J Immunol. 2008, 180: 2600-2607.
Weigert J, Neumeier M, Wanninger J, Schober F, Sporrer D, Weber M: Adiponectin upregulates monocytic activin A but systemic levels are not altered in obesity or type 2 diabetes. Cytokine. 2009, 45: 86-91. 10.1016/j.cyto.2008.10.017.
Malur A, Mccoy AJ, Arce S, Barna BP, Kavuru MS, Malur AG: Deletion of PPARγ in alveolar macrophages is associated with a Th-1 pulmonary inflammatory response. J Immunol. 2009, 182: 5816-5822. 10.4049/jimmunol.0803504.
Bonfield TL, Thomassen MJ, Farver CF, Abraham S, Koloze MT, Zhang X: Peroxisome proliferator-activated receptor-{gamma} regulates the expression of alveolar macrophage macrophage colony-stimulating factor. J Immunol. 2008, 181: 235-242.
Sierra-Filardi E, Puig-Kroger A, Blanco FJ, Nieto C, Bragado R, Palomero MI: Activin A skews macrophage polarization by promoting a proinflammatory phenotype and inhibiting the acquisition of anti-inflammatory macrophage markers. Blood. 2011, 117: 5092-5101. 10.1182/blood-2010-09-306993.
Thomassen MJ, Raychaudhuri B, Bonfield TL, Malur A, Abraham S, Barna BP: Elevated IL-10 inhibits GM-CSF synthesis in pulmonary alveolar proteinosis. Autoimmunity. 2003, 36: 285-290. 10.1080/0891693031000152688.
Thomassen MJ, Yi T, Raychaudhuri B, Malur A, Kavuru MS: Pulmonary alveolar proteinosis is a disease of decreased availability of GM-CSF rather than an intrinsic cellular defect. Clin Immunol. 2000, 95: 85-92. 10.1006/clim.2000.4859.
Bonfield TL, Russell D, Burgess S, Malur A, Kavuru MS, Thomassen MJ: Autoantibodies against granulocyte macrophage colony-stimulating factor are diagnostic for pulmonary alveolar proteinosis. Am J Respir Cell Mol Biol. 2002, 27: 481-486. 10.1165/rcmb.2002-0023OC.
Bonfield TL, Farver CF, Barna BP, Malur A, Abraham S, Raychaudhuri B: Peroxisome proliferator-activated receptor-gamma is deficient in alveolar macrophages from patients with alveolar proteinosis. Am J Respir Cell Mol Biol. 2003, 29: 677-682. 10.1165/rcmb.2003-0148OC.
Bonfield TL, John N, Malur A, Barna BP, Culver DA, Kavuru MS: Elevated monocyte chemotactic proteins 1, 2, and 3 in pulmonary alveolar proteinosis are associated with chemokine receptor suppression. Clin Immunol. 2005, 114: 79-85. 10.1016/j.clim.2004.09.004.
Bonfield TL, Swaisgood CM, Barna BP, Kavuru MS, Thomassen MJ: Elevated gelatinous activity in pulmonary alveolar proteinosis: role of macrophage-colony stimulating factor. J Leukoc Biol. 2006, 79: 133-139.
Ricote M, Huang JT, Welch JS, Glass CK: The peroxisome proliferator-activated receptor-γ (PPARγ) as a regulator of monocyte/macrophage function. J Leukoc Biol. 1999, 66: 733-739.
Mosser DM, Edwards JP: Exploring the full spectrum of macrophage activation. Nat Rev Immunol. 2008, 8: 958-969. 10.1038/nri2448.
Gordon S, Martinez FO: Alternative activation of macrophages: mechanism and functions. Immunity. 2010, 32: 593-604. 10.1016/j.immuni.2010.05.007.
Liu G, Yang H: Modulation of macrophage activation and programming in immunity. J Cell Physiol. 2013, 228: 502-512. 10.1002/jcp.24157.
Gordon S: Alternative activation of macrophages. Nat Rev Immunol. 2003, 3: 23-35. 10.1038/nri978.
Sica A, Mantovani A: Macrophage plasticity and polarization: in vivo veritas. J Clin Invest. 2012, 122: 787-795. 10.1172/JCI59643.
Fleetwood AJ, Lawrence T, Hamilton JA, Cook AD: Granulocyte-macrophage colony-stimulating factor (CSF) and macrophage CSF-dependent macrophage phenotypes display differences in cytokine profiles and transcription factor activities: implications for CSF blockade in inflammation. J Immunol. 2007, 178: 5245-5252.
Chawla A: Control of macrophage activation and function by PPARs. Circ Res. 2010, 106: 1559-1569. 10.1161/CIRCRESAHA.110.216523.
Weidenbusch M, Anders HJ: Tissue microenvironments define and get reinforced by macrophage phenotypes in homeostasis or during inflammation, repair and fibrosis. J Innate Immun. 2012, 4: 463-477. 10.1159/000336717.
Malur A, Baker AD, McCoy AJ, Wells G, Barna BP, Kavuru MS: Restoration of PPARgamma reverses lipid accumulation in alveolar macrophages of GM-CSF knockout mice. Am J Physiol Lung Cell Mol Physiol. 2011, 300: L73-L80. 10.1152/ajplung.00128.2010.
Livak KJ, Schmittgen TD: Analysis of relative gene expression data using real-time quantitative PCR and the 2(−Delta Delta C(T)) Method. Methods. 2001, 25: 402-408. 10.1006/meth.2001.1262.
Malur AG, Chattopadhyay S, Maitra RK, Banerjee AK: Inhibition of STAT 1 phosphorylation by human parainfluenza virus type 3 C protein. J Virol. 2005, 79: 7877-7882. 10.1128/JVI.79.12.7877-7882.2005.
Acknowledgements
This work was funded by North Carolina Biotechnology Center FRG-1013 and NIH RO1 AI164153 to MJT.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
HD contributed to acquisition of the data, analysis and interpretation of data, drafting of the manuscript and final approval of the version to be published; BPB contributed to the design, analysis and interpretation of data, drafting of the manuscript and final approval of the version to be published; AM contributed to the conception and design, acquisition of the data, analysis and interpretation of data and final approval of the version to be published; AGM contributed to acquisition of the data and final approval of the version to be published; MSK contributed to the acquisition of data and final approval of the version to be published; MJT contributed to the conception and design, acquisition of data, analysis and interpretation of data, drafting of the manuscript and final approval of the version to be published. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Dalrymple, H., Barna, B.P., Malur, A. et al. Alveolar macrophages of GM-CSF knockout mice exhibit mixed M1 and M2 phenotypes. BMC Immunol 14, 41 (2013). https://doi.org/10.1186/1471-2172-14-41
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2172-14-41