Abstract
Background
Cobalt chromium coronary stents are increasingly being used in percutaneous coronary interventions. There are, however, no reliable data about the characteristics of unfolding and visibility of this stent alloy in vivo. The aim of this study is to compare cobalt chromium coronary stents with conventional stainless steel stents using intracoronary ultrasound.
Methods
Twenty de novo native coronary stenoses ≤ 20 mm in length (target vessel reference diameter ≥ 2.5 and ≤ 4.0 mm) received under sequential intracoronary ultrasound either a cobalt chromium stent (Multi-Link Vision®; n = 10) or a stainless steel stent (Multi-Link Zeta®; n = 10).
Results
For optimal unfolding, the cobalt chromium stent requires a higher balloon deployment pressure (13.90 ± 2.03 atm) than the stainless steel stent (11.50 ± 2.12 atm). Furthermore, the achieved target vessel diameter of the cobalt chromium stent (Visibility-Index QCA/IVUS Multi-Link Vision®1.13 / Multi-Link Zeta® 1.04) is more easily overrated by Quantitative Coronary Analysis.
Conclusion
These data indicate that stent material-specific recommendations for optimal implantation pressure and different stent material with an equal design should both be considered in interpreting QCA-analysis.
Similar content being viewed by others
Background
With the addition of coronary stents to percutaneous coronary intervention (PCI), the incidence of re-stenosis has been significantly reduced. Unfortunately, re-stenosis rates still range from 16% to 32 %[1]. Efforts to reduce re-stenosis include coating of conventional stents and use of alternative materials and design. Drug Eluting Stents (DES) are already established in clinical practice[2], whereas little data are available with respect to innovative stent material.
Cobalt chromium represents a more biocompatible material that is being increasingly used in coronary stents (Guidant Multi-Link Vision®/Guidant Corporation, Driver-Stent®/Medtronic, Costar-Stent®/Biotronic). In comparison with stainless steel, cobalt chromium has a higher radial strength and radiopacity for similar electronegativity. This allows for the production of thinner struts with a similar radiological visibility[3].
Although, results of two cobalt chromium registries[3, 4] are already published, there are no data describing the basic characteristics of unfolding of a cobalt chromium stent. This information would be important to know in developing clinical recommendations for different alloys, since optimal inflation and complete adherence to vessel wall are key factors affecting the incidence of re-stenosis.
We investigated the balloon deployment pressure-related behaviour of a cobalt chromium stent (Multi-Link Vision®), comparing it to a similarly designed conventional stainless steel stent (Multi-Link Zeta®) using intravascular ultrasound. We also evaluated radiological visibility of both stents and the influence of radiological visibility on QCA-analysis.
Methods
Eighteen consecutive patients (14 men, 4 women, mean age 61 ± 9 years) with twenty single, de novo native coronary stenoses ≤ 20 mm in length were blindly randomised to either a Multi-Link Vision® cobalt chromium stent (n = 10) or to a Multi-Link Zeta® stainless steel stent (n = 10). Additional criteria for inclusion were age ≥ 18 years, clinical angina and/or a positive functional study and a target vessel reference diameter ≥ 2.5 mm and ≤ 4 mm.
Patients were excluded from the study if they presented with cardiogenic shock, acute coronary syndrome, intracoronary thrombus, vessel occlusion, target lesions in the left main artery, ostial or bifurcational stenosis, calcification of ≥ 180° of vessel circumference by intravascular ultrasound (IVUS), diabetes and/or known hypersensitivity to aspirin and clopidogrel. The study was approved by the ethics committee of the University of Cologne and all patients signed written informed consent before participating.
Percutaneous coronary intervention was performed in accordance with standard clinical procedures, and stent implantation without predilatation ("primary stenting") was encouraged. Pretreatment included an oral clopidogrel loading dose of 300 mg and aspirin 500 mg the day before intervention. Peri-interventional, weight-adapted heparin was given intravenously with consecutive control of activated clotting time. Implantation was performed with a primary balloon deployment pressure of 10 atmospheres (atm). If IVUS target criteria were not reached, a standardised further inflation with 13 atm and possibly 16 atm including additional IVUS control, followed. Post-procedural an oral antiplatelet therapy with clopidogrel 75 mg/day for at least 4 weeks and aspirin 100 mg/day as standard medication was obligatory.
Intravascular ultrasound imaging was performed after administering 0.2 mg of intracoronary nitroglycerin using a 30 MHz transducer within a 3.2 Fr imaging sheath (SCIMED/BSC, Maple Grove, Minnesota) and automatic transducer pullback of 0.5 mm/s. The distal and proximal reference segment was within 3 – 5 mm of the lesion or stent without a relevant stenosis (<20%). Quantitative Coronary Analysis (QCA, Pie Medical Imaging) was done for proximal and distal reference diameter (RD), minimal lumen diameter (MLD), diameter of stenosis and acute lumen gain.
The primary endpoint was balloon deployment pressure once IVUS criteria were reached. IVUS target criteria were similar to preceding studies[5], with a minimal lumen area (MLA) after stenting > 90% (for reference lumen area (RLA) ≤ 9.0 mm2), > 80% (for RLA > 9.0 mm2), a MLA > 90% of proximal RLA at the proximal end of the stent and a complete adherence to vessel wall. A secondary endpoint was angiographic visibility as generated by minimal lumen diameter in QCA and IVUS-analysis, respectively.
Statistical analysis was performed with SPSS, version 12.0 (SPSS Inc., 2003). Continuous variables are expressed as mean ± SD.
Results
Clinical data were comparable for both groups, except for the number of smokers (Vision® n = 7 / Zeta® n = 3), and were comparable to prior stent studies. Twenty five stents (13 ML Vision®, 12 ML Zeta®) were implanted with a 100% procedural success. An intraprocedural dissection in 3 patients required implantation of additional stents. In case of stent overlap, the same stent type was used.
The angiographic mean reference vessel diameter was 3.02 ± 0.40 mm (ML Vision® 3.04 ± 0.34 mm / ML Zeta® 2.99 ± 0.47 mm). Mean minimum lumen diameter was 0.70 ± 0.32 mm, which corresponds to a mean diameter stenosis of 76.5 ± 9.8% (Table 1).
Pre-dilatation was necessary in one case, in which a 1.5 × 20 mm balloon was used and dilatation pressure was 8 atm.
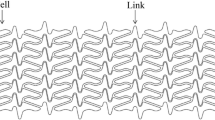
Mean balloon deployment pressure when IVUS criteria were reached was 13.90 ± 2.03 atm for Multi-Link Vision® and 11.50 ± 2.12 atm for Multi-Link Zeta® (Figure 1).
A mean post-procedural QCA-MLD of 3.32 ± 0.41 mm and a mean MLD of 3.07 ± 0.41 mm by intravascular ultrasound generated a mean Visibility-Index of 1.08. For Multi-Link Vision® (3.34 ± 0.34 mm [QCA] vs. 2.95 ± 0.17 mm [IVUS]), mean Visibility-Index was 1.13. The mean Visibility-Index for Multi-Link Zeta® (3.31 ± 0.48 mm [QCA] vs. 3.19 ± 0.55 mm [IVUS]) was 1.04 (Table 2).
Conclusion
Different material properties of alloys used in a specific stent design represent a key consideration in clinical practice that should be taken into account, particularly with regard to balloon deployment pressure. Furthermore, the achieved post-procedure lumen diameter as measured by QCA is more easily overestimated for the cobalt chromium stent than for the stainless steel stent due to material properties.
Based on these results, further investigation of material-specific changes in stent unfolding is necessary to guide and optimize the clinical implantation practice.
Limitations
The number of twenty de novo native coronary stenoses is small, but relevant preliminary differences were found that should be further explored in future investigations.
Three standardised balloon deployment pressures (10, 13, 16 atm) were chosen because every change between balloon and IVUS-catheter increases the risk of vascular damage. Thus, a continuous, incremental escalation of balloon deployment pressure is not practical in vivo.
References
Kastrati A, Hall D, Schömig A: Long-term outcome after coronary stenting. Curr Control Trials Cardiovasc Med. 2000, 1: 48-54. 10.1186/CVM-1-1-048.
Babapulle MN, Joseph L, Belisle P, Brophy JM, Eisenberg MJ: A hierarchical Bayesian meta-analysis of randomised clinical trials of drug-eluting stents. Lancet. 2004, 364: 558-9. 10.1016/S0140-6736(04)16850-5.
Kereiakes DJ, Cox DA, Hermiller JB, Midei MG, Bachinsky WB, Nukta ED, Leon MB, Fink S, Marin L, Lansky AJ, Guidant Multi-Link Vision Stent Registry Investigators: Usefulness of a cobalt chromium coronary stent alloy. Am J Cardiol. 2003, 92: 463-6. 10.1016/S0002-9149(03)00669-6.
Sketch MH, Ball M, Rutherford B, Popma JJ, Russell C, Kereiakes DJ, on behalf of the Driver Investigators: Evaluation of the Medtronic (Driver) cobalt-chromium alloy coronary stent system. Am J Cardiol. 2005, 95: 8-12. 10.1016/j.amjcard.2004.08.055.
Mudra H, di Mario C, de Jaegere P, Figulla HR, Macaya C, Zahn R, Wennerblom B, Rutsch W, Voudris V, Regar E, Henneke KH, Schachinger V, Zeiher A, OPTICUS (OPTimization with ICUS to reduce stent restenosis) Study Investigators: Randomized comparison of coronary stent implantation under ultrasound or angiographic guidance to reduce stent restenosis (OPTICUS Study). Circulation. 2001, 104: 1343-9.
Acknowledgements
This study was supported by a grant from Guidant Corporation (Indianapolis, IN, USA).
Author information
Authors and Affiliations
Corresponding author
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Hagemeister, J., Baer, F.M., Schwinger, R.H. et al. Compliance of a cobalt chromium coronary stent alloy – the COVIS trial. Trials 6, 17 (2005). https://doi.org/10.1186/1468-6708-6-17
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1468-6708-6-17