Abstract
Background
The impact of interventions on the progressive course of COPD is currently assessed by the slope of the annual decline in FEV1 determined from serial measurements of the post-, in preference to the pre-, bronchodilator FEV1. We therefore compared the yearly slope and the variability of the slope of the pre- versus the post-bronchodilator FEV1 in men and women with mild to moderate COPD who participated in the 5-year Lung Health Study (LHS).
Methods
Data were analyzed from 4484 of the 5887 LHS participants who had measurements of pre- and post-bronchodilator FEV1 at baseline (screening visit 2) and all five annual visits. The annual rate of decline in FEV1 (±SE) measured pre- and post-bronchodilator from the first to the fifth annual visit was estimated separately using a random coefficient model adjusted for relevant covariates. Analyses were performed separately within each of the three randomized intervention groups. In addition, individual rates of decline in pre- and post-bronchodilator FEV1 were also determined for each participant. Furthermore, sample sizes were estimated for determining the significance of differences in slopes of decline between different interventions using pre- versus post-bronchodilator measurements.
Results
Within each intervention group, mean adjusted and unadjusted slope estimates were slightly higher for the pre- than the post-bronchodilator FEV1 (range of differences 2.6-5.2 ml/yr) and the standard errors around these estimates were only minimally higher for the pre- versus the post-bronchodilator FEV1 (range 0.05-0.11 ml/yr). Conversely, the standard deviations of the mean FEV1 determined at each annual visit were consistently slightly higher (range of differences 0.011 to 0.035 L) for the post- compared to the pre-bronchodilator FEV1. Within each group, the proportion of individual participants with a statistically significant slope was similar (varying by only 1.4 to 2.7%) comparing the estimates from the pre- versus the post-bronchodilator FEV1. However, sample size estimates were slightly higher when the pre- compared to the post-bronchodilator value was used to determine the significance of specified differences in slopes between interventions.
Conclusion
Serial measurements of the pre-bronchodilator FEV1 are generally sufficient for comparing the impact of different interventions on the annual rate of change in FEV1.
Similar content being viewed by others
Background
The annual rate of change in FEV1 has been measured in numerous observational and interventional studies for nearly half a century. In the seminal work of Fletcher and Peto [1], on a cohort of 1136 smokers, an accelerated annual rate of loss of FEV1 was observed in a subset of smokers who were believed to be particularly vulnerable to the injurious effects of cigarette smoking leading to the development of chronic obstructive pulmonary disease. This observation established an accelerated annual loss of lung function as a characteristic feature of COPD supporting subsequent definitions of COPD as a progressive disease [2], although recent longitudinal data suggest that COPD is not always progressive [3]. In the aftermath of the Fletcher and Peto publication [1], longitudinal population-based studies have examined the influence of both smoking and other exposures, such as ambient air pollution, on lung function decline, mostly using the FEV1 measured without bronchodilator administration [4–6]. Beginning with the first Lung Health Study (LHS I), [7, 8], the preferred method of determining the slope of decline in other interventional studies, including trials of inhaled corticosteroids [9–12], N-acetycysteine [13] and long-acting inhaled bronchodilators with or without inhaled corticosteroids [14, 15], has relied mainly on the post-bronchodilator FEV1 measurement.
The decision to use the slope of the post- as opposed to the pre-bronchodilator FEV1 as the primary outcome in LHS I was based, in part, on the assumption that bronchodilator administration would reduce the influence of varying circadian and day-to-day bronchomotor tone on the measurement of FEV1[16–18], thereby reducing the variability of the annual slope of FEV1 decline, and potentially increasing the power of the study to show a significant difference in the slope of decline in FEV1 between the study groups. However, to date, it has not been established that use of the post- compared to the pre-bronchodilator FEV1 is associated with a lower variance of the slope of annual change in FEV1 in patients with COPD or that there is less month-to-month variability than in the pre-bronchodilator measurements. The objective of the present analysis was to use data from LHS I participants to compare the between-sessions variability of the pre- versus post-bronchodilator FEV1 near the beginning of the study and the variance of the annual slope of change in the pre- versus post-bronchodilator FEV1 measured over five years. If no difference in the variability of the slope of annual change in FEV1 can be discerned between these two methods of measuring the rate of change, then use of only the pre-bronchodilator measurement would simplify longitudinal studies of lung function change without compromising the ability to detect possible differences between different treatment regimens.
Methods
Study population and FEV1 measurements
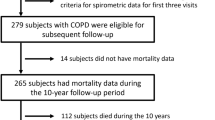
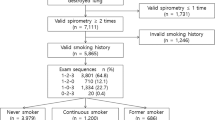
LHS I was a ten-center randomized clinical trial of 5,887 middle-aged smokers with the objective of determining whether an intervention program combining intensive smoking cessation counseling and an inhaled anticholinergic bronchodilator could slow the rate of decline in FEV1 over a five-year follow-up period during which subjects underwent pre- and post-bronchodilator spirometry annually [7, 8]. Entry criteria included a history of current regular smoking, ≥10 pack years of smoking, age 35-60 yrs and the absence of other significant pulmonary or other medical illness, as well as the presence of mild to moderate airflow limitation (see below). A history of asthma treated with regularly scheduled medication was also exclusionary. Potential subjects underwent 3 separate screening visits (Figure 1). At the first screening visit, spirometry was not rigidly controlled, but spirometric methods used at the 2nd and 3rd screening visits and at all visits post-randomization were performed using the same centrally supplied and certified equipment and were rigorously standardized and monitored to maintain suitable quality. At all of these spirometry sessions, three acceptable and two repeatable maneuvers were required from up to eight forced expirations using LHS-specific standards for acceptability and repeatability, as previously described [7, 19], and the largest FEV1 and FVC values from acceptable and repeatable maneuvers were recorded. Bronchodilator response to two inhalations of isoproterenol (200 μg) from a metered-dose inhaler was determined at the 2nd screening visit and at all subsequent visits, except the 3rd screening visit. At the latter visit, bronchoprovocation with methacholine was performed, the details of which have been published previously [20].
Eligible participants had to have a pre-bronchodilator ratio of FEV1 to FVC of ≤0.70 and a pre-bronchodilator FEV1 ≤90% predicted and ≥55% predicted [21] at the 2nd screening visit. The “pre-bronchodilator” measurement was defined as the measurement obtained before the administration of a short-acting bronchodilator [isoproterenol] as part of the study, as well as after an adequate washout period following any prior use of bronchodilator medication by participants. Eligible participants were randomized in a 1:2 ratio to receive “usual care” (UC) or “special intervention” (SI). The SI group received a four-month intensive smoking cessation program followed by a five-year relapse prevention program, along with physician advice and nicotine replacement. In addition, participants in the SI group were randomly assigned in a 1:1 ratio and in a double-blind fashion to receive either placebo (SIP group) or ipratropium bromide two inhalations, 18 μg per inhalation (SIA group), which they were instructed to take three times daily for the five-year duration of the study. The UC group received only brief counseling on entry into the study. All subjects were requested to return each year for a total of five post-randomization annual visits during each of which smoking status was determined (and verified by salivary cotinine and end-expired measurements of carbon monoxide) and spirometry was performed both before and after isoproterenol using the same methodology and rigorous standards as applied during the 2nd and 3rd screening visit (Figure 1). In addition, the SI group returned for a four-month post-randomization visit that included pre- and post-bronchodilator spirometry. Informed consent was obtained from all participants at each of the ten LHS clinical centers.
Written informed consent was obtained from all participants originally enrolled in the LHS. The study was approved by the institutional review boards of each of the participating centers and was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice guidelines.
Statistical analysis
Data from the LHS were reanalyzed to compare the annual FEV1 decline measured pre- bronchodilator versus post-bronchodilator for the three study groups (UC, SIP and SIA), separately. Baseline characteristics for the three treatment groups were summarized using descriptive statistics. Among the 5887 subjects in the original study, only the 4484 (~76%) who had measurements at both baseline and all five annual follow-up visits were included in this analysis. Demographic characteristics and mean baseline FEV1 values were compared between the included and excluded subgroups. For each included treatment group, the annual rate of decline in FEV1 measured pre- and post- bronchodilator from the first to the fifth annual visit was estimated separately using a random coefficient model. Time (year), gender, age, BMI, two-point methacholine concentration-FEV1 O’Connor slope [22] and baseline number of cigarettes smoked per day were included in the model as fixed effects; intercept and time (i.e., slope of FEV1) were random effects. The two-point slope was computed as the percent change in FEV1 at the highest delivered dose of methacholine from the postdiluent control FEV1 divided by the highest concentration of methacholine (in mg/ml) that the subject received. Since, on average, either no change or an increase in FEV1 was observed from baseline to the first annual visit, followed by a linear decline in FEV1 from annual visits 1 through 5 in the entire LHS 1 population, for the present analysis all slopes were calculated using data from the first through the fifth annual visit. In addition, for each subject individually a linear regression model was used to obtain the annual rate of decline in FEV1 for that subject from annual visits 1 through 5. The number of subjects who had a statistically significant individual annual rate of change in FEV1 (p < 0.05) and the mean and standard deviation of the slopes for those with and without a significant individual rate of change were tabulated for pre- and post- bronchodilator FEV1 separately within each of the three treatment groups.
Based on the estimated slope (annualized change in FEV1) and standard deviation determined for the three parallel LHS treatment groups, we performed sample size calculations to determine whether there are differences in the sample sizes needed to demonstrate a significant difference in slopes of FEV1 decline between the UC group and the SIP group, as well as between the UC group and the SIA group, using the pre- versus the post-bronchodilator FEV1. For these calculations, we assumed equal sizes for each group, a normal distribution of the annualized change in FEV1, a significance level of 0.05 (alpha) and 80% power (beta = 0.2) to detect the observed difference in the annualized change in FEV1 between the two study groups in each pair (UC and SIP, and UC and SIA) using a two-sided t-test. Sample sizes were also calculated for the SIA and SIP groups versus a hypothetical comparison study group with an assumed slope difference of 10, 15 and 20 ml/yr, respectively, to investigate possible differences in sample sizes using the pre-bronchodilator vs. the post-bronchodilator FEV1 for determining the slope.
All analyses were performed using SAS software.
Results
Average baseline characteristics for participants who were included and excluded in the analysis are shown in Table 1 for each study group. Baseline features were modestly but significantly different between the included and excluded participants for the following: in the SIA group, excluded subjects were more often male and non-Caucasian, had a slightly higher BMI and reported smoking more cigarettes/day and a greater number of pack-years; in the SIP group, excluded patients reported smoking more cigarettes/day; and in the UC group, excluded subjects had a lower FEV1. No significant differences in baseline characteristics across the subjects in the three treatment groups were noted, except for gender and BMI. The SIA group had more females than the SIP and UC groups (p = 0.009 and 0.006, respectively) and the BMI was slightly lower in the SIA group than the SIP and UC groups (p = 0.0077 and 0.0721, respectively). The latter differences were very small and unlikely to be clinically significant.
The linear slopes (mean and standard deviation) of the pre- and post-bronchodilator FEV1 change from annual visits 1 through 5 both unadjusted and adjusted (for age, gender, cigarettes/day and log of the 2-point methacholine concentration-FEV1 response slope) are shown for the UC, SIP and SIA groups separately in Table 2. The mean values (± SD) of the pre- and post-bronchodilator FEV1 at baseline and each annual visit are shown in Figure 2 and Additional file 1. Regardless of the adjustment for covariates, the mean slopes of both the pre- and post-bronchodilator FEV1 are steeper by 12.2-15.5 ml/yr for the UC group compared to both SI groups (Table 2), as previously reported for the post-bronchodilator slope in the entire LHS 1 population [7]. However, within each group, the mean unadjusted slope estimates are only slightly higher for the pre- than the post-bronchodilator FEV1 (range of differences 2.6-5.2 ml/yr) and the standard errors around these estimates are only minimally higher for the pre- vs. the post-bronchodilator FEV1 (range 0.05-0.11 ml/yr). Similarly, the mean adjusted slope estimates are slightly higher for the pre- than the post-bronchodilator FEV1 in each group (range of differences 2.5-5.1 ml/yr) and the standard errors around these estimates are only minimally higher for the pre- vs. the post-bronchodilator FEV1 (range 0.04-0.11 ml/yr). The similarity of the slopes of the pre- vs. post-bronchodilator FEV1 from annual visits 1 through 5 is readily discerned by inspection of curves drawn for the mean values of the pre- vs. post-bronchodilator FEV1 at each annual visit over this time period (Figure 2). Moreover, the standard deviations of the mean FEV1 at each of these time points are very similar on comparison of the pre- and post-bronchodilator values ( Additional file 1).
Table 3 shows the percentage of participants in each randomized group who exhibited a statistically significant individual slope of pre- and post-bronchodilator FEV1 change over annual visits 1 through 5. Within each group, the percentage of individual participants with a statistically significant slope was similar between the slopes estimated from the pre- versus the post-bronchodilator FEV1, the differences varying by only 1.4-2.7%. The percentage of UC participants who exhibited a statistically significant slope of both pre- and post-bronchodilator FEV1 decline (40.2 and 38.7%, respectively) was significantly higher than the percentage of participants in each SI group (range 25.4-30.5%) who demonstrated a statistically significant slope, most likely attributable to the generally steeper significant slopes in the UC group (range of means 53.5-56.7 ml/yr) than in the two SI groups (range of means 37.5-43.2 ml/yr) as a consequence of the significantly higher rates for sustained quitting in the SI groups than the UC group (7).
The differences of the pre- and post-bronchodilator FEV1 in the SIP group between screening visit 2 and month 4 reflect the month-to-month variability in FEV1 unconfounded by the introduction of maintenance treatment with a bronchodilator ( Additional file2). The mean difference in pre-bronchodilator FEV1 from screening visit 2 to month 4 is actually smaller than that for the post-bronchodilator measurements, although the variances are similar.
Using the pre- and post-bronchodilator FEV1, the sample sizes required 1) to demonstrate significant differences between the UC vs. SIA group and the UC vs. SIP group are shown in Table 4 and 2) to demonstrate a significant slope difference of 10, 15 and 20 ml/yr for the SIA and the SIP groups vs. the hypothetical comparison group are shown in Table 5. A smaller N was required to show a difference between the SIP and the UC group using the pre-bronchodilator compared to the post-bronchodilator FEV1, while, conversely, a larger N was needed to show a difference between the SIA and UC groups using the pre- compared to the post-BD FEV1 (Table 4). These differences in sample size estimates comparing the UC group with each of the SI groups are related to the differences in the means of the slopes (effect size) between the groups, as well as the differences in the SD shown in Table 2. On the other hand, comparison of the sample sizes needed to show statistical significance for specified differences in slope between each SI group and a hypothetical comparison group using pre- vs. post-bronchodilator data showed that slightly larger numbers of subjects would be required using pre- than post-bronchodilator FEV1 measurements, especially for relatively small hypothetical differences in slope (Table 5).
Discussion
We found that, for the UC and the two SI groups, both the mean slope and the variance of the slope of the annual change in the pre-bronchodilator FEV1 were fairly similar to the slope and variance of the slope determined using the post-bronchodilator FEV1 (Table 2), suggesting that the post-bronchodilator measurement offered little advantage over the pre-bronchodilator FEV1 for tracking the course of COPD in LHS participants. These findings are consistent with our observation of comparable between-month variability of the pre- and the post-bronchodilator FEV1 in the SIP group ( Additional file 1).
Our results indicating that the variability of the slope of annual change in FEV1 is not substantially reduced by determining the slope based on the post-bronchodilator compared to the pre-bronchodilator FEV1 are further supported by the observation that, within each group, the proportion of participants with a statistically significant individual slope of decline in the post-bronchodilator FEV1 was similar to the proportion with a statistically significant individual slope determined from the pre-bronchodilator FEV1 since the statistical significance of the individual slope of FEV1 decline is influenced, in large part, by the variance of the slope.
On the other hand, any possible advantage, with respect to savings in time and effort, of restricting the measurement of FEV1 to only the pre-bronchodilator value for studies of the impact of an intervention on the annual rate of change in FEV1 must be balanced by the comparative size of the sample required, with adequate power, to show a significant difference between the interventions. The sample size is driven by both the effect size and the variance of the annual slope. Therefore, we determined the sample sizes needed to show a significant difference between the UC group and each of the SI groups, as well as to show significant specified differences (10, 15 and 20 ml/yr) between each of the SI groups and a hypothetical comparison group. Inconsistent differences in the required sample size were shown for determining significant differences between the UC group and each of the SI groups using pre- vs. post-bronchodilator data (Table 4). However, in general, a modestly larger sample size was required to demonstrate significance for specified differences in slope between a hypothetical comparison group and each SI group, particularly for relatively small assumed differences in slope (Table 5), thus potentially incurring an additional cost for recruitment of a somewhat larger sample size if only the pre-bronchodilator FEV1 were measured.
In studies conducted over approximately the last 25 years comparing the impact of different therapeutic interventions in COPD on the progression of the disease, it became common practice to use the post-bronchodilator, rather than the pre-bronchodilator, FEV1 for calculating the annual rate of change as the primary measure of the course of the disease [7, 9–15]. The rationale for this practice, is likely to have been based on the belief that the post-bronchodilator value better “standardizes” the FEV1 than the pre-bronchodilator value, since the pre-bronchodilator value could be affected by day-to-day and within-day variability in bronchomotor tone, as well as by residual bronchodilation from the last dose of either rescue or maintenance bronchodilator medication if an adequate washout period was not observed. The goal of this “standardization” would be to reduce the variability of the FEV1 and thus better estimate the slope of the annual change in FEV1, thereby decreasing the sample size required to demonstrate a significant difference in slope between therapeutic interventions.
On the other hand, serial spirometry studies evaluating the time course of FEV1 over 24 hrs have failed to show any difference in the circadian pattern of FEV1 comparing responses to placebo with those to bronchodilator medication [23, 24]. Moreover, the short-term response to a bronchodilator is influenced by several factors [25] in consequence of which the post-bronchodilator increment in FEV1 is itself highly variable both within and between patients with COPD [26, 27]. One of the factors affecting the acute response to a bronchodilator measured in terms of the absolute improvement in FEV1 is the pre-bronchodilator FEV1 % predicted, such that, across the spectrum of GOLD stages of severity from moderate to very severe, the magnitude of the FEV1 response has been observed to be largest in patients with moderate COPD and smallest in patients with very severe COPD [28, 29]. Consequently, as COPD progresses from moderate to very severe airflow obstruction over time, one would expect a progressively smaller absolute increment in FEV1 after bronchodilator administration, which could influence the annual slope of decline in the post-bronchodilator FEV1. In contrast, patients with relatively mild airflow obstruction, as observed on the baseline visit of the LHS, exhibit a minimal response to a bronchodilator [7, 30], in contrast to the much greater response in patients with moderate to severe airflow obstruction, possibly due to the effect of Poisseuille’s Law [31]. Consequently, when such patients progress to a greater degree of airflow obstruction, one would expect a relatively larger acute response to a bronchodilator, as was demonstrated in the continuing and intermittent smokers over the 11 years of follow-up in the LHS [30]. Whether because of these or other factors, the yearly slope of FEV1 and the variance of this slope do, in fact, differ between the pre- vs. the post-bronchodilator FEV1 has heretofore not been specifically addressed.
This study has several strengths as well as weaknesses. The major strength is the exceptional rigor with which the centralized spirometry assessments were performed and continually monitored for quality control [19], thus minimizing variability due to technical factors. Other strengths include the large number of subjects studied (nearly 6,000, over three-quarters of whom completed all annual visits) and the relatively high representation of females (35%) compared to most other interventional studies in COPD. A weakness is the somewhat limited spectrum of COPD represented by the subjects, all of whom had only mild to moderate airflow obstruction at entry into the study and generally had not been prescribed maintenance bronchodilator or other medication for their COPD, so that our findings might not apply to patients with severe or very severe COPD nor to nonsmokers and those without COPD. Similarly, the average age of the participants (~48 yrs) was much lower than that of COPD patients participating in pharmacotherapeutic trials. The imbalance in some of the baseline characteristics between the ~76% of participants included in the analysis and the remainder who were excluded might be another limitation. To address this limitation, we re-analyzed the data to determine the estimated annual change in FEV1 in the total LHS population of 5,887 participants using multiple imputation of the missing data (see Additional file3). The results of this analysis yielded differences between the mean slopes and slope variances determined from the pre- versus the post-bronchodilator FEV1 that were very similar to those found when the analysis was restricted only to those who completed all annual visits. Another limitation is that COPD was defined by a pre-bronchodilator ratio of FEV1 to FVC of <70%, rather than the currently recommended post-bronchodilator ratio [2]. Consequently, some subjects with fully reversible airflow obstruction were included in the study. There were 503 subjects whose post-bronchodilator FEV1 % predicted was 90% or greater, and 1246 whose post-bronchodilator FEV1/FVC % was 70% or greater. On the other hand, subjects who were receiving regularly prescribed medication for asthma were excluded.
We conclude that serial measurements of the pre-bronchodilator FEV1 appear to be adequate for comparing the impact of different interventions on the annual rate of change in FEV1, thus simplifying the design of such longitudinal studies. On the other hand, relying only on the pre-bronchodilator measurement might require a slightly larger sample size to show significant differences between interventions, particularly if relatively small differences in slope are observed. Moreover, measurement of the response to a bronchodilator is important at baseline to exclude the presence of fully reversible airflow obstruction and, in addition, to describe the degree of partial reversibility for descriptive and potential analytic purposes, although the pre-bronchodilator FEV1 has been found to be just as accurate as the post-bronchodilator measurement in predicting mortality in the LHS [32]. In addition, if only the pre-bronchodilator measurement is performed over time, care should be taken to ensure that subjects withhold their concomitant bronchodilator medication for a suitable washout period prior to spirometry testing. Furthermore, whether or not post-bronchodilator measurements are also performed, subjects should be studied at approximately the same time of day to minimize variability due to the influence of circadian rhythm.
Abbreviations
- COPD:
-
Chronic obstructive pulmonary disease
- FEV1:
-
Forced expired volume in 1 second
- UC:
-
Usual Care group
- SI:
-
Special Intervention group
- SIP:
-
Special Intervention group assigned to placebo
- SIA:
-
Special Intervention group assigned to active bronchodilator
- S2:
-
Screen 2 visit
- M4:
-
Month 4 visit.
References
Fletcher C, Peto R: The natural history of chronic airflow obstruction. Br Med J. 1977, 1: 1645-1648. 10.1136/bmj.1.6077.1645.
Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD). 2010, http://www.goldcopd.org,
Casanova C, de Torres JP, Aguirre-Jaime A, Pinto-Plata V, Marin JM, Cordoba E, BAz R, kKCote C, Celli BR: The progression of chronic obstructive pulmonary disease is heterogeneous. The experience of the BODE cohort. Am J Respir Crit Care Med. 2011, 184: 1015-1021. 10.1164/rccm.201105-0831OC.
Detels R, Tashkin DP, Sayre JW, Rokaw SN, Massey FJ, Coulson AH, Wegman DH: The UCLA population studies of CORD. X. A cohort study of changes in respiratory function associated with chronic exposure to SOX, NOX and hydrocarbons. Am J Public Health. 1991, 81: 350-359. 10.2105/AJPH.81.3.350.
Tashkin DP, Detels R, Simmons M, Liu H, Coulson AH, Sayre J, Rokaw S: The UCLA Population Studies of Chronic Obstructive Respiratory Disease XI. Impact of air pollution and smoking on annual change in forced expiratory volume in one second. Am J Respir Crit Care Med. 1994, 149: 1209-1217.
Kohansal R, Martinez-Camblor P, Agusti A, Buist AS, Mannino DM, Soriano JB: The natural history of chronic airflow obstruction revised. An analysis of the Framingham Offsping Cohort. Am J Respir Crit Care Med. 2009, 180: 3-10. 10.1164/rccm.200901-0047OC.
Anthonisen NR, Connett JE, Kiley JP, Altose MD, Bailey WC, Buist AS, Conway WA, Enright PL, Kanner RE, O’Hara P, Owens GR, Scanlon PD, Tashkin DP, Wise RA, for the Lung Health Study Research Group, for the Lung Health Study Research Group: Effects of smoking intervention and the use of an inhaled anticholinergic bronchodilator on the rate of decline of FEV1. The Lung Health Study. JAMA. 1994, 272: 1497-1505. 10.1001/jama.1994.03520190043033.
Scanlon PD, Connett JE, Waller LA, Altose MD, Bailey WC, Buist AS, Tashkin DP, for the Lung Health Study Research Group, for the Lung Health Study Research Group: Smoking cessation and lung function in mild-to-moderate chronic obstructive pulmonary disease: the lung health study. Am J Respir Crit Care Med. 2000, 161: 381-390.
Pauwels RA, Lofdahl C-G, Laitinen LA, Schouten JP, Postma DS, Pride NB, Ohlsson SV: Long-term treatment with inhaled budesonide in persons with mild chronic obstructive pulmonary disease who continue smoking. N Eng J Med. 1999, 340: 1948-1953. 10.1056/NEJM199906243402503.
Burge PS, Calverley PMA, Jones PW, Spencer S, Anderson JA, Maslen TK: Randomised, double-blind, placebo-controlled study of fluticasone propionate in patients with moderate to severe chronic obstructive pulmonary disease: the ISOLDE trial. BMJ. 2000, 320: 1297-1303. 10.1136/bmj.320.7245.1297.
Vesto J, Sorensen T, Lange P, Brix A, Torre P, Viskum K: Long-term effect of inhaled budesonide im mild and moderate chronic obstructive pulmonary disease: a randomized controlled trial. Lancet. 1999, 353: 1819-1823. 10.1016/S0140-6736(98)10019-3.
The Lung Health Study Research Group: Effect of inhaled triamcinolone on the decline in pulmonary function in chronic obstructive pulmonary disease. N Engl J Med. 2000, 343: 1902-1909.
Decramer M, Rutten-van Molken M, Dekhuijzen PNR, Troosters T, van Herwaarden C, Pellegrino R, van Schayck CPO, Olivieri D, Del Donno M, De Backer W, Lankhorst I, Ardia A: Effects of N-acetylcysteine on outcomes in chronic obstructive pulmonary disease (Bronchitis Randomized on NAC Cost-Utility Study, BRONCUS): a randomized placebo-controlled trial. Lancet. 2005, 365: 1552-1560. 10.1016/S0140-6736(05)66456-2.
Tashkin DP, Celli B, Senn S, Burkhart D, Kesten S, Menjoge S, Decramer M, for the UPLIFT study investigators, for the UPLIFT study investigators: A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med. 2008, 359: 1543-1554. 10.1056/NEJMoa0805800.
Celli BR, Thomas NE, Anderson JA, Ferguson GT, Jenkins CR, Jones PW, Vestbo J, Knobil K, Yates JC, Calverley PMA: Effect of pharmacotherapy on rate of decline in lung function in chronic obstructive pulmonary disease. Results from the TORCH study. Am J Respir Crit Care Med. 2008, 178: 332-338. 10.1164/rccm.200712-1869OC.
Postma DS, Hoeter GH, vd Mark TW, Reig RP, Sluiter HJ: The effects of oral slow-release terbutaline on the circadian variation in spirometry and arterial blood gas levels in patients with chronic airflow obstruction. Chest. 1985, 87: 653-657. 10.1378/chest.87.5.653.
Pennock BE, Rogers RM, McCaffree DR: Changes in measured spirometric indices. What is significant?. Chest. 1981, 80: 97-99. 10.1378/chest.80.1.97.
Nisar M, Earis JE, Pearson MG, Calverley PMA: Acute bronchodilator trials in chronic obstructive pulmonary disease. Am Rev Respir Dis. 1991, 146: 555-559.
Enright PL, Johnson LR, Connett JE, voelker H, Buist AS: Spirometry in the Lung Health Study: I. Methods and quality control. Am Rev Respir Dis. 1991, 143: 1215-1233.
Tashkin DP, Altose MD, Bleecker ER, Connett JE, Kanner RE, Lee WW, Wise R, for the Lung Health Study Research Group, for the Lung Health Study Research Group: The Lung Health Study: Airway responsiveness to inhaled methacholine in smokers with mild to moderate airflow limitation. Am Rev Respir Dis. 1992, 145: 301-310.
Crapo RD, Morris AH, Gardner RM: Reference spirometric values using techniques and equipment that meet ATS recommendations. Am Rev Respir Dis. 1981, 123: 659-664.
O’Connor GT, Sparrow D, Weiss ST: A prospective longitudinal study of methacholine airway responsiveness as a predictor of pulmonary function decline: the Normative Aging Study. Am J Respir Crit Care Med. 1995, 152: 87-92.
Calverley PMA, Lee A, Towse L, van Noord J, Witeck TJ, Kelsen S: Effect of tiotropium bromide on circadian variation in airflow limitation in chronic obstructive pulmonary disease. Thorax. 2003, 58: 855-860. 10.1136/thorax.58.10.855.
van Noord JA, Aumann JL, Janssens E, Verhaert J, Smeets JJ, Meuller A, Cornelissen PJG: Effects of tiotropium with and without formoterol on airflow obstruction and resting hyperinflation in patients with COPD. Chest. 2006, 129: 509-517. 10.1378/chest.129.3.509.
Tashkin DP: Measurement and Significance of the Bronchodilator Response. Bronchodilators: Theory and Practice. Edited by: Jenne JW. 1987, Marcel Dekker, Inc, New York, 535-613.
Calverley PMA, Burge PS, Spencer S, Anderson JA, Jones PW, for the ISOLDE Study Investigators, for the ISOLDE Study Investigators: Bronchodilator reversibility testing in chronic obstructive pulmonary disease. Thorax. 2003, 58: 659-664. 10.1136/thorax.58.8.659.
Dorinsky PM, Reisner C, Ferguson GT, Menjoge SS, Serby CW, Witek TJ: The combination of ipratropium and albuterol optimizes pulmonary function reversibility testing in patients with COPD. Chest. 1999, 115: 966-971. 10.1378/chest.115.4.966.
Tashkin DP, Celli B, Decramer M, Liu D, Burkhart D, Cassino C, Kesten S: Bronchodilator responsiveness in patients with COPD. Eur Respir J. 2008, 31: 742-750. 10.1183/09031936.00129607.
Celli B, Tashkin DP, Rennard SI, McElhattan J, Martin U: Bronchodilator responsiveness and onset of effect with budesonide/formoterol pMDI in patients with COPD. Respir Med. 2011, 105: 1176-1188. 10.1016/j.rmed.2011.02.020.
Anthonisen NR, Lindgren PG, Tashkin DP, Kanner RE, Scanlon PD, Connett JE: Bronchodilator response in mild to moderate COPD over 11 years: Results from the Lung Health Study. Eur Respir J. 2005, 26: 45-51. 10.1183/09031936.05.00102604.
DuBois AB: Resistance to breathing. Handbook of Physiology, Section 3: Respiration, vol 1. Edited by: Fenn WO, Rahn H. 1964, American Physiological Society, Washington, DC, 451-452.
Mannino DM, Diaz-Guzman E, Buist S: Pre- and post-bronchodilator lung function as predictors of mortality in the Lung Health Study. Respir Res. 2011 Oct 12, 12: 136-10.1186/1465-9921-12-136.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
DT helped design the study, contributed to the collection of data, developed the concept for the statistical analysis, assisted in the interpretation of the results and drafted the manuscript; DH and EK assisted in the interpretation of the results and contributed to the writing of the manuscript; HW and NL carried out the statistical analysis; JC and RE oversaw the statistical analysis and assisted in the interpretation of the results. All authors read and approved the final manuscript.
Electronic supplementary material
12931_2012_1229_MOESM1_ESM.doc
Additional file 1: Mean (±SD) pre- and post-bronchodilator FEV 1 at baseline and each annual visit by intervention group. (DOC 53 KB)
12931_2012_1229_MOESM2_ESM.doc
Additional file 2: Mean values ± SD of pre- and post-bronchodilator FEV 1 at the 2ndscreening visit (S2) and the 4 month visit (M4) and the mean M4-S2 differences ± SD in SIP participants (N=1427). (DOC 44 KB)
12931_2012_1229_MOESM3_ESM.doc
Additional file 3: Estimates of annual change in FEV 1 (in liters) using multiple imputation of missing data in the entire LHS population*. (DOC 119 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Tashkin, D.P., Wang, HJ., Halpin, D. et al. Comparison of the variability of the annual rates of change in FEV1 determined from serial measurements of the pre- versus post-bronchodilator FEV1 over 5 years in mild to moderate COPD: Results of the lung health study. Respir Res 13, 70 (2012). https://doi.org/10.1186/1465-9921-13-70
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1465-9921-13-70