Abstract
Background
The information about paediatric meningiomas is poor. The purpose of this study was to review the clinical characteristic, treatment considerations and prognosis of paediatric meningiomas.
Methods
We retrospectively reviewed a series of 32 paediatric patients with meningiomas who received surgical resection at the Affiliated Hospital of Qingdao University between January 2002 and December 2010.
Results
The study group included 17 boys and 15 girls (range: 2–18 years, mean: 13.7 years). Thirteen patients were in the first decade of life and 19 patients were in the second decade. The most common symptoms were headache (33.3%) and epilepsy (25%), followed by cranial nerve dysfunction: distortion of commissure, vision disorder, acoasma and unconsciousness. The size of lesions was ranged 35–65 mm (mean 42.3 mm). Of these 32 patients, 16 were revealed WHO class I meningiomas, 5 were WHO class II, and 11 manifested WHO class III. Nine of 32 patients met the criteria that had tumor recurrence within follow-up.
Conclusions
Paediatric meningiomas usually have larger size, higher pathologic grade and unusual location. The influential factors for recurrence include lesion location, histological features and extent of removal. Complete tumor resection is the best choice to prevent recurrence and improve the prognosis.
Similar content being viewed by others
Background
Meningioma is one of the most common intracranial tumors in adulthood, constituting 20–30% of all intracranial neoplasm [1, 2]. The paediatric meningiomas are relatively uncommon. Meningiomas compose no more than 3% of all childhood primary intracranial tumors [2,3,4,5]. Previous literatures reported that paediatric meningiomas have different clinical features and prognosis compared with those of adult [6]. The information about paediatric meningiomas is poor, only several studies have attempted to analyze the characteristics of childhood meningiomas.
The aim of this clinical retrospective study was to review the characteristics, therapy considerations and outcomes of paediatric meningiomas in our center and other previous published data are reviewed.
Methods
A total of 32 paediatric patients (age under 18 years) with intracranial meningiomas underwent surgical therapy in the department of Neurosurgery, the Affiliated Hospital of Qingdao University from January 2002 to December 2010. The diagnosis was based on imageology, intra-operative findings and pathological. The clinical data were retrieved from the hospital information system. We recorded the age, sex, complaint, diagnosis, neoplasm location and size, surgical management and prognosis of all patients. All patients were evaluated with head computer tomography (CT) and/or magnetic resonance imaging (MRI) before and after operation. The radiological characteristics were analyzed. The extent of tumor resection was determined by reviewing operation record and postoperative radiological findings. All of the specimens obtained in the operation were histological verified and classified according to the World Health Organization classification 2000. The routine follow-up were scheduled at 1-, 6-, and 12-month, and thereafter annually after operation through telephone with the patients or their family members. The duration of follow-up was 6 months to 8 years (median 4 years).
Results
Of the 32 patients reported here, 17 were boys and 15 girls. The male-to-female ratio was 1.13:1. Age ranges from 2 to 18 years, with a mean age of 13.7 years. Thirteen patients were in the first decade of life and 19 patients were in the second decade. Twenty-eight patients were under 16-year-old and 14 were girls.
The most common symptoms were headache (33.3%) and epilepsy (25%), followed by cranial nerve dysfunction: distortion of commissure (16.7%), vision disorder (8.3%), acoasma (8.3%) and unconsciousness (8.3%). Two patients had cranial nerve dysfunction. Both of them were VII nerve affected, with the sign of commissure distortion. No motor deficit had been found in our series. The duration of clinical history ranged from 1 day to 10 years, mean 18.6 months. No child underwent chemo/radiotherapy before craniotomy.
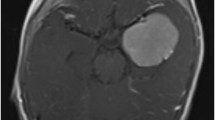
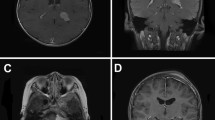
Fifteen of 32 cases were convexity meningiomas, 5 cases were skull base meningiomas, 10 cases were intraventricular, and 2 cases were infratentorial lesions. Three children had evidence of neurofibromatosis type 2 (NF-2) (Fig. 1.). The size of lesion was ranged 35–65 mm (mean 42.3 mm) in their maximum diameter. The size of 15 patients’ lesions was bigger than 5 cm in our series, and the biggest one located in intraventricular was 7.2 cm. The mean diameter size was 5.4 cm. Signal intensities on T1 and T2 weighted images of the lesions were variable, similar to adults. Dural attachment absent was found in 14 patients, and only one patients showed calcification signs on CT scanning. A low incidence of cystic formation in our series, only one cystic tumor had been found.
All 32 patients received surgical treatment. Microsurgical techniques were used routinely for all cases. The lesion was totally removed in 19 children, and sub-totally in 13 patients whose lesion located in the cerebral ventricle. If the tumor involved the skull bone and dura, the involved skull bone and dura was removed as much as possible. The big bone defect was repaired with normal bone. The normal bone was acquired from rib or ilium. The skull defect was repaired if the defect was bigger than 3 cm in diameter. The dural defect was repaired with fascia lata graft or artificial dural graft. All the specimens were sent to the pathology department for histological analysis. According to the histological analysis, 16 patients had grade I/benign type, 5 patients had grade II/atypical type, and 11 patients had grade III/anaplastic variant. The severe complication following operation was unfound. No perioperative deaths, vascular injuries, or complications lead to new neurological deficits in this series. There was no childhood patient underwent the routine chemo/radiotherapy after craniotomy.
Nine of 32 patients (28.13%) met a recurrence within follow-up. The recurrence information was studied in comparison with operational resection and histopathology. Out of 19 children who underwent gross total removed, recurrence was found in 4 children (21.05%). Five of the 13 patients who underwent subtotal removed had recurrence (38.46%). In 16 cases of benign type tumors, recurrence was seen in 4 patients (57.1%). In 11 cases of anaplastic variant tumors, recurrence was seen in 5 patients (45.45%). Once again surgical treatment was performed for 8 cases. The histological progression was observed in 6 cases (75%). A 17 years old boy with anaplastic variant tumor rejected surgical treatment again, underwent focal radiotherapy and died after 9 months because of cerebral hernia.
Discussion
Meningiomas are usually slowly growing benign tumors originating from arachnoidal cap cells of the meninges [7]. They constitute 20–30% of all intracranial neoplasms in adulthood. These patients are most commonly in middle-aged and gerontal. Paediatric meningiomas are relatively rare. They account for less than 3% of all primary intracranial neoplasms in childhood. In our series, they range in age from 2 to 18 years, with a mean age of 13.7 years, similar with previous studies [2, 8,9,10]. The male-to-female ratio is 1:2 for adulthood meningiomas, with female predominance. Males were predominance in paediatric meningiomas with the ratio is about 2–3:1 [11, 12]. Of our 32 cases, the ratio was 1.13:1, slight male predilection. While the reason is not clear, the sex hormones may play a role [3, 4, 13]. This suggests that the pathogenesis might be different between adulthood and childhood.
Although there is no confirmed evidence for the pathogenesis of primary paediatric meningiomas, many risk factors may be relational, such as ionizing radiation and association with neurofibromatosis. Approximately 10% of paediatric meningiomas were associated with neurofibromatosis [14]. There is a clear association between paediatric meningiomas and neurofibromatosis type 2 (NF-2) [15,16,17]. Rushing EJ et al. reported that about 72% paediatric patients with meningioma had NF-2 gene deletion, the NF2 gene deletion is not somatic deletion, only in tumor tissues [18, 19]. This phenomenon suggests that these two kinds’ neoplasm may be sharing the similar pathogenesis. Cranial ionizing radiation is one of the risk factors for meningiomas. The arachnoidal tissue in the meninges of children has higher radioactive susceptive, but radiation-induced meningiomas rarely manifest in childhood [18]. We didn’t find any radiation-induced signs in our series.
Meningiomas in childhood may develop anywhere in the cranium. They are usually observed in exceptional locations, such as: infratentorial, intraventricular, or skull base [10, 20]. Convexity of brain also is the most frequent location for paediatric meningiomas as adulthood. Intraventricular meningiomas are common in childhood, and most of them in the lateral cerebral ventricle. Arachnoid cells inclusions in the choroid plexus and velum interpositum may play a role [21]. The size of meningiomas is frequently larger in childhood than in adulthood [16]. More than 45% of the paediatric meningiomas are bigger than 5 cm in diameter 11. The mean diameter size of lesion was 5.4 cm in these 32 cases. The strong compensation ability of the cavitas cranii and the acataphasia of children may be the major reasons. Dural attachment or a dural tail sign on neuroimaging is usually absent, but cystic and calcified are not rare [9, 22]. Cysts were reported in 24% paediatric meningiomas compared with 2–7% in adulthood [14, 20]. Dural attachment absence may be due to that the tumor genesis from leptomeningeal elements lodging within the brain parenchyma or the ventricles. MRI characteristics of paediatric meningiomas are similar to adulthood. On MRI, the tumors are usually isointense to hypointense on T1-weighted imaging, isointense to hypointense on T2-weighted imaging and exhibit good contrast enhancement [8]. Heterogeneous enhancement was seen in malignant meningiomas.
The symptoms of paediatric meningiomas are nonspecific, variably according to its location and size. Headache is the most common symptom of paediatric meningiomas [9], and epilepsy is another common symptom. Previous literatures reported that the incidence of epilepsy was about 25–35%, and most related to the supratentorial cases [11, 13]. It is no noticeable physical characteristics to discriminate meningiomas from other diseases which could increase the intracranial pressure. Chronic increased intracranial pressure can also induce increased head circumference and late fontanel closure in younger children [13]. Cranial nerve dysfunction was caused by local compression and increased intracranial pressure, usually involving the II, III, IV, VI, VII and VIII nerves [11].
Surgical operation is the fundamental treatment for intracranial meningiomas. Complete tumor resection is the best choice to prevent recurrence and improve the prognoses. Surgical resection in paediatric meningiomas is a neurosurgical challenge considering their difficulty of early diagnosis, larger size at presentation, relatively less blood volume in children, occurrence of unusual location, tight adherence to vital vessels and nerves, and the various risks due to prolonged surgery like hypothermia, massive blood transfusion, etc. [11, 21]. Microsurgical techniques should be performed for each childhood tumor. The lesion and dural origin/attachment should be removed totally because the higher recurrence risk. Control of hemorrhage intraoperative and especial intensive care postoperative is necessary.
The WHO classification divides meningiomas into three grades: grade I, benign; grade II, atypical; and grade III, anaplastic/malignant [2, 15]. The histology of the meningiomas is different between childhood and adulthood. The ratio of malignant in paediatric meningiomas is 7–16%, significantly higher than in adulthood [11, 20, 23]. The influential factors for recurrence include location of the lesion, histological features and extent of surgical removal. From previous studies, the prognosis of paediatric meningiomas was worse than that of adults. A conservative therapy is unacceptable in children patients. The brain development had been impacted notwithstanding asymptomatic present. Meningiomas in children could grow vary large with asymptomatic. It usually too late to perfect operation until symptomatic appear. Adjuvant postoperative focal or systematic radiotherapy still remains controversial for younger patients. Uncertainty in prognosis, little evidence to support and the potential adverse long-term affect on brain function were the major reasons [8, 11, 14, 20]. Ionizing radiation also is one of the important reasons for childhood neoplasm pathogenesis [18]. Those patients should consider receive radiotherapy if their tumors were malignant or recurrent and couldn’t be removed completely. Only one child underwent recurrence and anaplastic variant meningioma received radiotherapy, but died after 9 months because of cerebral hernia. Chemotherapy was not considered in the treatment of meningiomas.
Conclusions
The paediatric meningiomas are relatively uncommon and are slight predominantly in males. These meningiomas are rare in the first decade of life. They usually have larger size, higher pathologic grade and unusual location compared with adult meningiomas. The symptoms of paediatric meningiomas are nonspecific, variably according to its location and size. The influential factors of recurrence include location of the lesion, histological features and extent of surgical removal. Complete tumor resection is the best choice to prevent recurrence and improve the prognoses.
Abbreviations
- CT:
-
Computed tomography
- MRI:
-
Magnetic Resonance Imaging
- NF-2:
-
Neurofibromatosis type 2
- WHO:
-
World Health Organization
References
Peng J, Liang ZG, Li KC. Intracranial malignant meningioma with cerebrospinal fluid dissemination: a case report. Chin Med J. 2011;124:1597–9.
Jaiswal S, Vij M, Mehrotra A, Jaiswal AK, Srivastava AK, Behari S. A clinicopthological and neuroradiological study of paediatric meningioma from a single centre. J Clin Neurosci. 2011;18:1084–9.
Caroli E, Russillo M, Ferrante L. Intracranial meningiomas in children: report of 27 new cases and critical analysis of 440 cases reported in the literature. J Child Neurol. 2006;21:31–6.
Zwerdling T, Dothage J. Meningiomas in children and adolescents. J Pediatr Hematol Oncol. 2002;24:199–204.
Jiang T, Tang GF, Lin Y, Peng XX, Zhang X, Zhai XW, et al. Prevalence estimates for primary brain tumors in China: a multi-center cross-sectional study. Chin Med J. 2011;124:2578–83.
Li X, Zhao JZ. Intracanial meningiomas of childhood and adolescence: report of 34 cases with follow-up. Childs Nerv Syst. 2009;25:1411–7.
Alexiou GA, Mpairamidis E, Psarros A, Sfakianos G, Prodromou N. Intracranial meningiomas in children. Report of 8 cases. Pediatr Neurosurg. 2008;44:373–5.
Menon G, Nair S, Sudhir J, Rao BR, Mathew A, Bahuleyan B. Childhood and adolescent meningiomas: a report of 38 cases and review of literature. Acta Neurochir. 2009;151:239–44.
Im SH, Wang KC, Kim SK, Oh CW, Kim DG, Hong SK, et al. Childhood meningioma: unusual location, atypical radiological findings, and favorable treatment outcome. Childs Nerv Syst. 2001;17:656–62.
Greene S, Nair N, Ojemann JG, et al. Meningiomas in children. Pediatr Neurosurg. 2008;44:9–13.
Liu YG, Li F, Zhu SG, Liu M, Wu C. Clinical features and treatment of meningiomas in children: report of 12 cases and literature review. Pediatr Neurosurg. 2008;44:112–7.
Li PL, Mao Y, Zhu W, Zhao NQ, Zhao Y, Chen L. Surgical strategies for petroclival meningioma in 57 patients. Chin Med J. 2010;123:2865–73.
Gao X, Zhang R, Mao Y, Wang Y. Childhood and juvenile meningiomas. Childs Nerv Syst. 2009;25:1571–80.
Symons P, Tobias V, Pereira J, Vonau M. Brain-invasive meningioma in a 16-month-old boy. Pathology. 2001;33:252–6.
Maranhão-Filho P, Campos JC, Lima MA. Intracranial meningiomas in children: ten-year experience. Pediatr Neurol. 2008;39:415–7.
Turgut M, Özcan OE, Bertan V. Meningiomas in childhood and adolescence: a report of 13 cases and review of the literature. Br J Neurosurg. 1997;11:501–7.
Lund-Johansen M, Scheie D, Muller T, Lundar T, Helseth E. Neurosurgical treatment of meningiomas in children and young adults. Childs Nerv Syst. 2001;17:719–23.
Kotecha RS, Junckerstorff RC, Lee S, Cole CH, Gottardo NG. Pediatric meningioma: current approaches and future direction. J Neuro-Oncol. 2011;104:1–10.
Rushing EJ, Olsen C, Mena H, Rueda ME, Lee YS, Keating RF, et al. Central nervous system meningiomas in the first two decades of life: a clinicopathological analysis of 87 patients. J Neurosurg. 2005;103:489–95.
Martinez-Lage JF, Poza M, Alcaraz J, Molina E. Giant meningioma of the III ventricle in a child: a case report and review of the literature. Childs Nerv Syst. 1993;9:306–8.
Sheikh BY, Siqueira E, Dayel F. Meningioma in children: a report of nine cases and review of the literature. Surg Neurol. 1996;45:328–35.
Arivazhagan A, Devi BI, Kolluri SV, Abraham RG, Sampath S, Chandramouli BA. Pediatric intracranial meningiomas -- do they differ from their counterparts in adults? Pediatr Neurosurg. 2008;44:43–8.
Kotecha RS, Pascoe EM, Rushing EJ, Rorke-Adams LB, Zwerdling T, Gao T, et al. Meningiomas in children and adolescents: a meta-analysis of individual patient data. Lancet Oncol. 2011;12:1229–39.
Acknowledgements
We thank all the members from the department of Neurological Intensive Care Unit and Neurosurgery, the affiliated hospital of Qingdao university and all patients in our study for cooperation and support.
Funding
Not applicable.
Availability of data and materials
All data generated or analysed during this cases report are included in this published article.
Authors’ contributions
FMC and TWZ Designed the research strategy; SP, LK, FW and WC extracted and analyzed data; FMC wrote the main manuscript text. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
This study was approved by the local human ethics committee of our institution, and informed consent was obtained from all patients or their guardians.
Ethics approval and consent to participate
The author daclare that all procedures in this cases report involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study had been approved by the local institutional review board and the Human Ethics Committee of the Affiliated Hospital of Qingdao University. (200112120046)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Fan, Mc., Fang, W., Liu, K. et al. Paediatric intracranial meningiomas: eight-year experience with 32 cases. Chin Neurosurg Jl 3, 21 (2017). https://doi.org/10.1186/s41016-017-0085-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41016-017-0085-4