Abstract
Background
This study aimed to understand the disease characteristics and treatment outcomes of Crohn’s disease (CD) in a real-world setting in China.
Methods
In this prospective, non-interventional, multicenter disease registry, adults (≥18 years) with existing and newly diagnosed CD were recruited from 14 medical centers across China from January 2015 to January 2017. The study consisted of the enrollment and follow-up periods, of 12 months each. Demographic, clinical characteristics, diagnostic duration and management of CD at enrollment were evaluated. Logistic regression analysis and stepwise multivariate logistic regression analysis used to assess the relationship between the risk factors and CD.
Results
Of 504 enrolled patients, 499 (99.0%) were eligible for analysis. The mean (SD) age at study enrollment was 32.3 (11.43) years and the majority (69.7%) of participants were male. In the past 15 years, a sustained decrease of the period of time in the diagnosis of CD was observed, at about 39.4 (24.11) months in 2010, which decreased to 3.1 (2.13) months in 2015. The most common presenting symptoms of CD included abdominal pain (78.0%), diarrhea (58.1%), weight loss (52.9%) and fever (30.1%). Oral ulcer (19.4%) and arthritis (9.8%) were the most common extra-intestinal manifestations. Non-stricturing non-penetrating (B1) (49.9%) behavior and ileocolonic involvement (L3) (56.2%) location were more frequent. Perianal disease was observed in 29.1% of the patients. Around 23.8% (119/499) patients had CD-related surgery other than perianal disease surgery. Older age at enrollment, longer disease course, complicated disease behavior and absence of perianal disease were all surgery risk factors (p < 0.05). The most common medications was immunomodulators (e.g., azathioprine) (41.5%), anti-TNFα agents (32.9%) and aminosalicylates (20.6%). The mean (SD) Crohn’s Disease Active Index (CDAI) score was 159.1 (91.45) and almost half of the patients (49.1%, 81/165) were in remission.
Conclusions
This study demonstrated the CD-disease characteristics, risk factors of CD-related surgery and perianal disease, and treatment strategies in a real-world setting in China and may help in developing programs to diagnose and manage patients with CD.
Similar content being viewed by others
Background
Crohn’s disease (CD) is a chronic, progressive and relapsing inflammatory bowel disease (IBD) that is often characterized by the presence of intestinal strictures, fistulas or abscesses [1]. The incidence rate of CD in Western countries has demonstrated a significant increasing trend, and it varies from 0.3 to 12.7 cases per 100,000 persons in Europe and 0 to 20.2 cases per 100,000 persons in North America [2, 3]. Similar to Western countries, the incidence of CD has increased over time in Asian countries [4,5,6,7]. While CD is well known in Western countries, it was reported in China about 30 years later: the first case of CD was reported in China in 1956 [8]. Although the overall incidence of CD in China is much lower than in Western countries, the incidence is increasing rapidly with urbanization and socioeconomic development [9]. The current estimated incidence is 0.51–1.09 cases per 100,000 persons in China [10, 11]. In Hong Kong, the incidence of CD has tripled over the last 10 years [12]. Since most studies focused only on particular regions of China, existing data are inadequate to represent the actual incidence of CD at the national level.
According to available data on CD, there is a substantial difference in the incidence and disease characteristics of CD in southern and northern China, as well as in coastal and inland areas [13, 14]. China is also known as a high-risk area for infectious diseases, especially tuberculosis [15]. Due to similar clinical, morphological and histological features of intestinal tuberculosis and CD, the differential diagnosis between these two disorders remains challenging, and must also be considered in terms of treatment modalities and strategies. Intriguingly, while the epidemiology, phenotypic characteristics and management of CD in Asia have the same features as that of Western countries, they also possess certain specific characteristics. A comprehensive understanding of the demographics and disease characteristics as well as diagnosis and treatment status of patients with CD is of great significance to improve the disease management in China. Furthermore, understanding of these factors can likely help optimize diagnosis and treatment and provide the basis for making public health policy decisions.
There is a paucity of population-based epidemiological studies to demonstrate the disease status, diagnosis and treatment patterns of CD in China. The aim of the present study was to build a hospital-based CD registry that would help to analyze the disease characteristics, diagnosis and treatment patterns, and potentially support understanding of treatment strategies for CD in clinical practice in China. Results of this study would help optimize and develop management strategies based on characteristics of CD patients in China.
Methods
Patients
Patients aged ≥18 years were recruited from 14 tertiary teaching medical centers in China from January 2015 to January 2017 (Additional file 1: Table S1). Patients were included if they had a confirmed diagnosis of CD, attended the outpatient clinics and/or hospital wards and were adhering to the physician’s advice through follow-up for up to 1 year.
Study design
In this prospective, non-interventional, multicenter disease registry, patients with a confirmed diagnosis of CD were enrolled regardless of the treatments received. All the eligible patients were followed for 1 year.
Study objectives
The primary objectives of the study were to collect data related to patient demographics and clinical manifestations. Secondary objectives included risk factors for different disease behaviors and locations, and factors related to surgery and medical treatment.
Study evaluations
At baseline, data were collected for variables including patient demographics, nicotine use history, alcohol use history, medical history and comorbid medical conditions, disease onset and diagnosis time, CD symptom profile, details of prior treatment regimen and surgery history. Surgery history included CD-related surgery and perianal disease-related surgery. CD-related surgery referred to any bowel resection due to CD complications. Baseline data were collected upon entry into the registry. During the observational period, each patient was followed for 1 year and data were collected approximately every 3 months to observe their clinical progression.
Patients were grouped based on location of the medical centers as coastal cities: Shanghai, Hangzhou, Guangzhou, Xiamen, and inland cities: Beijing, Changsha, Wuhan, Hefei (Additional file 1: Table S1). The Montreal classification was used to define disease location as L1: terminal ileum, L2: colon, L3: ileocolon and L4: involving upper gastrointestinal tract. Disease behavior was defined as B1: non-stricturing non-penetrating, B2: stricturing and B3: penetrating [16]. The disease activity was assessed using the Crohn’s Disease Active Index (CDAI).
Demographics and disease characteristics such as age, sex, body mass index, nicotine and alcohol use, family and medical history, months from disease onset to enrollment and months from initial definite diagnosis to enrollment were correlated at baseline.
Statistical analysis
A sample size of approximately 500 patients from 14 tertiary medical centers was needed to obtain data that was representative of CD patients in China. Eligible patients were enrolled in the registry irrespective of their treatments, and as this was a descriptive study, no formal hypotheses were tested in this registry. The sample size was determined by pragmatic considerations including feasibility and cost. Effectiveness outcomes were based on the full analysis set (FAS), which included patients who entered the registry and had at least one assessment visit during the treatment period. Baseline data were presented and analyzed in this study. All continuous variables were summarized using mean (standard deviation [SD]). All categorical variables were summarized using frequencies and percentages. Logistic regression analysis and a stepwise multivariate logistic regression analysis was conducted to examine the relationship between the risk factors and CD with entry α = 0.5 and stay α = 0.2 as the selection criteria. The 95% confidence interval (CI) and odds ratio (OR) were calculated. Statistically significant (p < 0.05) results obtained from this analysis of correlation factors using logistic regression model are presented here.
Ethical considerations
This study was conducted in accordance with the ethical principles of the Declaration of Helsinki and the International Conference on Harmonization Good Clinical Practice guidelines. The Independent Ethics Committee or the Institutional Review Board at each study site approved the trial design and eligible patients provided written informed consent before participating.
Results
Enrollment and demographic characteristics
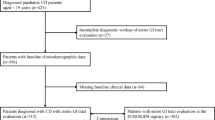
During the study period, 504 patients were screened and 499 patients were eligible. Among those 499 patients, 421 (84.4%) completed the registry and 1-year observational phase; 78 patients were excluded from the analysis mainly due to loss to follow-up (n = 60) and withdrawal of consent (n = 12) (Additional file 1: Table S2). Among 499 patients, 32.9% (164/499) were from South China, 28.9% (144/499) from East China, 21.1% (106/499) from Central China and 17.0% (85/499) from North China (Additional file 1: Table S1). About 61.7% (308/499) of patients were enrolled in centers located in coastal cities, and 38.3% (191/499) enrolled in centers in inland cities. The mean (SD) age was 32.3 (11.43) years (median: 30.0, range: 18 to 77 years), and a higher proportion of patients were male (69.7%, n = 348, male vs. female ratio: 2.30:1). The majority of patients never used nicotine (86.4%, n = 382) and never consumed alcohol (90.5%, n = 401). Patents enrolled in inland medical centers had a higher proportion of smoking (current user 10.3% vs. 6.9%, former user 9.7% vs. 2.9%, p = 0.0036) and drinking (former user 9.0% vs. 1.8%, p = 0.0023) than that of patients enrolled in coastal cities (Table 1). At baseline, hepatitis B was reported in 19 (3.8%) patients. Appendicitis and medical history of nephrolithiasis were reported in 10 (2.0%) patients each (Table 1).
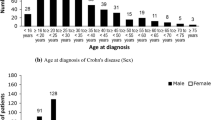
Abdominal pain (78.0%, 389/499), diarrhea (58.1%, 290/499), weight loss (52.9%, 264/499) and fever (30.1%, 150/499) were the most common symptoms of CD. Less common symptoms were bloody stool (25.1%, 125/499), anemia (22.8%, 114/499) and mucus or pus in stools (12.4%, 62/499) (Fig. 1a). Oral ulcer (19.4%, 97/499) and arthritis (9.8%, 49/499) were the most common extra-intestinal manifestations. Skin lesions such as nodular erythema and uveitis were relatively uncommon (Fig. 1b).
Time from disease onset to definite diagnosis
The mean (SD) time from disease onset to definite diagnosis was 32.0 (46.43) months, patients enrolled in inland centers had a longer duration for diagnosis (39.9 [58.84] vs. 27.0 [35.93] months, p = 0.0255) than patients enrolled in coastal centers. The patients with data available for different time periods were grouped by the year of disease onset (Table 2). The mean (SD) duration from disease onset to initial definitive diagnosis decreased significantly over the period of time from 79.4 (67.03) months before 2010, to 39.4 (24.11) months in 2010, and to 3.1 (2.13) months in 2015 (Table 2 and Fig. 2). There was a significant shortening of diagnostic duration in recent years.
Surgery history
Of the total 499 patients, 23.8% (119/499) had a history of CD-related surgery, and 15.8% (19/499) had a history of perianal disease related surgery. Demographics and baseline characteristics were comparable between patients with history of CD-related surgery and patients without. Patients who had a CD-related surgery history were older at disease onset (30.8 ± 10.98 vs. 27.0 ± 10.37 years, p = 0.0006), at initial definite diagnosis (34.1 ± 11.45 vs. 29.5 ± 10.66 years, p < 0.0001), and at enrollment (37.3 ± 11.95 vs. 30.8 ± 10.81 years, p < 0.0001) than patients without CD-related surgery history (Table 3). Time from disease onset to initial diagnosis (39.4 ± 47.57 vs. 29.6 ± 45.89 months, p = 0.0457) as well as time from disease onset to enrollment (78.6 ± 73.29 vs. 44.4 ± 51.32 months, p < 0.0001) were significantly longer in patients with a history of CD-related surgery. Fistulizing or penetrating CD behavior (B3) was higher (43.5% vs. 13.2%, p < 0.0001) in patients with history of CD-related surgery than in patients without history of CD-related surgery. On the contrary, patients with a CD-related surgery history had lower presence of perianal disease (16.8%, n = 20 vs. 32.6%, n = 124, p = 0.0009). Logistic model for correlation analysis revealed older age at enrollment (OR = 1.047, p < 0.01), longer disease course (months from disease onset to enrollment, OR = 1.009, p < 0.01), stricturing behavior (B2 vs. B1, OR = 2.815, p < 0.001), penetrating behavior (B3 vs B1, OR = 8.147, p < 0.001; B3 vs. B2, OR = 2.895, p < 0.001) and perianal disease (OR = 0.419, p < 0.001) were associated with CD-related surgery (Table 4).
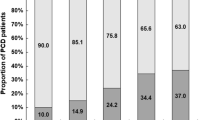
Disease behavior and location
At baseline, non-stricturing non-penetrating (B1) disease behavior (49.9%, 247/495) was the highest. Centers in coastal cities were taking care of more patients with B2 (33.8% vs. 23.7%), B3 (21.2% vs. 18.4%) behavior and perianal disease (36.7% vs. 16.8%) than inland centers (p < 0.0001). Increase in duration from disease onset to enrollment and increase in duration from disease initial definite diagnosis to enrollment in registry were risk factors associated with patients of B2 and B3 behavior (OR = 1.006, p = 0.002; and OR = 1.007, p = 0.009, respectively). Currently smoking (OR = 2.454, p = 0.020) was also associated with patients with B2 and B3 behavior (Additional file 1: Table S3).
CD was classified as being localized in the L3 region in the majority of patients (56.2%, 277/493) (Fig. 3). Former smokers had higher probability of having CD localized in terminal ileal (L1) region than ileocolonic (L3) region (OR = 0.205, p = 0.004, Additional file 1: Table S4). Body mass index (BMI) in normal range (18.5–24 kg/m2) was associated with colonic (L2) location compared with L1 location (OR = 0.404, p = 0.017).
Patients who had perianal disease were younger at disease onset (25.3 ± 9.40 vs. 29.0 ± 10.92 years, p = 0.0003), at initial definite diagnosis (27.7 ± 10.02 vs. 31.8 ± 11.19 years, p = 0.0001), and at enrollment (28.9 ± 10.05 vs. 33.7 ± 11.67 years, p < 0.0001) than patients without perianal disease (Table 5). Duration from initial diagnosis to enrollment (14.8 ± 24.97 vs. 22.9 ± 43.29 months, p = 0.0345) and duration from disease onset to enrollment (43.8 ± 44.55 vs. 56.2 ± 63.75 months, p = 0.0341) were significantly shorter in patients with perianal disease. Logistic model for correlation analysis revealed that younger age at enrollment (OR = 0.957, p < 0.001), shorter disease course (time from disease onset to enrollment, OR = 0.996, p = 0.036), smoking (former vs. never, OR = 0.209, p = 0.036), B2 disease behavior (OR = 0.514, p = 0.006), and L3 disease location (OR = 3.052, p < 0.001) were associated with perianal disease (Table 6). Patients with perianal disease had higher proportion of anti-tumor necrosis factor α (TNFα) agents use (41.7% vs. 29.6%, p = 0.0098) and antibiotics use (20.8% vs. 10.0%, p = 0.0012).
Medical treatment and disease activity
At baseline, the mean (SD) CDAI score was 159.1 (91.45) and half of the patients (49.1%, 81/165) were in disease remission. Severe CDAI scores at baseline were reported in only 1.2% (2/165) of the patients. Patients enrolled in coastal medical centers had a higher proportion of moderate active disease (30.6% vs. 16.3%), and a smaller proportion of mild active disease (17.6% vs. 35.0%) than patients enrolled in inland centers (p = 0.0094).
At baseline, most of the patients (88.4%, 441/499) had a history of using any medicine for CD management. Less than 50% of patients were receiving immunomodulators (41.5%, n = 207; e.g., azathioprine) or anti-TNFα agents (32.9%, n = 164). About one-fifth of patients were on aminosalicylates (20.6%, n = 103) or steroids (19.8%, n = 99) (Table 1). Compared with inland centers, coastal centers had a higher use of anti-TNF agents (37.0% vs. 26.2%, p = 0.0123), enteral nutrition (20.5% vs. 3.1%, p < 0.0001), antibiotics (19.2% vs. 3.1%, p < 0.0001), anti-tuberculosis (8.4% vs. 0.5%, p < 0.0001) and other agents including traditional Chinese medicine (35.1% vs. 3.7%, p < 0.0001), but with a lower use of steroids (14.9% vs. 27.7%, p = 0.0005).
Discussion
To our knowledge, this is one of the largest registry studies of CD in China till now, and the results reveal the disease characteristics, behaviors and treatment strategies of CD in China, including difference between inland and coastal medical centers. The results may be helpful to understand the current situation of CD in China. This registry study demonstrated that the number of male patients outweighed the number of female patients, which may reflect a higher prevalence of CD in men. Commonly reported symptoms of CD were abdominal pain, diarrhea, weight loss and fever. More than half of the patients had ileocolonic involvement, and half of the patients were of the non-stricturing non-penetrating behavior. Age, disease duration, B2 or B3 disease behavior and perianal disease were associated with CD-related surgery. This registry study also demonstrated that the diagnosis period was significantly shortened during the recent years in China.
Data of the present study demonstrated a male predominance in CD, with a male vs. female ratio of 2.30:1, which is consistent with the previous studies in Asian countries including data from Korea [7], Japan [17], India [18], Sri Lanka [19], Singapore [20] and others [21, 22]. In contrast, the incidence of CD in women is greater or equal to that in men in Western countries [23,24,25]. Thus far, no explanation is available for such discrepancies between Asian and Western populations, but this could be attributed to differences in genetic susceptibility and men having a greater possibility of seeking job opportunities in industrialized areas at a younger age, thus being exposed to potential environmental risk factors early in life. The peak incidence of CD observed in this study was in the fourth decade of life (32.3 years), consistent with previous reports from China [10, 26]. Studies in Western population have demonstrated a bimodal distribution in the age at onset of CD, with a peak occurring at 20–39 years and another peak at 50–79 years [27,28,29,30]. Studies in Asian populations have demonstrated either a less prominent second peak [7, 31, 32] or no second peak [33]. The exact reason for the bimodal distribution in the Western population is unclear, but it may be attributed to passive and active smoking in childhood and adulthood and sensitivities of different age groups to certain infectious factors [30, 34].
In terms of disease location, 56.2% patients had ileocolonic disease, whereas only 14.4% of the patients had colonic disease, which is consistent with the results from a single-center study from China [29]. Ileocolonic disease is also the most common CD phenotype in other Asian countries like Japan (65.8%) [35] and South Korea (77.7%) [7]. In Western countries, data on the disease location are relatively homogeneous largely with colonic, upper gastrointestinal and intestinal involvement. A population-based study from Hungary demonstrated that disease location for patients with CD was greatest in ileocolon (44.2%), followed by colon (35.6%), ileum (20.2%) and upper gastrointestinal region (2.4%) [36]. Disease behavior was clinically relevant as it is associated with the development of CD-related complications and need for surgery. At baseline, the disease behavior phenotypes (49.9% B1, 29.9% B2 and 20.2% B3) were concordant with a previous study from China and other studies from Asian countries [11, 33, 36]. Studies in western population have demonstrated that B1 was the most frequently observed behavior, with a frequency of nearly 80%. This difference might due to our registry patients who were not newly diagnosis CD patients, and the disease had already progressed to a more severe behavior. Accordingly, a larger proportion of patients change their behavior pattern to a more aggressive type (B2 and B3) after 5, 10 and 15 years of follow-up [37], and this may be attributed to increased smoking, disease location and clinical activity of the disease.
In concordance with other studies in the Asian population [36, 38, 39], abdominal pain, diarrhea and weight loss were the leading presenting symptoms of CD noted in the present study population. In the Western population, the incidence of diarrhea was the highest (79%), followed by abdominal pain (63%) and weight loss (21%) [40]. Certain extraintestinal manifestations such as oral ulcer, arthritis, skin lesions and uveitis often occur in patients with CD. The prevalence of extraintestinal manifestations was lower in the Asian population compared with the Western population (11% vs. 25–40%) [41,42,43]. Less frequent extraintestinal manifestations may be associated with relatively better prognosis among patients from Asian countries as compared with patients from Western countries.
Of the 499 patients, 23.8% (119/499) had history of CD-related surgery other than perianal disease surgery (15.8%). Older age at enrollment, longer disease duration, longer duration from disease onset to initial diagnosis and penetrating behavior were all risk factors related to CD surgery. A delayed diagnosis could result in missing the best timing for treatment, thus affecting the prognosis and increasing the risk of CD-related surgery [44]. Thus, diagnostic delay of CD is a challenge in several parts of the world. In Switzerland [45], the diagnostic delay was reported about 24 months. The analysis of the CD diagnosis period in the present registry revealed that the diagnostic period was significantly shortened in recent years. The current study found that patients with CD-related surgery history had a relatively lower presence of perianal disease. In the literature, patients with perianal disease carry a higher risk of surgery and this suggests a more severe disease course. [46] In the present study, patients with perianal disease also had a younger age at disease onset and a shorter duration from disease onset to enrollment, as well as a higher use of anti-TNF agents. These differences indicate that the presence of perianal disease may be shortened the diagnosis awareness and be helpful in differentiating from intestinal tuberculosis. A shorter diagnostic duration and a higher proportion of anti-TNF use might explain the negative association between perianal disease and bowel surgery.
In the present disease registry, immunomodulators were used frequently (41.5%) for the treatment of CD. A retrospective review in a population from East China demonstrated that 26.9% (61/227) patients had indications for immunomodulator use; however, such agents were prescribed to 34.4% of patients, of which, 37.5% received a subtherapeutic dose with no attempt of dose escalation [46]. The use of immunomodulators early in the course of the disease has been reported to be more effective in achieving clinical remission than conventional step-up therapy, but not in preventing relapse [47]. In Asia, anti-TNFs are used less frequently for the treatment of patients with CD. Sung et al. demonstrated that physicians in Asia favored anti-TNFs as a second-line therapy for CD [48]. A retrospective study from Korea, conducted from 1991 to 2007, reported that only 8.6% of patients with CD used infliximab [36]. Another study comparing the management of CD between Melbourne and Hong Kong demonstrated that a significantly higher percentage of patients were on anti-TNFs therapy in Melbourne than in Hong Kong (40% vs. 11%) [49]. Anti-TNFs are effective in inducing and maintaining clinical remission of CD [50, 51], and the use in the current study was higher (32.9%) than in other Asian countries. Thus, these results indicate that the update of new treatment paradigms was well adopted in China, especially in coastal medical centers. This multicenter study definitely helps inform a strategy for prevention and management programs for patients with CD in China by stratifying disease risk factors.
In the current study, because only baseline data were analyzed, disease progression and treatment effect could not be observed. Hence, further studies are warranted to describe the long-term disease progression. In addition, the small sample size of the current study may likely be interpreted as a selection bias. Patients were recruited from selected medical centers but not from national or regional registry. Since young patients < 18 years of age and women with pregnancy were excluded, the present study may not exactly reflect the profiles of the whole population. Adjuvant therapy such as enteral nutrition therapy, antibiotics and immunosuppressants may also affect the prognosis and disease behaviors.
Conclusions
This multicenter, observational study was conducted in China to analyze the nationwide disease characteristics, clinical behavior and treatment strategies in patients with CD. This study indicated that the clinical features of CD in China were different from those in Western countries in terms of age, sex distribution, disease location, disease behavior, the prevalence of extra-intestinal manifestations and treatment practices. These findings have important implications for local resource allocation, healthcare planning and to further update the clinical guidelines for management of CD in China.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Abbreviations
- B1:
-
Non-stricturing non-penetrating
- B2:
-
Structuring
- B3:
-
Penetrating;
- BMI:
-
Body mass index
- CD:
-
Crohn’s disease
- CDAI:
-
Crohn’s Disease Active Index
- CI:
-
Confidence interval
- FAS:
-
Full analysis set
- IBD:
-
Inflammatory bowel disease
- L1:
-
Terminal ileum
- L2:
-
Colon
- L3:
-
Ileocolon
- L4:
-
Upper gastrointestinal tract
- OR:
-
Odds ratio
- SD:
-
Standard deviation
- TNF:
-
Tumor necrosis factor
References
Ha F, Khalil H. Crohn’s disease: a clinical update. Ther Adv Gastroenterol. 2015;8(6):352–9.
Ananthakrishnan AN. Epidemiology and risk factors for IBD. Nat Rev Gastroenterol Hepatol. 2015;12(4):205–17.
Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G, Benchimol EI, Panaccione R, Ghosh S, Barkema HW, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142(1):46–54 e42 quiz e30.
Chuang CH, Lin SH, Chen CY, Sheu BS, Kao AW, Wang JD. Increasing incidence and lifetime risk of inflammatory bowel disease in Taiwan: a nationwide study in a low-endemic area 1998-2010. Inflamm Bowel Dis. 2013;19(13):2815–9.
Ng SC. Emerging trends of inflammatory bowel disease in Asia. Gastroenterol Hepatol. 2016;12(3):193–6.
Wei SC, Lin MH, Tung CC, Weng MT, Kuo JS, Shieh MJ, Wang CY, Ho WC, Wong JM, Chen PC. A nationwide population-based study of the inflammatory bowel diseases between 1998 and 2008 in Taiwan. BMC Gastroenterol. 2013;13:166.
Yang SK, Yun S, Kim JH, Park JY, Kim HY, Kim YH, Chang DK, Kim JS, Song IS, Park JB, et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986-2005: a KASID study. Inflamm Bowel Dis. 2008;14(4):542–9.
Wen S. A case report of gastric, duodenal and jejunal crohn’s disease. Chinese Med J. 1956;5:379–581.
Wang PQ, Hu J, Al Kazzi ES, Akhuemonkhan E, Zhi M, Gao X, de Paula Pessoa RH, Ghazaleh S, Cornelius T, Sabunwala SA, et al. Family history and disease outcomes in patients with Crohn’s disease: a comparison between China and the United States. World J Gastrointest Pharmacol Ther. 2016;7(4):556–63.
Zeng Z, Zhu Z, Yang Y, Ruan W, Peng X, Su Y, Peng L, Chen J, Yin Q, Zhao C, et al. Incidence and clinical characteristics of inflammatory bowel disease in a developed region of Guangdong Province, China: a prospective population-based study. J Gastroenterol Hepatol. 2013;28(7):1148–53.
Zhao J, Ng SC, Lei Y, Yi F, Li J, Yu L, Zou K, Dan Z, Dai M, Ding Y, et al. First prospective, population-based inflammatory bowel disease incidence study in mainland of China: the emergence of “western” disease. Inflamm Bowel Dis. 2013;19(9):1839–45.
Lakatos L, Kiss LS, David G, Pandur T, Erdelyi Z, Mester G, Balogh M, Szipocs I, Molnar C, Komaromi E, et al. Incidence, disease phenotype at diagnosis, and early disease course in inflammatory bowel diseases in Western Hungary, 2002-2006. Inflamm Bowel Dis. 2011;17(12):2558–65.
Hu D, Ren J, Wang G, Gu G, Liu S, Wu X, Chen J, Ren H, Hong Z, Li J. Geographic mapping of Crohn’s disease and its relation to affluence in Jiangsu province, an eastern coastal province of China. Gastroenterol Res Pract. 2014;2014:590467.
Yang H, Li Y, Wu W, Sun Q, Zhang Y, Zhao W, Lv H, Xia Q, Hu P, Li H, et al. The incidence of inflammatory bowel disease in northern China: a prospective population-based study. PLoS One. 2014;9(7):e101296.
Jia Z, Cheng S, Ma Y, Zhang T, Bai L, Xu W, He X, Zhang P, Zhao J, Christiani DC. Tuberculosis burden in China: a high prevalence of pulmonary tuberculosis in household contacts with and without symptoms. BMC Infect Dis. 2014;14:64.
Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006;55(6):749–53.
Yao T, Matsui T, Hiwatashi N. Crohn’s disease in Japan: diagnostic criteria and epidemiology. Dis Colon Rectum. 2000;43(10 Suppl):S85–93.
Das K, Ghoshal UC, Dhali GK, Benjamin J, Ahuja V, Makharia GK. Crohn’s disease in India: a multicenter study from a country where tuberculosis is endemic. Dig Dis Sci. 2009;54(5):1099–107.
Subasinghe D, Nawarathna NM, Samarasekera DN. Disease characteristics of inflammatory bowel disease (IBD): findings from a tertiary care Centre in South Asia. J Gastrointest Surg. 2011;15(9):1562–7.
Lee YM, Fock K, See SJ, Ng TM, Khor C, Teo EK. Racial differences in the prevalence of ulcerative colitis and Crohn’s disease in Singapore. J Gastroenterol Hepatol. 2000;15(6):622–5.
Makharia GK, Ramakrishna BS, Abraham P, Choudhuri G, Misra SP, Ahuja V, Bhatia SJ, Bhasin DK, Dadhich S, Dhali GK, et al. Survey of inflammatory bowel diseases in India. Indian J Gastroenterol. 2012;31(6):299–306.
Malekzadeh MM, Vahedi H, Gohari K, Mehdipour P, Sepanlou SG, Ebrahimi Daryani N, Zali MR, Mansour-Ghanaei F, Safaripour A, Aghazadeh R, et al. Emerging epidemic of inflammatory bowel disease in a middle income country: a nation-wide study from Iran. Arch Iran Med. 2016;19(1):2–15.
Kyle J. Crohn’s disease in the northeastern and northern isles of Scotland: an epidemiological review. Gastroenterology. 1992;103(2):392–9.
Shivananda S, Pena AS, Nap M, Weterman IT, Mayberry JF, Ruitenberg EJ, Hoedemaeker PJ. Epidemiology of Crohn’s disease in Regio Leiden, the Netherlands. A population study from 1979 to 1983. Gastroenterology. 1987;93(5):966–74.
Wu D, Chen C, Wu S, DAI L, XIA L, CHEN X. A retrospective study on clinical characteristics of paediatric Crohn’s disease. HK J Paediatr. 2014;19:169–74.
Zheng JJ, Zhu XS, Huangfu Z, Shi XH, Guo ZR. Prevalence and incidence rates of Crohn’s disease in mainland China: a meta-analysis of 55 years of research. J Dig Dis. 2010;11(3):161–6.
Ekbom A, Helmick C, Zack M, Adami HO. The epidemiology of inflammatory bowel disease: a large, population-based study in Sweden. Gastroenterology. 1991;100(2):350–8.
Loftus CG, Loftus EV Jr, Harmsen WS, Zinsmeister AR, Tremaine WJ, Melton LJ 3rd, Sandborn WJ. Update on the incidence and prevalence of Crohn’s disease and ulcerative colitis in Olmsted County, Minnesota, 1940-2000. Inflamm Bowel Dis. 2007;13(3):254–61.
Mocanu D, Catuneanu AM, Diculescu M, Gologan S, Sporea I. Current epidemiologic trends in Crohn’s disease: data from a tertiary referral Centre in Bucharest: (Fundeni institute, Center of Gastroenterology and Hepatology). Maedica (Buchar). 2010;5(2):95–101.
Park SJ, Kim WH, Cheon JH. Clinical characteristics and treatment of inflammatory bowel disease: a comparison of eastern and Western perspectives. World J Gastroenterol. 2014;20(33):11525–37.
Asakura K, Nishiwaki Y, Inoue N, Hibi T, Watanabe M, Takebayashi T. Prevalence of ulcerative colitis and Crohn’s disease in Japan. J Gastroenterol. 2009;44(7):659–65.
Ng SC, Tang W, Ching JY, Wong M, Chow CM, Hui AJ, Wong TC, Leung VK, Tsang SW, Yu HH, et al. Incidence and phenotype of inflammatory bowel disease based on results from the Asia-pacific Crohn’s and colitis epidemiology study. Gastroenterology. 2013;145(1):158–65 e152.
Moon CM, Park DI, Kim ER, Kim YH, Lee CK, Lee SH, Kim JH, Huh KC, Jung SA, Yoon SM, et al. Clinical features and predictors of clinical outcomes in Korean patients with Crohn’s disease: a Korean association for the study of intestinal diseases multicenter study. J Gastroenterol Hepatol. 2014;29(1):74–82.
Wang YF, Zhang H, Ouyang Q. Clinical manifestations of inflammatory bowel disease: east and west differences. J Dig Dis. 2007;8(3):121–7.
Oriuchi T, Hiwatashi N, Kinouchi Y, Takahashi S, Takagi S, Negoro K, Shimosegawa T. Clinical course and longterm prognosis of Japanese patients with Crohn’s disease: predictive factors, rates of operation, and mortality. J Gastroenterol. 2003;38(10):942–53.
Ye BD, Yang SK, Cho YK, Park SH, Yang DH, Yoon SM, Kim KJ, Byeon JS, Myung SJ, Yu CS, et al. Clinical features and long-term prognosis of Crohn’s disease in Korea. Scand J Gastroenterol. 2010;45(10):1178–85.
Cosnes J, Cattan S, Blain A, Beaugerie L, Carbonnel F, Parc R, Gendre JP. Long-term evolution of disease behavior of Crohn’s disease. Inflamm Bowel Dis. 2002;8(4):244–50.
Li X, Song P, Li J, Tao Y, Li G, Li X, Yu Z. The Disease Burden and Clinical Characteristics of Inflammatory Bowel Disease in the Chinese Population: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2017;14(3).
Jiang L, Xia B, Li J, Ye M, Yan W, Deng C, Ding Y, Luo H, Hou W, Zhao Q, et al. Retrospective survey of 452 patients with inflammatory bowel disease in Wuhan city, Central China. Inflamm Bowel Dis. 2006;12(3):212–7.
Penn KA, Whittle DO, Lee MG. Inflammatory bowel disease in Jamaica. Ann Gastroenterol. 2013;26(3):239–42.
Ephgrave K. Extra-intestinal manifestations of Crohn’s disease. Surg Clin North Am. 2007;87(3):673–80.
Hsu YC, Wu TC, Lo YC, Wang LS. Gastrointestinal complications and extraintestinal manifestations of inflammatory bowel disease in Taiwan: a population-based study. J Chin Med Assoc. 2017;80(2):56–62.
Luo CH, Wexner SD, Liu QS, Li L, Weiss E, Zhao RH. The differences between American and Chinese patients with Crohn’s disease. Color Dis. 2011;13(2):166–70.
Li Y, Ren J, Wang G, Gu G, Wu X, Ren H, Hong Z, Hu D, Wu Q, Li G, et al. Diagnostic delay in Crohn’s disease is associated with increased rate of abdominal surgery: a retrospective study in Chinese patients. Dig Liver Dis. 2015;47(7):544–8.
Vavricka SR, Spigaglia SM, Rogler G, Pittet V, Michetti P, Felley C, Mottet C, Braegger CP, Rogler D, Straumann A, et al. Systematic evaluation of risk factors for diagnostic delay in inflammatory bowel disease. Inflamm Bowel Dis. 2012;18(3):496–505.
Huang LJ, Zhu Q, Lei M, Cao Q. Current use of immunosuppressive agents in inflammatory bowel disease patients in East China. World J Gastroenterol. 2009;15(24):3055–9.
Kwak MS, Kim DH, Park SJ, Kim TI, Hong SP, Kim WH, Cheon JH. Efficacy of early immunomodulator therapy on the outcomes of Crohn’s disease. BMC Gastroenterol. 2014;14:85.
Sung JJ, Kamm MA, Marteau P. Asian perspectives in the management of inflammatory bowel disease: findings from a recent survey. J Gastroenterol Hepatol. 2010;25(1):183–93.
Prideaux L, Kamm MA, De Cruz P, Williams J, Bell SJ, Connell WR, Brown SJ, Lust M, Desmond PV, Chan H, et al. Comparison of clinical characteristics and management of inflammatory bowel disease in Hong Kong versus Melbourne. J Gastroenterol Hepatol. 2012;27(5):919–27.
Hanauer SB, Feagan BG, Lichtenstein GR, Mayer LF, Schreiber S, Colombel JF, Rachmilewitz D, Wolf DC, Olson A, Bao W, et al. Maintenance infliximab for Crohn’s disease: the ACCENT I randomised trial. Lancet. 2002;359(9317):1541–9.
Schreiber S, Khaliq-Kareemi M, Lawrance IC, Thomsen OO, Hanauer SB, McColm J, Bloomfield R, Sandborn WJ, Investigators PS. Maintenance therapy with certolizumab pegol for Crohn’s disease. N Engl J Med. 2007;357(3):239–50.
Acknowledgements
The authors thank the study participants, without whom the study would never have been accomplished.
Funding
This work was supported by Xi’an Janssen Pharmaceutical Ltd., Beijing, China. The funding body had a role in data analysis and data interpretation.
Author information
Authors and Affiliations
Contributions
JQ: principal investigator, who contributed to study design, study supervision and editing of the manuscript. YL: study design, protocol development, data interpretation, and drafting and editing of the manuscript. BC, XG, NH, MFH, ZR, ZL, JZ, DZ, XW, JR, JS, PZ, HW, MC, and JC: study design and implementation, protocol development, and data collection. PX, JL, MH, YFL, and HF: statistical analyses and data interpretation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the ethical principles originating in the Declaration of Helsinki and the International Conference on Harmonization Good Clinical Practice guidelines. The Institutional Review Board at each study site approved the trial design.(see the REMICADECRD4018 CSR IRB-IEC List).
All the eligible patients provided written informed consent before participating in the study.
Consent for publication
Not applicable.
Competing interests
This work was supported by Xi’an Janssen Pharmaceutical Ltd., Beijing, China. The funding body had a role in data analysis and data interpretation. No other competing interests exist.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1
: Table S1. List of participating centers; Full analysis set. Table S2. Subject dispositions; Screened analysis set. Table S3. Logistic model for each correlation factor to Crohn’s disease behavior (B1 vs. B2 + B3); Full analysis set. Table S4. Logistic model for each correlation factors to Crohn’s disease localization (L1 vs. L2 vs. L3 vs. L4); Full analysis set. (DOC 111 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Li, Y., Chen, B., Gao, X. et al. Current diagnosis and management of Crohn’s disease in China: results from a multicenter prospective disease registry. BMC Gastroenterol 19, 145 (2019). https://doi.org/10.1186/s12876-019-1057-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-019-1057-2