Abstract
The Gender Medicine Team (GMT), comprised of members with expertise in endocrinology, ethics, genetics, gynecology, pediatric surgery, psychology, and urology, at Texas Children's Hospital and Baylor College of Medicine formed a task force to formulate a consensus statement on practice guidelines for managing disorders of sexual differentiation (DSD) and for making sex assignments. The GMT task force reviewed published evidence and incorporated findings from clinical experience. Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) was used to assess the quality of evidence presented in the literature for establishing evidence-based guidelines. The task force presents a consensus statement regarding specific diagnostic and therapeutic issues in the management of individuals who present with DSD. The consensus statement includes recommendations for (1) laboratory workup, (2) acute management, (3) sex assignment in an ethical framework that includes education and involvement of the parents, and (4) surgical management.
Similar content being viewed by others
1. Introduction
A child with a disorder of sexual differentiation (DSD) poses a variety of challenges for the treating physician as well as for the parents and family. Although appropriate management has long been a matter of concern and often contention, no clinical practice guidelines have been established to help physicians inform parents and implement management approaches in a standardized fashion [1–8]. Our aim was to develop practice guidelines for managing DSD and for making sex assignments. Accordingly, we formed a Gender Medicine Team (GMT) task force, comprised of experts in the fields of endocrinology, ethics, genetics, gynecology, psychology, and urology, to evaluate the information available from our own experience and from a review of the literature. We utilized the Grading of Recommendation, Assessment, Development, and Evaluation (GRADE) system to grade the evidence and recommendations. With the review and recommendations offered by our task force, we developed a consensus statement for clinical management of DSD and for making sex assignments.
2. Methods
The GMT task force first identified four clinically relevant questions to be answered from the evidence. These questions were the following.
Question 1.
What constituted the most appropriate evaluation for infants with ambiguous genitalia or a DSD? This question was divided into the following subquestions.
-
(1a) What is the appropriate evaluation for CAH?
-
(1b) What is the most appropriate way to assess the hypothalamic pituitary gonadal axis in the context of ambiguous genitalia or hypothalamic pituitary hypogonadism?
-
(1c) What is the most appropriate evaluation for micropenis and for undescended testes for the evaluation of primary hypogonadism most likely in the context of dysgenetic testes?
-
(1d)
 What is the most appropriate evaluation for peripheral defects leading to micropenis, hypospadias with respect to[1, 2]the action of testosterone which could be in the context of(a)5 alpha-reductase deficiency or(b)biochemical and molecular genetic testing for androgen receptor defect, and[3]the production of testosterone with respect to the enzymatic machinery,
What is the most appropriate evaluation for peripheral defects leading to micropenis, hypospadias with respect to[1, 2]the action of testosterone which could be in the context of(a)5 alpha-reductase deficiency or(b)biochemical and molecular genetic testing for androgen receptor defect, and[3]the production of testosterone with respect to the enzymatic machinery, -
(1e) What genetic testing should be performed for ambiguous genitalia?
Question 2.
What is the most appropriate management for infants with ambiguous genitalia or a DSD who present with a life-threatening complication as a result of their condition?
Question 3.
What is the most appropriate approach to sex assignment in an infant with ambiguous genitalia or a DSD? This question was divided into the following subquestions.
-
(3a) Should clinical decision making for DSD be physician-dependent or reside within a Gender Medicine Team?
-
(3b) What role should the psychologist play on the Gender Medicine Team?
-
(3c) What is the ethical framework for sex assignment?
Question 4.
What is the most appropriate surgical management for infants with ambiguous genitalia or DSD? This question was divided into the following subquestions.
-
(4a) What is the most appropriate surgical management for infants with CAH?
-
(4b) What is the most appropriate feminizing surgery management of patients with DSD?
-
(4c) What is the most appropriate masculinizing surgery management of patients with DSD?
-
(4c) What is the most appropriate gonadectomy surgery management of patients with DSD?
The GMT task force then searched databases for research-based articles on infants/children with ambiguous genitalia or DSD. Databases included Cochrane Collaboration, PubMed, and Google Scholar. Articles were restricted to English-based publications. Key words/terms used to search the databases included: acute management, ambiguous genitalia, anatomical sex, androgen synthesis, chromosomal sex, gonads, hormonal sex, medical emergency, molecular sex, phallic structure, pigmentation of the genitalia, reproductive sex, sex assignment, sex of rearing, and "46,XX" male infants. In addition, surgical terms included vaginoplasty, clitoral reduction, clitoroplasty, and masculinizing and feminizing surgery.
Searches of the literature were performed for each topic and graded by a member of the Texas Children's Hospital Evidence-Based Outcomes Center using the approach recommended by the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) group [9, 10]. The GMT task force "used the best available research evidence that members identified to inform the recommendations and consistent language" of "both the strength of a recommendation and the quality of evidence" [10]. The quality of the evidence was evaluated as "very low quality," "low quality," "moderate quality," or "high quality." Recommendations were denoted as "strong" or "weak."
In conjunction with the GRADE system, the GMT task force evaluated an approach in practice by the Texas Children's Hospital Evidence-Based Outcomes Center. To formulate the consensus statement, members of the task force systematically reviewed the data according to their areas of expertise and contributed to the statement accordingly. Questions were distributed before drafting a manuscript and reaching a final consensus. Each member of the task force approved the final materials used. The final manuscript and the consensus statement were approved based on a vote by all members of the task force.
3. Results
The review of the literature using the Cochrane Collaboration, PubMed, SCOPUS, and Google Scholar yielded the articles for most of the questions posed. We found that a paucity of articles exists for this topic as a coherent whole but that almost all the questions were addressed in the literature, if only by one or a few articles. The results are provided below.
Question 1.
What constituted the most appropriate evaluation for infants with ambiguous genitalia or a DSD? We found that few outcome studies address the appropriate workup for children with DSD. A review of the literature called for using a multidisciplinary team and various diagnostic procedures for performing the workup. Literature results for the specific questions identified in order to arrive at a final consensus were the following.
 What is the appropriate evaluation for CAH?
What is the appropriate evaluation for CAH?
Three articles were specifically relevant to our research. One was a review article by Sultan et al. [11]. The other two articles that were useful were a review by Speiser and White [12], specifically addressing CAH and the consensus statement of the Lawson Wilkins Pediatric Endocrine Society and The European Society for Paediatric Endocrinology [13].
 What is the most appropriate way to assess the hypothalamic pituitary gonadal axis in the context of ambiguous genitalia or hypothalamic pituitary hypogonadism?
What is the most appropriate way to assess the hypothalamic pituitary gonadal axis in the context of ambiguous genitalia or hypothalamic pituitary hypogonadism?
In addition to the article by Sultan et al. [11] noted above, two review articles were pertinent: one by Grumbach [14] and the other a retrospective article by Parisi, et al. [15].
-
(1c) What is the most appropriate evaluation for micropenis and for undescended testes for the evaluation of primary hypogonadism most likely in the context of dysgenetic testes? Two retrospective studies, one by Kolon and Miller [16] and one by Davenport, et al. [17], and an observation study by Mirsa, et al. [18] specifically address our purposes.
-
(1d) What is the most appropriate evaluation for peripheral defects leading to micropenis, hypospadias as related to[1, 2]the action of testosterone which could be in the context of(a)5 alpha-reductase deficiency or(b)biochemical and molecular genetic testing for androgen receptor defect and [ 3 ] the production of testosterone with respect to the enzymatic machinery.
With respect to [1, 2]the action of testosterone, in the context of
-
(a)
5 alpha-reductase deficiency in addition to relying on the ordinary established practice of ordering testosterone and dihydrotestosterone, we found useful a retrospective observational study by Boehmer et al. [19, 20] and case reports by Imperato-McGinley et al. [21] and Cai et al. [22].
-
(b)
The molecular genetic testing for the androgen receptor, We found a case study by Deeb et al. [23].
With regard to[ 3 ] the production of testosterone with respect to the enzymatic machinery, our search of the literature yielded two observational studies, one by Codner et al. [24] and one by Eckstein et al. [25].
 What genetic testing should be performed for ambiguous genitalia?
What genetic testing should be performed for ambiguous genitalia?
Our search of the literature yielded the review article by Parisi et al. [15] and a retrospective observational study by Lu et al. [26].
Question 2.
What is the most appropriate management for infants with ambiguous genitalia or a DSD who present with a life-threatening complication as a result of their condition?
A review of the literature revealed no studies specifically evaluating the emergency management of children with ambiguous genitalia or DSD. We used the review articles by Sultan et al. [11] and Speiser and White [12].
Question 3.
What is the most appropriate approach to sex assignment in an infant with ambiguous genitalia or a DSD?
The literature search yielded the following articles that addressed the subquestions we posed in order to derive a final consensus.
 Should clinical decision making for DSD be physician-dependent or reside within a Gender Medicine Team? (Figure 1)
Should clinical decision making for DSD be physician-dependent or reside within a Gender Medicine Team? (Figure 1)

Two articles were useful in our attempt to answer this question: an evidence-based model by Schaeffer, et al. [27] and a study by Axelrad et al. [28].
 What role should the psychologist play on the Gender Medicine Team?
What role should the psychologist play on the Gender Medicine Team?
The review article by Parisi et al. [15] includes the use of a psychiatrist. The literature also yielded observational studies by Reiner and Gearhart [29], Migeon an Wisniewski [30], and Wisniewski et al. [31], as well as a review article in the American Academy of Pediatrics Section on Urology [32].
 What is the ethical framework for sex assignment?
What is the ethical framework for sex assignment?
We used a published critical appraisal tool to assess the literature on the ethics of DSD [33]. We also identified two proposed ethical frameworks for the management of DSD, by McCullough [34, 35] and by Wiesemann et al. [36], and a statement from an interdisciplinary research group from The Hastings Center by Frader et al. [37].
Question 4.
What is the most appropriate surgical management for infants with ambiguous genitalia or DSD?
To answer this question, we searched the literature for information addressing the following subquestions.
 What is the most appropriate surgical management for infants with CAH?
What is the most appropriate surgical management for infants with CAH?
The search yielded several useful articles: a retrospective observational study conducted by Stikkelbroeck et al. [38] and studies by Nordenskjöld et al. [39] and Schnitzer and Donahoe [40]. The evidence-based model by Schaeffer et al. [27] also provides details on the surgical management of CAH.
 What is the most appropriate feminizing surgery management of patients with DSD?
What is the most appropriate feminizing surgery management of patients with DSD?
The literature search yielded a total of 45 relevant English-written articles, 18 of which specifically addressed disorders resulting in 46, XX DSD and 16 of which addressed disorders resulting in vaginal agenesis, such as complete androgen insensitivity, Meyer Rokitansky Kuster Hauser syndrome, or CAH with urogenital sinus. All articles identified by the initial search criteria were scanned for significance by reviewing the title and abstract content. Additional articles were excluded if they were written in a language other than English, had no relevance to the question of interest, if they were case reports, review articles on the topic, expert opinions, or letters to the editor. Literature appraisal criteria determined the study quality and bias. Evaluation of available literature was based on GRADE criteria from weak recommendation with very low-quality evidence to strong recommendation with high-quality evidence. After GRADE criteria were applied, only 19 papers met standards for this intensive review to determine specific study characteristics such as age when surgery performed, need for reoperation or revision, Prader grading, and pubertal status.
 What is the most appropriate masculinizing surgery management of patients with DSD?
What is the most appropriate masculinizing surgery management of patients with DSD?
Total retrieval was 34 English and 6 non-English references. After initial abstract review, 13 articles were excluded because they did not address the questions of interest, or they were not applicable to our patient population. Ten articles were excluded because they were reviews or consensus statements. Six others were excluded because they were written in a foreign language. Thus, a total of 11 full articles in English were retrieved after abstract review. These studies were deemed to be eligible based on their potential to address the topics of interest. The GRADE criteria were applied to each study to evaluate its methodological quality. After analysis of all 11 articles for methodological rigor and relevance, we determined that there was a profound deficit of high-quality evidence to substantiate our recommendations. Therefore, we opted to accept all 11 manuscripts, despite their lesser quality and relative weaknesses and flaws, to be included in our assessment and to help guide our recommendations in this paper. Our review of the literature yielded low-quality data to support a single, unified surgical approach to patients with 46, XY DSD. The articles that were useful included a retrospective study by Chertin et al. [41], reports by Göllü et al. [42] and Lam et al. [43], a retrospective review by Nihoul-Fekètè et al. [44], and a long-term follow-up study by Farkas et al. [45], as well as reports by Mendonca et al. [46] and Lima et al. [47]. With regard to the appropriate timing of surgical intervention for patients with ovotesticular DSD and an underandrogenized perineum, no conclusive high-quality evidence was found.
 What is the most appropriate gonadectomy surgery management of patients with DSD?
What is the most appropriate gonadectomy surgery management of patients with DSD?
There are limited prospective studies available regarding gonadectomy for children and adolescents with disorders of sexual differentiation. Retrospective analyses and review articles were utilized using the following search terms: gonadectomy, malignant transformations, seminoma, and dysgenetic gonads. The articles we used were a case study by Olsen et al. [48] and reports by Dumic et al. [49] and Fallat and Donahoe [50].
4. Discussion
To evaluate and grade the evidence, we used the grading system developed by the GRADE, an international group with expertise in the development and implementation of evidence-based guidelines [9]. The GRADE system we used has been adopted by The Endocrine Society and a growing number of other organizations to develop clinical practice guidelines and to grade the strength of recommendations and the quality of the evidence [10, 51]. Linked to each recommendation is a description of the evidence, values that panelists considered in making the recommendation (when making these explicit was necessary), and remarks, a section in which panelists offer technical suggestions for testing conditions, dosing, and monitoring. These technical comments reflect the best available evidence applied to a typical patient. Often, this evidence comes from the unsystematic observations of the panelists and should, therefore, be considered "suggestions." A detailed description of this grading scheme has been published elsewhere [10].
The GMT task force has confidence that patients who receive care according to the strong recommendations will derive, on average, more good than harm. Strong recommendations require more careful consideration of the patient's circumstances, values, and preferences to determine the best course of action.
Based on this system, we developed our guidelines for each question identified in the Methods and Results sections, as noted below.
Question 1.
What constituted the most appropriate evaluation for infants with ambiguous genitalia or a DSD? The guideline for this question was developed after we reviewed and graded the literature for the following subquestions.
 What is the appropriate evaluation for CAH?
What is the appropriate evaluation for CAH?
The review article by Sultan et al. [11] recommends using a multidisciplinary team in every step of the diagnostic procedure, sex assignment, and treatment strategy. The authors suggest that the diagnostic workup should include family history, general examination for dysmorphic features, and grading based on the presence or absence of gonads and their palpability: (a) no gonads palpable (46, XX DSD, congenital adrenal hyperplasia [21-hydroxylase deficiency] or 46, XY DSD); (b) one gonad palpable, or abnormal gonadal differentiation (46, XY DSD, mixed gonadal dysgenesis [XO/XY], ovotesticular DSD); (c) two gonads palpable, or 46, XY DSD, impaired testosterone biosynthesis (androgen receptor defect 5c-reductase deficiency, ovotesticular DSD). This approach is relevant to more than just CAH. Approximately 75 percent of patients who present in the emergency room with ambiguous genitalia with hyponatremia and hyperkalemia and a lack of palpable testes have a diagnosis consistent with CAH.
Speiser and White [12] report that progress has been made with regard to the genetics of the various clinical forms of 21-hydroxylase deficiency, that the correlations between the genotype and the phenotype have been studied extensively, and that gene-specific prenatal diagnosis is now feasible. A consensus statement of the Joint LWPES/ESPE CAH Working Group [13] is in agreement with the statements made in the report by Speiser and White.
The newborn screen for CAH also might contribute insights in the diagnosis of a newborn in the setting of ambiguous genitalia with nonpalpable testes. However, the results of the newborn screen might not always precede the presentation [13].
There are no outcome studies addressing the above question.
Recommendation
We recommend that the standard workup for CAH include the following: electrolytes, glucose, 17OHP, plasma renin, D4 androstenedione, testosterone, 11deoxycortisol, and DHEA. (weak recommendation, very low-quality evidence).
 What is the most appropriate way to assess the hypothalamic pituitary gonadal axis in the context of ambiguous genitalia or hypothalamic pituitary hypogonadism?
What is the most appropriate way to assess the hypothalamic pituitary gonadal axis in the context of ambiguous genitalia or hypothalamic pituitary hypogonadism?
The underlying problem most likely is a hypothalamic GnRH pulse generator defect with subsequent hypogonadotropic hypogonadism. This condition might be in isolation or in the context of hypopituitarism. However, to establish the diagnosis of isolated hypogonadism in the context of micropenis, hypopituitarism needs to be ruled out. The GNRH pulse generator has developed and is well functional by the end of first trimester.
The article by Sultan et al. [11], who recommend the use of a multidisciplinary team in every step of the diagnostic procedure, sex assignment, and treatment strategy, was useful in this context as well as for addressing question (1a).
Grumbach [14] noted that because levels of FSH, LH, and sex steroid secretion are low in childhood and male infant levels of testosterone increase during the second week, reaching a maximum at 4 to 10 weeks and declining to low levels by the time the child is approximately 6 months old, in the scenario of micropenis with or without cryptorchidism, it is imperative to exploit the window of opportunity in order to establish the diagnosis hypogonadotropic hypogonadism. If the infantile GnRH gonadotropin spurt is captured, hypogonadotropic hypogonadism would be identified by the blunt response or ruled out by the appropriate peak. Establishing the diagnosis of hypogonadotropic hypogonadism in infancy precludes the uncertainties and delays in distinguishing constitutional delay in puberty from hypogonadotropic hypogonadism. Accordingly, hormone replacement therapy can be initiated at the normal age of pubertal onset. Infants with micropenis should be administered testosterone.
Parisi et al. [15] describe a Gender Assessment Team that has provided a multidisciplinary approach to the diagnosis, medical and surgical treatment, genetic counseling, and psychosocial support of 250 patients with DSD. These authors recommend that the endocrine evaluation include an assessment of the function of the hypothalamic pituitary gonadal axis and that studies include a gonadotropin profile, assessment of gonadal function, and assessment of other pituitary axes when indicated. The article states that tests are most revealing when obtained in infants between 2 and 4 months old.
There are no outcome studies addressing the above question.
Recommendation
We recommend the use of a multidisciplinary team for the assessment of the hypothalamic pituitary gonadal axis, that the diagnosis of hypogonadotropic hypogonadism should be established within the first 6 months of life, and that appropriate hormonal replacement therapy should be initiated immediately. (Strong recommendation, very low-quality evidence).
 What is the most appropriate evaluation for micropenis and for undescended testes for the evaluation of primary hypogonadism most likely in the context of dysgenetic testes?
What is the most appropriate evaluation for micropenis and for undescended testes for the evaluation of primary hypogonadism most likely in the context of dysgenetic testes?
In the context of primary hypogonadism, dysgenetic testes need to be ruled out. In their retrospective observational study, Kolon et al. [16] evaluated 77 prepubertal boys diagnosed with hypospadias, cryptorchidism, or micropenis. Sixty boys underwent one dose of human chorionic gonadotropin (hCG), and 17 underwent three daily age-adjusted doses of hCG. In the one-dose group, poststimulation testosterone was elevated 22- to 29-fold from baseline after a weight-based dose was administered and 34- to 35-fold after a dose based on body surface area was given. Testosterone increased 20-fold baseline in the multidose group. No significant difference was noted between the dihydrotestosterone levels in the single weight-based dose and the three-injection regimen.
In a retrospective observational study, Davenport et al. [17] reviewed the value of the hCG test in the evaluation of prepubertal boys with bilateral impalpable testes. The study was comprised of 31 boys, all of whom had an hCG test consisting of three intramuscular injections of hCG on successive days at a daily dose dependent on their age ( 1 year old, 500 units; 1–10 years, 1000 units;
1 year old, 500 units; 1–10 years, 1000 units;  10 years, 1500 units). Twenty-two boys responded to hCG and had testes the sizes of which were related to the degree of testosterone elevation after the stimulatory test. hCG had a positive predictive value of 89 percent and a negative predictive value of 100 percent. Measurements of gonadotropins and sex hormones can be substituted occasionally instead of hCG, in a narrow window when the infant is 14 days old to 90 days old [14].
10 years, 1500 units). Twenty-two boys responded to hCG and had testes the sizes of which were related to the degree of testosterone elevation after the stimulatory test. hCG had a positive predictive value of 89 percent and a negative predictive value of 100 percent. Measurements of gonadotropins and sex hormones can be substituted occasionally instead of hCG, in a narrow window when the infant is 14 days old to 90 days old [14].
The observational study conducted by Misra et al. [18] examined the role of Mullerian inhibiting substance (MIS) determination in the evaluation of 218 boys with mircorphallus and/or cryptorchidism. MIS was normal in 69.2 percent of boys with isolated microphallus compared with 38.1 percent of boys with microphallus and coexisting cryptorchidism ( ).
).
Recommendation
We recommend using hCG stimulation for the evaluation of primary hypogonadism and obtaining basal MIS measurement. (Strong recommendation, low-quality evidence).
 What is the most appropriate evaluation for peripheral defects leading micropenis, hypospadias, with respect to
What is the most appropriate evaluation for peripheral defects leading micropenis, hypospadias, with respect to
-
(1)
the action of testosterone, which could be in the context of
-
(a)
5 alpha-reductase deficiency.
-
(a)
In a retrospective observational study, Boehmer et al. [19, 20] reviewed 49 cases with presumptive diagnosis of androgen insensitivity syndrome. The review found that in 32 of the 49 (65.3%) patients, an androgen receptor gene mutation was found.
A case report on a 65-year-old male with 5 alpha-reductase deficiency 46, XY DSD was described by Imperato-McGinley et al. [21]. The man had no medical intervention before, during, or after puberty. The authors discovered that plasma levels of dihydrotestosterone and the in vivo conversion of radiolabeled testosterone to dihydrotestosterone were decreased.
In addition, an original pertinent case study by Cai et al. [22] of four Dominican families based on a study published in 1974 describes a large Dominican kindred of 23 families with 38 affected subjects, pointing to the autosomal recessive nature of the disease. Characterization of 5 alpha-reductase enzyme activity in cultured genital skin fibroblasts demonstrated a pattern of enzyme activity distinctly different from three previously described families with this condition. Single-strand polymorphism and DNA sequencing were used. Two other mutations of the 5 alpha-reductase-2 gene were found in affected subjects from two of the four families. One of these families had a point mutation on exon 2 of the 5 alpha-reductase-2 gene, in which substitution of adenine (GAC) for guanine (GGC) caused an aspartic acid replacement of glycine at amino acid 115 (G115D), and the other family had a substitution of adenine (AGT) for guanine (GGT) on exon 3, causing a serine replacement for glycine at amino acid 183 (G183S). Affected subjects from the two remaining families demonstrated the same exon 5 mutation of the 5 alpha-reductase-2 gene as previously detected in the large Dominican kindred. The phenotypic and biochemical characteristics of the 46, XY DSD were similar regardless of the genetic defect, except that one affected subject (C-VI-2) with the same exon 5 mutation as the large Dominican kindred had much more facial and body hair.
(b)biochemical and molecular genetic testing for androgen receptor defect
Deeb et al. [23] report a patient with severe undermasculinization and poor response to exogenous androgens. Androgen binding was performed, the AR gene was sequenced, and functional studies of the mutant protein were performed. The authors found that androgen binding was normal and that the novel mutation (A629W) in the AR hinge region resulted in severe undermasculinization at birth and resistance to androgens.
The McGill Androgen Receptor Gene Mutations Database [52] holds a collection of such characterized mutations in the AR gene, providing a valuable tool of genotype-phenotype correlation.
Although the diagnostic tools of testosterone dihydrotestosterone and their ratios either in minipuberty or under hCG are applied for confirmation of the diagnosis or for genetic counseling, it is necessary to proceed with the molecular diagnosis. Likewise, although it has been reported that MIS levels are helpful for indirect evaluation of androgen receptor defects, this observation is based on only a few reports [53].
Recommendation
We recommend (1) screening the androgen receptor gene for mutations, (2) studying androgen receptor expression and androgen binding in genital skin fibroblasts, and (3) evaluating testosterone levels. (Strong recommendation, very low-quality evidence).
(2)the production of testosterone with respect to the enzymatic machinery?
Codner, et al. [24] conducted an observational study to determine whether some patients with idiopathic hypospadias have HSD3B2 mutations. They measured basal plasma renin activity and performed an ACTH test for determination of 17-OH-pregnenolone, 17-OH-progesterone, cortisol, dehydroepiandrosterone sulfate, and androstenedione, and they used a human chorionic gonadotropin test for the determination of androstenedione, testosterone, and dihydrotestosterone on 90 patients with penile or perineoscrotal hypospadias and 101 healthy fertile male controls. They did not observe a clear steroidogenic pattern suggestive of 3 beta-HSD deficiency in any patient.
Eckstein et al. [25] conducted an observational study in six Arab individuals with familial 46, XY DSD caused by 17-beta hydroxysteroid dehydrogenase deficiency. The study revealed several metabolic aberrations associated with the disorder. The study also found that plasma androstenedione concentrations increased with age (29 ng/dL at 3 years of age to 563 ng/dL at 26 years of age) and that hCG markedly increased the plasma androstenedione in all six patients.
Recommendation
We recommend administering hCG to patients in order to increase androstenedione secretion, allowing for the diagnosis of the defect in prepubertal individuals. (Strong recommendation, low-quality evidence).
Widely available androgen receptor gene molecular testing is available allowing the detection of hundreds of clinically recognized mutations and further confirmation of the clinical diagnosis of complete and partial androgen insensitivity.
Recommendation
We recommend screening the androgen receptor gene for mutations, in cases of suspected complete or partial androgen insensitivity. (Strong recommendation, low-quality evidence).
Clinical molecular testing is now available for the evaluation of the 5 alpha-reductase-2 gene, building on knowledge gained from clinical cases, as outlined above, and correlation with mutations identified on both research and clinical bases. As with defects in the androgen receptor gene, although measuring testosterone, dihidrotestosterone, and their ratios either in minipuberty or under hCG can be helpful, confirmation of affected status suspected biochemically can now be diagnosed by molecular genetics.
Recommendation
We recommend molecular testing for 5 alpha-reductase-2 gene mutations when suspected based on phenotypic and biochemical characteristics. Overall, the GMT task force recommends the use of various diagnostic procedures and a multidisciplinary team approach for the workup of infants with ambiguous genital or a DSD. (Strong recommendation, very low-quality evidence).
 What genetic testing should be performed for ambiguous genitalia?
What genetic testing should be performed for ambiguous genitalia?
Parisi et al. [15] recommend karyotype analysis on peripheral blood or skin fibroblasts derived from genital skin or other sources, fluorescence in situ hybridization (FISH) to augment routine cytogenetics for rapid analysis and evaluation for sex chromosome mosaicism and/or chimerism, FISH for presence or absence of the sex-determining region on the Y chromosome (SRY), specialized molecular genetic testing for Y chromosome deletions, and other additional specialized genetic tests if indicated, based on the specific condition being evaluated.
The genetic field also has seen the emergence of array comparative genomic hybridization (aCGH), which is proving very useful in the evaluation of cases of ambiguous genitalia by simultaneously being able to provide the same information as a standard karyotype, evaluate for sex chromosome mosaicism and/or chimerism, and detect the presence or absence of SRY. This technology also has the advantage of being able to detect copy number abnormalities in the rest of the genome, which have traditionally been below the resolution of a standard karyotype. A growing number of such regions are being associated with ambiguous genitalia.
A retrospective observational study by Lu et al. [26] evaluated 638 neonates with various birth defects who were referred for chromosomal microarray analysis. Twelve patients presented with ambiguous genitalia. Targeted array-based comparative genomic hybridization had an overall detection rate of 33.3 percent in patients with ambiguous genitalia. This methodology can expedite and simplify the evaluation for ambiguous genitalia by identifying genomic imbalances and in some cases even mosaic abnormalities precisely and rapidly, providing timely molecular diagnoses, detecting more clinically relevant genomic abnormalities than can conventional cytogenetic studies, and supporting more informed decision making and management.
Recommendation
We recommend obtaining a karyotype and including additional testing as appropriate based on the phenotype and karyotype of the patient. We also recommend including array CGH testing as a part of the genetic workup for DSD. (Strong recommendation, low-quality evidence).
Question 2.
What is the most appropriate management for infants with ambiguous genitalia or a DSD who present with a life-threatening complication as a result of their condition?
The review article by Speiser and White [12] describes the workup required in cases of emergencies. These authors recommend that for CAH (and they include hypopituitarism with modifications), management should be directed toward the emergency condition: (a) for cases of suspected CAH (salt-losing variety), the physician should order a laboratory workup; the infant should be treated with D5 NS (dextrose in normal saline) and stress steroids (100 mg/m 2/day), with treatment modified after 24 hours, based on electrolyte correction; Florinef (0.1 mg po qd) should be added, with a switch to table salt (2.5 grams po qd/given in 24-hr worth of formula); (b) for cases of micropenis, and suspicion of hypopituitarism (the concern is hypoglycemia), the pituitary adrenal axis should be assessed for production of cortisol; the physician should initiate treatment (stress steroids: 100 mg/m 2/day Solucortef) while laboratory results are pending; (c) if neither of the acute conditions is the final diagnosis, the physician should withhold treatment until after the results of the workup are available.
Sultan et al. [11] recommended management of the acute presentation of suspected CAH with Solucortef stress doses and management of the chronic condition with glucocorticoids (hydrocortisone 10 to 20 mg/m²/day:tid Mineralocorticoids: 0.1 to 0.2 mg of Fludrocortisone sodium chloride 1 to 2.5 grams or 17 to 42 mmol of sodium chloride daily).
There are no outcome studies addressing the above question.
Recommendation
We recommend that treatment with stress dose steroids be initiated immediately, pending laboratory results. (Weak recommendation, very low-quality evidence).
Question 3.
What is the most appropriate approach to sex assignment in an infant with ambiguous genitalia or a DSD?
The guideline for this question was developed after we reviewed and graded the literature for the following subquestions.
 Should clinical decision-making for DSD be physician-dependent or reside within a Gender Medicine Team?
Should clinical decision-making for DSD be physician-dependent or reside within a Gender Medicine Team?
Practical guidelines have not been established for this situation as there are few outcome studies, and decision-making criteria have not been formally developed. Accordingly, we incorporated systematic reviews of the literature, which have guided and formulated our consensus practice at Texas Children's Hospital (TCH).
A review article by Schaeffer et al. [27] interprets and translates the 2002 consensus statement [13] noted earlier into medical, surgical, and mental health protocols and provides preliminary evidence that such protocols result in improved care and support for patients and families.
In an article by Axelrad et al. [28], the multidisciplinary Gender Medicine Team approach used at TCH is described and is recommended over the traditional physician-determined approach. The TCH approach includes (a) an ethical framework involving a team of specialists (including an ethicist) and (b) education and participation of the parents in the decision-making process. It is more comprehensive than other approaches previously reported and is designed to meet the multifaceted needs of individuals with DSD.
There are no outcome studies addressing the above question.
Recommendation
We recommend the use of a consensus approach that includes an ethical framework for parental decision-making, rather than the traditional physician-determined approach, when determining sex assignment in an infant with ambiguous genitalia or a DSD. (Strong recommendation, very low-quality evidence).
 What role should the psychologist play on the Gender Medicine Team?
What role should the psychologist play on the Gender Medicine Team?
Specific guidelines have not been established for this component as there are few outcome studies, and decision-making criteria have not been formally developed. Our clinical experience and the literature have shown that during diagnosis, medical workup, acute management, sex assignment, and throughout treatment, parents and affected children often have difficulties coping, have questions about how to manage inquiries from family and friends, experience uncertainty about the future, and at times demonstrate significant symptoms of anxiety and depression. The main task of the psychologist is to assist in the education and involvement of the parents to the best of the ability of the family members and to assess whether psychosocial difficulties are impacting the understanding of guidelines by any family members. The psychologist assists the family members in coping with the presentation of a medical difficulty in their child as well as normalizing the taboo often associated with the particular diagnoses involved [28].
Parisi et al. [15] include a psychologist in the recommendation for a team approach. An observational study by Reiner and Gearhart [29] assessed 16 genetic males in a cloacal-exstrophy clinic at the ages of 5 to 16 years. Eight of the 14 subjects assigned to female sex declared themselves male during the course of the study whereas the two children reared as male remained male. Sexual identity varied among the subjects assigned the female sex. Five persistently declared unwavering female identity, one refused to discuss sexual identity, and eight declared unwavering male identity. All subjects living as females expressed difficulty fitting in with female peers. The study revealed that neonatal sex assignment can result in unpredictable sexual identification and can present a variety of issues related to a child's psychosexual development.
In their observational study, Migeon et al. [30] interviewed 75 adults with 45, XY karyotype who presented as infants or children with variable degrees of undermasculinization of their genitalia treated at the Johns Hopkins Hospital Endocrine Clinic. Participants' knowledge of their condition, satisfaction with their knowledge, and desire for additional education about their intersex conditions were assessed. Almost half of the patients, reared male or female, were neither well-informed about their medical and surgical history nor satisfied with their knowledge.
The observational study by Wisniewski [31] assessed by questionnaire and medical exam 14 women with complete androgen insensitivity syndrome (CAIS). Eleven of the 14 (78%) women reported satisfaction with their genitalia; eight of the 14 (57%) women reported being mainly satisfied with their bodies; and five of the 14 (36%) reported being somewhat dissatisfied. All 14 women were satisfied with their sex of rearing, and 93 percent of women reported being heterosexual. The majority of women with CAIS studied received some form of counseling (83%) at various ages and for various lengths of time concerning aspects of their syndrome.
The review article in the American Academy of Pediatrics Section on Urology [32] considers the psychological factors associated with elective surgery on the genitalia of male children with hypospadias. The article noted that emotional, cognitive, and body-image development may be affected profoundly by both the genital deformity and the reconstructive surgery, and that aesthetic trauma varies dramatically by age. Postoperative behavioral problems such as aggressive or regressive behavior, night terrors, and anxiety may be more common at certain ages.
The description of the team approach by Axelrad et al. [28] includes a psychologist for various stages of the process and for family members.
Recommendation
We recommend the presence of a psychologist on the Gender Medicine Team to provide support to both patients and caregivers. (Strong recommendation, low-quality evidence).
 What is the ethical framework of sex assignment?
What is the ethical framework of sex assignment?
We used a published critical appraisal tool to assess the literature on the ethics of DSD: "Argument-based medical ethics: a formal tool for critically appraising the normative medical ethics literature" [33]. We identified two proposed ethical frameworks for the management of DSD, by McCullough [34, 35] and by Wiesemann et al. [36] in "Ethical principles and recommendations for the medical management of differences of sex development (DSD)/intersex in children and adolescents", and a statement from an interdisciplinary research group from The Hastings Center by Frader et al. [37]. The ethical frameworks and the statement emphasize the need to base ethical judgments on an evidence-based assessment of the affected infant; the centrality of the best interests of the infant and child it will become; the obligation of healthcare professionals to involve parents in the decision-making process; the obligation to avoid irreversible interventions and to undertake them only when they can be rigorously justified as necessary to protect and promote the interests of the infant and child it will become; the need to involve children in decision making appropriate to their developmental stages; the obligation to take into account the biopsychosocial variation in sex, gender, and gender identity and also cultural changes in which rigid gender identities and roles are being challenged by gender ambiguity.
The tools of ethics are (a) analysis of concepts to ensure that their meaning is clear and (b) argument, the use of logical reasoning to identify the implications of ethical concepts. These implications should then guide clinical judgment, decision making, and management. Rigorous use of concepts to make arguments produces conclusions that can be relied up to guide clinical practice.
The ethics of using clinical guidelines is based on the concept of fiduciary responsibility for the patient. This ethical concept was introduced into the history of medical ethics by two British physician-ethicists in the eighteenth century, John Gregory (1724–1773) of Scotland and Thomas Percival (1740–1804) of England.
Fiduciary responsibility has three components. (1) Physicians and other healthcare professionals should become scientifically and clinically competent by adhering to the rigors of the scientific method, as articulated in Francis Bacon's (1561–1626) "experience"-based philosophy of medicine. This was a nascent form of what has become evidence-based reasoning. The goal is to submit clinical judgment and decision making to the discipline of experience-based (evidence-based) practice to reduce bias in, and thereby increase the scientific reliability of, clinical judgment and decision making and thus create the intellectual integrity of the profession of medicine. (2) Physicians and other healthcare professionals should make the protection and promotion of the patient's health-related interests their primary concern and motivation. (3) Physicians and other healthcare professionals should treat medicine, psychology, nursing, and the other healthcare professions as public trusts that exist for the benefit of future physicians, patients, and society [33].
Practice guidelines are an essential tool for implementing the first component routinely in clinical practice. This consideration is especially important in the responsible management of DSD in light of the history of wide variation in clinical judgment and practice, resulting in many unnecessary and irreversible surgical interventions that have not been uniformly clinically beneficial and often clinically harmful.
Responsible management of DSD is guided by two ethical considerations. The first is to take account of the variations in the different components of biological sex, including genomic sex, anatomic sex (internal and external), hormonal sex, and brain sex and to appreciate that the more discordant these components of biological sex, the more variation that will be observed in subsequent gender, including gender identity and sexual orientation. When the components of biological sex align strongly, reliable predictions of gender identity can be made and recommendations for sex assignment can be made accordingly. The second ethical consideration is to prevent irreversible anatomic and physiologic effects of surgical assignment of sex, an especially compelling ethical consideration when the components of biological sex do not strongly align. The goal in such cases should be to preserve the anatomic and physiologic components of a change in gender identity later in a child's life [34].
There are no outcome studies addressing the above question.
Recommendation
We recommend that an ethicist be consulted on each case to ensure that the patient's individual needs are addressed according to the ethical framework established by the GMT. (Strong recommendation, very low-quality evidence).
Question 4.
What is the most appropriate surgical management for infants with ambiguous genitalia or DSD?
The guideline for this question was developed after we reviewed and graded the literature for the following subquestions.
 What is the most appropriate surgical management for infants with CAH?
What is the most appropriate surgical management for infants with CAH?
The retrospective observational study conducted by Stikkelbroeck et al. [38] evaluated eight female patients with salt-wasting CAH who underwent feminizing surgery in infancy from 1973 to 1983. The study consisted of a review of the patients' medical records ( ), a systematic evaluation of the current situation (
), a systematic evaluation of the current situation ( ) that included a written questionnaire to screen for psychopathology (YASAR), a structured gynecological examination, and a psychosexual interview. The patients were matched to 19 healthy female controls. Patients underwent various surgical interventions: clitoris reduction and single-stage vaginoplasty (
) that included a written questionnaire to screen for psychopathology (YASAR), a structured gynecological examination, and a psychosexual interview. The patients were matched to 19 healthy female controls. Patients underwent various surgical interventions: clitoris reduction and single-stage vaginoplasty ( ), and revaginoplasty (
), and revaginoplasty ( ). In the interviews, four patients identified themselves as heterosexual. Sexual milestones had been reached by all patients. Satisfaction with height, body hair, and external genitalia and sexual fantasies and interests in the patient group did not differ from the control group.
). In the interviews, four patients identified themselves as heterosexual. Sexual milestones had been reached by all patients. Satisfaction with height, body hair, and external genitalia and sexual fantasies and interests in the patient group did not differ from the control group.
A follow-up study by Nordenskjöld et al. [39] on 62 women with CAH aged 18 to 63 years and 62 age-matched controls to correlate findings of both operative method and mutations revealed no significant differences between the ability of controls and cases to achieve orgasm. Cases were more likely than controls to be unsatisfied with their vagina ( ), to experience pain during intercourse (
), to experience pain during intercourse ( ), to make their sexual debuts later in life (
), to make their sexual debuts later in life ( ), and not to have children (
), and not to have children ( ).
).
Schnitzer and Donahoe [40] describe the appropriate surgical therapy for infants with CAH. The authors recommend an early one-stage reconstructive surgery, with the patient's steroid replacement increased beforehand. The mainstays of the surgical repair are clitoral recession, correction of the urogenital sinus defect that results from failure of the vagina to complete migration to the perineum, and exteriorization of the vagina. The authors also recommend that the labioscrotal folds be trimmed, thinned, and elongated to create a more normal-appearing labia majora.
Schaeffer et al. [27] also recommend surgery according to the protocols they reviewed.
Recommendation
We recommend performing early, one-stage feminizing surgery for female infants with CAH. (Strong recommendation, low-quality evidence).
 What is the most appropriate feminizing surgery management of patients with DSD?
What is the most appropriate feminizing surgery management of patients with DSD?
Surgical management for children with disorders of sex development is a complex process that must be individualized with several goals in mind: preserving normal genital sensation, creating a normal introitus and providing an adequate vaginal opening at the perineum. A variety of techniques have been reported in the literature in the last few decades, but controversy remains with regard to the timing of performing feminizing genitoplasty and neovaginal reconstruction [54–56]. In various studies, children undergoing feminizing genitoplasty for a variety of DSD ranged in age from 1 day old to 33 years with mean follow-up periods of 2 months to 16 years. Stenosis rates reported in studies addressing delayed vaginoplasty ranged from 0 to 61.9 percent. Adequate vaginal length was reported in 60 to 100 percent of cases. Because there are no randomized controlled trials reported in this population with regard to specific types of surgical techniques or timing of reconstruction, data are limited to both small and large retrospective cohort studies, case series, case reports, and expert opinion.
Although most studies reported patient satisfaction with regard to cosmesis, stenosis rates were reported as high as 35 percent. Because of the small numbers within data subsets, an effect could not be assessed directly with regard to repair of a high vaginal defect as compared to a low urogenital sinus defect. Furthermore, the studies reviewed demonstrated too many inconsistencies to make direct head-to-head study comparisons.
Only three studies reported on pubertal evaluation following primary surgery as infants or toddlers. Specific outcomes with regard to sexual function or sensation were not available for those who underwent early feminizing genitoplasty.
The review addressing the appropriate timing and recommended surgical therapy for children with ambiguous genitalia consistent with 46, XX DSD or with conditions resulting in vaginal agenesis yielded 12 retrospective cohorts ( ranging from 11–178 patients) [57–68], 16 prospective cohorts (
ranging from 11–178 patients) [57–68], 16 prospective cohorts ( ranging from 14–200 patients) [69–84] and seven case series (
ranging from 14–200 patients) [69–84] and seven case series ( ranging from 3–8 patients) [85–91] published between 1995–2008.
ranging from 3–8 patients) [85–91] published between 1995–2008.
Studies addressing early feminizing genitoplasty for patients with Prader grade II–V included primary outcome measures of cosmetic result and stricture or stenosis formation [57–62, 69–77, 85–88]. Studies in this category reported mean age at the time of surgical reconstruction as well as at follow-up periods. Children undergoing feminizing genitoplasty for a variety of DSDs (CAH, mixed gonadal dysgenesis [MGD], ambiguous genitalia, androgen insensitivity syndrome [AIS], ovotestis, true hermaphrodite, intersex, Mayer Rokitansky Kuster Hauser [MRKH], adrenogenital syndrome, etc.) ranged in age from 1 day old to 33 years, with mean follow-up periods of 2 months to 16 years [57–62, 69–77, 85–88]. Although most studies reported patients' satisfaction with regard to cosmesis, stenosis rates were reported as high as 35 percent [69].
Because of the small numbers within data subsets, an effect could not be assessed directly with regard to repair of a high vaginal defect as compared to a low urogenital sinus defect. Furthermore, studies reviewed demonstrated too many inconsistencies to make direct head-to-head study comparisons. For instance, six studies reported one surgeon and one technique [58, 70–73, 85], five studies reported multiple surgeons ranging from one technique to several surgical techniques [75–77, 87, 88], and seven studies did not specifically list number of surgeons or techniques involved [57, 59–62, 74, 85, 86]. Only three studies reported on pubertal evaluation following primary surgery as infants or toddlers [71, 75, 86].
Specific outcomes with regard to sexual function or sensation were not available for those who underwent early feminizing genitoplasty. For delayed vaginoplasty, 16 studies reporting on eight different techniques (Dilator therapy, McIndoe, Davydov, Vecchietti, Sigmoid, Amnion, Creatsas, Williams) between 1997, and 2010 were assessed [63–68, 78–84, 89–91]. Reasons for performing vaginoplasty included MRKH, CAH, AIS, MGD, cloaca, vaginal agenesis, and true hermaphrodite. Patients' ages ranged from 7 to 26 years old at the time they underwent isolated vaginoplasty. Thirteen studies included only pubertal or postpubertal patients [63, 66, 67, 78–84, 89–91] whereas three studies included prepubertal females [64, 65, 68]. Follow-up periods varied from 3 to 111 months. Stenosis rates reported in studies addressing delayed vaginoplasty ranged from 0 to 61.9 percent [63–68, 78–84, 89–91]. Adequate vaginal length was reported in 60 to 100 percent of cases. Unwanted vaginal discharge was assessed in four studies utilizing bowel for neovaginal reconstruction, ranging from 4.3 to 100 percent [63–68, 78–84, 89–91].
Several consensus documents addressed disorders of sexual differentiation [54–56]. A clear trend throughout all existing recommendations is toward multidisciplinary management. Pediatric surgeons, urologists, and gynecologists advocate that cases of DSD should be individualized and no gender assignment should be made without proper evaluation. Surgical correction is delayed until a definitive diagnosis has been established. However, once established, the rationale for early surgical correction includes beneficial effects of estrogen in the initial 6 months postdelivery for wound healing and limiting postoperative stricture formation, minimizing family distress related to anatomic concerns, and mitigating the risks of stigmatization or gender identity confusion. Despite the best intentions, adverse outcomes also have led to recommendations from some organizations to delay surgery until an appropriate age of informed consent [54, 57, 58, 70]. Other surgeons still have advocated for staging feminizing genitoplasty based on the location of the vaginal confluence, though no prospective studies have specifically evaluated the many techniques for urogenital sinus repair.
Most surgeons agree that vaginoplasty cases may be more appropriately delayed among those requiring more complex reconstruction or at high risk for stricture formation [57, 58, 60, 70]. If decisions are made to perform clitororeduction, modern surgical trends are toward conservation of neurovascular and/or erectile structures, although long-term satisfaction and sexual function are unknown [54, 56, 70, 85, 87].
Finally, all consensus opinions recommend full informed consent prior to initiating the reconstruction process, with the caveat that certain cases may require staged procedures and/or revision in adolescence or adulthood [54–56].
Recommendation
We recommend that cases be individualized due to the spectrum in presentation, and that surgery should be delayed until a definitive gender assignment can be established. (Strong recommendation, low-quality evidence).
 What is the most appropriate masculinizing surgery management of patients with DSD?
What is the most appropriate masculinizing surgery management of patients with DSD?
Our review of the literature revealed scant and low-quality data to support a single, unified surgical approach to patients with 46, XY.
Techniques described for surgical reconstruction of the patient with an undermasculinized perineum and male gender assignment include staged versus primary hypospadias repair, scrotoplasty, orchidopexy, open or laparoscopic removal of müllerian structures, and insertion of prostheses. Controversy continues regarding the appropriate surgical technique(s) and the timing of surgical intervention, as no randomized controlled trials have been performed on this patient population. Our results yielded a variety of outcomes.
The 57 patients in the series by Chertin, et al. [41] who underwent various masculinizing genitoplasty techniques, according to the quality of the urethral plate, were evaluated at 6-year follow-up: 7 percent of children had breakdown of the urethroplasty and required redo surgery, 12.8 percent developed a urethral fistula requiring closure, and 59 percent achieved satisfactory cosmetic and functional results per parental and surgeon assessment.
The series of 85 children reported by Göllü et al. [42] had results that were contrary to other studies evaluating the outcomes of staged hypospadias repair, with a 34 percent complication and re-do operation rate.
Lam et al. [43] reported that of the 44 boys in their study who underwent staged repair, the complications rates were 6.8 percent for fistula formation and 23 percent for stricture. The minor complication rates reported were expected given the long neourethras created in the procedures they underwent. Mild pain with erection was reported by 8 percent; 92 percent were pleased with their physical appearance.
The retrospective study by Nihoul-Fékété et al. [44] of patients undergoing early corrective surgery for 46, XY DSD and ovotesticular DSD had a negative correlation between the number of basal procedures required and the year of birth, likely due to the adoption of one-stage procedures after 1980. Fourteen-year follow-up revealed that anatomical results were worse for idiopathic 46, XY DSD ( ), with three patients needing multiple surgical interventions and developing fistulas; one patient had an untreatable penile deformity. These authors also report that poor brain masculinization occurs in androgen receptor deficiency, explaining why sex reversal is rare in partial androgen insensitivity. In their series, patients with partial androgen insensitivity reared as males had very poor self-reported satisfaction after surgical treatment (range 3–11 operations) due mainly to buried penis and micropenis. Only one of four patients with deficiency caused by 5 alpha-reductase underwent the typical male gender transition that follows virilization during puberty. All four others requested female genitoplasty and appear to be well adjusted.
), with three patients needing multiple surgical interventions and developing fistulas; one patient had an untreatable penile deformity. These authors also report that poor brain masculinization occurs in androgen receptor deficiency, explaining why sex reversal is rare in partial androgen insensitivity. In their series, patients with partial androgen insensitivity reared as males had very poor self-reported satisfaction after surgical treatment (range 3–11 operations) due mainly to buried penis and micropenis. Only one of four patients with deficiency caused by 5 alpha-reductase underwent the typical male gender transition that follows virilization during puberty. All four others requested female genitoplasty and appear to be well adjusted.
In the long-term follow-up study by Farkas and Rosler [45] of 16 patients who underwent masculinizing genitoplasty for 17-hydroxysteroid dehydrogenase deficiency, in which a staged approach was used in most patients, complications included complete breakdown of the neourethra requiring re-do surgery in one patient, and three small fistulae, and development of distal meatal stenosis and orchidoepididymitis in one patient who underwent single-stage reconstruction. Overall, the authors conclude that combination of testosterone and staged surgery resulted in pleasing appearance of external genitalia in most patients and recommended MGP for androgen-responsive patients with 17-hydrogenase deficiency.
Mendonca et al. [46] reported a cohort of 46, XY patients with 5 alpha-reductase deficiency in Brazil; 14 of 25 patients registered as the female social sex changed to a male gender role around the time of puberty. Thirteen of these patients, after psychological evaluation, underwent 2- or 3-stage surgery consisting of orthophalloplasty, scrotoplasty with resection of vaginal pouch, urethroplasty, and orchidopexy when necessary. The most frequent complications were urethral fistula ( ) and scrotal abscess (
) and scrotal abscess ( ); one patient had bilateral epididymitis with transient penile and scrotal edema. Psychological evaluation of 25 patients reared as females revealed male identity in 13 of them. Subjects treated at a later age described social inadequacy, psychological anguish, and suicidal ideas, and all would have preferred to have been treated in childhood. Patients who changed to male sex appeared to have a better social adjustment than did those who kept female social sex. Thus, the authors conclude that their findings support the theory that in utero or postnatal exposure to testosterone leads to imprinting of male sexual identity.
); one patient had bilateral epididymitis with transient penile and scrotal edema. Psychological evaluation of 25 patients reared as females revealed male identity in 13 of them. Subjects treated at a later age described social inadequacy, psychological anguish, and suicidal ideas, and all would have preferred to have been treated in childhood. Patients who changed to male sex appeared to have a better social adjustment than did those who kept female social sex. Thus, the authors conclude that their findings support the theory that in utero or postnatal exposure to testosterone leads to imprinting of male sexual identity.
Lima et al. [47] reported that the six male patients in their study who underwent laparoscopic removal of Müllerian duct remnants had no complications, resumed oral intake by postoperative day one, and were discharged by day 5 after their catheters were removed. All patients remained free from urogenital tract infections, voiding dysfunctions or urinary incontinence at a follow-up range of 6 months to 4 years. The authors conclude that when compared with other surgical approaches, the laparoscopic approach provides minimally invasive access to the retrovesical space with excellent exposure, decreasing the incidence of complications and operative time and avoiding large scars.
With regard to the appropriate timing of surgical intervention for patients with ovotesticular DSD and an underandrogenized perineum, no conclusive high-quality evidence was found. Most manuscripts reviewed point to early surgical intervention once male sex assignment is made in an effort to minimize parental anxiety and the long-term psychological effects on the patient.
Recommendation
We recommend postponing surgical management until concordance can be established. For underandrogenized male patients and underlying testosterone deficiency, particularly 17-beta hydroxysteroid dehydrogenase deficiency, and incomplete androgen insensitivity, we recommend preoperative testosterone stimulation to confirm penile response to androgens and increase in phallus size, followed by masculinizing genitoplasty and orchidopexy. For underandrogenized male patients with 5 alpha-reductase deficiency, we recommend pre-operative testosterone stimulation followed by hypospadias repair and scrotoplasty, as well as dihydrotestosterone replacement. (Strong recommendation, low-quality evidence).
 What is the most appropriate gonadectomy surgery management of patients with DSD?
What is the most appropriate gonadectomy surgery management of patients with DSD?
The study by Olsen et al. [48] of a 15-month-old phenotypic female who was diagnosed as having 46,XY gonadal dysgenesis following karyotyping for Turner-like features resulted in gonadectomy at the time of bilateral ureteral reimplantation for vesicoureteral reflux showed gonadoblastoma; malignancy was established at 15 months.
In the case study by Dumic et al. [49], a 9-month-old infant with hypertrophic clitoris and separated urethral and vaginal opening was diagnosed as having 46,XY incomplete "pure gonadal dysgenesis." Examination of both gonads revealed gonadoblastoma and bilateral salpingo-gonadectomy; partial hysterectomy was performed.
Fallat and Donahoe [50] note that the gonads most at risk for malignant transformation are both dysgenetic and intraabdominal and that early gonadectomies are recommended, as malignancies have been reported in infancy. Predominant risk groups include syndromes of gonadal dysgenesis and Ullrich-Turner syndrome. Partial gonadectomy is feasible in individuals with ovotesticular DSD commensurate with sex of rearing. Histologically normal intraabdominal gonads may be left through puberty (androgen insensitivity syndromes) [31]. A palpably normal descended gonad in a child with a Y chromosome can be observed if the child is reared as male. Certain intersex syndromes with splice variants of the WT1 gene are susceptible to Wilms' tumors (Frasier and Denys-Drash syndromes).
Recommendation
We recommend early gonadectomy in cases of gonadal dysgenesis. However, in cases of CAIS, gonadectomy is delayed until after puberty. (Strong recommendation, very low-quality evidence.)
5. Remarks
These recommendations place a high value on patient- and family-centered care and interdisciplinary communication. Despite the lack of controlled data for infrastructure support and care delivery, we provide strong recommendations, in part because there is clear data in general care delivery that inconsistent communication and coordination lead to poor outcomes.
6. Consensus Statement
In addition to the studies described herein and that form our evidence-based conclusions, we have taken into consideration the consensus statement on management of intersex disorders by the International Consensus Conference on Intersex [55]. It has been reviewed and the classifications of the DSD have been taken into account by our team.
Based on the evidence described in the papers described herein, the GMT task force consensus statement includes recommendations for (1) laboratory workup, (2) immediate acute management, (3) sex assignment in an ethical framework that includes education and involvement of the parents, and (4) surgical management. The GMT task Force makes the following recommendations for clinical practice.
-
(1)
Laboratory Workup
-
(i)
Standard workup for CAH: electrolytes, glucose, 17OHP, plasma renin, D4 androstenedione, testosterone, 11deoxycortisol, DHEA.
-
(ii)
Standard workup for hypopituitarism/hypogonadotropic hypogonadism: testosterone, LH, FSH, glucose, T4 (free thyroxine by equilibrium dialysis), TSH, testosterone, LH, FSH [14], and random cortisol versus 1 mcg ACTH.
-
(iii)
Workup for micropenis, undescended testes in the context of primary hypogonadism or in the context of first valuation of action or production of testosterone biochemical levels: testosterone baseline, stimulation with HCG as referenced by Davenport [17] (500 units q day
 3 days for younger than 1 year of age), and draw testosterone, dihydrotestosterone on day 4.
3 days for younger than 1 year of age), and draw testosterone, dihydrotestosterone on day 4. -
(iv)
Genetic testing as appropriate for ambiguous genitalia depending on karyotype and phenotype [15], which includes molecular genetics as needed for 5 alpha-reductase and androgen receptor defects.
-
(i)
-
(2)
Immediate Acute Management
-
(i)
For CAH and hypopituitarism, management is directed toward the emergency condition.
-
(ii)
For suspected CAH (salt-losing variety), an appropriate laboratory workup is done, and the infant is treated with D5 NS (dextrose in normal saline) and stress steroids (100 mg/m 2/day), with treatment modified after 24 hours, based on electrolyte correction; Florinef (0.1 mg po qd) is added, with a switch to table salt (2.5 grams po qd/given in 24-hr worth of formula).
-
(iii)
For micropenis and suspicion of hypopituitarism (the concern is hypoglycemia), the pituitary adrenal axis is assessed for cortisol production and treatment (stress steroids: 100 mg/m 2/day Solucortef) is initiated while laboratory results are pending. If neither of the acute conditions is the final diagnosis, treatment is withdrawn after the results of the workup are available.
-
(i)
-
(3)
Sex Assignment. The GMT task force recommends that physicians implement an educational component within an ethical framework that includes the parents in the decision-making process. That framework is based upon the following interactions: practice is based on the composite of factors listed below, which serves as an educational tool for the parents and provides a platform for generating the consensus among the stakeholders [28].
-
(i)
The Gender Medicine Team discusses implications of establishing the child's sex assignment with the help and participation of the ethicist, presents the results and workup to the parents, and establishes the long-term setting for follow-up.
-
(ii)
Education is provided to the parents for the sex assignment process before a decision is reached. The parents are active participants in the process and are presented different components of sex assignment as well the different alternatives (Table 1).
-
(iii)
The GMT task force recommends postponing sex assignment until (1) the entire GMT, including the ethicist, has fully assessed the child's condition and the situation, and (2) the parents have received adequate education and counseling, if necessary, to participate in making the decision concerning their child's sex assignment.
-
(i)
The evaluation that the GMT follows is one of standard practice, which begins with determination of whether the type of DSD the patient has is one condition or if there is multiple-organ involvement. Evaluation of the external genitalia is followed, as needed, by ultrasound evaluation of the internal genitalia. Clinical testing to establish chromosomal and molecular sex is performed, as are studies to determine the gonadal sex and endocrine studies. The patient also is supported by psychological counseling. The precise algorithm used is shown in Figure 1.Precedence for this type of approach is exemplified by the gender assessment team described in Parisi et al. [15].
7. Conclusions
The medical practice of sex assignment for individuals with DSD defies the conventional path of any established decision-making process and opens an opportunity for the medical field to define a consensus practice for the different subspecialties involved in a Gender Medicine Team. Based on our experience in this field, we suggest that both the parents and an ethicist who can ensure that the sex-assignment decision is within an ethical framework for treating persons with DSD be included as participants in the consensus [28, 33, 34].
Guidelines are essential in our practice and, despite the paucity of systematic outcomes and prospective studies in the field of gender medicine, the workup and medical management of the infant born with ambiguous genitalia is now the standard of care. However, once the diagnostic workup and any necessary acute interventions have been completed, the practices for making sex assignments vary from center to center.
Accordingly, the team that we assembled at Texas Children's Hospital decided to operate on a consensus basis, using the multidisciplinary team's expertise and incorporating the work of the pioneers in the field. One such example is Maria New, who advocated prenatal diagnosis and treatment of CAH babies in utero to avoid virilization of the external genitalia [98].
The virilization of genitalia that occurs in infants with CAH 21-OHlase deficiency can be corrected during intrauterine life, establishing that sex assignment does not rely by any means on the phenotype of the external genitalia. Other pioneers in the field include Mel Grumbach, Charles Sulton, Phyllis Speiser, and Perrin White, who established the management of ambiguous genitalia [11, 12, 14] by expanding our understanding of the biology of conditions of DSD and by demonstrating how early hormonal abnormalities can affect the fetus (aromatization) [99]. More recently, Roger Gorski, one of the original pioneers in studying the sexual dimorphism of the brain, demonstrated that not only the external genitalia but also the brain is a sexually dimorphic organ and a target of the hormones [100]. In addition, Sherry Berenbaum [92] evaluated girls with CAH and found some variability in their play behavior as a consequence of the hormonal influences.
Using the wisdom we inherited from the pioneers in gender medicine, we established and implemented guidelines that include the participation of the parents within an ethical framework provided by our ethicist. We suggest a simple algorithm for the workup, follow the uniform practices of most centers as standard of care, establish the diagnosis, and, unless a medical emergency exists, delay surgery until education of the parents is completed. We will continue to incorporate the long-standing evidence in the field and to establish methodology by evaluating and grading our practice in this field. We target our management for gender stability by providing support through our psychologist in the event of a sex change, should that be the choice of the individual; this matter can be addressed as part of the course. There are, of course, certain financial implications with our model, and only time and new directions in health care will prove whether ours is an efficient model.
References
Blizzard RM: Intersex issues: a series of continuing conundrums. Pediatrics. 2002, 110 (3): 616-621. 10.1542/peds.110.3.616.
Root AW, Growth MD: Commentary: intersex issues—a series of continuing conundrums. Growth, Genetics & Hormones. 2003, 19: 7-
Thyen U, Richter-Appelt H, Wiesemann C, Holterhus P-M, Hiort O: Deciding on gender in children with intersex conditions: considerations and controversies. Treatments in Endocrinology. 2005, 4 (1): 1-8. 10.2165/00024677-200504010-00001.
Pescovitz OH, Eugster EA: Disorders of sexual differentiation. Pediatric Endocrinology: Mechanisms, Manifestations and Management. Edited by: Pescovitz OH, Eugster EA. 2004, Lippincott Williams & Wilkins, Philadelphia, Pa, USA, 243-253.
Houk CP, Lee PA: Intersexed states: diagnosis and management. Endocrinology and Metabolism Clinics of North America. 2005, 34 (3): 791-810. 10.1016/j.ecl.2005.04.014.
Diamond M: Pediatric management of ambiguous and traumatized genitalia. Journal of Urology. 1999, 162 (3): 1021-1028. 10.1016/S0022-5347(01)68054-6.
Diamond DA, Burns JP, Mitchell C, Lamb K, Kartashov AI, Retik AB: Sex assignment for newborns with ambiguous genitalia and exposure to fetal testosterone: attitudes and practices of pediatric urologists. Journal of Pediatrics. 2006, 148 (4, part 2): 445-449. 10.1016/j.jpeds.2005.10.043.
Brett AS, McCullough LB: When patients request specific interventions: defining the limits of the physician's obligation. The New England Journal of Medicine. 1986, 315 (21): 1347-1351. 10.1056/NEJM198611203152109.
Atkins D, Best D, Briss PA: Grading quality of evidence and strength of recommendations. British Medical Journal. 2004, 328 (7454): 1490-1494.
Swiglo BA, Murad MH, Schünemann HJ, Kunz R, Vigersky RA, Guyatt GH, Montori VM: A case for clarity, consistency, and helpfulness: state-of-the-art clinical practice guidelines in endocrinology using the grading of recommendations, assessment, development, and evaluation system. Journal of Clinical Endocrinology and Metabolism. 2008, 93 (3): 666-673.
Sultan C, Paris F, Jeandel C, Lumbroso S, Galifer RB: Ambiguous genitalia in the newborn. Seminars in Reproductive Medicine. 2002, 20 (3): 181-188. 10.1055/s-2002-35382.
Speiser PW, White PC: Congenital adrenal hyperplasia. The New England Journal of Medicine. 2003, 349 (8): 776-788. 10.1056/NEJMra021561.
Joint LWPES/ESPE CAH Working Group : Consensus statement on 21-hydroxylase deficiency from the Lawson Wilkins Pediatric Endocrine Society and the European Society for Paediatric Endocrinology. Journal of Clinical Endocrinology and Metabolism. 2002, 87 (9): 4048-4053. 10.1210/jc.2002-020611.
Grumbach MM: A window of opportunity: the diagnosis of gonadotropin deficiency in the male infant. Journal of Clinical Endocrinology and Metabolism. 2005, 90 (5): 3122-3127. 10.1210/jc.2004-2465.
Parisi MA, Ramsdell LA, Burns MW, Carr MC, Grady RE, Gunther DF, Kletter GB, McCauley E, Mitchell ME, Opheim KE, Pihoker C, Richards GE, Soules MR, Pagon RA: A gender assessment team: experience with 250 patients over a period of 25 years. Genetics in Medicine. 2007, 9 (6): 348-357. 10.1097/GIM.0b013e3180653c47.
Kolon TF, Miller OF: Comparison of single versus multiple dose regimens for the human chorionic gonadotropin stimulatory test. Journal of Urology. 2001, 166 (4): 1451-1454. 10.1016/S0022-5347(05)65807-7.
Davenport M, Brain C, Vandenberg C, Zappala S, Duffy P, Ransley PG, Grant D: The use of the hCG stimulation test in the endocrine evaluation of cryptorchidism. British Journal of Urology. 1995, 76 (6): 790-794.
Misra M, MacLaughlin DT, Donahoe PK, Lee MM: Measurement of Mullerian inhibiting substance facilitates management of boys with microphallus and cryptorchidism. Journal of Clinical Endocrinology and Metabolism. 2002, 87 (8): 3598-3602. 10.1210/jc.87.8.3598.
Boehmer ALM, Brüggenwirth H, Van Assendelft C, Otten BJ, Verleun-Mooijman MCT, Niermeijer MF, Brunner HG, Rouwé CW, Waelkens JJ, Oostdijk W, Kleijer WJ, Van Der Kwast TH, De Vroede MA, Drop SLS: Genotype versus phenotype in families with androgen insensitivity syndrome. Journal of Clinical Endocrinology and Metabolism. 2001, 86 (9): 4151-4160. 10.1210/jc.86.9.4151.
Boehmer ALM, Brüggenwirth H, Van Assendelft C, Otten BJ, Verleun-Mooijman MCT, Niermeijer MF, Brunner HG, Rouwé CW, Waelkens JJ, Oostdijk W, Kleijer WJ, Van Der Kwast TH, De Vroede MA, Drop SLS: Erratum: genotype versus phenotype in families with androgen insensitivity syndrome (The Journal of Clinical Endocrinology & Metabolism 86 (4151–4160)). Journal of Clinical Endocrinology and Metabolism. 2002, 87 (7): 3109-
Imperato-McGinley J, Peterson RE, Leshin M: Steroid 5α-reductase deficiency in a 65-year-old male pseudohermaphrodite: the natural history, ultrastructure of the testes, and evidence for inherited enzyme heterogeneity. Journal of Clinical Endocrinology and Metabolism. 1980, 50 (1): 15-22. 10.1210/jcem-50-1-15.
Cai L-Q, Zhu Y-S, Katz MD, Herrera C, Baéz J, Defillo-Ricart M, Shackleton CHL, Imperato-McGinley J: 5α-reductase-2 gene mutations in the Dominican Republic. Journal of Clinical Endocrinology and Metabolism. 1996, 81 (5): 1730-1735. 10.1210/jc.81.5.1730.
Deeb A, Jääskeläinen J, Dattani M, Whitaker HC, Costigan C, Hughes IA: A novel mutation in the human androgen receptor suggests a regulatory role for the hinge region in amino-terminal and carboxy-terminal interactions. Journal of Clinical Endocrinology and Metabolism. 2008, 93 (10): 3691-3696. 10.1210/jc.2008-0737.
Codner E, Okuma C, Iñiguez G, Boric MA, Avila A, Johnson MC, Cassorla FG: Molecular study of the 3β-hydroxysteroid dehydrogenase gene type II in patients with hypospadias. Journal of Clinical Endocrinology and Metabolism. 2004, 89 (2): 957-964. 10.1210/jc.2002-020873.
Eckstein B, Cohen S, Farkas A, Rösler A: The nature of the defect in familial male pseudohermaphroditism in Arabs of Gaza. Journal of Clinical Endocrinology and Metabolism. 1989, 68 (2): 477-485. 10.1210/jcem-68-2-477.
Lu X-Y, Phung MT, Shaw CA, Pham K, Neil SE, Patel A, Sahoo T, Bacino CA, Stankiewicz P, Kang S-HL, Lalani S, Craig Chinault A, Lupski JR, Cheung SW, Beaudet AL: Genomic imbalances in neonates with birth defects: high detection rates by using chromosomal microarray analysis. Pediatrics. 2008, 122 (6): 1310-1318. 10.1542/peds.2008-0297.
Schaeffer TL, Tryggestad JB, Mallappa A: An evidence-based model of multidisciplinary care for patients and families affected by classical congenital adrenal hyperplasia due to 21-hydroxylase deficiency. International Journal of Pediatric Endocrinology. 2010, 2010: 13.
Axelrad ME, Berg JS, Coker LA, Dietrich J, Adcock L, French SL, Gunn S, Ligon BL, McCullough LB, Sutton VR, Karaviti LP: The gender medicine team: "It takes a village". Advances in Pediatrics. 2009, 56 (1): 145-164. 10.1016/j.yapd.2009.08.001.
Reiner WG, Gearhart JP: Discordant sexual identity in some genetic males with cloacal exstrophy assigned to female sex at birth. The New England Journal of Medicine. 2004, 350 (4): 333-341. 10.1056/NEJMoa022236.
Migeon CJ, Wisniewski AB: Human sex differentiation and its abnormalities. Best Practice and Research: Clinical Obstetrics and Gynaecology. 2008, 17 (1): 1-18.
Wisniewski AB, Migeon CJ, Meyer-Bahlburg HFL, Gearhart JP, Berkovitz GD, Brown TR, Money J: Complete androgen insensitivity syndrome: long-term medical, surgical, and psychosexual outcome. Journal of Clinical Endocrinology and Metabolism. 2000, 85 (8): 2664-2669. 10.1210/jc.85.8.2664.
Kass E, Kogan SJ, Manley C, Wacksman JA, Klykylo WM, Meza A, Schultz J, Wiener E: Timing of elective surgery on the genitalia of male children with particular reference to the risks, benefits, and psychological effects of surgery and anesthesia. Pediatrics. 1996, 97 (4): 590-594.
McCullough LB, Coverdale JH, Chervenak FA: Argument-based medical ethics: a formal tool for critically appraising the normative medical ethics literature. American Journal of Obstetrics and Gynecology. 2004, 191 (4): 1097-1102. 10.1016/j.ajog.2004.06.060.
McCullough LB: The ethical concept of medicine as a profession: its origins in modern medical ethics and implications for physicians. Lost Virtue: Professional Character Development in Medical Education. Edited by: Kenny N, Shelton W. 2006, Elsevier, New York, NY, USA, 17-27.
McCullough LB: A framework for the ethically justified clinical management of intersex conditions. Advances in Experimental Medicine and Biology. 2002, 511: 149-173. 10.1007/978-1-4615-0621-8_10.
Wiesemann C, Ude-Koeller S, Sinnecker GHG, Thyen U: Ethical principles and recommendations for the medical management of differences of sex development (DSD)/intersex in children and adolescents. European Journal of Pediatrics. 2010, 169 (6): 671-679. 10.1007/s00431-009-1086-x.
Frader J, Alderson P, Asch A, Aspinall C, Davis D, Dreger A, Edwards J, Feder EK, Frank A, Hedley LA, Kittay E, Marsh J, Miller PS, Mouradian W, Nelson H, Parens E: Health care professionals and intersex conditions. Archives of Pediatrics and Adolescent Medicine. 2004, 158 (5): 426-428. 10.1001/archpedi.158.5.426.
Stikkelbroeck NMML, Beerendonk CCM, Willemsen WNP, Schreuders-Bais CA, Feitz WFJ, Rieu PNMA, Hermus ARMM, Otten BJ: The long term outcome of feminizing genital surgery for congenital adrenal hyperplasia: anatomical, functional and cosmetic outcomes, psychosexual development, and satisfaction in adult female patients. Journal of Pediatric and Adolescent Gynecology. 2003, 16 (5): 289-296. 10.1016/S1083-3188(03)00155-4.
Nordenskjöld A, Holmdahl G, Frisén L, Falhammar H, Filipsson H, Thorén M, Janson PO, Hagenfeldt K: Type of mutation and surgical procedure affect long-term quality of life for women with congenital adrenal hyperplasia. Journal of Clinical Endocrinology and Metabolism. 2008, 93 (2): 380-386. 10.1210/jc.2007-0556.
Schnitzer JJ, Donahoe PK: Surgical treatment of congenital adrenal hyperplasia. Endocrinology and Metabolism Clinics of North America. 2001, 30 (1): 137-154. 10.1016/S0889-8529(08)70023-9.
Chertin B, Koulikov D, Hadas-Halpern I, Farkas A: Masculinizing genitoplasty in intersex patients. Journal of Urology. 2005, 174 (4, part 2): 1683-1686. 10.1097/01.ju.0000176624.11667.5d.
Göllü G, Yildiz RV, Bingol-Kologlu M, Yagmurlu A, Fedakar Senyücel M, Aktug T, Gökcora IH, Dindar H: Ambiguous genitalia: an overview of 17 years' experience. Journal of Pediatric Surgery. 2007, 42 (5): 840-844. 10.1016/j.jpedsurg.2006.12.036.
Lam PN, Greenfield SP, Williot P, Zaontz MR, Snodgrass W: 2-stage repair in infancy for severe hypospadias with chordee: long-term results after puberty. Journal of Urology. 2005, 174 (4, part 2): 1567-1572. 10.1097/01.ju.0000179395.99944.48.
Nihoul-Fékété C, Thibaud E, Lortat-Jacob S, Josso N: Long-term surgical results and patient satisfaction with male pseudohermaphroditism or true hermaphroditism: a cohort of 63 patients. Journal of Urology. 2006, 175 (5): 1878-1884. 10.1016/S0022-5347(05)00934-1.
Farkas A, Rosler A: Ten years experience with masculinizing genitoplasty in male pseudohermaphroditism due to 17β-hydroxysteroid dehydrogenase deficiency. European Journal of Pediatrics. 1993, 152 (2): S88-S90. 10.1007/BF02125448.
Mendonca BB, Inacio M, Costa EMF, Arnhold IJP, Russell DW, Wilson JD: Male pseudohermaphroditism due to 5α-reductase 2 deficiency: outcome of a Brazilian cohort. Endocrinologist. 2003, 13 (3): 201-204. 10.1097/01.ten.0000081675.43801.42.
Lima M, Aquino A, Dòmini M, Ruggeri G, Libri M, Cimador M, Pelusi G: Laparoscopic removal of Müllerian duct remnants in boys. Journal of Urology. 2004, 171 (1): 364-368. 10.1097/01.ju.0000102321.54818.53.
Olsen MM, Caldamone AA, Jackson CL, Zinn A: Gonadoblastoma in infancy: indications for early gonadectomy in 46XY gonadal dysgenesis. Journal of Pediatric Surgery. 1988, 23 (3): 270-271. 10.1016/S0022-3468(88)80738-3.
Dumic M, Jukic S, Batinica S, Ille J, Filipović-Grcić B: Bilateral gonadoblastoma in a 9-month-old infant with 46,XY gonadal dysgenesis. Journal of Endocrinological Investigation. 1993, 16 (4): 291-293.
Fallat ME, Donahoe PK: Intersex genetic anomalies with malignant potential. Current Opinion in Pediatrics. 2006, 18 (3): 305-311. 10.1097/01.mop.0000193316.60580.d7.
Funder JW, Carey RM, Fardella C, Gomez-Sanchez CE, Mantero F, Stowasser M, Young WF, Montori VM, Edwards H: Case detection, diagnosis, and treatment of patients with primary aldosteronism: an endocrine society clinical practice guideline. Journal of Clinical Endocrinology and Metabolism. 2008, 93 (9): 3266-3281. 10.1210/jc.2008-0104.
The McGill Androgen Receptor Gene Mutations Database World Wide Web Server :http://androgendb.mcgill.ca/,
Rey R, Mebarki F, Forest MG, Mowszowicz I, Cate RL, Morel Y, Chaussain J-L, Josso N: Anti-müllerian hormone in children with androgen insensitivity. Journal of Clinical Endocrinology and Metabolism. 1994, 79 (4): 960-964. 10.1210/jc.79.4.960.
Tekgul S, Reidmiller H, Geharz E: Disorders of sex development. Guidelines on Pediatric Urology. 2008, European Association of Urology, European Society for Paediatric Urology, Arnhem, The Netherlands, 62-67. chapter 17
Lee PA, Houk CP, Ahmed SF, Hughes IA, Achermann J, Ahmed F, Baskin L, Berenbaum S, Bertelloni S, Brock J, Carmichael P, Chase C, Cohen-Kettenis P, Conte F, Copeland K, Donohoue P, Driver C, Drop S, Eugster E, Fujieda K, Giedd J, Green R, Grumbach M, Harley V, Hines M, Hiort O, Houk C, Hughes I, Lee P, Looijenga L, Mendoca B, Meyer-Bahlburg H, Migeon C, Morel Y, Mouriquand P, Nordenström A, Ransley P, Rapaport R, Reiner W, Richter-Appelt H, Rink R, Rissman E, Saenger P, Sandberg D, Schober J, Spack N, Thomas B, Thyen U, Vilain E, Warne G, Wilson J, Wisniewski A, Woodhouse C, Zucker K: Consensus statement on management of intersex disorders. Pediatrics. 2006, 118 (2): e488-e500. 10.1542/peds.2006-0738.
Allen L: Disorders of sexual development. Obstetrics and Gynecology Clinics of North America. 2009, 36 (1): 25-45. 10.1016/j.ogc.2009.02.001.
Savanelli A, Alicchio F, Esposito C, De Marco M, Settimi A: A modified approach for feminizing genitoplasty. World Journal of Urology. 2008, 26 (5): 517-520. 10.1007/s00345-008-0298-4.
Göllü G, Yildiz RV, Bingol-Kologlu M, Yagmurlu A, Fedakar Senyücel M, Aktug T, Gökcora IH, Dindar H: Ambiguous genitalia: an overview of 17 years' experience. Journal of Pediatric Surgery. 2007, 42 (5): 840-844. 10.1016/j.jpedsurg.2006.12.036.
Eroǧlu E, Tekant G, Gündoǧdu G, Emir H, Ercan O, Söylet Y, Danismend N: Feminizing surgical management of intersex patients. Pediatric Surgery International. 2004, 20 (7): 543-547. 10.1007/s00383-004-1208-5.
Graziano K, Teitelbaum DH, Hirschl RB, Coran AG: Vaginal reconstruction for ambiguous genitalia and congenital absence of the vagina: a 27-year experience. Journal of Pediatric Surgery. 2002, 37 (7): 955-960. 10.1053/jpsu.2002.33815.
Al-Bassam A, Gado A: Feminizing genital reconstruction: experience with 52 cases of ambiguous genitalia. European Journal of Pediatric Surgery. 2004, 14 (3): 172-178. 10.1055/s-2004-815869.
Gosalbez R, Castellan M, Ibrahim E, DiSandro M, Labbie A: New concepts in feminizing genitoplasty—is the fortunoff flap obsolete?. Journal of Urology. 2005, 174 (6): 2350-2353. 10.1097/01.ju.0000180419.62193.78.
Robson S, Oliver GD: Management of vaginal agenesis: review of 10 years practice at a tertiary referral centre. Australian and New Zealand Journal of Obstetrics and Gynaecology. 2000, 40 (4): 430-433. 10.1111/j.1479-828X.2000.tb01175.x.
Parsons JK, Gearhart SL, Gearhart JP: Vaginal reconstruction utilizing sigmoid colon: complications and long-term results. Journal of Pediatric Surgery. 2002, 37 (4): 629-633. 10.1053/jpsu.2002.31623.
Burgu B, Duffy PG, Cuckow P, Ransley P, Wilcox DT: Long-term outcome of vaginal reconstruction: comparing techniques and timing. Journal of Pediatric Urology. 2007, 3 (4): 316-320. 10.1016/j.jpurol.2006.09.008.
Fedele L, Frontino G, Motta F, Restelli E, Candiani M: Creation of neovagina in Rokitansky patients with a pelvic kidney: comparison of long-term results of the modified Vecchiettu and McIndoe techniques. Fertility and Sterility. 2010, 93 (4): 1280-1285. 10.1016/j.fertnstert.2008.12.020.
Creatsas G, Deligeoroglou E: Vaginal aplasia and reconstruction. Best Practice and Research: Clinical Obstetrics and Gynaecology. 2010, 24 (2): 185-191. 10.1016/j.bpobgyn.2009.11.002.
Rajimwale A, Furness PD, Brant WO, Koyle MA: Vaginal construction using sigmoid colon in children and young adults. BJU International. 2004, 94 (1): 115-119. 10.1111/j.1464-4096.2004.04911.x.
Bocciardi A, Lesma A, Montorsi F, Rigatti P: Passerini-Glazel feminizing genitoplasty: a long-term followup study. Journal of Urology. 2005, 174 (1): 284-288. 10.1097/01.ju.0000161211.40944.87.
Lesma A, Bocciardi A, Montorsi F, Rigatti P: Passirini-Glazel Feminizing genitoplasty: modifications in 17 years of experience with 82 cases. European Urology. 2007, 52 (6): 1638-1644. 10.1016/j.eururo.2007.02.068.
Braga LHP, Lorenzo AJ, Tatsuo ES, Silva IN, Pippi Salle JL: Prospective evaluation of feminizing genitoplasty using partial urogenital sinus mobilization for congenital adrenal hyperplasia. Journal of Urology. 2006, 176 (5): 2199-2204. 10.1016/j.juro.2006.07.063.
Sircili MHP, De Mendonca BB, Denes FT, Madureira G, Bachega TASS, De Queiroz E Silva FA: Anatomical and functional outcomes of feminizing genitoplasty for ambiguous genitalia in patients with virilizing congenital adrenal hyperplasia. Clinics. 2006, 61 (3): 209-214.
Lean WL, Deshpande A, Hutson J, Grover SR: Cosmetic and anatomic outcomes after feminizing surgery for ambiguous genitalia. Journal of Pediatric Surgery. 2005, 40 (12): 1856-1860. 10.1016/j.jpedsurg.2005.08.045.
Miranda ML, De Oliveira-Filho AG, Lemos-Marini SHV, Guerra G, Bustorff-Silva JM: Labioscrotal island flap in feminizing genitoplasty. Journal of Pediatric Surgery. 2004, 39 (7): 1030-1033. 10.1016/j.jpedsurg.2004.03.060.
Alizai NK, Thomas DFM, Lilford RJ, Batchelor AGG, Johnson N: Feminizing genitoplasty for congenital adrenal hyperplasia: what happens at puberty?. Journal of Urology. 1999, 161 (5): 1588-1591. 10.1016/S0022-5347(05)68986-0.
Krege S, Walz KH, Hauffa BP, Körner I, Rübben H: Long-term follow-up of female patients with congenital adrenal hyperplasia from 21-hydroxylase deficiency, with special emphasis on the results of vaginoplasty. BJU International. 2000, 86 (3): 253-259. 10.1046/j.1464-410x.2000.00789.x.
Krstic Z, Perovic S, Radmanovic S, Neclic S, Smoljanic Z, Jevtic P: Surgical treatment of intersex disorders. Journal of Pediatric Surgery. 1995, 30 (9): 1273-1281. 10.1016/0022-3468(95)90484-0.
Louis-Sylvestre C, Haddad B, Paniel B-J: Creation of a sigmoid neovagina: technique and results in 16 cases. European Journal of Obstetrics Gynecology and Reproductive Biology. 1997, 75 (2): 225-229. 10.1016/S0301-2115(97)00137-1.
Creatsas G, Deligeoroglou E, Makrakis E, Kontoravdis A, Papadimitriou L: Creation of a neovagina following Williams vaginoplasty and the Creatsas modification in 111 patients with Mayer-Rokitansky-Küster-Hauser syndrome. Fertility and Sterility. 2001, 76 (5): 1036-1040. 10.1016/S0015-0282(01)02836-9.
Roberts CP, Haber MJ, Rock JA: Vaginal creation for müllerian agenesis. American Journal of Obstetrics and Gynecology. 2001, 185 (6): 1349-1353. 10.1067/mob.2001.119075.
Brun J-L, Belleannée G, Grafeille N, Aslan A-F, Brun GH: Long-term results after neovagina creation in Mayer-Rokitanski-Kuster-Hauser syndrome by Vecchietti's operation. European Journal of Obstetrics Gynecology and Reproductive Biology. 2002, 103 (2): 168-172. 10.1016/S0301-2115(02)00031-3.
Cai B, Zhang JR, Xi XW, Yan Q, Wan XP: Laparoscopically assisted sigmoid colon vaginoplasty in women with Mayer-Rokitansky-Kuster-Hauser syndrome: feasibility and short-term results. BJOG. 2007, 114 (12): 1486-1492. 10.1111/j.1471-0528.2007.01514.x.
Creatsas G, Deligeoroglou E, Christopoulos P: Creation of a neovagina after Creatsas modification of Williams vaginoplasty for the treatment of 200 patients with Mayer-Rokitansky-Kuster-Hauser syndrome. Fertility and Sterility. 2010, 94 (5): 1848-52. 10.1016/j.fertnstert.2009.09.064.
Brucker SY, Gegusch M, Zubke W, Rall K, Gauwerky JF, Wallwiener D: Neovagina creation in vaginal agenesis: development of a new laparoscopic Vecchietti-based procedure and optimized instruments in a prospective comparative interventional study in 101 patients. Fertility and Sterility. 2008, 90 (5): 1940-1952. 10.1016/j.fertnstert.2007.08.070.
Chia WY: Tissue-preserving feminizing clitoroplasty: a preliminary report. Journal of Pediatric Urology. 2007, 3 (6): 457-460. 10.1016/j.jpurol.2007.04.010.
Pippi Salle JL, Braga LP, Macedo N, Rosito N, Bagli D: Corporeal sparing dismembered clitoroplasty: an alternative technique for feminizing genitoplasty. Journal of Urology. 2007, 178 (4): 1796-1801. 10.1016/j.juro.2007.03.167.
De Jong TPVM, Boemers TML: Neonatal management of female intersex by clitorovaginoplasty. Journal of Urology. 1995, 154 (2): 830-832. 10.1016/S0022-5347(01)67176-3.
Jenak R, Ludwikowski B, González R: Total urogenital sinus mobilization: a modified perineal approach for feminizing genitoplasty and urogenital sinus repair. Journal of Urology. 2001, 165 (6): 2347-2349. 10.1016/S0022-5347(05)66200-3.
Schätz T, Huber J, Wenzl R: Creation of a neovagina according to Wharton-Sheares-George in patients with Mayer-Rokitansky-Küster-Hauser syndrome. Fertility and Sterility. 2005, 83 (2): 437-441. 10.1016/j.fertnstert.2004.06.079.
Ismail IS, Cutner AS, Creighton SM: Laparoscopic vaginoplasty: alternative techniques in vaginal reconstruction. BJOG. 2006, 113 (3): 340-343. 10.1111/j.1471-0528.2005.00845.x.
Fotopoulou C, Sehouli J, Gehrmann N, Schoenborn I, Lichtenegger W: Functional and anatomic results of amnion vaginoplasty in young women with Mayer-Rokitansky-Küster-Hauser syndrome. Fertility and Sterility. 2010, 94 (1): 317-323. 10.1016/j.fertnstert.2009.01.154.
Berenbaum SA, Bailey JM: Effects on gender identity of prenatal androgens and genital appearance: evidence from girls with congenital adrenal hyperplasia. Journal of Clinical Endocrinology and Metabolism. 2003, 88 (3): 1102-1106. 10.1210/jc.2002-020782.
Wisniewski AB, Migeon CJ, Meyer-Bahlburg HFL, Gearhart JP, Berkovitz GD, Brown TR, Money J: Complete androgen insensitivity syndrome: long-term medical, surgical, and psychosexual outcome. Journal of Clinical Endocrinology and Metabolism. 2000, 85 (8): 2664-2669. 10.1210/jc.85.8.2664.
Köhler B, Lumbroso S, Leger J, Audran F, Grau ES, Kurtz F, Pinto G, Salerno M, Semitcheva T, Czernichow P, Sultan C: Androgen insensitivity syndrome: somatic mosaicism of the androgen receptor in seven families and consequences for sex assignment and genetic counseling. Journal of Clinical Endocrinology and Metabolism. 2005, 90 (1): 106-111.
Sarafoglou K, Ostrer H: Clinical review 111: familial sex reversal—a review. Journal of Clinical Endocrinology and Metabolism. 2000, 85 (2): 483-493. 10.1210/jc.85.2.483.
Boisen KA, Chellakooty M, Schmidt IM, Kai CM, Damgaard IN, Suomi A-M, Toppari J, Skakkebaek NE, Main KM: Hypospadias in a cohort of 1072 Danish newborn boys: prevalence and relationship to placental weight, anthropometrical measurements at birth, and reproductive hormone levels at three months of age. Journal of Clinical Endocrinology and Metabolism. 2005, 90 (7): 4041-4046. 10.1210/jc.2005-0302.
Hadjiathanasiou CG, Brauner R, Lortat-Jacob S, Nivot S, Jaubert F, Fellous M, Nihoul-Fekete C, Rappaport R: True hermaphroditism: genetic variants and clinical management. Journal of Pediatrics. 1994, 125 (5, part 1): 738-744. 10.1016/S0022-3476(06)80172-1.
New MI, Carlson A, Obeid J, Marshall I, Cabrera MS, Goseco A, Lin-Su K, Putnam AS, Wei JQ, Wilson RC: Extensive personal experience: prenatal diagnosis for congenital adrenal hyperplasia in 532 pregnancies. Journal of Clinical Endocrinology and Metabolism. 2001, 86 (12): 5651-5657. 10.1210/jc.86.12.5651.
Conte FA, Grumbach MM, Ito Y, Fisher CR, Simpson ER: A syndrome of female pseudohermaphrodism, hypergonadotropic hypogonadism, and multicystic ovaries associated with missense mutations in the gene encoding aromatase (P450arom). Journal of Clinical Endocrinology and Metabolism. 1994, 78 (6): 1287-1292. 10.1210/jc.78.6.1287.
Gorski RA: Hypothalamic imprinting by gonadal steroid hormones. Advances in Experimental Medicine and Biology. 2002, 511: 57-73. 10.1007/978-1-4615-0621-8_5.
Acknowledgments
The authors are very grateful to Dr. B. Lee Ligon of the Department of Pediatrics, Baylor College of Medicine for her editorial contributions. They also acknowledge Dr. David R. Roth from The Division of Pediatric Urology at Texas Children's Hospital for his support of the Gender Medicine Team consensus.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Douglas, G., Axelrad, M.E., Brandt, M.L. et al. Consensus in Guidelines for Evaluation of DSD by the Texas Children's Hospital Multidisciplinary Gender Medicine Team. Int J Pediatr Endocrinol 2010, 919707 (2010). https://doi.org/10.1155/2010/919707
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1155/2010/919707




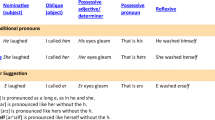
 What is the most appropriate evaluation for peripheral defects leading to micropenis, hypospadias with respect to[
What is the most appropriate evaluation for peripheral defects leading to micropenis, hypospadias with respect to[ 3 days for younger than 1 year of age), and draw testosterone, dihydrotestosterone on day 4.
3 days for younger than 1 year of age), and draw testosterone, dihydrotestosterone on day 4.