Abstract
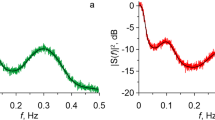
This article shows that significant numerical differences in the estimates of respiratory sinus arrhythmia (RSA) parameters by the spectral method and the RMSSD index (standard deviation of the number of first differences between adjacent normal RR intervals) are a consequence of the semantic difference between these estimates: while the spectral method estimates the power and standard deviation of fluctuations in heart rate variability (HRV) in the high-frequency range, RMSSD measures the standard deviation of the HRV rate of change over the full range of HRV frequencies. An analysis of the errors of the spectral method caused by the mismatch between the high-frequency range and the respiration range is presented. Simultaneous recordings of electrocardiography and respiration of 18 young and 17 elderly subjects were used for calculations. It is shown that the errors of the spectral method are 16 ± 9% for the group of young subjects and 29 ± 10% for the group of older subjects. The RMSSD estimates exceed the estimates of the spectral method by an average of 1.4 times. Mathematical analysis of the respiratory rate dependence of the RMSSD index showed that for two records of RR intervals with coinciding spectral estimates of the RSA amplitude, the RMSSD indices can differ by more than 1.5 times depending on the respiratory rate. A method for estimating the rate of change in RR intervals in the respiratory range based on cross-correlation analysis is proposed. The error of the method depends on the number of RR intervals in the record and does not exceed 4% at a heart rate of 60 bpm for a 10-min recording and 6% for a 5-min recording. The method requires simultaneous recordings of ECG and respiration but does not require the construction of spectral densities.



Similar content being viewed by others
REFERENCES
Guidelines: heart rate variability. Standards of measurement, physiological interpretation, and clinical use, Eur. Heart J., 1996, vol. 17, p. 354.
Baevskii, R.M. and Ivanov, G.G., Heart rate variability: theoretical aspects and potential clinical applications, Ul’trazvuk. Funkts. Diagn., 2001, no. 3, p. 108.
Shaffer, F., McCraty, R., and Zerr, C.L., A healthy heart is not a metronome: an integrative review of the heart’s anatomy and heart rate variability, Front. Psychol., 2014, vol. 5, p. 1040.
Shaffer, F. and Ginsberg, J.P., An overview of heart rate variability metrics and norms, Front. Public Health, 2017, vol. 5, p. 258.
Vanderlei, L.C., Pastre, C.M., Hoshi, R.A., et al., Basic notions of heart rate variability and its clinical applicability, Rev. Bras. Cir. Cardiovasc., 2009, vol. 24, no. 2, p. 205.
Elstad, M., O’Callaghan, E.L., Smith, A.J., et al., Cardiorespiratory interactions in humans and animals: rhythms for life, Am. J. Physiol.: Heart Circ. Physiol., 2018, vol. 315, no. 1, p. H6.
Serafi, A.S., Heart rate variability (HRV)—analysis and clinical significance, Int. J. Biol. Biotech., 2018, vol. 15, no. 2, p. 193.
Olexova, L.B., Sekaninova, N., Jurko, A., Jr., et al., Respiratory sinus arrhythmia as an index of cardiac vagal control in mitral valve prolapse, Physiol. Res., 2020, vol. 69, suppl. 1, p. S163.
Grossman, P. and Taylor, E.W., Toward understanding respiratory sinus arrhythmia: relations to cardiac vagal tone, evolution and biobehavioral functions, Biol. Psychol., 2007, vol. 74, no. 2, p. 263.
Simoyi, M.F., Respiratory sinus arrhythmia in athletes, the young, and the old, Biomed. J. Sci. Tech. Res., 2020, vol. 30, no. 3, p. 23359.
Heathers, J.A.J., Everything hertz: methodological issues in short-term frequency-domain HRV, Front. Physiol., 2014, vol. 5, p. 177.
Pinna, G.D., Maestri, R., Torunski, A., et al., Heart rate variability measures: a fresh look at reliability, Clin. Sci., 2007, vol. 113, no. 3, p. 131.
Draghici, A.E. and Taylor, J.A., The physiological basis and measurement of heart rate variability in humans, J. Physiol. Anthropol., 2016, vol. 35, no. 1, p. 22.
Hayano, J. and Yuda, E., Pitfalls of assessment of autonomic function by heart rate variability, J. Physiol. Anthropol., 2019, vol. 38, no. 1, p. 3.
Stein, P.K., Le, Q.C., and Domitrovich, P.P., Development of more erratic heart rate patterns is associated with mortality post-myocardial infarction, J. Electrocardiol., 2008, vol. 41, no. 2, p. 110.
Bernardi, L., Rossi, M., Soffiantino, F., et al., Cross correlation of heart rate and respiration versus deep breathing, Diabetes, 1989, vol. 38, no. 5, p. 589.
Bakhilin, V.M., Cross-correlation and cross-spectral analysis of the relationship between fluctuations in heart rate and respiration, Vestn. Ross. Voenno-Med. Akad., 2012, no. 1(37), p. 193.
Terebizh, V.Yu., Vvedenie v statisticheskuyu teoriyu obratnykh zadach (Introduction into the Statistical Theory of Inverse Problems), Moscow: FIZMATLIT, 2005.
Goldberger, A.L., Amaral, L.A., Glass, L., et al., PhysioBank, PhysioToolkit, and PhysioNet: components of a New Research Resource for Complex Physiologic Signals, Circulation, 2000, vol. 101, no. 23, p. E215.
Funding
The study was performed within the project of scientific research topics included in the scientific work plans of scientific organizations and higher educational institutions implementing research programs supported by the federal budget in accordance with Appendix no. 2 to the order of the Ministry of Science and Higher Education of the Russian Federation no. 15n of March 21, 2019.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the biomedical ethics principles formulated in the 1964 Helsinki Declaration and its later amendments and approved by the local bioethical committee of the St. Petersburg Research Institute of Ear, Throat, Nose and Speech (St. Petersburg).
Conflict of interests. The authors declare that they do not have a conflict of interest.
Informed consent. Each study participant provided a voluntary written informed consent signed by him after explaining to him the potential risks and benefits, as well as the nature of the upcoming study.
Additional information
Translated by E. Babchenko
Rights and permissions
About this article
Cite this article
Bakhilin, V.M. Estimates of the Parameters of Respiratory Sinus Arrhythmia. Hum Physiol 48, 440–448 (2022). https://doi.org/10.1134/S0362119722040028
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S0362119722040028