Abstract
Gender and socioeconomic differences in subjective life expectancy (SLE) are an unexplored arena in the geriatric literature concerning low-resource settings. Information on several health outcomes that might influence the SLE could guide targeted interventions, particularly in countries with rapidly ageing populations like India. This study aimed to explore SLE and the associations of SLE with the objective and subjective health status of older Indian adults, based on the mindsponge mechanism that links the contextual factors with individuals' evaluation of health. Data from the Longitudinal Ageing Study in India were used and the final sample included 5969 older adults aged 60 years and above. Independent t-tests were used to assess the gender difference in SLE according to various health-related factors. Additionally, we used generalized linear regression models (GLMs) with a logit link and a binomial family to fulfil the study objectives. The proportion of older adults who reported a 100% probability of survival for a 1-year period was nearly 38%, compared with 12% and 6% of the respondents who reported the same for 5 and 10 years survival periods, respectively. Older men reported a greater average probability of own survival than older women for all the time periods. Older men who reported poor self-rated health had a significantly lower SLE for a 1-year period (β = −0.232, SD = 0.107) and a 5-year period (β = −0.226, SD = 0.077) than those who reported good self-rated health. On the other hand, older women with poor self-rated health had a significantly lower SLE for a 10 years time horizon than women with good self-rated health. Underweight men had significantly lower SLE for a 1-year period than men with normal BMI (β = −0.213, SD = 0.097). Further, cognitively impaired women reported significantly lower SLE for a 1-year period (β = −0.399, SD = 0.108) and 5 years period (β = −0.160, SD = 0.077). Depressed older men reported significantly lower SLE for 1-year period (β = −0.309, SD = 0.101), 5-year period (β = −0.194, SD = 0.084), and 10-year period (β = −0.129, SD = 0.071). The current findings, supporting the mindsponge mechanism, indicate that older adults base their estimation of longevity on health factors that they are aware of or not. This finding has significant implications for health professionals and public policy in planning targeted interventions that can benefit at-risk population cohorts.
Similar content being viewed by others
Introduction
Life expectancy (LE) has increased significantly over the past 100 years globally (Lima et al., 2016). Better living standards and health services have contributed most to the substantial increases in life expectancy (Lima et al., 2016). In less than a quarter of a decade, the global life expectancy at birth (LEB) increased from 64 to 71 years between 1990 and 2013 and is still increasing significantly (Lima et al., 2016; World Health Organization, 2015). Moreover, the proportion of the world’s population aged 60 and up will nearly double from 12% to 22% between 2015 and 2050 (Srivastava and Gill, 2020).
In India, the LEB increased from 54 to 67 years in the period of 1981–2011 (Singh et al., 2017). This demographic transition accompanied by declining fertility and mortality will further increase the LEB and will also lead to an increased ageing population in the country (Srivastava and Gill, 2020). Currently, older adults account for about 8% of India’s total population, but this figure is anticipated to climb to 19% by 1950 (Srivastava and Gill, 2020). According to the Census of India, the proportion of older adults in the overall population rose from 5.6% in 1961 to 8.6% in 2011 and is expected to rise to 20% in 2050.
This significant increase in life expectancy also impacts the decision-making related to later life among older adults (Delavande et al., 2017). The decisions on investments, retirement, savings, health care, and migration are paramount (Delavande et al., 2017). People have expectations about their survival, i.e., remaining years of life, and increased expectations lead to positive decisions related to their life that result in active and healthy ageing and contribute to the household/community economy and overall wellbeing of the population (Delavande et al., 2017; Siegel et al., 2003). Previous literature suggests that subjective life expectancy (SLE) can predict mortality (Kim and Kim, 2017; Siegel et al., 2003; Smith et al., 2001). Researchers have attempted to explore how individuals assess their survival expectancy and some studies have pointed out possible associations between subjective health status (Balia, 2014; Jylhä, 2009) and individuals’ perspectives of objective health outcomes, such as obesity and chronic conditions (Falba and Busch, 2005; Zick et al., 2014). Mental health conditions, too, are reported to have an impact on perceived life expectancy among older adults. Clinical depression, subclinical distress, and anxiety have been reported as significant risk factors for declined physical functioning and mortality (Gruenewald and Kemeny, 2007). Further, Griffin et al. (2013) proposed a biopsychosocial model to predict SLE. In his model, Griffin et al. (2013) proposed four categories of predictors, i.e., (1) biomedical and genetic factors; (2) socioeconomic factors; (3) health behaviours; and (4) psychosocial factors.
A significant gender differential exists in reporting of SLE, i.e., it was revealed that women underestimate their survival chances more than men (Palloni and Novak, 2016; Philipov and Scherbov, 2020). However, some studies revealed that older men had higher chances to report low perceived life expectancy (Kobayashi et al., 2017). Age also plays a significant role in determining the perceived life expectancy among older adults (Kobayashi et al., 2017). Younger older adults are expected to have higher SLE; however, age-restricted studies argued that having survived for more years allows the older person to overestimate SLE (Australian Institute of Health and Welfare, 2003). It has been argued that people with low socioeconomic status had lower SLE because these people have more health problems and disabilities or they sense they would develop these problems in the future (Mirowsky and Ross, 2000; Ross and Mirowsky, 2002, 2008). Literature suggests that healthy life behaviour increases life expectancy, i.e., maintaining appropriate body mass index, abstaining from the consumption of alcohol and tobacco, and eating healthy food (Sarafino, 2004). Being a smoker, consuming alcohol, and suffering from non-communicable diseases were associated with low SLE (Kobayashi et al., 2017). SLE also differs by ethnicity of an individual (Irby-Shasanmi, 2013). Lack of knowledge on disparities in SLE is also considered to be one of the reasons for over or underestimation of LE (Lillie-Blanton et al., 2000).
There is a dearth of literature focusing on the relationship between health status with SLE among older adults in low and middle-income countries. Moreover, gender and socioeconomic differences in SLE are also an unexplored arena in geriatric literature in low-resource settings like India. Mindsponge theory, a construct that proposes how individuals respond to information, suggests that factors, such as socio-cultural settings, available healthcare services, health-related information and awareness positively impact the individual’s evaluation of own health (Nguyen et al., 2022). When an individual is exposed to new and external information such as subjective and objective information on one’s health, the individual applies an information filtering process to gauge the new information inputs for benefits and alignment to their core values, and when perceived as beneficial, they incorporate the information into their mindset, determining their self-perceived longevity. A dynamic and contextual conceptualization of SLE as a result of positive health evaluation would provide evidence for identifying and prioritizing policies for vulnerable older populations. In addition, at the population level, information on several health outcomes that might influence the SLE could guide targeted interventions, particularly in countries with rapidly ageing populations like India.
The present study aimed to assess SLE in association with the objective and subjective health status of older adults. Given the aforementioned literature, we developed a framework incorporating the mindsponge mechanism (Q. H. Vuong and Napier, 2015), which is summarized in Fig. 1. Premised on existing literature that highlights the impact of the individual's perception of their ageing process on their health and survival in later life (Westerhof et al., 2014), this study hypothesized that adverse objective and subjective health outcomes are associated with lower levels of SLE among older adults.
Methods
Data
We used data from the first wave of the Longitudinal Study of Ageing in India (LASI) conducted between April 2017 and November 2018. LASI is a nationally representative population-based longitudinal survey of more than 72,000 individuals aged 45 years or older across all states and union territories of India (excluding Sikkim). It provided a range of social, health, retirement, and economic well-being for older adults in India. Moreover, in the expectation module of the LASI survey, respondents were asked about their chances of survival in different time horizons. LASI data is harmonized with Health and Retirement Study (HRS) in the United States and is comparable to several other surveys such as China Health and Retirement Longitudinal Study (CHARLS). In LASI, a multistage stratified cluster sample design was used for the sample selection, including a three-stage sampling design in rural areas and a four-stage sampling design in urban areas. In the data collection process, face-to-face interviews were conducted at the respondent’s household with the help of a computer-assisted personal interview (CAPI). The LASI survey was conducted through a partnership between the International Institute for Population Sciences (IIPS), Harvard T. H. Chan School of Public Health (HSPH), and the University of Southern California (USC). All the participants were provided with information brochures explaining the purpose of the survey, ways of protecting their privacy, and the safety of the health assessments.
Final sample
The LASI survey administered an expectations module to a randomly selected 33% of the total number of respondents (Delavande et al., 2017). Out of all respondents aged 60 years and over (n = 31,464), nearly 24.1% (n = 7583) were randomly selected for the survival expectation module. Out of selected 7583 older adults, 206 (0.03%) refused to participate in the expectation module. Moreover, we excluded 1408 (18.6%) older adults due to missing values in independent variables. Our final sample size included 5969 older adults aged 60 years and above.
Outcome variable
‘Subjective life expectancy’ (SLE) is the outcome variable in the present study. The ‘survival’ section in the expectations module contains the questions that assessed the respondents’ subjective probability of survival for different time horizons (i.e., 1, 5, and 10 years). The expectations module uses an interactive elicitation technique in which the respondents were asked to allocate up to 10 beans on the plate to determine the likelihood that certain events will happen. Before moving to the survival section, a proper explanation of the probability concepts was given to the respondents, along with the following introduction:
I will ask you several questions about the chance or likelihood that certain events are going to happen. There are 10 beans in the cup. I would like you to choose some beans out of these 10 beans and put them in the plate to help me understand what you think the likelihood or chance is of a specific event happening. If you do not put any beans in the plate, it means you are sure that the event will NOT happen. If you add beans, this means that you think the likelihood that the event happens will increase. If you put 10 beans in the plate, it means you are sure the event will happen. One bean represents one chance out of 10. For example, if you put one or two beans, it means you think the event is not likely to happen but it is still possible. If you pick 5 beans, it means that it is just as likely it happens as it does not happen (50-50). If you pick 6 beans, it means the event is slightly more likely to happen than not to happen. There is not a right or wrong answer; I just want to know what you think. Let me give you an example. Imagine that you are playing Ludo. Say I ask you the chance that you will win the game. Suppose that you think that you would win for sure because you always win, you put all 10 beans in the plate. Suppose that if you think you will never win, you put no beans in the plate.
After that, in the ‘survival’ section, the respondents were asked about their survival in the upcoming 1, 5, and 10 years. The questions were asked in the following terms.
Now, I would like to ask you to consider the likelihood that you may be alive as time goes by. We hope that nothing bad will happen to you, but nevertheless, something unfortunate may occur over the next years despite all precautions that you may take. If you don’t want to, you do not need to answer this question.
Pick the number of beans that reflects how likely you think it is that
-
You will be alive one year from now.
-
You will be alive 5 years from now.
-
You will be alive 10 years from now.
Thus, for each survival question, the total score ranged between 0 and 10 according to the number of beans selected by the respondents. Further, we divided responses by 10 so that SLE is expressed as a proportion ranging from 0 to 1 in our analysis.
Explanatory variables
The primary focus of the study was to assess the association between survival expectations and health-related factors, including self-rated health, body mass index (BMI), cognition impairment, depression, limitations in basic activities of daily living (ADLs) and instrumental activities of daily living (IADL). For assessing self-rated health, the respondents were asked, “Overall, how is your health in general? Would you say it is very good, good, fair, poor, or very poor?”. For analysis purposes, we further recoded it into ‘good’ and ‘poor.’ Body mass index (BMI) was calculated by dividing weight (kg) by height squared (m2) and categorized as ‘underweight (<18.5 kg/m2)’, ‘normal (18.5–24.9 kg/m2)’, and ‘overweight/obese (≥25 kg/m2)’ (Zhang et al., 2020).
LASI adopted the Health and Retirement Study (HRS) cognition module for assessing cognitive health. Our study defined cognitive impairment based on five cognitive domains: memory, arithmetic function, orientation, executive function, and object naming. In these domains, different cognitive measures were assessed, including immediate (0–10 points) and delayed word recall (0–10 points); orientation related to time (0–4 points), and place (0–4 points); executive functioning based on paper folding (0–3 points) and pentagon drawing (0–1 points); arithmetic ability based on serial 7s (0–5 points), computation (0–2 points) and backward counting from 20 (0–2 points); and object naming (0–2 points). The overall cognition score ranges between 0 and 43. The detailed scoring of the cognitive tests was provided in the supplementary material (S1). The lowest 10th percentile is used as a proxy measure of cognitive impairment (Pandav et al., 2002).
To assess the depressive symptoms among the respondents, LASI used the 10-item Centre for Epidemiological Studies-Depression (CES-D) scale (Irwin et al., 1999; Radloff, 1977). CES-D included seven negative symptoms (feeling depressed, low energy, trouble concentrating, feeling alone, bothered by things, fear of something, and everything is an effort) and three positive symptoms (feeling happy, satisfied, and hopeful) with possible responses: rarely or never (<1 day), sometimes (1 or 2 days), often (3 or 4 days), and most or all of the time (5–7 days) in a week prior to the interview. For negative symptoms, rarely or never (<1 day) and sometimes (1 or 2 days) were scored zero, and often (3 or 4 days) and most or all of the time (5–7 days) categories were scored one. Scoring was reversed for positive symptoms. After adding the scores from the 10 items, the composite score of the depressive symptoms lies between 0 and 10. In our study, a score of four or higher is considered to represent clinically significant symptoms on the 10-item scale (Kumar et al., 2016).
The functional health of the respondents was assessed with limitations in basic and instrumental ADLs. LASI survey included six basic ADLs (BADLs) (dressing, indoor mobility, bathing, eating difficulties, getting in or out of bed, and using the toilet) and seven instrumental ADLs (IADLs) (food preparation like cooking and serving, shopping for groceries, taking medication, making telephone calls, doing work around the house or garden, ability to handle finances, and getting around or finding an address in unfamiliar places). We have created two variables for assessing the functional limitations: difficulty in ADLs (at least one difficulty in six BADLs) and difficulty in IADLs (at least one difficulty in seven IADLs).
Control variables
We included various individual, lifestyle, and household factors in our study. Various individual factors include age (in years) (60–69, 70–79, and 80+ years), education level (no education, primary, secondary, and higher), marital status (currently married, widowed, and others), working status (never worked, currently working, not currently working). Lifestyle factors included currently smoking or chewing tobacco (no, yes), and alcohol use (never, infrequent non-heavy, frequent non-heavy, and heavy episodic drinker). Various household-level factors were MPCE quintile (poorest, poorer, middle, richer, and richest), place of residence (rural, urban), religion (Hindu, Muslim, Christian, others), caste (Scheduled Caste, Scheduled Tribe, Other Backward Class (OBC), others), and regions (north, central, east, northeast, west, south).
Statistical methods
Descriptive statistics (means and percentages) were used to assess the characteristics of the older adults included in the final sample. All the analyses used LASI constructed weighting and clustering variables to account for the complex survey design of LASI. Independent t-tests were used to assess the gender difference in subjective expectations of own survival according to various health-related factors. Considering that our dependent variable, ‘survival expectations,’ is a proportion with values ranging from 0 to 1, we used generalized linear regression models (GLMs) with a logit link and a binomial family (Buis, 2010). This type of model is used to overcome the non-linear effects and non-normal error distribution, and it employs a maximum-likelihood estimator and is considered appropriate when the outcome variable lies between 0 and 1 (Buis, 2010). The analyses were conducted for the own survival expectations of the respondents for 1, 5, and 10 years for both men and women. Various individual-, lifestyle-, and household-level factors were adjusted in all the models. Stata 15.0 software was used for the analysis. A p-value of 0.10 is considered significant.
Results
Table 1 presents the sample characteristics of the older adults (2865 men and 3104 women) included in the sample. The age distribution is similar among both men and women. A higher proportion of older women were uneducated than older men (68.6% vs. 35.5%). Around 81.5% of older men and 46.1% of older women were currently married, and half of the older women (51.2%) were widowed. About 45.3% of men and 20.1% of women were employed at the time of the survey. Nearly half of older men (45.8%) and one-fifth of women (21.6%) were currently using smoke or smokeless tobacco. Heavy episodic drinking was comparatively higher among older men than women (6.7% vs. 0.8%). A higher proportion of women reported poor self-rated health than men (21.9% vs. 19.8%). The prevalence of cognitive impairment (20.7% vs. 6.7%) and depression (28.2% vs. 24.0%) was higher in older women than in men. About 20.0% of older men and 28.4% of women were either overweight or obese. Regarding activities of daily living (ADL), women had greater difficulty with both basic ADL (20.3% vs. 15.9%) and instrumental ADL (50.1% vs. 32.9%) compared to men. According to religion, around three-fourths of both older men and women participants were Hindus. Most of the participants were rural residents (65.7% men vs. 65.6% women).
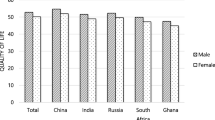
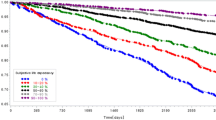
Figure 2 shows the gender differences in the average probability of own survival among older adults at 1, 5, and 10 years. The figure suggests that the average reported chances of own survival decrease with an increased time horizon in both older men and women. The weighted distribution of the subjective probability of own survival for all three survival periods (1, 5, and 10 years) is shown in Fig. 3. It depicts that the majority of the respondents reported a greater probability of their own survival for a shorter period (i.e., 1 year); however, this probability decreases with increasing time horizon (i.e., 5, 10 years). For instance, the proportion of older adults who reported a 100% probability of survival for a 1-year period was nearly 38%, compared with 12% and 6% of the respondents who reported the same for 5 and 10 years survival periods, respectively.
Table 2 presents the gender differences in own survival according to various health-related factors for the periods of 1, 5, and 10 years. Overall, older men reported a greater average probability of own survival than older women for all the time periods. Older men with good self-rated health, who were overweight or obese, had no depression, no cognitive impairment, no limitations in basic and instrumental activities of daily living, reported a significantly higher average of subjective probabilities of own survival than older women for all the time periods.
Table 3 presents the results of GLMs regressing subjective probability of own survival for different time periods, according to various health outcomes by gender, adjusted for individual-, lifestyle-, and household-level factors. Older men who reported poor self-rated health had a significantly lower subjective probability of own survival for a 1-year period (β = −0.232, SD = 0.107) and a 5-year period (β = −0.226, SD = 0.077) than those who reported good self-rated health. On the other hand, older women with poor self rated-health had a significantly lower subjective probability of own survival for a 10 years time horizon than women with good self-rated health. Underweight men had significantly lower subjective life expectancy for a 1-year period than men with normal BMI (β = −0.213, SD = 0.097). Among women, there was no significant association between BMI and own survival expectations. We did not find a significant association between cognitive impairment and own survival expectations in older men. In contrast, cognitively impaired women reported significantly lower subjective probability of own survival for a 1-year period (β = −0.399, SD = 0.108) and 5 years period (β = −0.160, SD = 0.077). Depressed older men reported significantly lower expectations of own survival for 1-year period (β = −0.309, SD = 0.101), 5-year period (β = −0.194, SD = 0.084), and 10-year period (β = −0.129, SD = 0.071). In contrast, older women with depression reported a lower subjective probability of own survival only for a 1-year period (β = −0.196, SD = 0.103); however, this association is not significant for 5 and 10 years periods. For both men and women, subjective survival probabilities were not associated with limitations in ADLs for all time periods. On the other hand, among both men and women, limitations in IADLs were significantly associated with a lower subjective probability of own survival for a 10 years period.
Discussion
Subjective survival expectancy influences major life decisions such as retirement and can have an impact on decisions taken by individuals to engage in healthy ageing activities (Ho, 2021). There has been a dearth of studies examining SLE of older Indian adults, particularly with reference to their health outcomes. This is the first population-based research that illuminates subjective and objective health outcomes that are related to SLE amongst older adults in India using a nationally representative sample. Significant associations were found with self-rated health, BMI, cognitive impairment, depression and functional limitation in IADL albeit with variation between men and women. This is consistent with previously reported research (Balia, 2014; Falba and Busch, 2005; Jylhä, 2009; Zick et al., 2014).
Stark differences between older men and women were observed in their SLE after factoring in individual, lifestyle and household level variables. This is consistent with previous research that reports gender differences in survival expectancy, and that women tend to underestimate their survival expectancy (Palloni and Novak, 2016; Philipov and Scherbov, 2020). The demographic features of the sample provide some insights into this finding. In comparison to men, a greater proportion of women had no education (68.6 vs. 35.5), were widowed (51.2 vs. 16.0), and never worked (47.7 vs. 3.8). This highlights the disadvantaged position that older women hold that could also explain their overall lower (in comparison to men) estimation of longevity for the periods of 1, 5 and 10 years. The role of family and societal gender discrimination on women’s health particularly for older women in India has been previously reported (Agewell Foundation, 2015). Older women in many households are burdened with domestic chores and caring for grandchildren, and their health concerns and perspectives are rarely considered by families and society at large resulting in health disparities. This is particularly relevant to households where women are not educated and are socially frail with restricted structural social support that eventuates with widowhood, low socioeconomic status and in rural dwellings (Borooah, 2016; Jensen, 2005; Perkins et al., 2016; Subramanian et al., 2005). Women from this study sample also reported poor self-rated health (21.9 vs. 19.8), depression (28.2 vs. 24.0), cognitive impairment (20.7 vs. 6.7) and functional limitation in IADL (50.1 vs. 32.9). These observations persisted with significant associations with SLE when individual, lifestyle and household factors were adjusted. This finding points to the greater likelihood of women having lesser opportunities to age well despite having a longer life span compared to men. This is on par with recently reported Korean research that raises concern over women’s underestimation of life expectancy (Ho, 2021).
For older men in this study sample, poor self-rated health significantly lowered their predictions of survival for 1-year and 5-year periods. Similarly, women who reported poor self-rated health also predicted their 10-year survival probability as significantly lower than their counterparts who reported good self-rated health. Current health status and the presence of comorbidities can influence older people’s self-rated health and in turn affect their predictions of longevity (Griffin et al., 2013). This also implies that people with comorbidities could have negative expectations of their health which in turn might affect their involvement in health improvement behaviours. Both men and women who had limitations in IADL had significantly lower SLE than their counterparts who did not have any limitations in this domain. Being functionally limited in one category of IADL might mean the individual perceives this as a loss of independence and can have restrictive effects on their social participation (Lahav and Katz, 2020). This finding is crucial for the early identification of at-risk individuals who could benefit from identifying new or alternative support systems to enable social engagement and well-being. Both men and women in this sample who had depression perceived their life expectancy as significantly lower. Prevalence of depression increases in older age (Pilania et al., 2019) and can contribute to negative expectations of the future and perceptions of shorter life spans. Prior research on older Indian population cohorts reported a high prevalence of late-life depression (Pilania et al., 2019) and likely associations of poor self-rated health, difficulty in ADL and IADL with late-life depression (Muhammad and Meher, 2021). These studies have also established similar associations between depression and cognitive impairment. However, in this study, we found a significant association between cognitive impairment and 1-year subjective life expectancy only amongst women. A major proportion of both men and women in this study were residents in rural areas and from the South, East and Northern regions. Socioeconomic disparities are previously reported between rural and urban dwelling older adults that disproportionately affect their access and affordability to health services (Srivastava and Muhammad, 2022). Similar differences are observed in different regions where sociocultural support networks that are available for older adults impact their health outcomes (Borooah, 2016).
Studies that have focussed on subjective longevity have mainly analysed data on Western populations, however, these studies may not be relevant to the Indian older adult cohorts that have wide socioeconomic and cultural diversity that impacts their potential and access to resources for healthy ageing. This research addresses this gap by especially providing information on health-related factors that influence SLE. This is impactful for health and social policy makers to plan services addressing the needs of the at-risk older cohorts. Estimating subjective life expectancy will enable policymakers to gain insights into the older adult’s perception of ageing, which could be utilized to determine the demands for health and social services, education and long-term care needs. It also emphasises the need for health and social policy directives that address the determinants of subjective life expectancy such as promoting a healthy lifestyle, increasing awareness and improving health and living conditions. The current findings also align with the recently conceptualized mindsponge mechanism which demonstrates that healthcare services and related information could positively influence individuals’ decision-making (Q.-H. Vuong, 2022). This mechanism also emphasizes that public trust and transparency are the most crucial factors in the healthcare system and mere improvements in infrastructure and technology without attending to the social aspects would result in negative perceptions and evaluations of patients (Q.-H. Vuong et al., 2022), which can ultimately impact their decision making negatively. The mindsponge framework also helps to explain the findings related to gender differences, where the differences could be attributed to the individual’s mind-set, framed by exposure to life events, cultural values and beliefs influencing subjective judgements and trust. The updating feature of the mindsponge framework can also help explain the association between objective health status (e.g., limitations in IADL) and lower subjective life expectancy, especially among older women. More qualitative research is warranted in this direction, exploring aspects of healthcare and individuals’ subjective judgements via a gender lens.
There are some limitations to this research. Firstly, we could only establish the presence of associations between the primary and explanatory variables and not the direction of causality owing to the restrictions of cross-sectional design. We also could not determine reverse causality, particularly considering people with terminal conditions whose response might have been largely influenced by their known survival period. Subjective life expectancy can change with age and change of circumstances. In the current study, we are limited with information obtained at one time and hence are unable to explore the factors that motivate changes to subjective longevity. Future research that examines longitudinal data is needed to identify changes in SLE and relevant motivating factors. Additionally, besides serving as a theoretical framework, mindsponge mechanism can directly support statistical analytics using the same approach (Nguyen et al., 2022). This can be a plausible direction for future research while evaluating the SLE.
Conclusion
The current findings, supporting the mindsponge mechanism, indicate that older adults base their estimation of longevity on health factors that they are aware of or not. This finding adds to the knowledge on subjective longevity for the Indian older population and has significant implications for health professionals and public policy in planning targeted interventions that can benefit at-risk population cohorts. Future studies are warranted on the aspects of healthcare services and awareness and other qualitative factors that are associated with subjective health-related judgements and LE.
Data availability
The study uses secondary data which are available on reasonable request through https://www.iipsindia.ac.in/content/lasi-wave-i.
References
Agewell Foundation (2015) Gender discrimination among older women in India - a national study. Agewell Research and Advocacy Centre. https://www.agewellfoundation.org/pdf/reports/GENDER%20DISCRIMINATION%20AMONG%20OLDER%20WOMEN%20IN%20INDIA.pdf
Australian Institute of Health and Welfare (2003) The Active Australia Survey: a guide and manual for implementation, analysis and reporting. Australian Institute of Health and Welfare
Balia S (2014) Survival expectations, subjective health and smoking: evidence from SHARE. Empir Econ 47(2):753–780
Borooah VK (2016) Gender disparities in health outcomes of elderly persons in India. J S Asian Dev 11(3):328–359
Buis ML (2010) Analyzing proportions. Eighth German Stata Users Group Meeting, 12. Census of India Website: Office of the Registrar General & Census Commissioner, India. (n.d.). https://censusindia.gov.in/. Accessed 23 Oct 2021
Delavande A, Lee J, Menon S (2017) Eliciting survival expectations of the elderly in low-income countries: evidence from India. Demography 54(2):673–699
Falba TA, Busch SH (2005) Survival expectations of the obese: is excess mortality reflected in perceptions? Obes Res 13(4):754–761
Griffin B, Loh V, Hesketh B (2013) A mental model of factors associated with subjective life expectancy. Soc Sci Med 82:79–86
Gruenewald TL, Kemeny ME (2007) Psychoneuroimmunological processes in aging and health. In Aldwin CM, Park CL, Spiro A III (eds) Handbook of health psychology and aging. The Guilford Press, pp. 97–118
Ho J-H (2021) Subjective life expectancy in transition: a longitudinal study of Korean baby boomers. Asian Popul Stud 17(2):148–161
Irby-Shasanmi A (2013) Predictors of subjective life expectancy among African Americans. Res Aging 35(3):322–347
Irwin M, Artin KH, Oxman MN (1999) Screening for depression in the older adult: criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D). Arch Intern Med 159(15):1701–1704
Jensen RT (2005) Caste, culture, and the status and well-being of widows in India. University of Chicago Press, Chicago
Jylhä M (2009) What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med 69(3):307–316
Kim J-H, Kim J-M (2017) Subjective life expectancy is a risk factor for perceived health status and mortality. Health Qual Life Outcomes 15(1):1–7
Kobayashi LC, Beeken RJ, Meisel SF (2017) Biopsychosocial predictors of perceived life expectancy in a national sample of older men and women. PLoS ONE 12(12):e0189245
Kumar S, Nakulan A, Thoppil SP, Parassery RP, Kunnukattil SS (2016) Screening for depression among community-dwelling elders: usefulness of the center for epidemiologic studies depression scale. Indian J Psychol Med 38(5):483–485
Lahav O, Katz N (2020) Independent older adult’s IADL and executive function according to cognitive performance. Occupation Particip Health 40(3):183–189
Lillie-Blanton M, Brodie M, Rowland D, Altman D, McIntosh M (2000) Race, ethnicity, and the health care system: public perceptions and experiences. Med Care Res Rev 57(1_suppl):218–235
Lima MG, Belon AP, Barros M (2016) Happy life expectancy among older adults: differences by sex and functional limitations. Rev Saúde Publica 50:64
Mirowsky J, Ross CE (2000) Socioeconomic status and subjective life expectancy. Soc Psychol Q 63(2):133–151
Muhammad T, Meher T (2021) Association of late-life depression with cognitive impairment: evidence from a cross-sectional study among older adults in India. BMC Geriatr 21(1):1–13
Nguyen M-H, La V-P, Le T-T, Vuong Q-H (2022) Introduction to Bayesian Mindsponge Framework analytics: an innovative method for social and psychological research. Methods X, 101808
Palloni A, Novak B (2016) Subjective survival expectations and observed survival: how consistent are they? Vienna Yearbook Popul Res 14:187
Pandav R, Fillenbaum G, Ratcliff G, Dodge H, Ganguli M (2002) Sensitivity and specificity of cognitive and functional screening instruments for dementia: the Indo-US Dementia Epidemiology Study. J Am Geriatr Soc 50(3):554–561
Perkins JM, Lee H, James KS, Oh J, Krishna A, Heo J, Lee J, Subramanian SV (2016) Marital status, widowhood duration, gender and health outcomes: a cross-sectional study among older adults in India. BMC Public Health 16(1):1032. https://doi.org/10.1186/s12889-016-3682-9
Philipov D, Scherbov S (2020) Subjective length of life of European individuals at older ages: temporal and gender distinctions. PLoS ONE 15(3):e0229975
Pilania M, Yadav V, Bairwa M, Behera P, Gupta SD, Khurana H, Mohan V, Baniya G, Poongothai S (2019) Prevalence of depression among the elderly (60 years and above) population in India, 1997–2016: a systematic review and meta-analysis. BMC Public Health 19(1):832. https://doi.org/10.1186/s12889-019-7136-z
Radloff LS (1977) The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas 3(1):385–401
Ross CE, Mirowsky J (2002) Family relationships, social support and subjective life expectancy. J Health Soc Behav 43(4):469–489
Ross CE, Mirowsky J (2008) Neighborhood socioeconomic status and health: Context or composition? City Community 7(2):163–179
Sarafino EP (2004) Context and perspectives in health psychology. In Sutton S, Baum A, Johnston M. The Sage handbook of health psychology. SAGE Publications Ltd, pp. 1–26
Siegel M, Bradley EH, Kasl SV (2003) Self-rated life expectancy as a predictor of mortality: evidence from the HRS and AHEAD surveys. Gerontology 49(4):265–271
Singh A, Shukla A, Ram F, Kumar K (2017) Trends in inequality in length of life in India: a decomposition analysis by age and causes of death. Genus 73(1):1–16
Smith VK, Taylor DH, Sloan FA (2001) Longevity expectations and death: can people predict their own demise? Am Econ Rev 91(4):1126–1134
Srivastava S, Gill A (2020) Untreated morbidity and treatment-seeking behaviour among the elderly in India: analysis based on National Sample Survey 2004 and 2014. SSM-Popul Health 10:100557
Srivastava S, Muhammad T (2022) Socioeconomic vulnerability and frailty among community-dwelling older adults: cross-sectional findings from longitudinal aging study in India, 2017–18. BMC Geriatr 22(1):1–11
Subramanian SV, Nandy S, Irving M, Gordon D, Smith GD (2005) Role of socioeconomic markers and state prohibition policy in predicting alcohol consumption among men and women in India: a multilevel statistical analysis. Bull World Health Organ 83:829–836
Vuong QH, Napier NK (2015) Acculturation and global mindsponge: an emerging market perspective. Int J Intercult Relat 49:354–367. https://doi.org/10.1016/j.ijintrel.2015.06.003
Vuong Q-H (2022) A New Theory of Serendipity: nature, emergence and mechanism. Walter De Gruyter GmbH
Vuong Q-H, Le T-T, La V-P, Nguyen M-H (2022) The psychological mechanism of internet information processing for post-treatment evaluation. Heliyon 8(5):e09351. https://doi.org/10.1016/j.heliyon.2022.e09351
Westerhof G, Gabrian (née Miche) M, Brothers A, Barrett A, Diehl M, Montepare J, Wahl H-W, Wurm S (2014) The influence of subjective aging on health and longevity: a Meta-Analysis of Longitudinal Data. Psychol Aging https://doi.org/10.1037/a0038016
World Health Organization (2015) World health statistics 2015. World Health Organization
Zhang J, Xu L, Li J, Sun L, Qin W (2020) Association between obesity-related anthropometric indices and multimorbidity among older adults in Shandong, China: a cross-sectional study. BMJ Open https://doi.org/10.1136/bmjopen-2019-036664
Zick CD, Smith KR, Mayer RN, Taylor LB (2014) Family, frailty, and fatal futures? Own-health and family-health predictors of subjective life expectancy. Res Aging 36(2):244–266
Author information
Authors and Affiliations
Contributions
Conceived and designed the research paper: SS and T.M; Analysed the data: MK; Contributed agents/materials/analysis tools: T.M, SS and PS; Wrote the manuscript: PS, T.M, SS and MK. All authors read, reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The Indian Council of Medical Research (ICMR) extended the necessary guidance, guidelines and ethical approval for conducting the LASI survey. And all methods were carried out in accordance with relevant guidelines and regulations as per the Declaration of Helsinki.
Informed consent
The survey agencies that conducted the field survey for the data collection collected prior consent (signed and oral) for both the interviews and biomarker tests from the eligible respondents in accordance with Human Subjects Protection.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kumar, M., Srivastava, S., Muhammad, T. et al. Examining the association between health status and subjective life expectancy among older Indian adults based on the mindsponge approach. Humanit Soc Sci Commun 9, 359 (2022). https://doi.org/10.1057/s41599-022-01368-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1057/s41599-022-01368-1
- Springer Nature Limited