Abstract
The World Health Organization (WHO) recognizes a critical shortage of health workers as a growing global crisis. The shortage persists despite local and global efforts to recruit health workers ethically. Unequal migration of healthcare professionals, most often from low to high-resource countries, overwhelmingly defeats the objective of achieving Universal Health Coverage (UHC). If not addressed, especially given emerging global pandemics like COVID-19, the critical shortage of health workers could decimate vulnerable public health systems. This Viewpoint describes the Root-Stem Model, a six-stage process of strategic factors affecting work life that could help policymakers address the challenge of brain-drain among healthcare workers in low-income countries.
Similar content being viewed by others
Key messages
-
Critical shortage of healthcare workers driven by brain-drain is a growing global health crisis with important public health effects in low-resource settings.
-
The Root Stem Model (RSM) of workforce retention uses a multistage cyclic process encompassing education, recruitment, job training, work environment, remuneration, and investment of work gains, and resources for analyzing work life and opportunities for improvement.
-
The RSM enables effective policy interventions against brain drain by offering an integrated view of the workers’ needs, a framework for measuring and comparing the effectiveness of human resource programs or policies simultaneously, or both.
Introduction
The World Health Organization defines ‘health system’ as the combination of all organizations, people, and actions whose primary intent is to promote, restore or maintain health [1]. Health care workers (HCW) are the most important component of a health system [2]. Equitable distribution of HCWs and their services across populations is paramount to meeting health needs. Since the colonial era, historians have documented the migration of HCWs from low-income regions to affluent parts of the globe. In 1972, approximately 6% of doctors worldwide were expatriates; 75% of them worked in the United States of America (US), the United Kingdom (UK), and Canada [3]. Anyangwe and Mtonga reported that in 2007, the US had 14% of the global population, 10% of the global disease burden, 37% of the world’s health workforce, and 50% of worldwide expenditure of funds for health. Sub-Saharan Africa, with about 11% of the global population, had 24% of the world’s disease burden, but only 3% of the world’s health personnel, and accounted for less than 1% of the global expenditures on health [4]. This situation has not improved. As Haakanestad et al., reported, more than half of the global shortfall in each healthcare cadre is in sub-Saharan Africa and south Asia [5].
Even in high-resource countries, a shortage of healthcare workers is a notable public health concern, especially in rural settings. Globally, 75% of physicians and 65% of nurses work in urban areas, even though half of the world's population lives in rural areas [6]. The United States has an average of 30.8 physicians (MDs) per 10,000 people in urban areas compared to 10.9 in rural areas [7, 8]. In Australia, rural populations (mostly Aboriginal and Torres Strait Islanders) constitute 28% of the entire population but studies show that policymakers address their public health concerns 22% below the expected national average [9]. As a result, this remote population receives less quantity and quality of health services than that enjoyed by other Australians [10]. Industrialized countries recruit international medical graduates (IMGs) and other HCWs for their rural populations mainly from low-resource countries. In the US, the Conrad State 30 Program permits each of the 50 states to use special immigration provisions (the J-1 Visa Waivers) to employ up to 30 international medical graduates (IMGs) [11, 12]. UK-trained doctors dislike working in low-resource settings, even in the UK, hence concentrate in cities, leaving the National Health Service (NHS) to depend on IMGs in such areas [13]. Countries including the US, UK, Canada [14, 15], New Zealand and Australia [16,17,18] annually recruit foreign-trained HCWs from low-resource countries to compensate for their growing deficit in the rural medical workforce. This practice creates an even more serious deficit than would exist if all graduates were to remain in the supplying countries. Who will compensate for the gaps in national health systems?
Universal Health Coverage
Universal Health Coverage is both a technical framework and a hope, especially for underserved populations. The hope is to create societies globally characterized by justice and equity in the provision of services. Adequate availability and distribution of healthcare staff, especially physicians, are key to increasing access to essential health services and to achieve the desired health outcomes. The WHO recommends a doctor-to-population ratio of 1:1000 [19], but in 2017 approximately 40% of its member countries remained below this ratio [6].
Recent emergence of the COVID-19 pandemic underscores the undeniable fact that public health is ‘non-divisible’ and ‘non-excludable’ among groups constituting a population, hence it fits the definition of ‘public good’ [20]. Public goods, once produced, benefit all and the price of eliminating nonpayers from enjoying the benefits of the good or service inhibits achieving full welfare value for all [21]. In 1976, Dr. Halfdan Mahler, then Director General of the World Health Organization (WHO) proclaimed his vision for a Health for All by 2000 policy initiative [22]. In 1978, he set out his vision in a more functional and explicit way that led the world to sign the Declaration of Alma-Ata [23]. The Declaration proclaimed access to basic health services to be a fundamental human right. It also coined the term ‘primary health care’ (PHC), and called it a universal, community-based public health model focusing on preventive and curative services [24]. The concept of 2010 WHO’s Universal Health Coverage (UHC) stems from Dr. Mahler’s Health for All by 2000 initiative. In 2008, Dr. Mahler confessed that his intention had not been to eradicate all diseases and illnesses by 2000 but to draw the world’s attention on health inequities [22]. By ensuring a continued battle against health inequalities, UHC seeks to:
ensure that all people can use the promotive, preventive, curative, rehabilitative and palliative health services they need, of sufficient quality to be effective, while also ensuring that the use of these services does not expose the user to financial hardship (WHO, 2010) [25].
The UHC model has three pillars: equal population coverage, provision of a variety of health services, and reduction of out-of-pocket health expenditures [26]. All three depend on the availability of skilled healthcare workers. Investment in recruiting, training, and retaining healthcare workers is essential if governments are to improve their primary healthcare systems. Unbalanced migration of health workers wastes investment in national medical education as well as causing critical shortages of the health workforces where they are most needed.
COVID-19 an accelerating or inhibiting context for health worker’s migration
During the pandemic of COVID-19, the world has experienced rising mortality rates, attributable directly and indirectly to coronavirus infection [27]. This situation has overwhelmed healthcare systems by filling hospital beds with COVID-19 patients, reducing care for those with serious non-COVID-19 conditions, while limiting admissions and accelerating earlier patient discharges from hospitals. These necessities crippled other hospital functions and strained human resources [28,29,30,31]. The need for health care workers increased during the pandemic, even more in lower resource countries than elsewhere. The COVID-19 pandemic inhibited the usual migration of healthcare workers through travel restrictions and border closures around the world. In some way these travel restrictions helped developing economies, if temporarily, to retain health workers, and opened a window for creating policies to retain workers post-pandemic.
High-resource countries eased their usual ways of employing foreign medical doctors during the pandemic. The US removed a requirement for these doctors to pass the United States Medical Licensing Examination (USMLE) STEP 2 Clinical Skills examination to practice in their country [32]. The suspended exam was part of the second phase of the three-step examination process for physicians’ medical licensure in the U.S. The European Commission, UK, and all other member countries of the Organization for Economic Co-operation and Development (OECD) introduced policies that facilitated border crossing for foreign health professionals and recognition of their qualifications. Both expedited addition of these HCWs to work in their health systems [33]. These high resources increased efficiency in recruiting to compensate for a shortage of HCWs while maintaining COVID-19 precautions.
Thus, pandemic restrictions slowed the brain drain, and afforded an opportunity for policymakers from both spheres to reflect on the health worker’s migration inequalities. The post-pandemic period requires the formulation of an ethical global policy framework, to assist WHO’s Global Health Workforce Network to engage in practical steps against HCWs brain drain.
The Root Stem Model of health worker’s retention
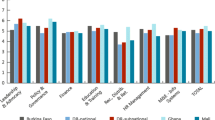
To gain insights into how health systems in lower resource settings can retain their workforces, especially during the COVID19 pandemic and under similar circumstances in the future, we propose the use of the Root Stem Model (RSM). It offers a holistic approach for exploring workforce retention by strategically targeting the workforce process stages: (1) Academic education (2) recruitment; (3) job training; (4) remuneration; (5) workforce environment; (6) investment in skills and resources. This model treats work life as affected by various related factors, in a multistage cyclic process (Fig. 1). Below we illustrate the importance of each step.
Academic education
The former President of South Africa, Nelson Rolihlahla Mandela, once said “Education is the most powerful weapon which you can use to change the world.” [34]. Neither the United States [35] nor Ireland [36] solved its problem of retaining its medical workforce for underserved areas by increasing the numbers of medical students. The qualities of doctors proved to be more important. Medical education strategies most likely to influence graduating physicians to work in rural or low resource settings include: providing medical curricula in rural settings, improving admission policies to enroll more rural students, providing conditional scholarships in deprived areas, establishing rural preceptorships, and enhancing undergraduate rural medicine programs [37, 38].
Worldwide most medical schools remain in urban areas [35, 39] and adapt medical students to urban environments. Medical schools could establish satellite rural campuses for at least some courses. And governments should construct new medical schools in rural areas and recruit more local rural students to serve their own communities. A recent Australian study of medical students found that rural practice self‐efficacy is positively related to current rural practice and future intention to practice rurally [40].
Recruitment and job training
Thailand suffered a critical shortage and maldistribution of the health workforce for a long time before making major policy changes. In 1994 and 2005, the Ministry of Education and the Ministry of Public Health (MOPH) sponsored two national programs: the Collaborative Project to Increase Production of Rural Doctors (CPIRD) and One District One Doctor (ODOD), respectively [41,42,43]. CPIRD recruits medical students from their rural domiciles; ODOD recruits from more targeted remote rural areas and provides full government scholarships. Both are ‘bonding schemes.’ That is, they obligate health professional beneficiaries of government scholarships to work in public service for a specified period of time after graduating. Assessments of the Thai programs in 2015 and 2017 revealed that 92% of medical graduates stayed in rural areas and were likely to continue there [43, 44]. These results imply that policy strategies focused on rural recruitment of medical students, community-based medical education, mandatory service, and hometown placement contribute to improving retention.
Job training refers to “a planned effort by a company to facilitate employees’ learning of job-related competencies” [45]. It requires continuous investment in human resources to acquire up-to-date skills, knowledge, and expertise to achieve organizational goals [45]. A competent human resource is easily motivated, autonomous, and makes substantial contributions to the organization’s productivity. Such people help organizations cope with competing forces affecting the workplace by cultivating employee competence at required levels. Continuing professional development training programs and social and emotional support programs for rural HCWs are both effective for retention [6]. On-job and off-job training are key for employee job satisfaction; both play pivotal roles in grooming, retaining and attracting well-qualified personnel, especially in medical institutions where specialist training and retention are highly important [46]. Job training promotes learning and a positive change in employee professional behavior [47]. It is a key factor for retaining workers.
Workforce environment
Favorable workforce environments require collaboration among policy stakeholders at departmental, district, national, regional, and global levels [48]. Strategies that target improving the external socio-physical environment as well as psycho-personal needs of health workers are more effective than either alone [49]. Efforts to recruit and retain health workers in remote areas are more effective if governments address work environment issues including housing, communication systems, running water, road conditions, adequacy of medical supplies, quantity and quality of medical facilities, and continuing educational opportunities [50, 51]. And to make rural communities appeal to HCWs, policymakers should create desirable work environments with supportive management, safe and well-equipped clinical work environments, and broadband internet [52].
Motivating factors for job satisfaction include recognition, involvement in decision-making processes, promotions, achievement, autonomy, communication, job importance, degree of professionalism, organizational climate, interpersonal relationships, working for a reputable agency, supervisory support, positive affectivity, job security, workplace flexibility, working within a team environment and reasonable working hours [46].
Remuneration
Tanzania, Rwanda, and Burundi, among others, have tried Pay for Performance (P4P) schemes, also called Performance-based financing (PBF), to improve poor health worker performance and shortages [53]. Performance-based financing means funding healthcare workers, in part, based on performance to encourage health workers and management to improve efficiency, quality of care, and retention in low-resource countries [54]. Research indicates added benefits if managers ask workers for feedback and involve them in policy-making processes [46].
Paying rural allowances sufficient to compensate for health worker’s inability to engage in extra jobs for more income can support retention. If such compensation is too small and infrequent, however, it may result in demotivation [55, 56]. In Israel, incentives affected residency location decisions for young doctors, particularly among those who grew up in remote areas; 65% of these doctors opted to continue working there. Combining recruitment of medical students from remote areas and meaningful incentives can improve their intention to stay [57]. Thus, it is important to combine targeted incentives with other retention measures.
Investment
A 2016 study to investigate the importance of motivation factors in rural health workers in Sierra Leone found that poor working conditions, financial costs of separation from families, limited access to further training, longer working hours (due to staff shortages), and inability to earn from other sources made working in rural areas less attractive [55]. A study in the US showed that an increase in healthcare expenditure resulted in better economic performance that boosted income, national gross domestic product (GDP), productivity, and poverty alleviation [58]. Expansion of medical tourism expansion may also boost foreign currency reserves that LIC countries can use to help retain skilled health workers [59]. Authors of a study in Uganda concluded that policymakers should prioritize adequate remuneration, equitable job promotions, and leadership opportunities for rural health workers by financial investments to increase opportunities for rural health workers to equal or exceed those of their urban counterparts [60]. For low- and middle-income countries investing in public health for all improves social welfare and stimulates economic growth [61].
Next steps
The Root Stem Model (RSM), highlighting the interconnectivity of stages for preparing and retaining HWCs, could be applied as a conceptual policy framework to early-stage processes of reforming health policy. It takes into account important factors in the global health workforce labor markets and can help guide macro and micro-policy-making processes and simulations [62]. As a microsimulation model it can help its users to analyze the effects of health care reform on “improved healthcare access”—cost and coverage of care and compare the effectiveness of human resource programs or policies simultaneously, or at different times and/or places. As to drawbacks, this model provides only low specificity on particular issues, and hence cannot be used alone to assess specialized programs. Altogether, RSM can be instrumental in offering a quick cross-sectional view and guide which functions to determine, and develop efficient policy strategies and sequences that can deliver favorable outcomes in human resources, health services, and health finance management policies for governments, and non-state actors in public health.
Conclusion
This Viewpoint presented measures to ease the consequences of ‘brain drain’, unequal migration, and ill-distribution of healthcare workers between developed and developing countries, and between urban and rural areas. We propose the adoption of the Root Stem Model to guide formulation, monitoring, and evaluation of policies and programs to relieve shortages of health workers in low-resource settings. Comprehensive policies should target all parts of the process to bring job satisfaction, organizational commitment, and, ultimately, retention of healthcare workers.
References
Durán A, Kutzin J, Martin-Moreno JM, Travis P. Understanding health systems: scope, functions and objectives. Health systems: Health, wealth, society and wellbeing Maidenhead. Open University Press: McGraw-Hill; 2011. p. 19–36.
Joseph B, Joseph M. The health of the healthcare workers. Indian J Occup Environ Med. 2016;20(2):71–2.
Bach S. Migration patterns of physicians and nurses: still the same story? Bull World Health Organ. 2004;82(8):624–5.
Anyangwe SCE, Mtonga C. Inequities in the global health workforce: the greatest impediment to health in sub-Saharan Africa. Int J Environ Res Public Health. 2007;4(2):93–100.
Haakenstad A, Irvine CMS, Knight M, Bintz C, Aravkin AY, Zheng P, et al. Measuring the availability of human resources for health and its relationship to universal health coverage for 204 countries and territories from 1990 to 2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet. 2022;399(10341):2129–54.
Mosadeghrad AM, Isfahani P. Physician retention in deprived areas: a letter to the editor. Tehran Univ Med J TUMS Publ. 2022;79(12):992–3.
Hub RHI. Rural Healthcare Workforce USA: 2021; 2021 [updated 3/30/2021; cited 2021 3/30/2021]. https://www.ruralhealthinfo.org/topics/health-care-workforce.
Services USDoHaH. AREA HEALTH RESOURCES FILES (AHRF) USA: U.S. Department of Health and Human Services 2018 [updated 3/30/2021; cited 2021 3/30/2021]. https://data.hrsa.gov/.
Roberts R, Maylea C. Is rural mental health workforce a policy imperative? Aust J Rural Health. 2019;27(5):454–8.
Cosgrave C. The whole-of-person retention improvement framework: a guide for addressing health workforce challenges in the rural context. Int J Environ Res Public Health. 2020;17(8):2698.
Johnson K, Kaltenbach E, Hoogstra K, Thompson M, Hagopian A, Hart L. How international medical graduates enter US graduate medical education or employment. New York: WWAMI Center for Health Workforce Studies, University of Washington, School of Medicine, Department of Family Medicine; 2003.
Klaric S. The Conrad State 30 Improvement Act: remedying the physician shortage. S Cal Rev L Soc Just. 2008;18:611.
Simpson JM. Where are UK trained doctors? The migrant care law and its implications for the NHS–an essay by Julian M Simpson. BMJ. 2018;361:k2336.
Baerlocher MO. The importance of foreign-trained physicians to Canada. Clin Invest Med. 2006;29(3):151–3.
Hoag H. Canada increasingly reliant on foreign-trained health professionals. Can Med Assoc J. 2008;178(3):270.
Han G-S, Humphreys JS. Overseas-trained doctors in Australia: community integration and their intention to stay in a rural community. Aust J Rural Health. 2005;13(4):236–41.
Gorman DF, Brooks PM. On solutions to the shortage of doctors in Australia and New Zealand. Med J Aust. 2009;190(3):152–6.
Arnold P. A unique migration: South African doctors fleeing to Australia: CreateSpace USA; 2011.
Kumar R, Pal R. India achieves WHO recommended doctor population ratio: a call for paradigm shift in public health discourse! J family Med Primary Care. 2018;7(5):841–4.
Chen LC, Evans TG, Cash RA. Health as a global public good. Glob Public Goods. 1999;1:284–304.
Cowen T. Public goods. The concise encyclopedia of economics. 2008:197–9.
Snyder A. Halfdan mahler. The Lancet. 2017;389(10064):30.
To A. Health for all beyond 2000: the demise of the Alma-Ata Declaration and primary health care in developing countries. Med J Aust. 2003;178(1):17–20.
Muldoon LK, Hogg WE, Levitt M. Primary care (PC) and primary health care (PHC). Can J Public Health. 2006;97(5):409–11.
Watkins DA, Jamison DT, Mills T, Atun T, Danforth K, Glassman A, et al. Universal Health Coverage and Essential Packages of Care. In: Jamison DT, Gelband H, Horton S, Jha P, Laxminarayan R, Mock CN, et al., editors. Disease Control Priorities: Improving Health and Reducing Poverty. Washington (DC): The International Bank for Reconstruction and Development/The World Bank © 2018 International Bank for Reconstruction and Development / The World Bank.; 2017.
Mathur MR, Williams DM, Reddy KS, Watt RG. Universal health coverage: a unique policy opportunity for oral health. J Dent Res. 2015;94(3 Suppl):3S-5S.
Islam N, Shkolnikov VM, Acosta RJ, Klimkin I, Kawachi I, Irizarry RA, et al. Excess deaths associated with covid-19 pandemic in 2020: age and sex disaggregated time series analysis in 29 high income countries. BMJ. 2021;373:n1137.
Tangcharoensathien V, Bassett MT, Meng Q, Mills A. Are overwhelmed health systems an inevitable consequence of covid-19? Experiences from China, Thailand, and New York State. BMJ. 2021;372:n83.
Dorsett M. Point of no return: COVID-19 and the U.S. healthcare system: an emergency physician’s perspective. Sci Adv. 2020;6(26):eabc5354.
Amat Y, editor Barcelona Institute for Global Health (ISGlobal). CUGH 2021 Virtual Conference: CUGH.
Mohamed K, Rezaei N, Rodríguez-Román E, Rahmani F, Zhang H, Ivanovska M, et al. International efforts to save healthcare personnel during COVID-19. Acta Biomed. 2020;91(3):e2020044-e.
Rajesh A, Desai TJ, Patnaik R, Asaad M. Termination of the USMLE step 2 CS: perspectives of surgical residents with diverse medical backgrounds. J Surg Res. 2021;265:60–3.
Scarpetta S, Dumont J-C, Socha-Dietrich K. Contribution of migrant doctors and nurses to tackling COVID-19 crisis in OECD countries. Paris: OECD; 2020. p. 10.
Baggaley R, Calleja JMG, Marum L, Marum E. Knowledge is power; information is liberation. Bull World Health Organ. 2013;91(12):898.
Evans DV, Jopson AD, Andrilla CHA, Longenecker RL, Patterson DG. Targeted medical school admissions: a strategic process for meeting our social mission. Fam Med. 2020;52(7):474–82.
Humphries N, Crowe S, Brugha R. Failing to retain a new generation of doctors: qualitative insights from a high-income country. BMC Health Serv Res. 2018;18(1):144.
Curran V, Rourke J. The role of medical education in the recruitment and retention of rural physicians. Med Teach. 2004;26(3):265–72.
Hsueh W, Wilkinson T, Bills J. What evidence-based undergraduate interventions promote rural health? N Z Med J. 2004;117(1204):U1117.
Rabinowitz HK, Paynter NP. The rural vs urban practice decision. JAMA. 2002;287(1):113.
Bentley M, Dummond N, Isaac V, Hodge H, Walters L. Doctors’ rural practice self-efficacy is associated with current and intended small rural locations of practice. Aust J Rural Health. 2019;27(2):146–52.
Lertsukprasert S. Collaborative Project to Increase Production of Rural Doctors to Tackle Physician Shortage Problem of Ministry of Public Health—โครงการผลิตแพทย์เพื่อชาวชนบทกับการแก้ไขปัญหาความขาดแคลนแพทย์ของกระทรวงสาธารณสุข. J Health Sci วารสารวิชาการสาธารณสุข. 2018;17(Sup.7):SVII1906–14.
Putthasri W, Suphanchaimat R, Topothai T, Wisaijohn T, Thammatacharee N, Tangcharoensathien V. Thailand special recruitment track of medical students: a series of annual cross-sectional surveys on the new graduates between 2010 and 2012. Hum Resour Health. 2013;11(1):47.
Arora R, Chamnan P, Nitiapinyasakul A, Lertsukprasert S. Retention of doctors in rural health services in Thailand: impact of a national collaborative approach. Rural Remote Health. 2017;17(3):1–10.
Nithiapinyasakul A, Arora R, Chamnan P. Impact of a 20-year collaborative approach to increasing the production of rural doctors in Thailand. Int J Med Educ. 2016;7:414–6.
Huang W-R. Job training satisfaction, job satisfaction, and job performance. Career Dev Job Satisf. 2019:25.
Rad AMM, Yarmohammadian MH. A study of relationship between managers' leadership style and employees' job satisfaction. Leadership in Health services. 2006.
Crutzen R, Peters G-JY. Evolutionary learning processes as the foundation for behaviour change. Health Psychol Rev. 2018;12(1):43–57.
Khalil M, Alameddine M. Recruitment and retention strategies, policies, and their barriers: a narrative review in the Eastern Mediterranean Region. Health Sci Rep. 2020;3(4):e192.
Sirili N, Simba D. It is beyond remuneration: bottom-up health workers’ retention strategies at the primary health care system in Tanzania. PLoS ONE. 2021;16(4):e0246262.
Goma FM, Tomblin Murphy G, MacKenzie A, Libetwa M, Nzala SH, Mbwili-Muleya C, et al. Evaluation of recruitment and retention strategies for health workers in rural Zambia. Hum Resour Health. 2014;12(1):S1.
Shah SM, Zaidi S, Ahmed J, Rehman SU. Motivation and retention of physicians in primary healthcare facilities: a qualitative study from Abbottabad, Pakistan. Int J Health Policy Manag. 2016;5(8):467–75.
Abelsen B, Strasser R, Heaney D, Berggren P, Sigurðsson S, Brandstorp H, et al. Plan, recruit, retain: a framework for local healthcare organizations to achieve a stable remote rural workforce. Hum Resour Health. 2020;18(1):63.
Ireland M, Paul E, Dujardin B. Can performance-based financing be used to reform health systems in developing countries? Bull World Health Organ. 2011;89(9):695–8.
Olafsdottir AE, Mayumana I, Mashasi I, Njau I, Mamdani M, Patouillard E, et al. Pay for performance: an analysis of the context of implementation in a pilot project in Tanzania. BMC Health Serv Res. 2014;14(1):392.
Wurie HR, Samai M, Witter S. Retention of health workers in rural Sierra Leone: findings from life histories. Hum Resour Health. 2016;14(1):3.
Makapela NC, Useh U. Rural allowance and the retention of health professionals in selected Hospitals in the North West Province of South Africa. J Hum Ecol. 2013;44(2):129–38.
Ashkenazi Y, Gordon M, Rosen B. Using financial incentives to attract medical residents to the periphery: the Israeli experience. Health Policy. 2019;123(1):80–6.
Raghupathi V, Raghupathi W. Healthcare expenditure and economic performance: insights from the United States data. Front Public Health. 2020;8:156.
Beladi H, Chao C-C, Ee MS, Hollas D. Medical tourism and health worker migration in developing countries. Econ Model. 2015;46:391–6.
Namusoke Kiwanuka S, Akulume M, Tetui M, MuhumuzaKananura R, Bua J, Ekirapa-Kiracho E. Balancing the cost of leaving with the cost of living: drivers of long-term retention of health workers: an explorative study in three rural districts in Eastern Uganda. Glob Health Action. 2017;10(sup4):1345494.
Jamison DT, Summers LH, Alleyne G, Arrow KJ, Berkley S, Binagwaho A, et al. Global health 2035: a world converging within a generation. The Lancet. 2013;382(9908):1898–955.
Ringel JS, Eibner C, Girosi F, Cordova A, McGlynn EA. Modeling health care policy alternatives. Health Serv Res. 2010;45(5 Pt 2):1541–58.
Acknowledgements
None.
Funding
No funding was received for the current study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interest
The author declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Makuku, R., Mosadeghrad, A.M. Health workforce retention in low-income settings: an application of the Root Stem Model. J Public Health Pol 43, 445–455 (2022). https://doi.org/10.1057/s41271-022-00361-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1057/s41271-022-00361-x